Summary
Background
Primary epiploic appendagitis (PEA) is a rare cause of abdominal acute or subacute complaints. Diagnosis of PEA is made with ultrasonography (US) or when computed tomography (CT) reveals a characteristic lesion.
Case Report
We report on two patients with PEA. In one patient PEA was first seen with US and confirmed with contrast enhanced CT, and in the second patient CT without contrast enhancement demonstrated PEA. In both patients an outpatient recovery with conservative non-surgical treatment is described.
Conclusions
Medical personnel should be aware of this rare disease, which mimics many other intra-abdominal acute and subacute conditions. A correct diagnosis of PEA with imaging procedures enables conservative and successful outpatient management avoiding unnecessary surgical intervention and additional costs.
Keywords: epiploic appendagitis, abdominal pain, ultrasonography, computed tomography
Background
Primary epiploic appendagitis is a very rare condition that results from inflammation of an epiploic appendage in an otherwise healthy patient. Owing to a lack of pathognomonic clinical features and awareness of the disease, primary epiploic appendagitis (PEA) is rarely diagnosed as the cause of acute and subacute abdominal complaints. Recognition of PEA has increased over the past 10 years owing to the increasing use of abdominal ultrasonography and the introduction of cross-sectional imaging CT scans for the primary evaluation of abdominal pain [1,2].
Case Reports
A 52-year-old male Caucasian patient presented with a dull constant, localized and non-migratory abdominal pain. Physical examination revealed localized tenderness in the left lower abdominal quadrant and his symptoms besides the pain only included epigastric discomfort. At admission an abdominal ultrasound examination demonstrated a non-compressible hyperechogenic paracolic oval shaped mass in the area of pain (Figure 1).
Figure 1.
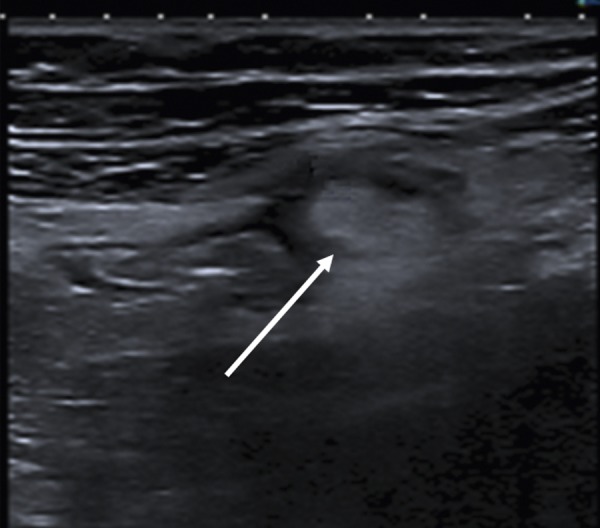
Ultrasonography image of epipolic appendagitis showed an hyperechogenic paracolic oval-shaped mass in the left lower abdominal quadrant.
Additionally an abdominal computed tomography (CT) with intravenous contrast medium was performed and demonstrated an oval lesion, maximum diameter 2.4 cm, with fat attenuation, located adjacent to the descending colon. The inflamed and thickened visceral peritoneum surrounding the fat-containing appendage was demonstrated as hyperattenuating ring and the diagnosis of PEA was completed (Figures 2 and 3). Laboratory parameters were not determined in this patient. As outpatient a therapy with non-steroidal anti-inflammatory drugs (ibuprofen 600 mg twice daily) was initiated. Within 7 days the patient’s complaints resolved and further recovery was uneventful.
Figures 2 and 3.

Longitudinal and transverse abdominal CT with contrast enhancement demonstrated the inflamed lesion (arrow) adjacent to the descending colon and showed an oval area of fat attenuation with a diameter of 2.4 cm surrounded by a hyperattenuating ring.
