Summary
Background
Frequent co-existence of bronchial asthma and depression or anxiety is an unquestioned phenomenon. In contrast, little is known about the relationship between the degree of asthma control and the prevalence of depression and anxiety. The aim of this study was to determine the potential relationship between the degree of asthma control and the prevalence of depression and anxiety.
Material/Methods
This study included a group of 128 randomly selected asthmatic individuals with various degree of asthma control. The study was based on a questionnaire survey, using the following tools: the Asthma Control Test, Beck Depression Inventory, and State-Trait Anxiety Inventory (STAI) – X-1 and X-2 questionnaires. All the questionnaires were completed during a single follow-up visit at the clinic.
Results
The occurrence of depression and its severity significantly correlated with the degree of asthma control. Individuals with depression were characterized by a significantly lower degree of asthma control compared to depression-free individuals (p<0.001). The degree of asthma control decreased significantly with increasing severity of depression (R=−0.367; p<0.001). No significant correlation was observed between the degree of asthma control and the levels of trait anxiety (R=−0.095; p=0.295) and state anxiety (R=−0.093; p=0.308).
Conclusions
The prevalence of depression and its severity significantly correlate with the degree of asthma control. Large, standardized multicenter studies of the relationship between the degree of asthma control and the prevalence of depression and other psychopathological symptoms are needed. Furthermore, it seems reasonable to introduce the screening of asthmatics for mental disorders.
Keywords: bronchial asthma, asthma test control, depression, anxiety
Background
Proper and complete evaluation of the patient is essential since it markedly influences the efficacy of treatment. Detecting comorbidity frequently affects the prognosis and therapeutic decisions. Although a thorough examination of the patient is always the duty of the physician, the potential presence of comorbidities requires a particularly active search for a given pathology. Conversely, investigating the potential relationships between various disorders is a task for scientists, and many previous and ongoing studies have dealt with this problem. The co-existence of mental and somatic disorders is a particularly interesting and infrequently diagnosed phenomenon. Previous studies have revealed that depression and anxiety disorders can co-exist with chronic heart failure and chronic obstructive pulmonary disease, among others, and that these comorbidities are associated with higher mortality, increased use of healthcare services, higher prevalence of disability, and a lower quality of life [1].
According to the Global Initiative for Asthma (GINA) international guidelines of 2006, satisfactory degree of asthma control is the principal goal of effective therapy [2]. Furthermore, the degree of control forms the basis for the clinical classification of asthma and determines the proper selection of treatment modality. High severity and poor control markedly diminish the quality of life for asthma patients. Subjectively evaluated quality of life in asthma patients, besides being affected by other factors, can be modulated by anxiety and depression.
Studies of co-existence of various psychopathological conditions in patients with bronchial asthma have been performed over many years [3–6]. The results of these studies have confirmed a higher prevalence of depression and anxiety in these patients. Katon et al observed that the prevalence of depression and anxiety disorders in adolescents with asthma is twice as high as in controls [7].
Depression and increased anxiety are commonly attributed to severe, life-threatening somatic disorders [8]. However, Centanni observed that depression and anxiety are more common in asthma patients than in individuals with other somatic disorders of similar severity [9].
The aforementioned relationships are still not fully understood. The relatively frequent co-existence of somatic and mental disorders suggests that they possibly share common components in their pathogenesis. Other possible explanations of these relationships were also proposed. Wamboldt’s results suggest potential involvement of genetic factors; the study analyzed the correlation between depression symptoms and atopy, and revealed that as many as 64% of cases where these 2 conditions co-existed were associated with familial predispositions [10].
Moreover, the results of some studies suggest that coping skills training can alleviate the severity of depressive symptoms observed in asthma patients [11].
Frequent co-existence of bronchial asthma and depression or high levels of anxiety is an unquestioned phenomenon. In contrast, little is known about the relationship between the degree of asthma control and the prevalence of depression and anxiety, the latter considered in the context of a transient state as well as a relatively stable personality trait. This prompted us to perform a detailed analysis of the problem.
The aim of this study was to determine the potential relationship between the degree of bronchial asthma control and the prevalence of such psychological disorders as depression and anxiety.
