Summary
Background
To assess the relations between albuminuria and selected cardiovascular risk factors.
Material/Methods
The study population comprised 200 apparently healthy soldiers aged 28.8±8.1, observed for 36 months.
Results
Albuminuria was revealed in 9% of the studied group at the beginning of the study and in 12.7% at the end of the observation. Albumins increased from 97.0±61.0 mg/24 hours to 165.0±25.7 mg/24 hours after 36 months of observation. The increase of diastolic blood pressure, body mass, C-reactive protein (CRP), and low-density lipoprotein (LDL) was found in the “albuminuria subgroup” after 3 years of observation. This subgroup also presented significantly higher homocysteine and CRP serum concentrations in comparison with the “non-albuminuria group” in the first phase of the study and after 3 years of follow-up.
Conclusions
Albuminuria was found to be a relatively frequent and persistent abnormality in the studied group. The study demonstrated the relationship between the occurrence and the severity of albuminuria and selected biochemical and demographic cardiovascular risk factors. Determination of albuminuria is a useful, early marker of cardiovascular risk in young male professional soldiers.
Keywords: albuminuria, hyperhomocysteinemia, cardiovascular risk factors
Background
Albuminuria, defined as presence of albumins with a value between 30 mg and 300 mg/24 hours or as urinary albumin-to-creatinine ratio >30 mg/g, is recognized as an independent cardiovascular risk factor [1,2].
The prevalence of albuminuria is 5–7% in the general population and it occurs in up to 40% of patients with hypertension or diabetes [3,4]. Population studies indicate that male sex, smoking, low-high density lipoproteins (HDL) concentration, diabetes, and age are confirmed cardiovascular risk factors and correlate with the prevalence of incidental albuminuria in the general population [5].
Multicenter population studies show that albuminuria has predictive value in apparently healthy individuals [6].
Some data also suggest that albuminuria may be the expression of generalized endothelium dysfunction and induces the vascular inflammatory process and subsequent atherosclerosis [7].
Hyperhomocysteinemia is considered as an independent cardiovascular risk factor that is especially linked to atherosclerotic coronary disease, as well as cerebral and renal vessel disease. The CoLaus Study, which focused on metabolic syndrome and included 5913 residents of Lozanna, Poland, revealed a correlation of hyperhomocysteinemia and hyperuricemia with albuminuria, independently of each other. This correlation was also independent of renal function. The study also showed increased risk of albuminuria in people who are MTHFR gene carriers for homocysteine. It may be interpreted as evidence of potential risk of renal damage caused by homocysteine [8].
We also found a study from France in the literature available, which describes the 12-month observation of 2045 male military personnel in Paris and the surrounding area [9]. Albuminuria appeared to be present in many cases of metabolic syndrome.
The data presented above inspired us to perform our own study focused on the long-term assessment of albuminuria in professional soldiers and its potential association with common cardiovascular risk factors.
Material and Methods
The study was carried out in 200 male soldiers aged 28.8±8.1 years from a group of 1000 subjects who met the following criteria: military unit doctor’s opinion that the subject was in good health, and consent to participate in the study.
The study protocol comprised:
– a questionnaire on cardiovascular risk to be completed by the subjects,
– a medical examination,
– blood and urine tests.
The first part of the questionnaire asked for information about health-related habits such as alcohol consumption, smoking, and diet. Recurrent disturbances connected with the use of the above-mentioned factors were recognized as dependency, according to the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders) [10].
The second part of the questionnaire assessed family history of cardiovascular diseases, with special attention to hypertension and diabetes.
The medical examination comprised:
– a routine physical examination with triple blood pressure measurement (on 3 consecutive days under the same conditions),
– anthropometric measurements: body mass and height with the calculation of BMI (Body Mass Index) and WHR (Waist Hip Ratio).
