Summary
Background
The aim of the research was to evaluate the effectiveness of the phased rehabilitation program in patients after traumatic brain injury, one developed by the authors and controlled by the strategic plan, pertaining to their quality of life compared to patients treated according to a standard, phased rehabilitation program.
Material/Methods
The study included 40 patients of post traumatic brain injury treated at the Rehabilitation Clinic of the L. Rydygier Academy of Medical Sciences in Bydgoszcz and the Department of Medical Rehabilitation of the Cracow Rehabilitation Centre. An experimental group included 20 patients rehabilitated by a strategic approach and a control group consisted of 20 patients treated before the introduction of this approach. In assessing the effectiveness of rehabilitation, a structured interview was used with clinical observation and the Battery of Quality of Life Assessment. The study was conducted twice: before and after eight weeks of rehabilitation.
Results
The quality of life of people after brain injury is affected by self-service difficulties, difficulties in meeting the physiological needs and loss of psychophysical comfort, decreased mobility, impaired cognitive functions and executive and social functions. There is no consistency between the stated (subjective) level of quality of life of the patient, and the depth of objectively measured disability resulting from the injury sustained.
Conclusions
A rehabilitation program controlled by a strategic plan, in collaboration with the patient treated subjectively is more effective in improving the quality of life, since the cooperating patient is more motivated to carry out individually designed goals. A rehabilitation program based on a strategic plan is worthy of recommendation for the treatment and improvement of patients after cranio-cerebral trauma.
Keywords: treatment plan, individual needs, effectiveness of rehabilitation
Background
Every year about 1 million people in Europe suffer a cranio-cerebral injury.
In as many as 75 to 80% of these cases, mild brain damage is diagnosed as a result, while in the remaining 10 to 15% the damage is severe [1]. Following these lesions, somatoform disorders, cognitive, emotional and behavioural disorders are observed, which are often wrongly considered to be psychogenic [2]. In any case, these conditions reduce the quality of life for patients [3].
Brain injury, especially one that takes place with more severe consequences, radically, rapidly and permanently changes the patient’s quality of life [3,4]. In this context, more important than all the inconvenience and discomfort is a sense of radical discontinuity in the course of life, now divided into two periods:
before the accident,
after the accident.
The literature includes, as noted by [1], hundreds of reports on the various consequences of brain injury. The authors discuss the cognitive deficits, behavioural problems, learning difficulties and deterioration of adaptive behaviour, especially in children and adolescents with severe damage, perceptual disturbances associated with the sense of body in space and motor deficits [1,2,4–6].
A person affected by severe brain trauma must learn many new skills and ways of coping with difficulties, some of which (e.g. riding in a wheelchair) are quite new, while others are long since learned activities (e.g. walking, bathing), yet now performed in quite different conditions. This difficult learning process, one following a traumatic brain injury and successive, various surgical procedures, hospitals stays and rehabilitation centres, etc., often takes place over many weeks, months or even years [3,7].
Many patients complain that the big obstacle in mastering these skills is a sense of social isolation and fear that they are left alone, unable to rely on anyone. The basic question: “What next?” can rarely be answered [6,7], and this prompts the patient to conclude that all those routine words of comfort are ungrounded, while the future looks bleak [8,9].
This situation is aggravated by the fact that victims of brain injuries, most often caused by car accidents, are often young people, active in their personal life or at work, who intended to study, start a family or pursue a career. Patients with traumatic brain injury often complain that after the accident nothing is like before. “I had a whole life ahead of me,” they say, “and now what will become of me?” It often happens that a person who before the accident was in the prime of life, in an important position, complains: “I was somebody, and now I am nobody!”
Stancin et al. [2] observe that still surprisingly little is known about social functioning and quality of life after severe cranio-cerebral trauma. The importance of social competence as a forecast of a wide range of effects is often stressed, including psychological adjustment, achievement in professional life and health status [3–6]. Stancin et al. [2] find that poor performance in social functioning may play a major role in lowering the quality of life in patients after traumatic brain injury. However, the authors note that these results do not correlate with the lives of patients in the later period after the accident.
The observations of clinicians and research [3–5] indicate that the lives of patients after cranio-cerebral trauma, in the later period after the accident, can vary:
some are successful, overcome barriers and find a way of life that gives them a sense of satisfaction,
others break down, get into specific states of mourning after the loss of existing skills, states of loneliness, isolation and social dependence.
Meanwhile, the factors responsible for success or failure in the process of rehabilitation are not fully understood. According to many scholars, failures in rehabilitation are considered one of the main factors responsible for the disturbance in the adaptability of the organism [10,11], and decreased quality of life in patients after traumatic brain injury [4,12]. According to these authors, it is therefore important to carry out further research on the relation of effectiveness of rehabilitation with the quality of life of patients after cranio-cerebral trauma.
The essence of quality of life
In medical studies of patients with a variety of brain damage types, the definition of Health-Related Quality of Life – HR-QOL is most commonly used [13–16]. The essence of Health-Related Quality of Life is often identified with the degree of perceived well-being, lack of symptoms and psychological condition and the ability to undertake various activities [16].
A review of the literature allows one to observe that this term is used in at least three different meanings. And so the quality of life is understood as:
measure of negative impact on the mental health of a patient of some chronic and/or secondary symptoms of illness or injury not constituting a direct threat to their life [8,9,17–20].
measure of the effectiveness of treatment, i.e., the final effect of treatment (called “outcome”), which is rated on a scale of patient’s “quality of life” after completing a particular treatment program [21–25].
reference point in making difficult decisions in life in the severe and incurable states: for example, the decision to abandon resuscitation procedures when serious damage to the body appears to be irreversible [26–31].
In this paper we have adopted the definition which the authors from the Cracow Rehabilitation Centre have developed [31–33]). The basis of the definition is that a feeling of contentment and happiness regarded as essential to quality of life depends largely on the difference felt by the patient between:
needs (at the physiological level),
desires (at the emotional level),
dreams (at the mental and spiritual level),
and their current implementation and the real (or perceived) opportunities for their implementation in the future. Thus understood, the essence of quality of life turns out to be more useful in the clinical approach to nervous system damage [31], particularly in those patients who have suffered brain and brain stem injury [3], as it is determined by the difference between the present state and the target state of the patient in light of the possibilities of reducing this gap to an acceptable level limited by the disease [7].