Material and Methods
Population
This study included a group of 128 randomly selected asthmatic individuals with various degree of asthma control. All participants were managed by: 1) the Department of Respiratory Medicine and Tuberculosis at the Ludwik Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Torun; 2) the Allergology Outpatient Clinic at the Voivodeship Tuberculosis and the Lung Diseases Outpatient Clinic with Specialist Clinics in Bydgoszcz; and 3) the Allergology Outpatient Clinic at the Nowy Szpital NZOZ in Œwiecie. The study was performed between October 2008 and May 2009. The protocol of the study was approved by the Local Bioethics Committee of the Ludwik Rydygier Collegium Medicum in Bydgoszcz. All participants gave their written informed consent to participate in the study.
The study was based on a questionnaire survey, using the following tools: the Asthma Control Test, Beck Depression Inventory, and State-Trait Anxiety Inventory (STAI) – X-1 and X-2 questionnaires. All the questionnaires were completed during a single follow-up visit at the clinic.
Degree of asthma control
The degree of asthma control was determined using the asthma control test (ACT) [12]. Participants responded to 5 questions pertaining to a recent 4-week period. The questions verified occurrences of episodes of dyspnea, sleep impairment due to asthma symptoms, limitations in daily activities, the use of rescue inhalatory medications, and self-rated degree of asthma control. Each question was scored from 1 to 5 points. A score of 20 points or higher corresponded to controlled asthma.
Depression level
Level of depression was evaluated with the long form of the Beck Depression Inventory (BDI – Long Form) [13]. The participants were required to answer 21 questions and each answer was scored on a scale from 0 to 3. The BDI overall score corresponds to the depression levels in a given individual, with higher overall scores indicative of more severe depressive symptoms. The individual is considered free from depression if the overall score is 11 points or less.
Levels of trait anxiety and state anxiety
Anxiety level was determined using the State-Trait Anxiety Inventory (STAI), which examines anxiety as a transient state (X-1 questionnaire) and a relatively stable personality trait (X-2 questionnaire) [14]. Each questionnaire consists of a 20-question inventory, with answers scored from 1 to 4. Higher overall scores suggest higher levels of anxiety.
Statistical analysis
Statistical analysis included the Mann-Whitney U test and the Kruskal-Wallis test. Power and direction of relationships between 2 continuous variables was determined using the Spearman’s rank coefficient of correlation (R). Significance of relationships between the pairs of discrete variables was verified with the Pearson’s chi-square test. All calculations were carried out using the Statistica 8 (StatSoft®) software package, with the level of significance assumed at p≤0.05.
Results
Our study included a group of 128 randomly selected patients, among them 5 individuals who were excluded from further analysis due to incomplete data. As a result, 123 patients were studied, and their characteristics are presented in Table 1. Average age of the participants was 41.73±14.13 years. Due to low representation of individuals living in towns with population fewer than 10,000 and those from cities with 50,000 to 100,000 inhabitants, for the purpose of further analysis these participants were incorporated into the subgroups of countryside dwellers and inhabitants of cities with 10,000 to 50,000 population, respectively.
Table 1.
Characteristics of study participants.