The biochemical blood testing comprised the following parameters:
– sodium and potassium (ion-selective electrode),
– creatinine (buffered kinetic Jaffe reaction method) and calculation of estimated glomerular filtration rate (e-GFR) according to the Cockroft-Gault (C-G) formula,
– urea (kinetic method with urease and glutamate dehydrogenase),
– uric acid and C-reactive protein -CRP (ultrasensitive nephelometric method),
– total cholesterol (enzymatic-colorimetric method with cholesterol esterase),
– fractions of cholesterol: HDL i LDL, apolipoprotein A (ApoA), apolipoprotein B (ApoB) (direct non-precipitating method),
– triglycerides (enzymatic-colorimetric method),
– homocysteine (fluorescence polarization method).
The diagnostic algorithm for albuminuria was carried out as follows:
– after exclusion of the urinary tract infection, the test for albuminuria was performed 3 times (morning micturition, dipstick type test – Micral Test II-Roche),
– if there were 2 positive results, the quantitative albuminuria assessment in diurnal urine was done using kinetic nephelometry ARAY 360; the test was repeated 3 times in 6 months;
– albuminuria of 30–300 mg/24h was recognized as the positive result of the quantitative test [1],
– persons with double-positive results on the quantitative test were included into the group with albuminuria.
The t test for non-related variables was used for the statistical analysis. The Kendall correlation test was employed for the assessment of dependence of cardiovascular risk factors. The value of p<0.5 was interpreted as statistically significant. The statistical analysis also included regression analysis, Kolmogorov-Smirnov test, and U-Mann-Whitney test. The non-parametric variables were assessed using chi2 test. The SPSS 8.0 package was used for the analysis.
Results
The 36-month follow-up evaluation included 180 of 200 soldiers involved in the study. Therefore, further analysis was performed for the group of 180 soldiers. Table 1 shows selected anthropometric parameters and blood pressure values in the studied population at the beginning of the study and after 36 months. Statistically significant differences were found only in the case of BMI and diastolic blood pressure. Table 2 contains data reflecting health-related behavior in the studied group.
Table 1.
Selected anthropometric parameters and blood pressure values in the studied population at the beginning of the study and after 36 months.
| Parameter | Studied group (180 persons) I stage X̄±SD | Studied group (180 persons) II stage – after 36 months X̄±SD | Statistical significance |
|---|---|---|---|
| Body Mass Index | 25.7±3.2 | 26.4±3.1 | p<0.05 |
| WHR | 0.92± 0.07 | 0.91±0.05 | p≥0.05 |
| Systolic blood pressure (mmHg) | 128.4±13.2 | 124.9±12.5 | p≥0.05 |
| Diastolic blood pressure (mmHg) | 78.6±8.7 | 84.4±7.9 | p<0.0001 |
Table 2.
Assessment of health-related behavior in the studied group.
| Parameter | Studied group (180 persons) I stage | Studied group (180 persons) II stage – after 36 months | Statistical significance |
|---|---|---|---|
| Alcohol abuse | 64 | 18 | p<0.05 |
| Nicotine dependence | 40 | 18 | p<0.05 |
| Low-cholesterol diet | 38 | 143 | p<0.05 |
Data in Table 2 confirm the improvement of health-related behavior of military personnel in the study group. The more restrictive health policy, apparently related to the restructuring of the Polish Armed Forces and associated redundancies, which took place during the study period, may be the potential reasons for this improvement.
The study group had normal values for serum sodium concentration, potassium, glucose, creatinine, and urea. According to the Cockroft-Gault equation, creatinine clearance values (e-GFR) were 124 ml/min/1.73 m2 at the beginning of the observation and 132.6 ml/min/1.73 m2 after 36 months. The mean values of serum uric acid, CRP, total cholesterol, HDL and LDL fractions of cholesterol, ApoA, ApoB, triglycerides, and homocysteine were normal. Albuminuria was found in 18 persons in stage I of observation (9%) and in another 5 persons in stage II – in total, 23 persons (12.7%). This group contained all people with albuminuria revealed in stage I of observation.