Through a comprehensive approach to human functioning in all its dimensions (physiological, emotional, mental and spiritual), which in fact, as noted by Grochmal-Bach [34], are hardly separable – the possibilities are also created by evaluating the effects of rehabilitation.
It is common knowledge that the effects of serious emotional problems can be felt in human physiology. The spiritual crisis often leads to unfavourable changes in many systems, and only an exceptional man in the face of serious, long-term illness or disability feels inner peace and the closeness of God. This does not mean that the physiotherapist has to be simultaneously a doctor, psychotherapist and priest for their patients. However, without attention to the overall situation of the patient’s life it may be doubted whether our influence will have satisfactory results. Thus, examination of the effectiveness of rehabilitation in relation to the quality of life seems to be even more purposeful, with particular emphasis on the relation of the efficacy of a comprehensive, strategic approach to the issues of the quality of life discussed here. Escape from these issues can only be bought at the expense of the resignation from assessing the quality of life for our patients, which deprives all kinds of rehabilitation effects of the raison d’être.
Material and Methods
Research issues
Assumptions and objective of the study
The aim of this study was to evaluate the effectiveness of the phased rehabilitation program in patients with cranio-cerebral trauma, controlled by the strategic plan [35–37], pertaining to their quality of life compared to patients treated according to a standard, phased rehabilitation program2.
Taking the assumption that conduct in the standard rehabilitation programs of the various treatments and therapy techniques being only in response to current problems does not lead to the overarching goal of rehabilitation, which is activating the mechanisms of adaptation and compensation, enabling the patient to obtain the best possible quality of life [16,23,38], a rehabilitation program controlled by a strategic plan was introduced, developed by Pąchalska et al. [36]. According to the authors, this program is geared towards the target, implemented with the cooperation of a patient after cranio-cerebral trauma, and adapted to the individual needs of a patient, treated subjectively. This approach assumes a significant contribution of the patient in the process of developing and implementing this plan.
Particular attention was paid to such factors as:
The specificity and complexity of the clinical picture in the absence of appropriate rehabilitation programs.
The overall situation of the patient’s life after rehabilitation and in particular social isolation and dependence.
The effectiveness of existing, standard rehabilitation programs for people with brain and brain stem injuries.
Material
The study included 40 patients with post traumatic brain injury treated at the Rehabilitation Clinic of the L. Rydygier Academy of Medical Sciences in Bydgoszcz (with the consent of the head of the Department) and the Department of Medical Rehabilitation in the Cracow Rehabilitation Centre (with the consent of the Head). The control group (n=20, including 11 men and 9 women) are patients rehabilitated according to a staged rehabilitation program [37] applied before the introduction of the strategic plan developed within the framework of the experiment, and focused on the goal. The experimental group (n=20, including 13 men and 7 women) are patients also rehabilitated according to a staged rehabilitation program, with additional application of the goal-oriented strategic program [36].
Such a selection of groups was due to:
lack of a goal-oriented strategic program in the course of the rehabilitation of the control group,
need to verify the new program in a clinical setting by comparing the results obtained in the process of rehabilitation of patients in the experimental group and the control group conducted according to the same rehabilitation program, where, additionally, a goal-oriented strategic program was used in the experimental group.
Biographical and clinical characteristics of the patients studied
The biographical and clinical characteristics of the patients studied are shown in Table 1 and 2.
Table 1.
Biographical and clinical characteristics of patients in K group.
| No. | Age | Sex | Cause of injury | GCS | Significant clinical symptoms | ||
|---|---|---|---|---|---|---|---|
| Injuries | Procedures | The main ailments | |||||
| 1. | 27 | M | Traffic accident (driver) | 5 | Brain injury, epidural and subdural hematoma of right temporal area, hydrocele of fronto-parietal area, fracture of the sternum. | Neurosurgery 3-fold, removal of hematoma and hydrocele, cranial bone defects | Hemiplegia, with a predominance of the left side, vertigo, difficulty breathing, medium grade mixed aphasia, impaired attention, working memory impairment, impaired executive functions. |
| 2. | 37 | M | Traffic accident (driver) | 4 | Brain injury, cerebral oedema. | None | Hemiparesis, balance disorder, emotional and motivational disorders, impaired working memory, frontal lobe syndrome characteristics, impaired executive functions |
| 3. | 22 | M | Traffic accident (hit motorbike rider) | 5 | Brain trauma, cerebral oedema, bone fracture of the left and right forearm. | None | Tetraparesis pronounced in the lower extremities, knees and feet contractures, emotional and motivational disorders, impaired working memory, frontal lobe syndrome characteristics, impaired executive functions. |
| 4. | 22 | F | Traffic accident (hit pedestrian) | 7 | Brain injury, subdural hematoma around the left frontal-parietal-temporal area, skull fracture, fracture of the left lower leg | Neurosurgery, craniotomy, removal of acute subdural hematoma, bone loss, orthopaedic, bone fusion of the left lower leg | Right-sided hemiparesis, slight motor aphasia, emotional and motivational disorders, impaired executive functions. Limitation of independence |
| 5. | 14 | F | Traffic accident (hit bike rider) | 5 | Brain injury, extensive epidural hematoma, skull fracture, right leg contusion | Neurosurgery, craniotomy, evacuation of hematoma, cranial bone defects | Left-sided hemiparesis, retrograde amnesia, abdominal pain, impaired executive functions, emotional-motivational disorders |
| 6. | 28 | F | Traffic accident (driver) | 7 | Brain injury, intracranial hematoma, pelvic fracture, injury of internal organs | Surgery | Tetraplegia, emotional-motivational disorders, limitation of independence. |
