Summary
Background
Bony wall damages in the region of the middle and posterior cranial fossa are usually observed in cases of chronic otitis media. These defects can also be congenital, post-traumatic, iatrogenic or due to tumors. They can potentially lead to the development of intracranial complications.
Material/Methods
We analyzed patients who were diagnosed as having bony wall damage in the region of the middle and/or posterior cranial fossa. We also discuss methods of reconstruction during otosurgery.
The analysis involves patients who underwent middle ear operations in the Department of Otolaryngology at the Jagiellonian University of Krakow between 2004 and 2008; 495 otosurgeries were performed during this period of time.
Results
In 70% of patients the reason for otosurgery was chronic otitis media. In 20%, bone defects occurred simultaneously with otosclerosis. Less than 10% underwent otosurgery for other reasons. Bony wall damage in the region of the middle and posterior cranial fossa were diagnosed in 46 patients who underwent surgery. In patients with bony wall damage, otogenic intracranial complications were described in 14 cases.
Conclusions
The performed reconstruction methods for bony wall damage, which used the fascia, strengthened with the pedicle muscle flap for larger defects and with either bone lamella or cartilage in specific cases, proved successful.
Nearly 80% of bony wall damages in the region of the middle and posterior cranial fossa remain asymptomatic and are discovered incidentally during middle ear surgery. The above observations emphasize the significant role of pre-operative imaging diagnostics.
Keywords: chronic otitis media, skull bone defects, otosurgery
Background
Chronic otitis media is characterized by conductive hearing loss, tympanic membrane perforation and persistent or recurrent discharge from the ear. The least advanced changes in the middle ear are observed in the cases of simple chronic otitis media. Other types of chronic infection in the middle ear, and in particular those accompanied by the presence of inflammatory granulation or cholesteatomatous pathology, are characterized by bone erosion observed in the middle ear, which, apart from hearing impairment due to ossicular chain destruction, may lead to otogenic complications [1,2].
Bony wall damage in the region of the middle and/or posterior cranial fossa can cause otogenic intracranial complications such as:
epidural empyema,
subdural empyema,
sigmoid sinus thrombophlebitis,
otogenic meningitis,
cerebellar abscess, brain abscess,
hydrocephalus,
meningoencephalocele.
Defects of the bony wall of the facial nerve and semicircular canal fistula are also damages caused by chronic otitis media and lead to otogenic intratemporal complications such as:
otogenic fascial nerve paresis,
labyrinthitis.
Cases of skull bone defects resulting from congenital, post-traumatic or iatrogenic conditions or from the neoplasmatic process are less frequent. Regardless of their etiology, they always can potentially cause complications [3,4].
Although instances of otogenic intracranial complications are rare in epidemiological terms, an overview of this group of patients is reasonable considering the risk to the lives of such patients and to their organ function.
Aim
The aim of this work is to analyze patients with bony wall damage in the region of the middle and posterior cranial fossa which were found in the course of otosurgery. We discuss the observed intracranial complications and diseases these conditions caused. The skull bone reconstruction methods that were applied in these patients are described as well.
Material and Methods
Between 2004 and 2008, otosurgeries were performed on 495 patients. Over 70% of patients underwent operations due to chronic inflammatory condition; 20% underwent surgery due to otosclerosis; and less than 10% underwent otosurgery for other reasons such as tumors, post-traumatic changes, etc. The study group included 264 women and 231 men; the oldest patient was 76 years of age, and the youngest patient was 7 years of age. The average patient age was 36 years.
As a member of the International Otology Audit Group, the Otolaryngology Research Hospital has been analyzing in detail all ear operations performed since 2004. This study involved the prospective analysis of patients who were diagnosed during surgery as having bony wall damage in the region of the middle and/or posterior cranial fossa. Statistical tests were performed.
In patients presented symptoms pointing to intracranial complications due to the pathologic process in the middle ear, otosurgery was the planned procedure intended to eliminate the source of infection and reconstruct bony walls within the area of the middle ear.