A statistically significant increase of albuminuria was found in the albuminuria subgroup after 36 months of observation. Moreover, the values of diastolic blood pressure, body mass, and generally recognized cardiovascular risk factors such as LDL concentration and CRP were statistically higher after 36 months (Table 3).
Table 3.
Selected parameters in the albuminuria subgroup at the beginning of the study and after 36 months of observation.
| Parameter | Albuminuria subgroup stage I (n= 18) X̄±SD | Albuminuria subgroup stage II – after 36 months (n= 23) X̄±SD | Statistical significance |
|---|---|---|---|
| Albuminuria (mg/24 hours) | 97.0±61.0 | 165.0±25.7 | p<0.05 |
| Diastolic blood pressure (mmHg) | 76.6±7.5 | 84.4±9.2 | p<0.05 |
| Body mass (kg) | 80.2±9.6 | 82.3±13.8 | p<0.05 |
| CRP (mg/dl) | 0.24±0.1 | 0.4±0.6 | p<0.05 |
| LDL (mg/dl) | 113.58± 37.47 | 123.3±31.5 | p<0.05 |
The Kendall test was used to assess correlations in the group of soldiers with albuminuria. The test is useful for assessment of small groups characterized by different values of analyzed parameters. In stage I, there were significant correlations between albuminuria and other factors: age (p<0.001), body mass (p<0.008), total cholesterol serum concentration (p<0.001), LDL cholesterol fraction concentration (p<0.001), and homocysteine (p<0.002).
The significance test of the regression analysis model revealed that LDL cholesterol fraction and age predicted occurrence of albuminuria (R2=0.709; F2,13=19.312; p<0.001). The strength of association between LDL, age, and albuminuria was expressed as the coefficient β and was 0.048 and 0.047, respectively (statistically significant values). This means that the probability of occurrence of albuminuria in men aged 28.7±8.1 years with LDL plasma concentration of 113±37 mg/dl is statistically significant. The significant relationships between albuminuria and age, as well as albuminuria and body mass, were found in the II stage of the study. The positive correlation between CRP and albuminuria (p<0.06; π=0.20) and negative correlation between albuminuria and ApoB concentration (p<0.06; π=0.19) were observed. Both correlations were close to statistical significance.
Table 4 presents selected parameters in the non-albuminuria subgroup (157 soldiers) at the beginning of the study and after 36 months of observation. Significant changes of blood pressure, ApoB, and homocysteine concentrations in the II stage of the study were also found. The systolic blood pressure and homocysteine concentration decreased, whereas the ApoB increased after 3 years of observation.
Table 4.
Selected parameters in the non-albuminuria subgroup at the beginning of the study and after 36 months of observation.
| Parameter | Non-albuminuria subgroup – stage I (n=157) X̄±SD | Non-albuminuria subgroup – stage II (after 36 months) (n=157) X̄±SD | Statistical significance |
|---|---|---|---|
| Systolic blood pressure (mmHg) | 128.4±13.2 | 123.4±10.6 | p<0.05 |
| ApoB (mg/dl) | 0.99 ±0.86 | 1.1±0.4 | p<0.05 |
| HCY (μmol/l) | 11.6±4.1 | 11.4±3.3 | p<0.05 |
The next step in the statistical analysis was comparison of mean values of atherosclerosis risk factors between the albuminuria subgroup and the non-albuminuria subgroup at the beginning of the study and after 36 months of observation.