| 7. | 22 | F | Traffic accident (passenger) | 4 | Brain injury, subarachnoid hematoma, skull, mandible, pelvis, left elbow fracture, bruised left shoulder and hip joint and the left lung. | None | Tetraparesis pronounced on the right side, trace aphasia, ossification of the left elbow and shoulder joint, vertigo, emotional and motivational disorders, post-traumatic depression, frontal lobe syndrome characteristics. |
| 8. | 30 | F | Traffic accident (driver) | 4 | Brain injury | None | Left-sided hemiparesis, balance disorders, emotional-motivational disorders, depression |
| 9. | 21 | M | Traffic accident (driver) | 5 | Brain injury, subdural hematoma of the right fronto-temporal area, left temporal area hydrocele, skull fracture, right clavicle fracture, lung contusion. | Neurosurgery, trepanation of the skull and evacuation of hematoma, cranial bone defects, orthopaedic 2-fold of hand and foot contractures | Tetraparesis pronounced in the lower extremities and the left upper extremity, limitation of independence, decreased vision, working memory, frontal lobe syndrome characteristics, apraxia, executive dysfunction. |
| 10. | 22 | M | Traffic accident (hit motorbike rider) | 6 | Brain injury, cerebral oedema, thoracic trauma, contusion of internal organs | None | Discrete right handed paresis, medium grade motor aphasia, characteristics of frontal lobe syndrome, apraxia, executive dysfunction. |
| 11. | 30 | M | Traffic accident (hit pedestrian) | 5 | Brain injury, subdural hematoma of fronto-parietal area, fracture of the left humerus and bones of the left forearm and left lower leg bones. | Neurosurgery, craniotomy, cranial bone defects, orthopaedic, amputation of the left foot | Tetraplegia, balance disorders, mixed medium grade aphasia, dysarthria. |
| 12. | 15 | M | Traffic accident (hit pedestrian) | 3 | Brain injury, skull fracture, intracerebral hematoma, fracture of the mandible, the right forearm, left lower leg bones, pelvic bones, bruised right lung and right kidney. | Neurosurgery, decompression, cranial bone defects, orthopaedic, twice; fusion of shin and thigh bone | Right handed paresis, limited self-reliance, emotional and motivational disorders, hemianopia, frontal lobe syndrome characteristics. |
| 13. | 23 | F | Traffic accident (driver) | 7 | Brain injury, cerebral oedema, intracerebral hematoma, | None | Limb muscle weakness, pain in the knees, frontal lobe syndrome, apraxia, impaired working memory, confabulation. |
| 14. | 53 | M | Traffic accident (driver) | 5 | Brain injury, subdural hydrocele, in the forehead, lung contusion | Neurosurgery, trepanation, evacuation of hydrocele | Left lower limb monoplegia, limited self-reliance, frontal lobe syndrome, impaired executive functions, emotional and motivational disorders |
| 15. | 18 | M | Traffic accident (hit motorbike rider) | 5 | Brain injury, subarachnoid hematoma, skull fracture, fracture of the left metatarsal bones, skull fracture, fracture of the left metatarsal bones. | Orthopaedic, fixing of bones of left foot | Tetraplegia, mild dysarthria, impaired executive functions, limited self-reliance, difficult contact. |
| 16. | 19 | M | Traffic accident (motorbike rider, collision with a tree) | 6 | Brain injury, subarachnoid hematoma, hydrocephalus, skull fracture, fracture of the femur on the left and right, fracture of left and right forearm, fracture of the ribs on the right side and the bones of the pelvis, right lung puncture. | Neurosurgery 2 times, removal of hematoma, valve implantation, orthopaedic, hand bone fixation, femoral fixation, surgery | Tetraparesis pronounced in the right hand, emotional and motivational disorders. |
| 17. | 17 | F | Traffic accident (driver) | 5 | Cerebral trauma, broken rib, right lung contusion, pneumothorax, pelvic trauma, fracture of the right metacarpals. | None | Tetraparesis pronounced on the right side, slight motor aphasia, reduced independence. |
| 18. | 30 | F | Traffic accident (passenger) | 3 | Cerebral trauma, pneumothorax, contusion of the right lung, pelvic fracture | Thoracic surgery | Tetraparesis pronounced on the right side. Residual motor aphasia. Frontal lobe syndrome. Memory impairment. Disorders of executive functions. |
| 19. | 43 | M | Traffic accident (driver) | 4 | Brain injury, intracerebral hematoma | Neurosurgery, evacuation of hematoma, cranial bone defects | Tetraparesis with pronounced spasticity on the left side. Frontal lobe syndrome. Disorders of executive functions. Confabulation. Anosognosia. |
| 20. | 33 | F | Traffic accident (passenger) | 6 | Brain injury, subdural hematoma of left temporo-parietal area, pelvic fracture, fracture of the right lower leg | Neurosurgery, evacuation of hematoma, cranial bone defects, temporo-parietal craniotomy with decompression | Spastic tetraparesis, reduced independence, impeded verbal contact. |
Table 2.
Biographical and clinical characteristics of patients in E group.
| No. | Age | Sex | Cause of injury | GCS | Significant clinical symptoms | ||
|---|---|---|---|---|---|---|---|
| Injuries | Procedures | The main ailments | |||||
| 1. | 48 | M | Traffic accident (hit pedestrian) | 4 | Cerebral trauma, cerebral oedema, broken ribs on the right side, the right humerus fracture, fracture of the right lower leg, puncture of the right lung, pneumothorax | Orthopaedic, fixation of ribs and lower leg bones | Monoparesis of right leg, rib and chest pains, difficulty breathing, blurred vision, reduced independence, working memory impairment, impaired executive functions. |
| 2. | 14 | M | Traffic accident (hit bike rider) | 3 | Brain injury, cerebral oedema, subdural hematoma. | Neurosurgery, trepanation and evacuation of hematoma | Tetraparesis pronounced on the left side, limitation of autonomy, medium grade motor aphasia. |
| 3. | 25 | F | Traffic accident (passenger) | 3 | Brain injury, intracerebral hematoma, dislocation of left shoulder, right lung contusion | Neurosurgery, bilateral trepanation | Right-handed hemiplegia, slight motor aphasia, reduced independence, executive dysfunction, apraxia, frontal lobe syndrome characteristics |
| 4. | 17 | M | Traffic accident (hit bike rider) | 3 | Cerebral trauma, fracture of left femur | None | Right-handed hemiparesis, slight motor aphasia, agraphia and apraxia. |
| 5. | 31 | M | Traffic accident (truck driver) | 3 | Brain injury | None | Tetraparesis pronounced in the right lower limb. Gait disturbance, mild dysarthria, dysgraphia, memory impairment, impaired executive functions. |
| 6. | 48 | M | Traffic accident (driver) | 3 | Brain injury, cerebral oedema, temporal bone fracture, rib fracture on the left side, the left lung injury | Neurosurgery, cranial bone defects | Right-handed hemiplegia, frontal lobe syndrome characteristics, medium grade motor aphasia. Agraphia, apraxia, executive dysfunction. |
| 7. | 23 | M | Traffic accident (driver) | 5 | Cerebral trauma, fracture of the right lower leg, | Orthopaedic right lower leg amputation, | Left lower limb monoplegia, contracture of stump, hearing loss, confabulation. |