Results
The bony wall damage in the region of the middle and/or posterior cranial fossa was diagnosed during surgery in 46 patients (ie, approximately 10% of all ear surgeries). This group included 20 women and 26 men, between 7 and 68 years of age. The average patient age was 33.4 years.
The recommendation for surgical treatment in 89% of cases with bony wall damage was due to chronic otitis media (COM) and in 9% of cases was due to tumors (3 patients treated due to squamous cell cancer of the middle ear and 1 case of paraganglioma). In another patient, bone erosion occurred along with immobilization of the stapes due to the development of otosclerosis.
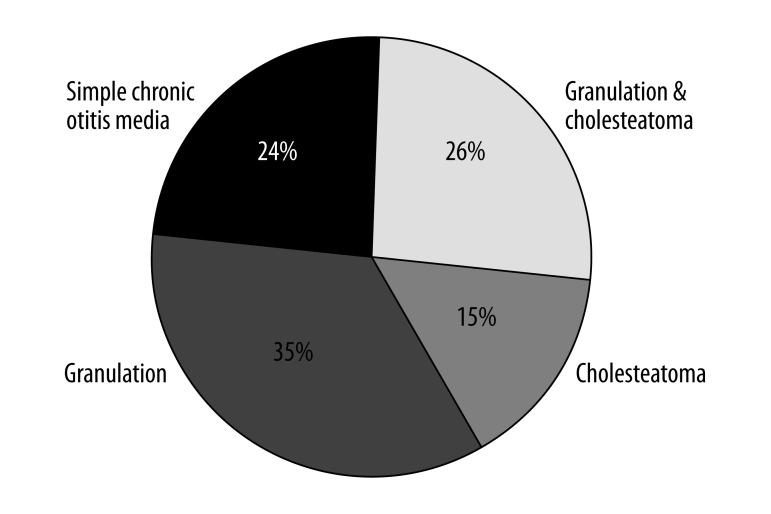
The most frequent condition observed in the middle ear was granulation tissue, less frequently coexistent with cholesteatoma. Isolated cholesteatoma was a relatively rare case, diagnosed in only 7 patients. Considering the location of cholesteatoma in general, it should be emphasized that in the majority of cases the process was highly developed and it covered the tympanic cavity and the air cells of the mastoid process (70% of the patients with cholesteatoma). In the group diagnosed with middle ear infection, 25% of patients with bony wall damage exhibited a simple chronic otitis media (Figure 1).
Figure 1.
Middle ear pathology in patients with COM who developed bony wall damages in the region of the middle and/or posterior cranial fossa.
Bony wall damages in the region of the middle and posterior cranial fossa were usually diagnosed incidentally during surgeries performed for the treatment of abnormalities that commonly resulted from chronic inflammatory conditions. In the remaining patients, middle ear surgery was the planned procedure intended to eliminate the source of infection and reconstruct previously diagnosed bony wall damages within the area of the middle ear.
The most frequently diagnosed damage was in the region of the base of the middle cranial fossa (approximately 80% of cases). A comparable frequency of approximately 10% was observed with regard to damage of the posterior cranial fossa and both the posterior and middle cranial fossa. Diagnosed bony wall damage in the region of middle and posterior cranial fossa was usually small, less than 1 cm in diameter. They were successfully closed with fascia or fascia with the additional strength of the pedicle muscle flap.
