Summary
Background
The aim of this study was to compare the possible clinical parameters for prediction of successful labor induction in Chinese nulliparous women.
Material/Methods
A retrospective, observational trial of labor induction was performed, using a single dose of 10 mg controlled-release dinoprostone for preinduction cervical ripening in 127 nulliparous women (gestational age 38–42 weeks, singleton cephalic presentation). The characteristics of the women with successful labor induction (defined as vaginal delivery achieved on the day of admission; n=80) and failed labor induction (n=47) were compared.
Results
The main differences observed between the groups were gravidity (P<0.05), induction-active labor interval (5.16±2.98 vs. 8.40±3.41; P<0.05) and birth weight (3421.11±368.14 vs. 3566.36±345.16; P<0.05). Logistic regression demonstrated that gravidity (P<0.05) and induction-active labor interval (P<0.05), but not Bishop score, were significant and independent contributing factors for successful labor induction. In the receiver operating characteristic curves for the prediction of successful labor induction, the best cut-off value for gravidity was 3 (95% confidence interval [CI] 0.64–0.83, P=0.000), and the best cut-off value for the induction-active labor interval was 7.96 (95%CI 0.66–0.85, P=0.000).
Conclusions
Less gravidity and shorter induction-active labor interval predict successful labor induction with reasonable accuracy.
Keywords: Bishop score, gravidity, labor induction, nulliparous women
Background
Induction of labor is a safe and efficacious method for vaginal delivery, but there is an increased risk of failed induction and subsequent cesarean delivery [1]. Moreover, an unplanned emergency cesarean delivery during labor poses increased risk for maternal morbidity and mortality in comparison with a planned elective cesarean delivery [2–4]. Therefore, several attempts have been made to predict the outcome of labor induction.
Traditionally, the assessment of the status of the cervix before labor induction has been accomplished using the Bishop score. In addition to this, it has been suggested that a variety of other maternal and fetal factors, as well as screening tests, can be used to predict the success of labor induction. Certain characteristics of the woman (parity, age, weight, height and body mass index), and of the fetus (birth weight and gestational age) have been associated with the success of labor induction [5–10], but there has been no research into this in Chinese women. Dinoprostone is the most commonly used agent for preinduction cervical ripening in China, the effects and properties of which have been extensively investigated [11–15]. The purpose of this study was to identify the clinical parameters that can be used to predict the outcome of induction of labor in nulliparous Chinese women.
Material and Methods
Patient characteristics
From January 2008 to January 2009, 127 nulliparous women were prospectively recruited into the study. The investigation was approved by the Institutional Ethics Committee. All patients gave written consent prior to cervical assessment. The study included nulliparous women between 38 and 42 weeks of gestation (assessed by rigorous menstrual history or an ultrasound conducted before 20 weeks), with singleton pregnancy, cephalic presentation, Bishop score ≤6 and absence of active labor. Exclusion criteria were uterine scar due to previous cesarean delivery or myomectomy, placenta previa, allergy or asthma in response to prostaglandins, and abnormal non-stress test result before the induction. Patients were assessed by digital examination using the Bishop score, which included 5 parameters that give a score of 0–10 points. The Bishop score was assessed by 2 operators, blinded to the results of the other examiner.
Procedures
Preinduction cervical ripening was performed using 10 mg of controlled-release dinoprostone inserted as a single dose (Propess 10 mg, Controlled Therapeutics, East Kilbride, Scotland). The insert is a preparation of prostaglandin E2 packaged in a hydrogel polymer matrix and designed for slow intravaginal release of 10 mg dinoprostone at a rate of 0.3 mg/h over 12 h. Oxytocin augmentation was started in women with unsatisfactory progress of labor (failure of progressive cervical dilatation and fetal descent, and/or inadequate uterine activity). Continuous electronic fetal heart rate monitoring was employed.
For the purpose of the study analysis, the women were divided into 2 groups, with either successful or failed induction of labor. Induction was defined as successful only if vaginal delivery was achieved by induction protocols started on the day of admission. Patients who were given night rest and had the procedures restarted the next day were classified as failed induction, even if they subsequently delivered vaginally. The induction-active labor interval was defined as the period from the administration of dinoprostone to the establishment of regular uterine activity.
Statistical analysis
Data were entered into the statistical software program SPSS13.0. Normally distributed data were analyzed via the Kolmogorov-Smirnov test. Results are presented as the mean±SD or median. The Wilcoxon rank sum test was used for ranked data, and measurement data were compared with t-test or non-parametric rank sum test. In order to deal with uncertainty in estimation, 95% confidence intervals (CI) were generated for post-test probabilities around the point estimate. Univariate and multivariate logistic regression analysis was performed to determine the variables that contributed to the prediction of labor. Receiver operating characteristic (ROC) curves were used to assess the ability of clinical parameters to predict labor induction. For 2-sided tests, P<0.05 was considered statistically significant.