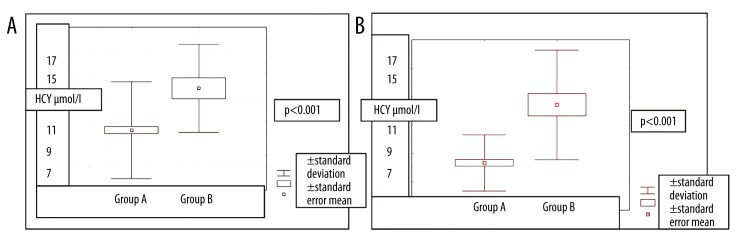
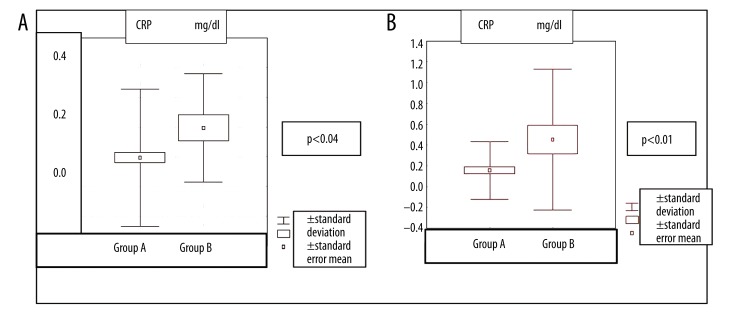
Homocysteine and CRP levels at the beginning of the study and after 36 months of the observation were significantly higher in the albuminuria subgroup than in the non-albuminuria subgroup (Figures 1, 2).
Figure 1.
The homocystein values in the group with albuminuria (A) in comparision to the group without albuminuria (B) at the beginning and after 36 months of the study.
Figure 2.
The CRP values in the group with albuminuria (A) in comparision to the group without albuminuria (B) at the beginning and after 36 months of the study.
With respect to the charts of CRP for groups A and B, although the chart is mathematically (statistically) correct, physiological values of CRP are always greater than zero.
The HDL cholesterol fraction and ApoA concentration were significantly lower in the albuminuria subgroup at the beginning of the study, but this was not the case after 36 months of observation.
The results of the questionnaire did not reveal any important differences in health-related behavior or family history of cardiovascular diseases between the albuminuria subgroup and non-albuminuria subgroup.
Discussion
We found that albuminuria was a relatively frequent and persistent abnormality in young and apparently healthy soldiers. After 36 months of observation it was confirmed in all 18 individuals (9% of the studied group) who demonstrated albuminuria in stage I of the study and in 5 more soldiers in whom albuminuria had not been observed at the beginning of the observation. Therefore, the albuminuria subgroup finally comprised 23 persons (12.7% of the observed population). The significant increase of albuminuria, correlating with cardiovascular risk factors such as diastolic blood pressure, CRP, and BMI was revealed throughout the 36-month observation in this subgroup. These unsatisfactory findings were observed despite the beneficial role of the health-related actions that been introduced in the whole study group (Table 2).
In the EPIMIL study (epidemiology of metabolic syndrome in 2045 French military personnel) of male military staff in the Paris area, aged 38.6±8.8 years, albuminuria was significantly more frequent in the group of 185 men (9% of the studied population) with metabolic syndrome in comparison to the remaining group of 1860 persons. The authors of the EPIMIL study used metabolic syndrome criteria according to the NCEP ATP III classification [9]. The significantly higher values of LDL cholesterol, albuminuria, and CRP were found in the group with metabolic syndrome compared to the group without metabolic syndrome. Contrary to our findings, the EPIMIL study did not reveal any differences in homocysteine level between groups with and without metabolic syndrome.
According to the results of the Polish PolNef study, which included 2471 persons aged 18 to 98 years from the general population of northern Poland, albuminuria was diagnosed (using dipstick test for albuminuria and chemical turbidimetric method) in 11.9%. In the subgroup of young males (age similar to our population), albuminuria was found in 8.9% [11].
Our study showed a significant correlation between albuminuria and homocysteinemia. In the albuminuria subgroup, the homocysteine concentration was higher than in the non-albuminuria subgroup, at the beginning of the study as well as after 36 months. Additionally, in the albuminuria subgroup, homocysteine concentration after 36 months was higher than at the beginning of the study. However, this trend was statistically non-significant.
The CoLaus study, comprising 5913 inhabitants of Lozanna, aged 35–37 years, including 2744 Caucasian men, showed that hyperhomocysteinemia (defined as serum homocysteine concentration >15 μmol/l) correlated significantly with albuminuria [8].