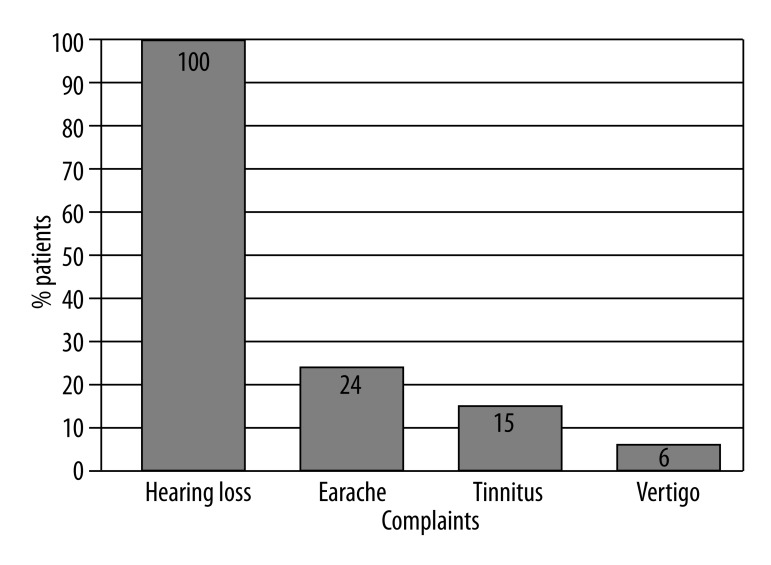
In patients with bony wall damage in the region of the middle and posterior cranial fossa the most frequently reported condition was hearing impairment; 11 patients complained of earache, including all patients with a tumor in the area of the middle ear. Tinnitus, either isolated or present with other ailments, was observed in 7 patients. Three patients suffered from dizziness and 29 patients reported different levels of hearing impairment without other symptoms (Figure 2).
Figure 2.
Complaints before otosurgery in patients with bony wall damages in the region of the middle and/or posterior cranial fossa.
Discharge of cerebrospinal fluid was present in the preoperative history of 4 patients.
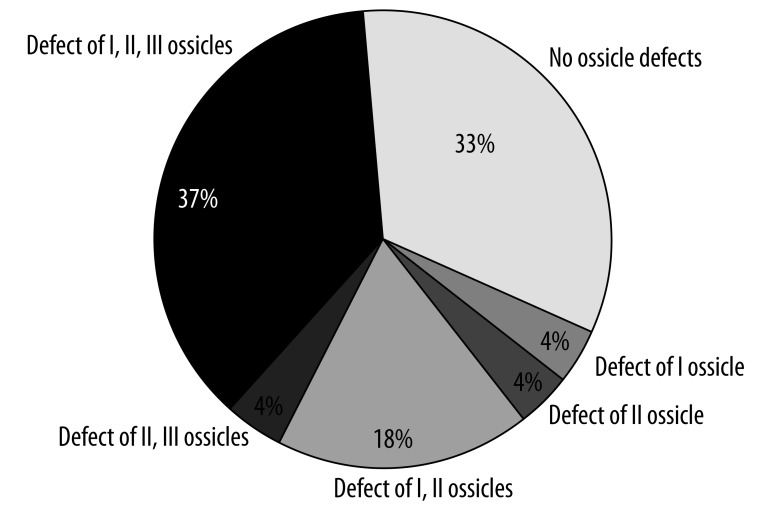
Damage to the ossicular chain was observed in 67% of the patients operated on. In the majority of cases the damage covered all ear ossicles (37% of the patients). Simultaneous damage to the first and the second ossicle was observed relatively often (in 8 patients). The cases of other combinations of damage to the ossicular chain were singular. However, it must be pointed out that isolated damage to the stapes was not observed nor was simultaneous damage to the first and the third ossicle (Figure 3).
Figure 3.
Defects of the ossicular chain in patients with bony wall damages in the region of the middle and posterior cranial fossa.
In the preoperative history, otorrhea was present in 37 patients, which is more than 80% of all the patients who underwent otosurgery.