Results
General results
Baseline characteristics of both treatment groups are presented in Tables 1, 2. There were no statistically significant differences in race, maternal age, gestational age, body mass index, the fetal sex or the Bishop score at the time of admission (Table 1). The gravidity in the successful labor induction group was less than in the failed labor induction group (P<0.05). Indications for labor induction were impaired glucose tolerance (IGT) or gestational diabetes mellitus (GDM; n=38), postdates (n=36), premature rupture of membranes (n=19), macrosomia (n=8), hypertension disorders (n=6) and other medical or fetal problems necessitating delivery (n=20). The indications did not differ between the failed and successful labor induction groups. Mean induction-active labor interval in the successful labor induction group was shorter than in the failed labor induction group (5.16±2.98 vs. 8.40±3.41; P<0.001; Table 2). Mean birth weight in the successful labor induction group was lower than in the failed labor induction group (3421.11±368.14 vs. 3566.36±345.16; P<0.05).
Table 1.
The clinical characteristics of the study population.
| Characteristics | Successful induction (n=80) | Failed induction (n=47) | P value |
|---|---|---|---|
| Maternal age, years | 29.50±2.73 | 29.43±2.80 | 0.883 |
| Gestational age, weeks | 39.78±1.02 | 39.96±1.06 | 0.352 |
| Body mass index, kg/m2 | 20.51±2.21 | 20.69±2.59 | 0.413 |
| Gravidity, n (%) | 0.038* | ||
| 1 | 39 (48.8%) | 18 (38.3%) | |
| 2 | 29 (36.3%) | 13 (27.7%) | |
| ≥3 | 12 (15.0%) | 16 (34.0%) | |
| Indications for induction | |||
| GDM or IGT | 21 (26.3%) | 17 (36.2%) | 0.205 |
| Prolonged pregnancy | 21 (26.3%) | 15 (31.9%) | 0.442 |
| PROM | 12 (15.0%) | 7 (14.9%) | 0.968 |
| Pregnancy-related hypertension | 5 (6.3%) | 1 (2.1%) | 0.415 |
| Large for gestational age | 3 (3.8%) | 5 (10.6%) | 0.229 |
GDM – gestational diabetes mellitus; IGT – impaired glucose tolerance; PROM – premature rupture of membranes;
P<0.05 by Wilcoxon Rank-Sum Test.
Table 2.
The clinical characteristics of the study population.
| Characteristics | Successful induction (n=80) | Failed induction (n=47) | P value |
|---|---|---|---|
| Bishop score | 3.99±1.20 | 3.91±1.20 | 0.740 |
| Induction-active labor interval | 5.16±2.98 | 8.40±3.41 | 0.002* |
| Uterine hyperstimulation | 9 (11.3%) | 5 (10.6%) | 0.953 |
| Meconium-stained amniotic fluid | 17 (21.2%) | 14 (29.8%) | 0.247 |
| Abnormal fetal heart rate | 25 (31.3%) | 9 (19.1%) | 0.159 |
| Apgar score < 7 | 8 (10.0%) | 1 (2.1%) | 0.201 |
| Birth weight, g | 3421.11±368.14 | 3566.36±345.16 | 0.033* |
| Male | 36 (45.0%) | 19 (40.4%) | 0.833 |
P<0.05 by Student’s t test.
Of the 127 women recruited, 80 (63%) delivered vaginally within 24 h of labor induction. Of the remaining 47 women classified as having failed induction, 16 (34%) delivered vaginally the next day after rest for a night and repetition of the same induction protocol, and 31 (66%) underwent cesarean delivery. The indications for cesarean section were patient request for social reasons (n=19), arrest of cervical dilation (n=4), intrapartum repetitive late and/or severe variable fetal heart rate decelerations (n=3), meconium-stained amniotic fluid (n=3) and arrest of fetal descent (n=2).
Logistic regression
In a univariate logistic regression model that included all variables that might have an effect on the success of labor induction, gravidity (OR=0.61, 95%CI 0.408–0.892; P=0.011) and induction-active labor interval (OR=0.85, 95%CI 0.769–0.937; P=0.001) correlated significantly with successful induction. The 5 components of the Bishop score alone, and the total Bishop score were, however, not associated with successful vaginal delivery within 24 h of induction (Table 3).