| 8. | 47 | M | Traffic accident (driver) | 3 | Brain injury, intracerebral hematoma, fracture of the left clavicle, | None | Left-side hemiparesis, deep imbalance, pollakiuria, medium level motor aphasia, agraphia, apraxia, impaired working and autobiographical memory, confabulation, frontal lobe syndrome characteristics, impaired executive functions, reduced independence, |
| 9. | 42 | F | Trauma as a result of a beating to the head | 3 | Brain injury, intracerebral hematoma, bone fracture of the pelvis and left femur | Orthopaedic, fixation of the femur | Tetraparesis pronounced on the left side, quadriplegic contractures, motor aphasia medium grade, dysarthria, agraphia, apraxia |
| 10. | 63 | F | Traffic accident (hit pedestrian) | 4 | Brain injury, subarachnoid hematoma of the forehead, skull fracture | None | Slight tetraparesis pronounced on the left side, difficulty breathing, frontal lobe syndrome characteristics, working memory impairment, loss of vision in right eye, limited independence |
| 11. | 28 | M | Traffic accident (hit pedestrian) | 3 | Brain injury, subarachnoid hematoma, subdural hydrocele of fronto-parietal area, rib fractures on the right side, fracture of right shoulder blade, right wrist fracture, paralysis of the right shoulder plexus, injury to internal organs, contusion of the right lung. | Neurosurgery, decompression of the hematoma, hydrocele removal. | Tetraparesis pronounced on the right side, ossification of right hip and knee, emotional-motivational disorders, reduced self-reliance, apraxia, frontal lobe syndrome characteristics, impaired executive functions. |
| 12. | 37 | F | Traffic accident (hit pedestrian) | 3 | Brain injury, cerebral oedema, skull fracture, broken ribs, broken right tibia, pelvic fracture, injury of internal organs, | Orthopaedic, right knee, twice, surgery, removal of the spleen | Tetraparesis pronounced on the left side, high intensity of knee pain, difficulty breathing, motor aphasia medium grade, agraphia, dysarthria, reduced independence. |
| 13. | 22 | M | Traffic accident (driver) | 3 | Brain injury, subarachnoid hematoma, fracture of the ribs on the left side, left shoulder blade fracture, right clavicle fracture, lung contusion. | None | Monoplegia of lower limb, impaired working memory and attention, executive function disorders |
| 14. | 51 | M | Traffic accident (driver) | 3 | Brain injury, intracerebral hematoma, subdural hydrocele of the forehead, right forearm fracture, numerous cuts on forearms. | Neurosurgery, decompression of hematoma and hydrocele in the forehead, cranial bone defects | Tetraparesis pronounced on the right side, frontal lobe syndrome characteristics, slight motor aphasia, reduced independence |
| 15. | 39 | M | Traffic accident (hit pedestrian) | 4 | Cerebral trauma, broken ribs on the left side, the left lower leg fracture, injury of internal organs | Orthopaedic, left knee fixation, surgery, excision of the spleen | Tetraparesis pronounced on the left side, difficulty breathing, emotional-motivational disorders, frontal lobe syndrome characteristics, apraxia, executive dysfunction, reduced independence. |
| 16. | 27 | M | Traffic accident (driver) | 3 | Brain injury, cerebral oedema, fracture of right femur, right lower leg fracture, left lung contusion. | Orthopaedic, right femur fixation and left. Lower limb contractures surgery | Tetraparesis pronounced on the left side, emotional disorders, dysarthria, impaired executive functions. |
| 17. | 22 | F | Traffic accident (hit bike rider) | 3 | Brain injury, multiple fractures of the temporal bone, fracture of the left femur and left lower leg bones, right thumb | Orthopaedic, left lower leg bone fixation. | Right-sided hemiparesis, frontal lobe syndrome characteristics, working memory impairment, impaired executive functions |
| 18. | 37 | M | Accident at work (crushed by a wall) | 3 | Cerebral trauma, fracture of the left femur | Orthopaedic, left femur fixation | Tetraparesis, trismus, ossification of left elbow, impaired working memory, executive function disorders |
| 19. | 26 | F | Traffic accident (hit pedestrian) | 4 | Brain injury, subdural hematoma in fronto-parietal area, subdural hydrocele. | Neurosurgery, 3 times removal of hematoma and hydrocele, cranial bone defects | Pronounced spastic tetraplegia in the right side, medium grade mixed aphasia, emotional and motivational disorders, impaired working and long-term memory, frontal lobe syndrome characteristics, reduced independence. |
| 20. | 24 | F | traffic accident (driver) | 3 | brain injury, cerebral oedema, subarachnoid hematoma. | none | tetraplegia, dysarthria, medium grade motor aphasia, impaired working and long-term memory, reduced independence. |
The age of the patients in both groups was in the range from 14 to 63 years. 90% of respondents in Group K and 70% in Group E are young people, and their ages ranged from 20 to 40 years. The average age in group K was 26.3 years (s=9.48), while in Group E it was 33.6 years (s=12.71) and did not differ significantly (t=2.11, df=19; p<0.05).
The immediate cause of injury in the vast majority of patients was a traffic accident. And so, in group C all test subjects have suffered a cranio-cerebral injury following a traffic accident, including 9 persons as drivers, 3 persons as passengers, 4 people as motorbike riders, 1 person as a cyclist, and 3 people hit by a car. In group E, the vast majority of patients suffered a brain injury following a road accident, in which 8 people were drivers, 1 person – a passenger, three people – cyclists, and 6 people were hit pedestrians. Only 2 people have suffered brain injury as a result of other causes including 1 person with brain injury due to other reasons and 1 person due to being crushed by a wall.
In line with previous reports [1,37], severe brain injury was determined by the lowest post-resuscitation score on the Glasgow Coma Scale – GCS [3] with a score of 8 points or less. Moderate brain injury was defined as a GCS score of 9 to 12 points or 13–15 points, with accompanying damage to the skull, intracranial injury, or extensive cerebral oedema visible during routine clinical neuroimaging; posttraumatic neurological abnormality; loss of consciousness longer than 15 minutes.
All subjects, patients from both Group K and Group E, suffered the cranio-cerebral injury and stayed as a result of this injury in a coma lasting from 21 days to 9 months. At the time of admission to the ICU patients had from 3 to 7 points on the Glasgow scale and as a result suffered from multiple, post-traumatic neurological abnormalities and post-traumatic amnesia. Neuroimaging studies (CT, MRI) confirmed intracranial abnormalities in them.