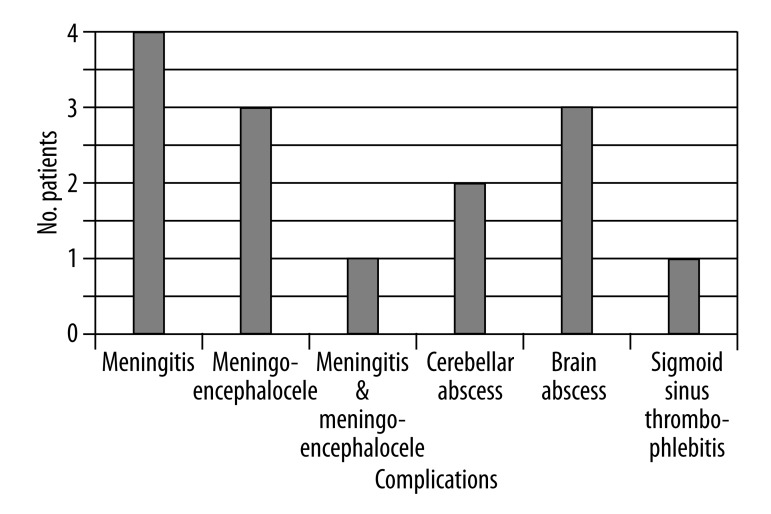
Otogenic intracranial complications were diagnosed in 30% of all patients (ie, 14 patients subject to surgery) with skull bone damage. In the majority of patients, skull bone losses were found incidentally, yet 4 patients had been treated for meningitis before the surgery. In 2 cases, meningoencephalocele was diagnosed during surgery. In 1 case, meningoencephalocele occurred along with recurrent meningitis. The meningoencephalocele in each case was described in the middle fossa, and never in the posterior fossa. Two patients were diagnosed for cerebellar abscess. Despite the otosurgery and the follow-up neurosurgical treatment, 1 of these patients died. Three cases of brain abscess were observed, with the location within the temporal lobe, typical for otogenic complications. One patient also suffered from sigmoid sinus thrombophlebitis (Figure 4).
Figure 4.
Observed intracranial complications.
All mentioned otogenic intracranial complications developed in the course of chronic otitis media. They were usually diagnosed in patients with COM with inflammatory granulation or cholesteatoma (10 out of the 14 patients with otogenic intracranial complications).
Simple chronic otitis media was coexistent with intracranial complication in 4 cases – 2 meningitis, 1 meningocele and 1 meningocele complicated by meningitis.
Authors searched for the link between a location of bony wall damages in the region of the middle and posterior cranial fossa and types of intracranial complications in the group of 42 patients with chronic otitis media. The multifield contingency tables for the patients with bony defects to the cranial fossa was taken into consideration, and the chi-squared ratio was established. Power of relationship was measured as a Cramer ratio. The Cramer ratio for this relationship is 0.82. This test was confirmed with the chi-squared NW ratio. The results were given as statistically significant for p (α)<0.05. Significant statistical correlation (chi-squared 32.6) was found between the bony wall damage located in the region of middle cranial fossa and the meningocele in this region. The most common significant statistical intracranial complication for the patients with bony wall damage in the region of the middle cranial fossa is meningocele. In the patients with bony wall damage in the posterior cranial fossa, the most common significant statistical intracranial complication is cerebellar abscess.
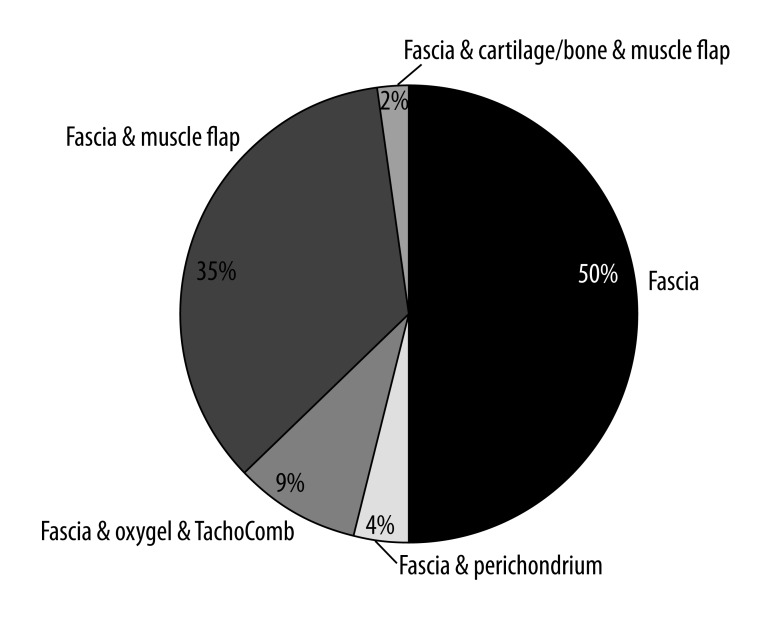
The method of reconstructing skull bone losses depended on their severity. The most popular material used to reconstruct the bony wall of the skull base was the fascia of the temporal muscle. In the cases of minor losses, the surgical treatment consisted in covering the exposed dura mater with a fragment of the fascia. The fascia was often strengthened additionally with Oxycel and TachoComb. Considerable losses were sealed by supporting the earlier described layer with a piece of cartilage. Larger losses were covered using an additional pedicle muscle flap to support the structure and to obliterate the surgical cavity in the temporal bone. The largest losses, more than 1 cm in diameter, were sealed using 3 layers; the third layer, located between the fascia and the pedicle muscle flap described above, was a fragment of bone taken from either the anterior or the lateral wall of the maxillary sinus accessed through the sublabial approach (Figure 5).