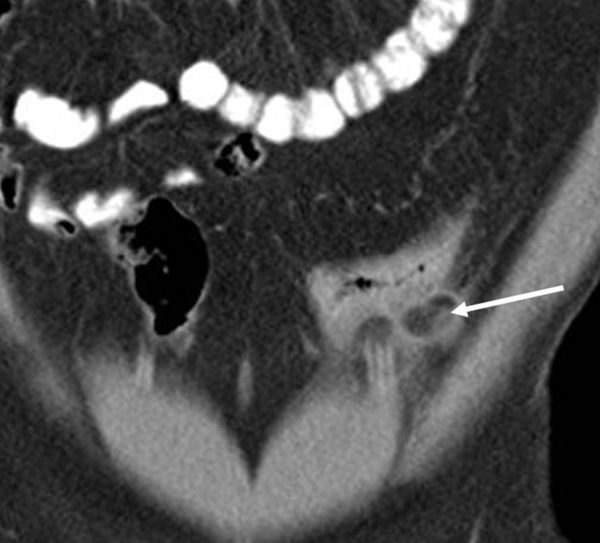
In the second patient, a 62-year-old male Caucasian, who was evaluated because of inguinal hernia, physical evaluation demonstrated tenderness in the left sided lower abdominal quadrant. Because the patient refused application of intravenous contrast medium the abdominal computed tomography (CT) without intravenous contrast medium demonstrated an oval lesion, maximum diameter 2.6 cm, located adjacent to the descending colon. The inflamed and thickened visceral peritoneum surrounding the fat-containing appendage was demonstrated with an edematous ring and the diagnosis of PEA was completed (Figures 4 and 5). Laboratory parameter were leukocytes 10.6×109/L (normal 4–9), C-reactive peptide 1.0 mg/dl (normal <0.5), fibrinogen 509 mg/dl (normal 210–400), all the routine laboratory parameters, including erythrocyte sedimentation rate, liver- and pancreas enzymes, were within normal limits. At an external institution outpatient therapy with antibiotic drugs (ciprofloxacin 250 mg and metronidazol 500 mg, each twice daily) was initiated. Within 3 days the patient’s complaints resolved and further recovery was uneventful.
Figures 4 and 5.


Longitudinal and transverse abdominal CT without contrast enhancement demonstrated the inflamed lesion (arrow) adjacent to the descending colon and showed an oval area with a diameter of 2.6 cm surrounded by an edematous ring.
Discussion
Appendices epiploicae are pouches of subserosal fat lining the entire length of the colon. They appear in two parallel rows next to the anterior and the posterior taenia coli, and are attached to the colonic wall by a vascular stalk. Approximately 100 appendices epiploicae per colon exist and they are clustering mainly in the cecal and sigmoid region. Therefore, pain is usually located in the left, sometimes in the right lower abdominal quadrant [2,3]. Although, this pain can be located in all abdominal regions and may be in the location of an acute or subacute abdominal condition such as diverticulitis, cholecystitis and appendicitis [4,5]. It was suggested that many patients treated for mild diverticulitis may have PEA and it was reported that up to 7% of all patients clinically suspected of having diverticulitis may have epiploic appendagitis [6,7].
Due to the lack of pathognomonic clinical features the diagnosis of epiploic appendagitis is difficult and rare. Symptoms include acute and recurrent non-migratory abdominal pain, local tenderness, postprandial fullness, early satiety, epigastric discomfort, vomiting, bloating, diarrhea, intermittent febrile temperature, and moderate weight loss. The pain is usually described as dull, constant, non-migrating, and physical examination reveals a well-localized tenderness. Abnormal laboratory parameters may include slightly elevated C-reactive peptide and neutrophile leukocytes, all the other routine laboratory parameters are within normal limits [1]. During the last few years with the introduction of cross-sectional imaging and the increasing use of abdominal CT scans for primary evaluation of abdominal pain, the recognition of PEA is increasing. In the past, diagnosis in many patients was attained during surgery [8,9], but imaging procedures are now increasingly used for this purpose. Normal epiploic appendages cannot be seen on CT scans. PEA is thought to be an inflammatory condition and to arise primarily from a torsion causing ischemia and infarction with aseptic fat necrosis, spontaneous venous thrombosis, and is a localized sterile inflammation in and surrounding one epiploic appendage [11]. CT is the diagnostic modality of choice for patients with suspected PEA because PEA has a characteristic appearance on CT [12–14].
Abdominal ultrasound in experienced hands has revealed PEA in an increasing number of patients. PEA on ultrasonography is shown as a non-compressible hyperechogenic paracolic oval-shaped mass (Figure 1) [15–17].
Conclusions
However, appropriate diagnosis with CT allows a successful outpatient treatment avoiding surgery and unnecessary additional costs. Usually patients recover with conservative non-surgical treatment, with anti-inflammatory drugs or without medication. Careful physical examination and awareness of the characteristic imaging findings of PEA support the suggestion that surgical intervention is only recommended if conservative medical treatment fails to improve a patient’s symptoms and clinical signs of PEA.
Footnotes
Competing interests
The authors declare no competing interests.