And so, in group K, 2 patients had 3 points, 4 patients had 4 points on the Glasgow scale, 8 patients had 5 points, 3 patients had 6 points and 3 patients had 7 points on the Glasgow scale, while in group E, 15 patients had 3 points, 4 patients had 4 points and one patient 5 points on the Glasgow scale. The average value of the Glasgow scale points in group K was higher (x=5.05, s=1.16) than in group E (x=3.3, s=0.56), and the difference was statistically significant (t=5, 55, df=19, p<0.01).
In most people due to being hit on the head hematoma has developed within the brain. And so, in group K hematoma occurred in 13 patients and was mostly reabsorbed without having to operate in 4 patients, while 9 patients underwent surgery. In group E, in turn, hematoma occurred in 10 patients and was mostly reabsorbed without need for operation in 5 patients, and 5 underwent hematoma surgery.
In group K surgical losses in the bones of the skull occurred in 7 patients, while in group E in 5 patients.
In patients both in group K as well as in group E a variety of neurological ailments occurred. And so, in group K epilepsy was found in 6 patients, headaches in 18 patients, visual disorders in 11 patients. Dizziness was found in 12 patients. In group E, epilepsy was found in 7 patients, headaches in 19 patients, visual disorders occurred in 9 patients, and dizziness in 13 patients.
Two patients had a leg amputated, including one patient from group K and one from group E.
Research methods
In the studies, the following methods and tools were used:
Analysis of documentation (medical history, test results, including MRI and CT).
Clinical history, appropriately focused on the purpose of research [3]. Particular emphasis was put on: a way to deal with the constraints of the disease, patient attitudes, with particular reference to the image of oneself and one’s own future, the hierarchy of values and goals in life, the patient’s personality before the disease and life satisfaction.
Neuropsychological tests (screened) using standard procedures for assessing disorders of consciousness and cognitive processes: including memory and attention impairment, visual spatial function, executive functions, speech disorders of the aphasia or dysarthria type, emotional and motivational disorders and behavioural disorders [3].
-
Quality of Life Assessment Scale in Cranio-Brain Trauma Patients[33]. Quality of life assessment was performed in 8 divisions of the main factors that determine the quality of life. They are as follows:
self-service (independence in performing activities of daily living),
physiological needs (sphincter and sexual desire control),
physical and psychological comfort (pain and sleep disorders and mood control),
mobility (including locomotion),
communication,
cognitive functions (including memory, attention, logical thinking),
social functions (initiating and maintaining contact with other people in typical situations),
transportation (use of various modes of transport).
In each category five activities were evaluated in terms of the estimated percentage participation of the patient in its performance. The level of assistance required by the patient is determined pointwise by the following scale, adapted from the widely used International Standards of Neurological and Functional Classification of Spinal Cord Injuries – ASIA Scale [39]:
1 or 2 points: complete dependence (the patient’s own contribution: 0–25%);
3 to 5 points: limited autonomy (patient’s own contribution: 50%, 75%, and independently, but under the supervision of a guardian);
6 to 7 points: autonomy (the patient’s own contribution: 100% with or without adaptive devices).
Points were awarded on the basis of own examination and clinical history.
5. Assessment of the degree of brain damage which uses the Glasgow Coma Scale - GCS, Posttraumatic Amnesia Rating Scale, the analysis of documentation and CT and/or MRI neuroimaging test.
The organization and conduct of the tests
All tests were performed by the same person under similar location conditions and test circumstances, which gives a more reliable assessment of treatment outcome. The selection for groups was targeted, all individuals from both group K and group B, were awaken from the long-term post-traumatic (not pharmacological) coma. Persons available and suitable for research in terms of intellectual ability were selected.
Patients were tested twice, the first test was carried out before the start of rehabilitation, and the second after eight weeks of its duration.
The experiment excluded patients with very profound aphasia and patients with dementia. This fact was associated with the need for patient’s participation in some stages of the strategic planning process.
All subjects gave written informed consent to participate in the experiment, according to the protocol by the Bioethics Committee of the L. Rydygier Academy of Medical Sciences in Bydgoszcz.
The test methods were fully accepted by the subjects. Each of the subjects signed a written consent to being tested. The research project has the approval of the Bioethics Committee of the university.
Results
Changes in quality of life of the patients studied after cranio-cerebral trauma, including the results of research into the comparison of average results achieved by patients in both treatment groups in each category of Quality of Life Rating Scale [33] are shown in Table 3.
Table 3.
Summary of average results obtained in first and second test by patients in both treatment groups in the various categories of quality of life assessment.
| Group | Exam | Category | |||||||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | ||
| Experimental | 1 | 3.55 | 2.75 | 3.25 | 2.95 | 3.25 | 3.15 | 2.35 | 1.45 |
| 2 | 5.55 | 3.95 | 5.45 | 4.95 | 4.75 | 4.90 | 3.85 | 2.15 | |
| Control | 1 | 4.25 | 3.25 | 3.35 | 3.95 | 3.85 | 3.45 | 2.95 | 1.65 |
| 2 | 4.95 | 3.55 | 4.45 | 4.65 | 4.15 | 3.95 | 3.25 | 1.95 | |
A – Self-service; B – Satisfying physiological needs; C – Physical and psychological comfort; D – Movement efficiency; E – Communication; F – Cognitive functions; G – Social functions; H – Using the means of transport.
The quality of life of people after brain injury is affected by self-service difficulties, difficulties in meeting the physiological needs and loss of psychophysical comfort, decreased mobility, impaired cognitive functions (including communication difficulties) and executive and social functions disorders.
Statistical analysis performed using Student’s t-test for associated pairs shows that, upon comparing the average scores obtained by patients from both groups in each of the eight categories included in the applicable scale of quality of life assessment, the differences between the results from the first and second tests are highly statistically significant, at p=0.000035 for patients in group E, and in group K (p=0.0069). However, it is worth noting that the results of group K are significantly higher in the first study (p=0.00016), while in the second study, patients from group E, received significantly higher scores (p=0.016). This means a larger, statistically significant improvement, which occurred in group E, as a result of conducted rehabilitation, despite the slightly older age, and significantly worse outcomes in the Glasgow scale.