| Gender | Males | Females | ||||||||
| n | % | n | % | |||||||
| 33 | 26.8 | 90 | 73.2 | |||||||
| Place of residence | Countryside | Towns up to 10 000 | Towns up to 50 000 | Cities up to 100 000 | Cities over 100 000 | |||||
| n | % | n | % | n | % | n | % | n | % | |
| 43 | 35.0 | 4 | 3.3 | 39 | 31.7 | 7 | 5.7 | 30 | 24.4 | |
| Employment | Employed | Unemployed | ||||||||
| n | % | n | % | |||||||
| 68 | 55.3 | 55 | 44.7 | |||||||
| Prevalence of depression | Depression | Depression-free | ||||||||
| n | % | n | % | |||||||
| 40 | 32.5 | 83 | 67.5 | |||||||
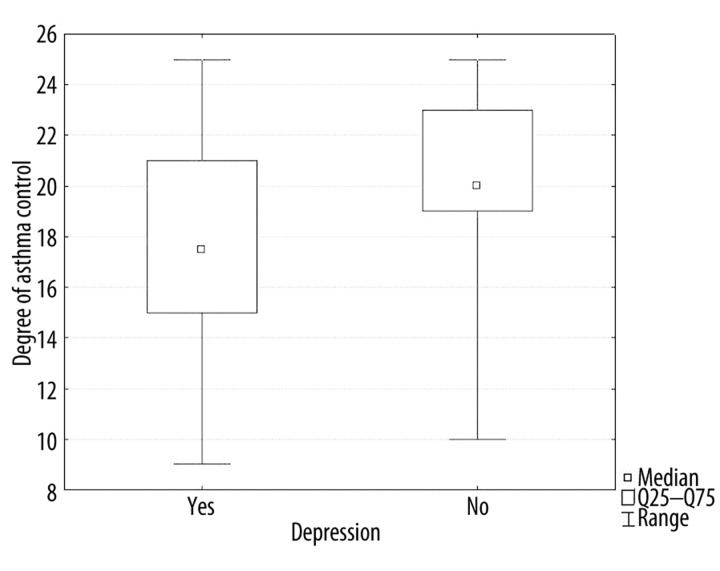
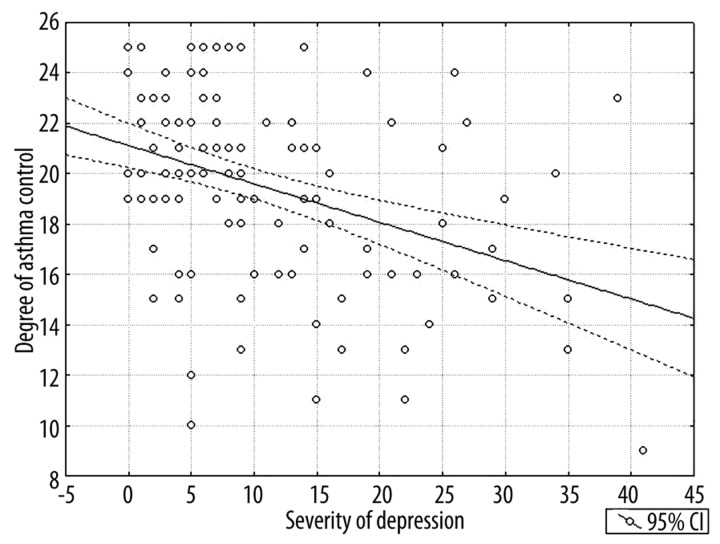
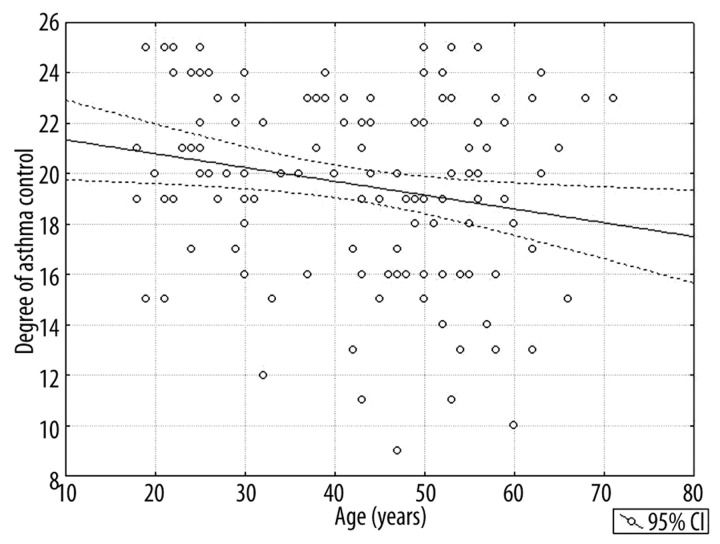
Our study revealed that the participant’s age, the occurrence of depression and its severity significantly correlate with the degree of bronchial asthma control. Individuals with depression were characterized by significantly lower degree of asthma control compared to depression-free individuals (p<0.001, Table 2, Figure 1). Furthermore, the degree of asthma control decreased significantly with increasing severity of depression (R=−0.367, p<0.001, Figure 2) and age of the responder (R=−0.188, p=0.037, Figure 3).