Table 3.
Logistic regression analysis of the relationship between successful labor induction and the independent variables.
| Variable | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| Odds ratio (95% CI) | P | Odds ratio (95% CI) | P | |
| Gestational age | 1.010 (0.885–1.152) | 0.882 | ||
| Gravidity | 0.603 (0.408–0.892) | 0.011* | 0.653 (0.433–0.983) | 0.041** |
| Bishop score total | 1.053 (0.779–1.423) | 0.738 | ||
| Dilatation | 0.993 (0.939–1.050) | 0.816 | ||
| Effacement | 1.017 (0.633–1.635) | 0.943 | ||
| Consistency | 1.155 (0.647–2.060) | 0.626 | ||
| Position | 1.060 (0.534–2.104) | 0.868 | ||
| Station | 0.955 (0.479–1.904) | 0.896 | ||
| Induction-active labor interval | 0.849 (0.769–0.937) | 0.001* | 0.857 (0.775–0.947) | 0.002** |
P<0.05 by univariate analysis;
P<0.05 by multivariate analysis.
Multiple logistic regression analysis also showed that only the gravidity and induction-active labor interval, and not the Bishop score or any of its individual parameters, were independent predictors of successful labor induction (Table 3).
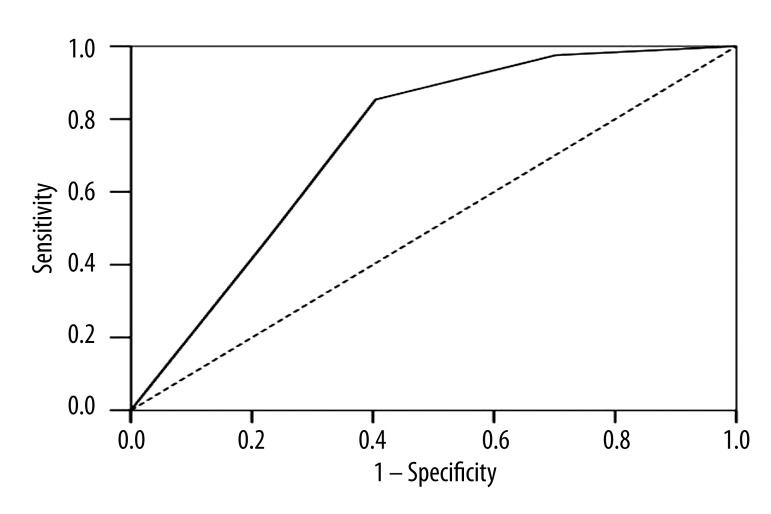
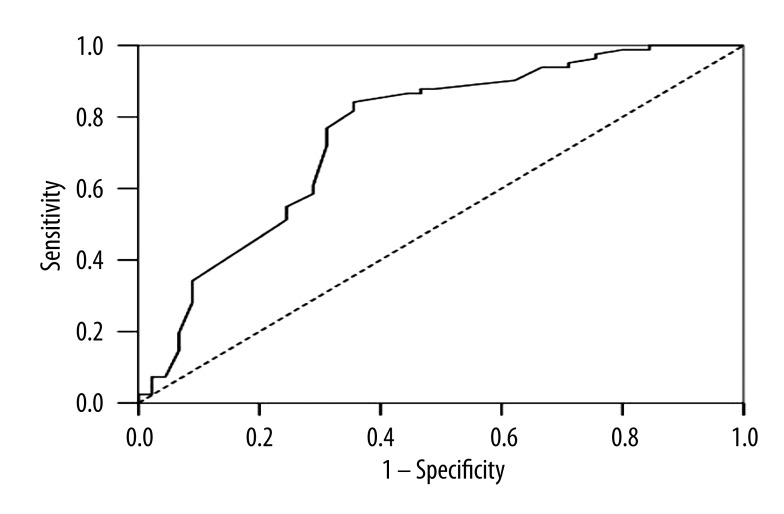
ROC analysis
In ROC curves, the best cut-off point for the prediction of successful induction of labor was 3 for gravidity, and 7.96 for induction-active labor interval. The area under the curves (AUC) of the ROC for gravidity (AUC=0.738; P<0.001) and for induction-active labor interval (AUC=0.753; P<0.001) were greater than that for the Bishop score (AUC=0.520; P=0.706) in predicting a successful labor induction (Figures 1, 2).
Figure 1.
Receiver operating characteristic (ROC) curve for gravidity (area under the curve [AUC]=0.738, 95%CI 0.64–0.83; P=0.000).
Figure 2.