Figure 5.
Performed skull base reconstruction.
In the majority of cases, the treatment described above proved successful. Postoperative recurrence of discharge of cerebrospinal fluid was observed in 1 patient due to very extensive loss in the middle and posterior cranial fossa and the synostosis at the passage between the sigmoid sinus and the transverse sinus. In that case the skull bone loss was treated additionally in the course of craniotomy; the procedure proved successful.
Seven patients were diagnosed as having loss of the facial canal. Half of the patients with the exposed nerve VII also presented a fistula on the lateral semicircular canal. Fistula on the lateral semicircular canal was diagnosed in 5 patients.
Discussion
Direct contact between cerebral tissue and the regions of the middle ear infected by the inflammatory process creates favorable conditions for the development of intracranial complications. Bony wall damages in the region of middle and posterior cranial fossa are one of many factors contributing to development of otogenic complications (Figure 6). Other mechanisms contributing to otogenic complications, such as inflammatory changes to the bone tissue and thrombophlebitis, also exist [5–7].
Figure 6.
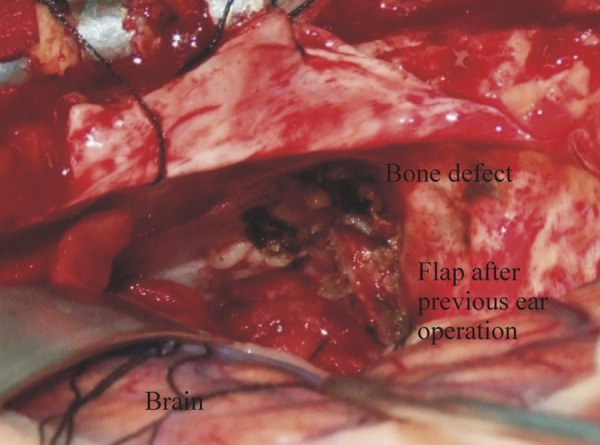
Intracranial approach: Defect of middle and posterior cranial fossa.
In 80% of cases, the damage was found in the region of the middle cranial fossa. Isolated damage of the posterior cranial fossa was described in only 10% of patients in the studied group. During the studied time period, damage to the bony wall of the middle and posterior cranial fossa were observed in 10% of patients. This result confirms our earlier observations [8,9]. Intracranial complications were present in about 30% of patients with an exposed pachymeninx. Meningitis was diagnosed in the majority of cases, and meningocele was observed less frequently. Other types of complications were diagnosed in singular cases.
Almost 80% of skull bone defects remained asymptomatic, and they were diagnosed incidentally during otosurgery performed for the treatment of chronic inflammatory changes or during surgery of the stapes in patients with otosclerosis.