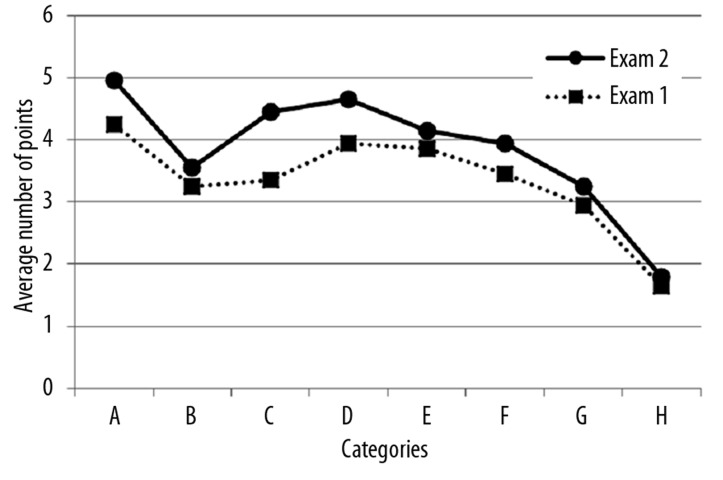
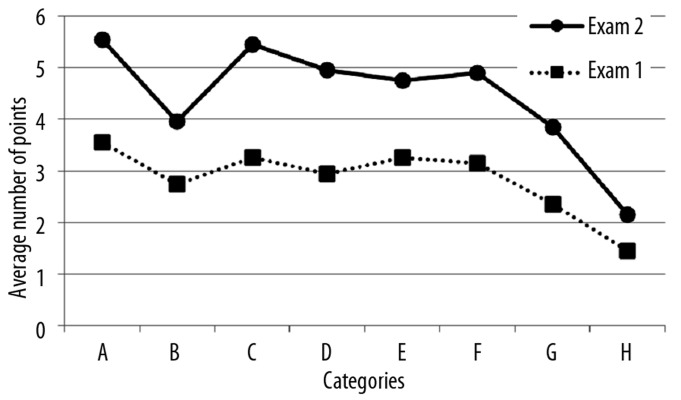
The results obtained by patients from both groups in the various categories of quality of life assessment are also shown graphically in Figures 1 and 2.
Figure 1.
Average results obtained in first and second test by patients in the control group in each category of quality of life assessment.
Figure 2.
Average results obtained in first and second test by patients in the experimental group in each category of quality of life assessment.
It was found that the differences between the results from the first and second test in group E are much larger than in group K. The group K profile shape has not changed much during the period from the first to the second test, while in group E, the shape is different significantly. In group K only the changes in category D are indicated, i.e. mobility and category E, i.e. the ability to communicate, while in group E, changes also occur in category C, i.e. in terms of physical and psychological comfort resulting from improvement in adaptability.
Motor functions, in both studied groups, are most susceptible to change associated with the rehabilitation process, while the least vulnerable are functions related to the use of different modes of transport. This change is much greater in subjects from group E than in those from group K.
There is no consistency between the stated (subjective) level of quality of life of the patient and the depth of objectively measured disability resulting from then injury sustained.
Discussion
In the summary and discussion it should be emphasized that the results obtained in this study may be affected by the depth of brain damage associated with the results obtained by the studied patients on the Glasgow scale. These results, as shown in the biographical characteristics of patients, were significantly worse in group E than in group K. Better final results obtained by patients from group E are all the more surprising, since at baseline, patients in this group obtained significantly lower scores than patients in group K. The fact that the studied groups were not at the same level of efficiency in the early studies did not result from a methodological error, but the neurological condition. Patients from group E had significantly lower values in the Glasgow scale than patients from group K.
Statistically significant differences between the two groups support the thesis, presented at the beginning of the article, that the quality of life of patients after cranio-cerebral injuries is ultimately determined not solely by the parameters for assessing the quality of life (because in this respect, patients in both treatment groups were well-paired), but the subjective reception of the course of their lives.
According to reports in the literature, also in this study a lack of consistency was found between the stated (or subjective) level of patient quality of life, and the objectively measured depth of his disability.
No one, admittedly, expresses satisfaction, e.g., with total paralysis of four extremities (this would raise reasonable doubts as to the sanity of the subject), however, cases were encountered in the material presented here where a person with lighter injuries mentioned a greater degree of discontent in a given range of functioning than a person who has suffered an irreversible loss of this function [21].
The specificity and complexity of the clinical picture of patients after cranio-cerebral injuries reduces the effectiveness of individual rehabilitation procedures, if the patient is unable to make an informed decision, or does not want to recognize own problems. With the passive attitude, resistance of the patient makes his general life situation after the rehabilitation unchanged, which deepens the dependence and/or social isolation [3].
The existing standard rehabilitation programs for people with various brain injuries are not adapted to the individual needs of patients after cranio-cerebral trauma, and regardless of possible improvements obtained with respect to several parameters (especially motor parameters) they do not allow for an increase in the quality of life. This is due to the fact that the patient is a passive object of the interactions of a physiotherapist and is devoid of his own voice in the process of his own treatment, something which is also emphasised by other authors [1,40].
A rehabilitation program aimed at the execution of individual goals, controlled by a strategic plan, in collaboration with the patient treated subjectively is more effective in improving the quality of life, since the patient at hisown discretion is responsible for the execution of individual goals. Objective progress achieved due to individual treatments is reflected in the subjective assessment of quality of life by the patient.
The benefits of the introduction into clinical practice of a strategic plan include not only the psychosocial parameters, but also physiological and motor parameters. The program is worth recommending for treatment and improvement of patients after cranio-cerebral injuries.
Conclusions
The obtained results allow one to formulate the following conclusions:
The quality of life of people after brain injury is affected by self-service difficulties, difficulties in meeting the physiological needs and loss of psychophysical comfort, decreased mobility, impaired cognitive functions (including communication difficulties) and executive and social functions disorders.
There is no consistency between the stated (subjective) level of quality of life of the patient and the depth of objectively measured disability resulting from the injury sustained.
Motor functions, in both studied groups, are most susceptible to change associated with the rehabilitation process, while the least vulnerable are functions related to the use of different modes of transport. This change is much greater in subjects from group E than in those from group K.
The existing standard rehabilitation programs for people with various brain injuries are not adapted to the individual needs of patients after cranio-cerebral trauma, and regardless of the possible improvements obtained with respect to several parameters (especially motor parameters) they do not allow for an increase in the quality of life, because the patient is a passive object of the interactions of the physiotherapist and is devoid of his own voice in the process of his own treatment.