Receiver operating characteristic (ROC) curve for induction-active labor interval (area under the curve [AUC]=0.753, 95%CI 0.66–0.85; P=0.000).
Discussion
The condition of the cervix at the start of induction is an important predictor, with the modified Bishop score being a widely used scoring system. However, the present study indicates that the Bishop score appeared to have poor predictive value for the success of labor induction. These observations are consistent with the study of fetal fibronectin by Blanch et al. [16], who demonstrated that only in the nulliparous women could the fetal fibronectin test be correlated with the length of the latent phase, as well as with the induction to delivery interval. Our findings are also in accordance with the results of a report by Roman et al. [17], who showed that cervical status prior to induction of labor was associated with the length of the latent phase of labor, but not that of the active phase, and that the performance of cesarean delivery for dystocia was specifically indicated only in women in the active phase of labor.
In a prospective study by Reis et al. [18], obstetric history (previous vaginal delivery), but not cervical length measurement, accurately predicted successful labor induction. Likewise, Gonen et al. [19] prospectively evaluated 86 women and found that parity was an independent predictor of vaginal delivery in induced labor. Wing et al. [20] also reported that the clinical characteristic of parity predicted the likelihood of success of cervical ripening and labor induction with intravaginal misoprostol administration. Park [21] reported that in terms of previous obstetric history, women with only previous midtrimester loss or preterm delivery had a significantly higher risk of failed labor induction than those with at least 1 previous term delivery. In the present study, gravidity, but not parity, was associated with successful labor induction. Because of family planning, most pregnant Chinese women are nulliparous; however, some women have a history of 1 or more abortions, so the details of previous pregnancies were recorded. Our results show that gravidity correlated significantly with successful induction – the higher the gravidity of a women, the higher the hazard of failed induction. This observation implies that the response to labor induction in parous women depends mainly on the period of gestation at which they experienced cervical ripening and dilatation phases in previous pregnancies, but the response to induction of labor in nulliparous women may be influenced by abortion history in those who have not experienced cervical ripening, as cervical injury may have occurred. The result also suggests that the sensitivity of response to prostaglandin was not increased in women with a history of abortion. Further studies are required to determine whether women with higher previous gravidity have a significantly higher risk of failed labor induction. The present study also showed that the mean induction-active labor interval in the successful labor induction group was shorter than in the failed labor induction group. This finding, which has not previously been reported, suggests that the performance of a woman in the initial phase of induction may be indicative of her eventual response to the induction of labor.
Conclusions
Several investigators have reported that birth weight is an independent factor for the risk of primary cesarean delivery. Pevzner et al. [22] reported that birth weight below 4000 g was a significant factor in the prediction of successful induction of labor. Crane et al. [23] reported that birth weight was associated with vaginal delivery within 24 h of induction, which is in agreement with our findings. Since this information is not known before delivery, from a practical point of view, accurate methods for the prenatal estimation of actual birth weight would be useful in predicting which women will have a successful induction of labor.
Footnotes
Source of support: Departmental sources
References
- 1.Lilford RJ, van Coeverden de Groot HA, et al. The relative risks of caesarean section (intrapartum and elective) and vaginal delivery: a detailed analysis to exclude the effects of medical disorders and other acute pre-existing physiological disturbances. Br J Obstet Gynaecol. 1990;97(10):883–92. doi: 10.1111/j.1471-0528.1990.tb02442.x. [DOI] [PubMed] [Google Scholar]
- 2.Ryding EL, Wijma K, Wijma B. Experiences of emergency cesarean section: A phenomenological study of 53 women. Birth. 1998;25(4):246–51. doi: 10.1046/j.1523-536x.1998.00246.x. [DOI] [PubMed] [Google Scholar]
- 3.Creedy DK, Shochet IM, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth. 2000;27(2):104–11. doi: 10.1046/j.1523-536x.2000.00104.x. [DOI] [PubMed] [Google Scholar]