The recommendation for surgical treatment was based on chronic inflammatory conditions in more than 90% of cases (the damage was also observed in 3 patients with tumor and 1 patient who underwent surgery due to otosclerosis). In patients with bony wall damages in the region of the middle and posterior cranial fossa, the defects co-occurred more frequently with abnormal granulation tissue in the middle ear, including cancerous granulation tissue. Chronic cholesteatoma otitis media had a smaller effect on the exposure of the dura mater of the skull bone. In the studied group, isolated cholesteatoma changes were observed in 15% of patients; co-occurrences of cholesteatoma with granulation tissue were observed more frequently. The cholesteatoma most often affected all areas within the middle ear. This prevalence was reflected in the degree of damage to the ossicular chain, given that damage to all of the ossicles was observed most frequently, but simultaneous damage to the malleus and the anvil was less frequent.
In 25% of cases bony wall damage was observed in patients with simple chronic otitis media.
Before surgery a considerable number of patients complained of temporary discharge from the ear and hearing impairment. The patients with granulation tissue complained more frequently of earaches.
The above observations emphasize the significant role of pre-operative imaging diagnostics, particularly computer-aided tomography and magnetic resonance, in diagnosing skull bone defects (Figure 7A, B). Diagnostics are especially important due to the lack of any symptoms that would suggest intracranial complications in the majority of patients [10,11].
Figure 7.
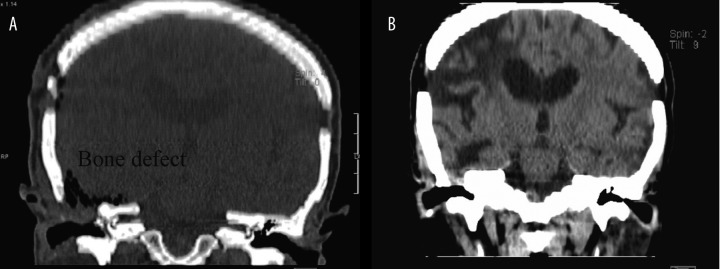
CT of the head – frontal plane: Bone defect – before (A) and after (B) surgery.
During surgical treatment of skull bone defects, reconstruction of the conducting system in the middle ear was performed in each case. None of the patients underwent radical surgery, which confirms that skull bone defects and otogenic complications can be treated with highly satisfactory results without such surgery. In cases of more substantial defects, an effective method of treating damage has involved the use of the fascia with the additional strength of the pedicle muscle flap. These described reconstruction methods correspond to worldwide reports in this field [12,13]. With large defects, reconstruction can also be carried out using the cartilage from the tragus or the bone lamella (eg, from the wall of the maxillary sinus) to strengthen the reconstruction between the fascia and the pedicle flap of the temporal muscle.
All patients with skull bone defects exhibited defects of the bony wall of the fascial nerve or the fistula in the lateral semicircular canal, with a frequency comparable to that of intracranial complications (approximately 12%). None of the patients was diagnosed with facial palsy, and the condition of the fistula in the lateral semicircular canal correlated with clinical symptoms such as vertigo. In addition, none of the patients in the analyzed group reported a history of pre-operative head damage.
In the described group of patients, all bony wall damage in the region of the middle and posterior cranial fossa were operated on using the otosurgical approach. However, it must be emphasized that in the case of a large defect, particularly one in which meningocele co-occurs, successful treatment of erosion may require a neurosurgical approach or both approaches at the same time (ie, through the ear as well as through the cranial fossa). This combination approach corresponds to the information provided in the published literature.
Conclusions
Bony wall damages of the middle or posterior cranial fossa usually remain asymptomatic. Most of them (80–90%) are diagnosed incidentally during otosurgery. This observation emphasizes the significance of pre-operative imaging diagnostics.
Skull bone defects in the region of the middle and posterior cranial fossa are 10 times more frequent within the middle cranial fossa than in the posterior or both middle and posterior cranial fossa.
Meningocele occurred in 10% of patients with the skull bone defect.
Meningocele was not observed in patients with defects in the region of the posterior cranial fossa.
The small number of defects to the posterior cranial fossa explains the rare occurrence of cerebellar abscess, which is a typical complication in acute inflammation or suppurated hematoma, and is more frequent in children.
Skull bone defects often coexisted with substantial damage to the ossicular chain.