Source of support: Departmental sources
References
- 1.Schnedl WJ, Krause R, Tafeit E, et al. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol. 2011;8:45–49. doi: 10.1038/nrgastro.2010.189. [DOI] [PubMed] [Google Scholar]
- 2.Almeida AT, Melao L, Viamonte B, et al. Epiploic appendagitis: an entity frequently unknown to clinicians - diagnostic imaging, pitfalls, and look-alikes. Am J Roentgenol. 2009;193:1243–51. doi: 10.2214/AJR.08.2071. [DOI] [PubMed] [Google Scholar]
- 3.Jalaguier A, Zins M, Rodallec M, et al. Accuracy of multidetector computed tomography in differentiating primary epiploic appendagitis from left acute colonic diverticulitis associated with secondary epiploic appendagitis. Emerg Radiol. 2010;17:51–56. doi: 10.1007/s10140-009-0822-x. [DOI] [PubMed] [Google Scholar]
- 4.Sangha S, Soto JA, Becker JM, Farraye FA. Primary epiploic appendagitis: an underappreciated diagnosis. A case series and review of the literature. Dig Dis Sci. 2004;49:347–50. doi: 10.1023/b:ddas.0000017463.46961.94. [DOI] [PubMed] [Google Scholar]
- 5.Jain TP, Shah T, Juneia S, Tambi RL. Case of the season: primary epiploic appendagitis: radiological diagnosis can avoid surgery. Semin Roentgenol. 2008;43:4–6. doi: 10.1053/j.ro.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Rioux M, Langis P. Primary epiploic appendagitis: Clinical, US, and CT findings in 14 cases. Radiology. 1994;191:523–26. doi: 10.1148/radiology.191.2.8153333. [DOI] [PubMed] [Google Scholar]
- 7.Breda Vriesman AC, Lohle PNM, et al. Infarction of omentum and epiploic appendage: diagnosis, epidemiology and natural history. Eur Radiol. 1999;9:1886–92. doi: 10.1007/s003300050942. [DOI] [PubMed] [Google Scholar]
- 8.Sand M, Gelos M, Bechara FG, et al. Epiploic appendagitis – clinical characteristics of an uncommon surgical diagnosis. BMC Surgery. 2007;7:11. doi: 10.1186/1471-2482-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silva PD, Ripple J. Laparoscopic diagnosis and treatment of an infarcted epiploic appendage. J Am Assoc Gynecol Laparosc. 1996;3:325–27. doi: 10.1016/s1074-3804(96)80024-7. [DOI] [PubMed] [Google Scholar]
- 10.Uehara R, Isomoto H, Yamaguchi N, et al. Epiploic appendagitis in a 27-year-old man. Med Sci Monit. 2011;17:CS113–15. doi: 10.12659/MSM.881968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain TP, Shah T, Juneia S, Tambi RL. Case of the season: primary epiploic appendagitis: radiological diagnosis can avoid surgery. Semin Roentgenol. 2008;43:4–6. doi: 10.1053/j.ro.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Ozkurt H, Karatag O, Karaarslan E, et al. Brief clinical review: CT findings in epiploic appendagitis. Surgery. 2007;141:530–32. doi: 10.1016/j.surg.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Sandrasegaran K, Maglinte DD, Rajesh A, Akisik FM. Primary epiploic appendagitis: CT diagnosis. Emerg Radiol. 2004;11:9–14. doi: 10.1007/s10140-004-0369-9. [DOI] [PubMed] [Google Scholar]
- 14.Singh AK, Gervais DA, Hahn PF, et al. CT appearance of acute epiploic appendagitis. Am J Roentgenol. 2004;183:1303–7. doi: 10.2214/ajr.183.5.1831303. [DOI] [PubMed] [Google Scholar]
- 15.Matsunaga H, Fuji Y, Taniguchi N. Ultrasonographic findings in epiploic appendagitis. J Med Ultrasonics. 2010;37:31–32. doi: 10.1007/s10396-009-0237-z. [DOI] [PubMed] [Google Scholar]
- 16.Görg C, Egbring J, Bert T. Contrast-enhanced ultrasound of epiploic appendagitis. Ultraschall in Med. 2009;30:163–67. doi: 10.1055/s-2008-1027891. [DOI] [PubMed] [Google Scholar]
- 17.Danse EM, Van Beers BE, Baudrez V, et al. Epiploic appendagitis: color Doppler sonographic findings. Eur Radiol. 2001;11:183–86. doi: 10.1007/s003300000672. [DOI] [PubMed] [Google Scholar]