Table 2.
Degree of asthma control depending on the presence of depression.
| Variable | Depression (n=40) | Depression-free (n=83) | p value | ||
|---|---|---|---|---|---|
| Mean ±SD | Median (Q25–Q75) | Mean ±SD | Median (Q25–Q75) | ||
| Degree of asthma control | 17.7±3.88 | 17.5 (15–21) | 20.52±3.20 | 20 (19–23) | <0.001 |
Figure 1.
Comparison of the degree of asthma control in individuals with and without depression.
Figure 2.
Correlation of the degree of asthma control and severity of depression.
Figure 3.
Correlation of the degree of asthma control and age (years).
In contrast, no significant correlation was observed between the degree of asthma control and the levels of trait anxiety (R=−0.095, p=0.295) and state anxiety (R=−0.093, p=0.308).
Discussion
Based on review of the literature published between 1980 and 2002 [15], the prevalence of anxiety and mood disorders among bronchial asthma patients can be estimated at 41–52%. A comparable prevalence of depression (32.5%) was documented in our participants, and the slight differences that were observed may have resulted from using different diagnostic tools and the small size of the analyzed groups. In contrast, a surprisingly low co-existence rate of asthma and psychopathological disorders was reported by Spinoza-Leal, who performed a comparative analysis of asthmatic and healthy Mexicans [16]. Nonetheless, his study confirmed that the prevalence of mental disorders in asthma patients is higher than in healthy individuals (anxiety and depression were observed in 30% and 8% of asthmatics, respectively, compared to 18% and 3% in healthy individuals). The lower prevalence of psychopathologies in asthmatics analyzed by Spinoza-Leal can be explained by the different type of diagnostic tool used (Hospital Anxiety and Depression Scale), the different ethnic and cultural background of the studied population, and the relatively young age of patients (34 years of age on average).
Numerous previous studies have not confirmed the relationship between asthma severity and the occurrence of psychopathological symptoms [15]. Current studies of the problem are usually based on the Asthma Control Test (ACT). Nonetheless, their results are still inconclusive – according to some studies, only anxiety [17], and according to others, only depression [18] correlates with the degree of asthma control. In a 1994 study, Janson [19] observed a correlation between the prevalence of anxiety and depression and the occurrence of asthma symptoms. In another study [15], anxiety and depression were more frequent among patients with “difficult” asthma. In our study, the prevalence of depression and its severity were significantly correlated with the degree of asthma control. In contrast, no correlation was observed between the degree of asthma control and the state and trait anxiety levels. This raises the question for the reason behind the discrepancies in the results of these aforementioned studies. Obviously, they can result from methodological differences. Firstly, one should consider all the possible limitations related to using a questionnaire as a diagnostic tool. It has been demonstrated that the results of a questionnaire survey can be modulated by the conditions of testing (filling out the questionnaire at the hospital in the presence of another person vs. completing a questionnaire that was sent by mail at home) [20]. Consequently, a standardized multicenter trial, including large populations with various ethnic and cultural backgrounds, and taking into account their sociological characteristics, is needed in order to comprehensively explain the character of the relationships in question.
Due to the recommended (and widespread) application of the Asthma Control Test in management of asthma patients, we decided to search for potential correlations between its results and the prevalence of psychopathological disorders. However, one should keep in mind that ACT is a relatively subjective tool. Thus, one can ask whether similar relationships can be observed using objective indicators of asthma activity. Previous studies have not confirmed a significant correlation between the prevalence of psychosomatic disorders and bronchial hyper-responsiveness (during provocation with methacholine) [17,19] or daily fluctuation in peak expiratory flow (PEF) [19]. Moreover, the results of spirometric studies are inconclusive. Krommydas et al [21] observed a significant decrease in FEV1 and FEV1/FVC in patients with depression symptoms, while no relationships between the results of depression scale and pulmonary functioning were documented in another study [22]. Consequently, the question of clinical significance of these studies still remains open.