A rehabilitation program controlled by a strategic plan, in collaboration with the patient treated subjectively is more effective in improving the quality of life, since the cooperating patient is more motivated to carry out individually designed goals.
The benefits of the introduction into clinical practice of a strategic plan include not only the psychosocial parameters, but also physiological and motor parameters. Having a specific, real purpose in the rehabilitation has considerable impact on the patient’s attitude towards their own future, as well as honest, cognitive image of their own situation.
A rehabilitation program based on a strategic plan is worthy of recommendation for the treatment and improvement of patients after cranio-cerebral injuries.
Footnotes
Who is eligible for the Comprehensive Rehabilitation Program? In order to receive services, the patient must: (1) have a traumatic brain injury, a traumatic spinal cord injury, or both. These injuries must have significantly affected the patients ability to perform daily activities, (2) be at least 16 years old by the time they finish the program, (3) be a Polish citizen or immigrant alien, (4) have lived in Poland for at least six months or have a primary caregiver who has lived in Poland for at least six months, (5) be medically stable enough to participate in rehabilitation activities, (6) agree to participate in the services offered by the DARS CRS program, as well as to participate in a strategic approach to rehabilitation.
What happens in the CRS program? Every person in the CRS program receives their own treatment plan, based on their individual needs, according to a strategic plan so-understood. The goal of the CRS program is to help people be more independent in their homes and communities. The patients were treated according to the In-patient Comprehensive Medical Rehabilitation - A team of medical experts providing consumers with therapy, medical care, and other help.
Source of support: Departmental sources
References
- 1.Yeates KO, Swift E, Taylor HG, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10:412–26. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 2.Stancin T, Drotar D, Taylor HG, et al. Health-related quality of life of children and adolescents following traumatic brain injury. Pediatrics [On-line] 2002;109:e34. doi: 10.1542/peds.109.2.e34. [DOI] [PubMed] [Google Scholar]
- 3.Pąchalska M. Neuropsychologia kliniczna: urazy mózgu. [Clinical Neuropsychology: Brain injuries]. Warszawa: Wydawnictwo Naukowe PWN; 2007. [in Polish] [Google Scholar]
- 4.Rubin KH, Bukowski W, Parker J. Peer interactions, relationships, and groups. In: Eisenberg N, editor. Handbook of child psychology: Social, emotional, and personality development. 5th ed. New York: Wiley; 1998. pp. 619–700. [Google Scholar]
- 5.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1998;29:540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 6.Buliski L. Social reintegration of TBI patients: A solution to provide long-term support. Med Sci Monit. 2010;16(11):PH14–23. [PubMed] [Google Scholar]
- 7.Pąchalska M. Rehabilitacja neuropsychologiczna. [Neuropsychological Rehabilitation]. Lublin: Wydawnictwo UMCS; 2008. [in Polish] [Google Scholar]
- 8.Judd FK, Burrows GD. Liaison psychiatry in a spinal injuries unit. Paraplegia. 1986;24:6–19. doi: 10.1038/sc.1986.3. [DOI] [PubMed] [Google Scholar]
- 9.Stensman R. Adjustment to traumatic spinal cord injury. A longitudinal study of self-reported quality of life. Paraplegia. 1994;32:416–22. doi: 10.1038/sc.1994.68. [DOI] [PubMed] [Google Scholar]
- 10.Adolphs R. The neurobiology of social cognition. Curr Opin Neurobiol. 2001;11:231–39. doi: 10.1016/s0959-4388(00)00202-6. [DOI] [PubMed] [Google Scholar]
- 11.Grady CL, Keightley ML. Studies of altered social cognition in neuropsychiatric disorders using functional neuroimaging. Can J Psychiatry. 2002;47:327–36. doi: 10.1177/070674370204700403. [DOI] [PubMed] [Google Scholar]
- 12.Rosenthal M, Christensen BK, Thomas PR. Depression following traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 1998;79:90–103. doi: 10.1016/s0003-9993(98)90215-5. [DOI] [PubMed] [Google Scholar]
- 13.Sintonen H, Pekurinen M. A fifteen-dimensional measure of health-related quality of life (15D) and its applications. In: Walker S, Roser R, editors. Quality of Life assessment Key issues in the 1990s. Dordrecht: Kluwer Academic Publishers; 1993. pp. 185–95. [Google Scholar]
- 14.Snowdy HA, Jr, Snowdy PH. Stabilization procedures in the patients with acute spinal cord injury. Critical Care Clinic. 1992;3(3):449–62. [PubMed] [Google Scholar]
- 15.Taylor-Sarno M. Quality of life in the first post-stroke year. Aphasiology. 1997;11:665–79. [Google Scholar]
- 16.Bulpitt CJ. Quality of life as an outcome measure. Postgrad Med J. 1997;73:613–16. doi: 10.1136/pgmj.73.864.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craig A, Hancock K, Dickson H. Improving the long-term adjustment of spinal cord injured persons. Spinal Cord. 1999;37:345–50. doi: 10.1038/sj.sc.3100829. [DOI] [PubMed] [Google Scholar]
- 18.Curcoll ML. Psychological approach to the rehabilitation of the spinal cord injured: the contribution of relaxation techniques. Paraplegia. 1992;30:425–27. doi: 10.1038/sc.1992.93. [DOI] [PubMed] [Google Scholar]
- 19.Vaidyananthan S, Soni BM, Brown E, et al. Effect of intermittent urethral catheterization and oxybutynin bladder installation on urinary continence status and quality of life in a selected group of spinal cord injury patients with neuropathic bladder dysfunction. Spinal Cord. 1998;36:409–14. doi: 10.1038/sj.sc.3100573. [DOI] [PubMed] [Google Scholar]