Our study showed an interesting correlation between albuminuria and demographic cardiovascular risk factors such as BMI and diastolic blood pressure (p<0.05). Similar to the EPIMIL study, we did not confirm the influence of nicotine dependence or alcohol abuse on the occurrence of albuminuria. However, unlike the EPIMIL study, we did not find an influence of family cardiovascular risk history on the occurrence of albuminuria. The persistence of, or even increase in, albuminuria in soldiers tested during the 36-month follow-up could be associated with an increase in diastolic blood pressure and BMI, which might result from the insufficient effect of health-related actions and the fact that the observation period was shorter than in other population studies [12,13].
Conclusions
Albuminuria has been revealed as a relatively frequent and persistent abnormality in young and apparently healthy soldiers. The demonstrated relationships between albuminuria and selected biochemical and demographic cardiovascular risk factors indicate that albuminuria is a useful early marker of cardiovascular risk in young male professional soldiers.
Footnotes
Source of support: Departmental sources
References
- 1.Singh A, Satchell SC. Microalbuminuria: causes and implications. Pediatr Nephrol. 2011;26:1957–65. doi: 10.1007/s00467-011-1777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levey AS, de Jong PE, Coresh J, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80(1):17–28. doi: 10.1038/ki.2010.483. [DOI] [PubMed] [Google Scholar]
- 3.Jones CA, Francis ME, Eberhardt MS, et al. Microalbuminuria In the US population: Third National Heath and Nutrition Examination Survey. Am J Kidney Dis. 2002;39(3):445–59. doi: 10.1053/ajkd.2002.31388. [DOI] [PubMed] [Google Scholar]
- 4.Young BA, Katon WJ, von Korff M, et al. Racial and ethnic differences in microalbuminuria prevalence in a diabetes population: the pathways study. J Am Soc Nephrol. 2005;16(1):219–28. doi: 10.1681/ASN.2004030162. [DOI] [PubMed] [Google Scholar]
- 5.O’Seaghdha CM, Hwang S-J, Upadhyay A, et al. Predictors of incydent albuminuria In the Framingham Offspring Kohort. Am J Kidney Dis. 2010;56(5):852–60. doi: 10.1053/j.ajkd.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agewall S, Björn F. Microalbuminuria and intima-media thickness of the carotid artery in clinically healthy men. Atherosclerosis. 2002;164(1):161–66. doi: 10.1016/s0021-9150(02)00056-4. [DOI] [PubMed] [Google Scholar]
- 7.Ritz E. Renal dysfunction as a novel risk factor; Microalbuminuria and cardiovascular risk. Kidney Int. 2005;67:25–28. doi: 10.1111/j.1523-1755.2005.09306.x. [DOI] [PubMed] [Google Scholar]
- 8.Marti F, Vollenweider P, Marques-Vidal PM, et al. Hyperchomocysteinemia is independently associated with albuminuria In the population-based CoLaus study. BMC Public Health. 2011;26(11):733–43. doi: 10.1186/1471-2458-11-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bauduceau B, Baigts F, Bordier L. Epidemiology of the metabolic syndrome in 2045 French military personnel (EPIMIL study) Diabetes Metab. 2005;31(4):353–59. doi: 10.1016/s1262-3636(07)70204-5. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and Statistical Manual Disorders. IV. Washington (DC): American Psychiatric Association; 1994. [Google Scholar]
- 11.Król E, Rutkowski B, Czarniak P, et al. Early Detection of Chronic Kidney Disease: Results of the PolNef Study. Am J Nephrol. 2009;29(3):264–73. doi: 10.1159/000158526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fox CS, Gona P, Larson MG, et al. A multi-marker approach to predict incident CKD and microalbuminuria. J Am Soc Nephrol. 2010;21(12):2143–49. doi: 10.1681/ASN.2010010085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Seaghdha CM, Hwang S-J, Upadhyay A, et al. Predictors of Incident Albuminuria in the Framingham Offspring Cohort. Am J Kidney Dis. 2010;56(5):852–60. doi: 10.1053/j.ajkd.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]