One can ask about the direction of causative relationship between the prevalence of asthma and mental disorders; this question cannot be answered based on the results of our study. Plausibly, any disease-related limitations in functioning can predispose to the development of psychopathological symptoms. However, this hypothesis was at least partly disproven by the results of Centanni et al. [9] who observed that depressive symptoms are more frequent in asthma patients than in individuals with chronic liver failure, an example of another severe somatic disease. Perhaps a more detailed examination of the symptoms of depressed mood would be able to find those that are specific for asthma. Additionally, depression can exacerbate asthma symptoms directly (it is suggested that it can impair the voluntary activation of the diaphragm, thus impairing the respiratory drive [23]) or indirectly (via a decreased motivation for proper asthma control, and poorer coping with the disease). Also, a possible synergism between asthma and depression, where one exacerbates the other, has been postulated [24].
Interestingly, our study revealed no significant correlation of state and trait anxiety level with the degree of asthma control. However, discrepancies between the results of previous studies in this matter suggest a careful interpretation, and the need for further large and standardized studies to explain the actual status of the problem in question.
Our study confirmed that both the prevalence and severity of depression are related to the degree of asthma control. In view of similar results presented by other authors, this finding constitutes sufficient rationale for implementing screening of the asthmatic population for possible mental disorders. The protocols of potential therapeutic intervention should be analyzed in terms of their effectiveness in controlling mental symptoms and their influence on the course of asthma. Particularly important is the question of whether improved control of asthma can alleviate the mental complaints, or are parallel therapeutic efforts needed to control both the asthma and the co-existing mental problems. Screening asthma patients for psychopathological disorders can also be effective in terms of healthcare economics since asthmatics with mental comorbidities, including depression and anxiety, have been observed to use healthcare services with increased frequency [25,26]. Further studies are needed in this matter due to their potential therapeutic implications. Some authors have reported positive effects of behavioral training [11] and respiratory exercise [27] on the level of psychopathological symptoms observed in asthmatics. Furthermore, one should keep in mind that co-existing depression can be associated with poorer cooperation of asthma patients [15].
All of these aforementioned arguments, along with the still relatively low detection rates of psychopathological conditions in asthmatics, suggest that this relationship deserves more attention and further research.
Conclusions
The prevalence of depression and its severity significantly correlate with the degree of bronchial asthma control.
No significant correlations were observed between the levels of state anxiety and trait anxiety and the degree of bronchial asthma control.
Carrying-out large, standardized multicenter studies seems to be necessary due to significant discrepancies in the results of studies conducted on small study groups.
In light of the existence of statistically significant correlation between the prevalence of asthma and psychopathological symptoms and the low percentage of clinical diagnoses of mental disorders in the population of asthmatics, it seems reasonable to introduce the screening of this group of patients for mental disorders.
Footnotes
Source of support: Departmental sources
References
- 1.Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25:1209–21. doi: 10.1002/gps.2463. [DOI] [PubMed] [Google Scholar]
- 2.NIH Publication 02-3659. Bethesda, MD: Global strategy for asthma management and prevention. available on: http://www.ginasthma.com. [Google Scholar]
- 3.Goodwin RD, Jacobi F, Thefeld W. Mental disorders and asthma in the community. Arch Gen Psychiatry. 2003;60:1125–30. doi: 10.1001/archpsyc.60.11.1125. [DOI] [PubMed] [Google Scholar]
- 4.Nascimento I, Nardi AE, Valenca AM, et al. Psychiatric disorders in asthmatic outpatients. Psychiatry Res. 2002;110:73–80. doi: 10.1016/s0165-1781(02)00029-x. [DOI] [PubMed] [Google Scholar]