The applied reconstruction methods result in successful reconstruction of the continuity of the walls of the middle ear during ossiculoplasties.
The probability of skull base defects is higher in patients with granulation tissue than in those with cholesteatoma.
Footnotes
Conflict of interest
None
Source of support: Departmental sources
Financial disclosure
This research was supported by statutory funds of the Department of Otolaryngology of the Jagiellonian University, Krakow, Poland. There are no financial interests the authors may have in companies or other entities that have an interest in the information in the Contribution (e.g., grants, advisory boards, employment, consultancies, contracts, honoraria, royalties, expert testimony, partnerships, or stock ownership in medically related fields). The authors have no financial interest.
References
- 1.Migirov L, Duvdevani S, Kronenberg J. Otogenic intracranial complications: a review of 28 cases. Acta Otolaryngol. 2005;125(8):819–22. doi: 10.1080/00016480510038590. [DOI] [PubMed] [Google Scholar]
- 2.Bento R, de Brito R, Ribas GC. Surgical management of intracranial complications of otogenic infection. Ear Nose Throat J. 2006;85(1):36–39. [PubMed] [Google Scholar]
- 3.Escada P, Vital JP, Capucho C, et al. Meningoencephalic herniation into the middle ear. Rev Laryngol Otol Rhinol. 1999;120(1):47–52. [PubMed] [Google Scholar]
- 4.Patel RB, Kwartler JA, Hodosh RM, et al. Spontaneous cerebrospinal fluid leakage and middle ear encephalocele in seven patietnts. Ear Nose Throat J. 2000;79(5):372–73. 376–78. [PubMed] [Google Scholar]
- 5.Gubbels SP, Selden NR, Delashaw JB, Jr, et al. Spontaneous middle fossa encephalocele and cerebrospinal fluid leakage: diagnosis and management. Otol Neurotol. 2007;28(8):1131–39. doi: 10.1097/MAO.0b013e318157f7b6. [DOI] [PubMed] [Google Scholar]
- 6.Nahas Z, Tatlipinar A, Limb CJ, et al. Spontaneous meningoencephalocele of the temporal bone: clinical spectrum and presentation. Arch Otolaryngol Head Neck Surg. 2008;134(5):509–18. doi: 10.1001/archotol.134.5.509. [DOI] [PubMed] [Google Scholar]
- 7.Manckoundia P, Mazen E, Saloff Coste A, et al. A case of meningitis due to Achromobacter xylosoxidans denitrificans 60 years after a cranial trauma. Med Sci Monit. 2011;17(6):CS63–65. doi: 10.12659/MSM.881796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiatr M, Skladzien J, Tomik J. Otogenic intracranial complications from data collected at Department of Otolaryngology Collegium Medicum Jagiellonian University between 1998–2006. Przegl Lek. 2006;63(11):1173–76. [PubMed] [Google Scholar]
- 9.Baran Z, Skladzien J, Tomik J, et al. Ubytki kostne środkowego i tylnego dołu czaszki stwierdzone u chorych operowanych z powodu przewlekłego zapalenia ucha środkowego. Otorynolaryngol – Przegl Klin. 2005;4(4):199–201. [in Polish] [Google Scholar]
- 10.Skarzynski H, Lorens A, Piotrowska A, et al. Hearing preservation in partial deafness treatment. Med Sci Monit. 2010;16(11):CR555–62. [PubMed] [Google Scholar]
- 11.Wiatr M, Skladzien J, Moskala M. Massive Posttraumatic Otorrhoea – Case Report. Int Adv Otol. 2009;5(1):122–25. [Google Scholar]
- 12.Penido Nde O, Borin A, Iha LC, et al. Intracranial complications of otitis media: 15 years of experience in 33 patients. Otolaryngol Head Neck Surg. 2005;132(1):37–42. doi: 10.1016/j.otohns.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Bento R, de Brito R, Ribas GC. Surgical management of intracranial complications of otogenic infection. Ear Nose Throat J. 2006;85(1):36–39. [PubMed] [Google Scholar]