- 4.van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intraoperative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997;74(1):1–6. doi: 10.1016/s0301-2115(97)02725-5. [DOI] [PubMed] [Google Scholar]
- 5.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2002. Natl Vital Stat Rep. 2003;52(10):1–113. [PubMed] [Google Scholar]
- 6.Zhang J, Yancey MK, Henderson CE. US. National trends in labor induction, 1989–1998. J Reprod Med. 2002;47(2):120–24. [PubMed] [Google Scholar]
- 7.Chandra S, Crane JM, Hutchens D, Young DC. Transvaginal ultrasound and digital examination in predicting successful labor induction. Obstet Gynecol. 2001;98(1):2–6. doi: 10.1016/s0029-7844(01)01386-2. [DOI] [PubMed] [Google Scholar]
- 8.Rozenberg P, Goffinet F, Hessabi M. Comparison of the Bishop score, sonographic measurement of cervical length and fibronectin assay in predicting time to delivery and type of delivery at term. Am J Obstet Gynecol. 1999;183(3):589–99. [Google Scholar]
- 9.Robinson CJ, Hill EG, Alanis MC, et al. Examining the effect of maternal obesity on outcome of labor induction in patients with preeclampsia. Hypertens Pregnancy. 2010;29(4):446–46. doi: 10.3109/10641950903452386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daskalakis G, Thomakos N, Hatziioannou L, et al. Sonographic cervical length measurement before labor induction in term nulliparous women. Fetal Diagn Ther. 2006;21(1):34–38. doi: 10.1159/000089045. [DOI] [PubMed] [Google Scholar]
- 11.Austin S, Sanchez-Ramos L, Adair CD. Labor induction with intravaginal misoprostol compared with the dinoprostone vaginal insert: a systematic review and metaanalysis. Am J Obstet Gynecol. 2010;202(6):624.e1–9. doi: 10.1016/j.ajog.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Rath W. A clinical evaluation of controlled-release dinoprostone for cervical ripening – a review of current evidence in hospital and outpatient settings. J Perinat Med. 2005;33(6):491–99. doi: 10.1515/JPM.2005.087. [DOI] [PubMed] [Google Scholar]
- 13.Gai MY, Zhang JP, Li Y, et al. Clinical evaluation of propess for induction of term pregnancy. Zhonghua Fu Chan Ke Za Zhi. 2003;38(4):210–12. [PubMed] [Google Scholar]
- 14.Zou LY, Fan L, Duan T, et al. Clinical study on dinoprostone suppositories 0.8 mm used in cervical ripening and labor induction of women with term pregnancy of premature rupture of the membranes: a multicenter study. Zhonghua Fu Chan Ke Za Zhi. 2010;45(7):492–96. [PubMed] [Google Scholar]
- 15.Chang CH, Chang FM. Randomized comparison of misoprostol and dinoprostone for preinduction cervical ripening and labor induction. J Formos Med Assoc. 1997;96(5):366–69. [PubMed] [Google Scholar]
- 16.Blanch G, Olah KS, Walkinshaw S. The presence of fetal fibronectin in the cervicovaginal secretions of women at term-its role in the assessment of women before labor induction and in the investigation of the physiologic mechanisms of labor. Am J Obstet Gynecol. 1996;174(1 Pt 1):262–66. doi: 10.1016/s0002-9378(96)70405-2. [DOI] [PubMed] [Google Scholar]
- 17.Roman H, Verspyck E, Vercoustre L, et al. The role of ultrasound and fetal fibronectin in predicting the length of induced labor when the cervix is unfavorable. Ultrasound Obstet Gynecol. 2004;23(6):567–73. doi: 10.1002/uog.1076. [DOI] [PubMed] [Google Scholar]
- 18.Reis FM, Gervasi MT, Florio P, et al. Prediction of successful induction of labor at term: role of clinical history, digital examination, ultrasound assessment of the cervix, and fetal fibronectin assay. Am J Obstet Gynecol. 2003;189(5):1361–67. doi: 10.1067/s0002-9378(03)00725-7. [DOI] [PubMed] [Google Scholar]
- 19.Gonen R, Degani S, Ron A. Prediction of successful induction of labor: comparison of transvaginal ultrasonography and the Bishop score. Eur J Ultrasound. 1998;7(3):183–87. doi: 10.1016/s0929-8266(98)00042-1. [DOI] [PubMed] [Google Scholar]
- 20.Wing DA, Tran S, Paul RH. Factors affecting the likelihood of successful induction after intravaginal misoprostol application for cervical ripening and labor induction. Am J Obstet Gynecol. 2002;186(6):1237–40. doi: 10.1067/mob.2002.123740. [DOI] [PubMed] [Google Scholar]
- 21.Park KH. Transvaginal ultrasonographic cervical measurement in predicting failed labor induction and cesarean delivery for failure to progress in nulliparous women. Korean Med Sci. 2007;22(4):722–27. doi: 10.3346/jkms.2007.22.4.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pevzner L, Rayburn WF, Rumney P, Wing DA. Factors predicting successful labor induction with dinoprostone and misoprostol vaginal inserts. Obstet Gynecol. 2009;114(2 Pt 1):261–67. doi: 10.1097/AOG.0b013e3181ad9377. [DOI] [PubMed] [Google Scholar]