- 20.Sapountzi-Krepia D, Soumilas A, Papadakis N, et al. Post-traumatic paraplegics living in Athens. The impact of pressure sores and UTIs on everyday life activities. Spinal Cord. 1998;36:432–37. doi: 10.1038/sj.sc.3100641. [DOI] [PubMed] [Google Scholar]
- 21.Clayton K, Chubob R. Factors associated with the quality of life of long-term spinal cord injured persons. Arch Phys Med Rehabil. 1994;75:633–38. doi: 10.1016/0003-9993(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 22.Dennis RE, Williams W, Giangreco MF, Cloninger CJ. Quality of life as a context for planning and evaluation of services for people with disabilities. Exceptional Children. 1993;59:499–512. doi: 10.1177/001440299305900603. [DOI] [PubMed] [Google Scholar]
- 23.Kannisto M, Merikanto J, Alaranta H, et al. Comparison of health-related quality of life in three subgroups of spinal cord injury patients. Spinal Cord. 1998;36:193–99. doi: 10.1038/sj.sc.3100543. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy P, Hamilton LR. The needs assessment checklist. A clinical approach to measuring outcome. Spinal Cord. 1999;37:136–39. doi: 10.1038/sj.sc.3100745. [DOI] [PubMed] [Google Scholar]
- 25.Pruitt SD, Wahlgren DR, Epping-Jordan JE, Rossi AL. Health behaviour in persons with spinal cord injury. Development and initial validation of an outcome measure. Spinal Cord. 1998;36:724–31. doi: 10.1038/sj.sc.3100649. [DOI] [PubMed] [Google Scholar]
- 26.Firsching R. Moral dilemmas of tetraplegia, the “locked-in” syndrome, the persistent vegetative state and brain death. Spinal Cord. 1998;36:741–43. doi: 10.1038/sj.sc.3100713. [DOI] [PubMed] [Google Scholar]
- 27.MacQueen BD, Pąchalska M. Zaburzenia porozumiewania się u chorych po urazach czaszkowo-mózgowych. In: Herzyk A, Daniluk B, Pąchalska M, MacQueen BD, editors. Neuropsychologiczne konsekwencje urazów głowy Jakość życia pacjentów. [Neuropsychological consequences of head injuries Quality of life of patients]. Lublin: Wydawnictwo UMCS; 2003. pp. 99–118. [in Polish] [Google Scholar]
- 28.MacQueen BD, Pąchalska M, Łukowicz M, Pufal A. Ocena funkcji wykonawczych u sportowców po urazach czaszkowo-mózgowych. [Assessment of executive functions in athletes after cranio-cerebral trauma]. Ortopedia Traumatologia Rehabilitacja. 2003;5(6):797–811. [in Polish] [PubMed] [Google Scholar]
- 29.MacQueen BD, Talar J, Ossowski R. Dylematy etyczno-moralne w terapii pacjentów z zespołem pourazowego uszkodzenia pnia mózgu. In: Talar J, editor. Urazy pnia mózgu Kompleksowa diagnostyka i terapia. [Injuries to the brain stem Comprehensive diagnostics and therapy]. Bydgoszcz: Katedra i Klinika Rehabilitacji AMB; 2002. pp. 328–60. [in Polish] [Google Scholar]
- 30.Pąchalska M, Baranowski P, MacQueen BD, Knapik H. Ocena rehabilitacji neuropsychologicznej chorych z wysokimi urazami rdzenia oraz uszkodzeniem mózgu. [Assessment of neuropsychological rehabilitation of patients with high spinal injuries and brain damage]. Ortopedia Traumatologia Rehabilitacja. 2000;2:44–49. [in Polish] [PubMed] [Google Scholar]
- 31.Pąchalska M, Baranowski P, Fraczuk B, et al. Zaburzenia funkcji poznawczych i emocjonalnych u chorych po urazach typu „whiplash”. [Disorders of cognitive and emotional functions in patients after a “whiplash” trauma]. Ortopedia Traumatologia Rehabilitacja. 2000;3:34–38. [in Polish] [PubMed] [Google Scholar]
- 32.Pąchalska M, MacQueen BD. How to measure HR-QOL. Video presented during the session of 28th Congress of the International Medical Society for Paraplegia IMSOP; Innsbruck. 7–9.05.1997. [Google Scholar]
- 33.Pąchalska M, MacQueen BD. Skala Oceny Jakości Życia Pacjentów po Urazach Czaszkowo-Mózgowych. [Quality of Life Rating Scale in Cranio-Cerebral Trauma Patients]. Kraków: Fundacja na Rzecz Osób z Dysfunkcjami Mózgu; 1998. [in Polish] [Google Scholar]
- 34.Grochmal-Bach B. Somatoterapia – a wartości noetyczne zwizane z cierpieniem. [Somatic therapy – and the bioethical values associated with suffering]. Sztuka Leczenia. 1996;2:95–100. [in Polish] [Google Scholar]
- 35.Pąchalska M, Talar J, Fraczuk B, et al. Rehabilitacja zaburze funkcji wykonawczych u pacjentów z pourazowymi uszkodzeniami mózgu. [Rehabilitation of executive dysfunction in patients with posttraumatic brain injuries]. Ortopedia Traumatologia Rehabilitacja. 2001;2(4):182–86. [in Polish] [Google Scholar]
- 36.Pąchalska M, Talar J, Fraczuk B, et al. Strategiczne podejście do rehabilitacji osób z wysokimi urazami rdzenia kręgowego. [A strategic approach to rehabilitation of people with high spinal cord injuries]. Ortopedia Traumatologia Rehabilitacja. 2001;3(1):89–99. [PubMed] [Google Scholar]
- 37.Talar J, Pąchalska M, Łukowicz M, et al. Etapowy program leczenia i rehabilitacji pacjentów z zespołem pourazowego uszkodzenia pnia mózgu. In: Talar J, editor. Urazy pnia mózgu Kompleksowa diagnostyka i terapia. [Injuries to the brain stem Comprehensive diagnostics and therapy]. Bydgoszcz: Department and Clinic of Rehabilitation at AMB; 2002. pp. 207–80. [in Polish] [Google Scholar]
- 38.Taylor HG, Yeates KO, Wade SL, et al. A prospective study of short – and longterm outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 39.Baranowski P. Zastosowanie Międzynarodowych Standardów Neurologicznej i Funkcjonalnej Klasyfikacji Urazów Rdzenia Kręgowego (Skala ASIA) [Application of the International Standards of Neurological and Functional Classification of Spinal Cord Injuries (ASIA scale)]. Ortopedia Traumatologia Rehabilitacja. 2000;2:31–34. [in Polish] [PubMed] [Google Scholar]
- 40.Mako G. Ocena skuteczności sterowanego planem strategicznym programu rehabilitacji chorych po stłuczeniu pnia mózgu w zakresie jakości życia. [Assessment of the effectiveness of the rehabilitation program controlled by a strategic plan for patients after brain stem contusion in terms of quality of life]. Kraków: Fundacja na Rzecz Osób z Dysfunkcjami Mózgu; 2004. [in Polish] [Google Scholar]