- 5.Nejtek VA, Brown ES, Khan DA, et al. Prevalence of mood disorders and relationship to asthma severity in patients at an inner-city asthma clinic. Ann Allergy Asthma Immunol. 2001;87:129–33. doi: 10.1016/s1081-1206(10)62206-5. [DOI] [PubMed] [Google Scholar]
- 6.Zhang T, Carleton BC, Prosser RJ, Smith AM. The added burden of comorbidity in patients with asthma. J Asthma. 2009;46:1021–26. doi: 10.3109/02770900903350473. [DOI] [PubMed] [Google Scholar]
- 7.Katon W, Lozano P, Russo J, et al. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. J Adolesc Health. 2007;41:455–63. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strine TW, Mokdad AH, Balluz LS, et al. Depression and anxiety in the United States: findings from the 2006 Behavioral Risk Factor Surveillance System. Psychiatr Serv. 2008;59:1383–90. doi: 10.1176/ps.2008.59.12.1383. [DOI] [PubMed] [Google Scholar]
- 9.Centanni S, Di Marco F, Castagna F, et al. Psychological issues in the treatment of asthmatic patients. Respir Med. 2000;94:742–49. doi: 10.1053/rmed.1999.0766. [DOI] [PubMed] [Google Scholar]
- 10.Wamboldt MZ, Hewitt JK, Schmitz S. Familial association between allergic disorders and depression in adult Finnish twins. Am J Med Genet. 2000;96:146–53. doi: 10.1002/(sici)1096-8628(20000403)96:2<146::aid-ajmg4>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 11.Tousman S, Zeitz H, Taylor LD. A pilot study assessing the impact of a learner-centered adult asthma self-management program on psychological outcomes. Clin Nurs Res. 2010;19:71–88. doi: 10.1177/1054773809354290. [DOI] [PubMed] [Google Scholar]
- 12.Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 14.Spielberger CD, Gorsuch RL, Luschene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press; 1970. [Google Scholar]
- 15.Baumeister H, Korinthenberg K, Bengel J, Härter M. Bronchial asthma and mental disorders – a systematic review of empirical studies. Psychother Psychosom Med Psychol. 2005;55:247–55. doi: 10.1055/s-2004-834681. [DOI] [PubMed] [Google Scholar]
- 16.Espinosa Leal FD, Parra Román M, Méndez NH, et al. Anxiety and depression in asthmatic adults in comparison to healthy individuals. Rev Alerg Mex. 2006;53:201–6. [PubMed] [Google Scholar]
- 17.Wang G, Wang L, Szczepaniak WS, et al. Psychological status in uncontrolled asthma is not related to airway hyperresponsiveness. J Asthma. 2010;47:93–99. doi: 10.3109/02770900903331119. [DOI] [PubMed] [Google Scholar]
- 18.Wang L, Mo ZC, Ji YL. The study on relationship between negative mood states and asthma control and quality of life. Sichuan Da Xue Xue Bao Yi Xue Ban. 2009;40:544–47. [PubMed] [Google Scholar]
- 19.Janson C, Björnsson E, Hetta J, Boman G. Anxiety and depression in relation to respiratory symptoms and asthma. Am J Respir Crit Care Med. 1994;149:930–34. doi: 10.1164/ajrccm.149.4.8143058. [DOI] [PubMed] [Google Scholar]
- 20.Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health. 2005;27:281–91. doi: 10.1093/pubmed/fdi031. [DOI] [PubMed] [Google Scholar]
- 21.Krommydas GC, Gourgoulianis KI, Angelopoulos NV, et al. Depression and pulmonary function in outpatients with asthma. Respir Med. 2004;98:220–24. doi: 10.1016/j.rmed.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 22.Rimington LD, Davies DH, Lowe D, Pearson MG. Relationship between anxiety, depression, and morbidity in adult asthma patients. Thorax. 2001;56:266–71. doi: 10.1136/thorax.56.4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen GM, Hickie I, Gandevia SC, McKenzie DK. Impaired voluntary drive to breathe: a possible link between depression and unexplained ventilatory failure in asthmatic patients. Thorax. 1994;49:881–84. doi: 10.1136/thx.49.9.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rubin NJ. Severe asthma and depression. Arch Fam Med. 1993;2:433–40. doi: 10.1001/archfami.2.4.433. [DOI] [PubMed] [Google Scholar]
- 25.Di Marco F, Verga M, Santus P, et al. Close correlation between anxiety, depression, and asthma control. Respir Med. 2010;104:22–28. doi: 10.1016/j.rmed.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 26.Gershon AS, Wang C, Guan J, To T. Burden of comorbidity in individuals with asthma. Thorax. 2010;65:612–18. doi: 10.1136/thx.2009.131078. [DOI] [PubMed] [Google Scholar]
- 27.Thomas M. Are breathing exercises an effective strategy for people with asthma? Nurs Times. 2009;105:22–27. [PubMed] [Google Scholar]