Summary
Unreamed Intramedullary nailing and external fixation are 2 major treatments widely used in Gustilo grade III open tibial fractures, but the difference in effectiveness and complication remains controversial. We retrieved original publications of comparative studies from medical literature databases and selected 9 of them for a meta-analysis. Observation items include malunion and deep infection rate, non-union and comparison of time to union. The analysis showed a lower malunion rate using unreamed intramedullary nailing than external fixation. No significant differences were revealed in deep infection/nonunion rate and time to union. More studies of larger scale and better design are needed to reach an ultimate and definite conclusion.
Keywords: open tibial fractures, unreamed, intramedullary nailing, external fixator, meta-analysis
Background
Multiple and combined injuries, which frequently occur with the presence of severe open fractures, have always been a troublesome concern for both emergency and traumatic physicians. These fractures often have complicated categories due to complex traumatic mechanism, and management therefore is difficult and challenging. With recent advances in treatment, use of antibiotics, improvement in wound care, drainage and surgery skill [1], the aim in severe open fracture treatment has moved from the “era of limb preservation” to the “era of the preservation of function” (Tscherne, 1984). But controversies still remain regarding some therapeutic issues.
Currently there are 2 major surgical therapies for open tibial fractures. Intramedullary nailing allows earlier extremity weight loading and less stress shielding, [2] which can result in better fracture union. External fixation also is popular because of its easy application and economy, while pin site complications such as infection may be major hazards to consider and to prevent [3]. External fixation is usually recommended more for severe open fractures, and it is more successful in superficial bones such as the tibia [4].
Epidemiology research on tibial fractures in Asian populations has shown a consistent ratio of more than a third for open fractures, and most of these fractures are comminuted ones [5]. Gustilo grading for open tibial fracture is defined according to the soft tissue coverage, contamination of the fracture site, fracture complexity and major vascular injuries, etc [6]. External fixation is frequently used within this category because internal fixation methods may need more exposure of the wound site and therefore increase the risk of further contamination. However, with use of systemic antibiotics and better avoidance of bone gap [7] many clinicians also prefer unreamed intramedullary nailing, which provides a relatively more rigid fixation and better bone union efficacy with less bone cavity exposure and less bone marrow related complications [8].
We assessed the results of comparative studies and controlled trials designed to determine the therapeutic effects of the 2 different methods. The following items were observed in our analysis: the mean time to union, wound infection, nonunion and malunion rates of both groups. As the choice of these 2 methods remained inconsistent, our purpose was to better define their advantages and disadvantages, and thereby enabling better decision making.
Literature Search
A study protocol was developed in our study in order to define the analysis, consisting of a discreet search strategy, the establishment of precise trial inclusion criteria, and a standardized, objective data extraction process. No concerns on ethical topics were generated, and no conflict of interest had been reported within this analysis.
We searched the Pub Med, the Cochrane Library, EMBASE, MEDLINE, CNKI and Springer databases to find relevant citations for our study, published between 1986 and 2010. A search strategy was used to identify relevant articles for inclusion in the meta-analysis. We used the following MeSH terms: tibial fractures, open fractures (classification as subheading), intramedullary nailings, and external fixators. The set of search terms must be arranged so as to include all possible combinations. When needed, query formulations are applied to identify a specific term (eg, tibial OR tibia, fracture OR fractures, nailing OR nail OR nails, fixator OR fixation OR fixators). The attributive “unreamed” is not constricted before the term “intramedullary nailings” and thus increases the sensitivity of research. Terms were exploded whenever needed within those databases. We also reviewed the bibliographies from citations for relevant articles. Correspondence with active researchers in the field was also performed.
We also hand searched conference proceedings from meetings on traumatic orthopedics and fractures in the past 10 years and some journals in orthopedics, including Journal of Bone and Joint Surgery, Journal of Orthopaedic Trauma, Injury, etc. We read the meta-analyses that had been done in relevant fields and retrieved the possibly eligible articles that were cited within those articles.
Selection Criteria
We have included articles based on the following criteria: (i) prospective, randomized or case-control or cohort studies investigating the difference between intramedullary nailing and external fixator for Grade III open tibial fractures; (ii) external fixation methods refer to any fixation method needing an external fixator, and internal fixation methods are restricted as unreamed intramedullary tibial nailing, because it is widely used in severe open fractures for its minimal bone cavity exposure and smaller incidence of embolism [9], and a reportedly better effect for bone formation than reamed methods [10]; (iii) diagnostic criteria for the specific type of open tibial fracture: the definition of Grade III was rigorously applied as stated by Gustilo et al. as follows [11]: any segmental fractures with displacement of bones, or diaphyseal segmental loss; fractures with associated vascular injury requiring repair; any high-velocity gunshot wound or injury caused by crushing force from fast moving vehicles; (iv) outcomes of our special interest must be included in the article (eg, time to union, rate of malunion and nonunion, rate of deep infection). Reported outcome measures must be with odds ratio (OR) or relative risk (RR) with 95% confidence interval. For continuous variables, outcome for each group must include an average with standard deviation. When lack of data occurs, a remedy measure had to be applied. All potentially relevant papers were reviewed and extracted independently by 2 investigators (Xiao Fang and Liangyu Zhao), and disagreements were resolved by discussion and consensus.
Assessment of Study Methodological Qualities
As many of the studies included in this meta-analysis were retrospective or did not meet the full requirement of randomization, there is not a precise scale for the assessment of study quality. The quality of the included comparative studies was evaluated with the tool recommended in the Cochrane Handbook (version 5.1.0, updated March 2011) as “The Cochrane Collaboration’s tool for assessing risk of bias”. This scale includes 6 specific domains as major concerns – sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other sources of bias. The quality-assessing details of the studies were listed in Table 1.
Table 1.
Methodological assessment of the included articles for the analysis using the Cochrane Collaboration’s tool for assessing risk of bias.
| Reference | Sources of risk of bias | |||||
|---|---|---|---|---|---|---|
| Adequate sequence generation | Allocation concealment | Blinding of participants, personnel and outcome assessors | Incomplete outcome data | Selective outcome reporting | Other | |
| Holbrook 1989 | No | Unclear | Yes | Yes | Yes | No |
| Whitelaw 1990 | No | Unclear | Yes | Yes | Yes | No |
| Tornetta 1993 | No | Unclear | Yes | Yes | Yes | No |
| Tu 1995 | No | Unclear | Yes | Yes | Yes | No |
| Schandelmaier 1997 | No | Unclear | Yes | Yes | Yes | No |
| Alberts 1999 | No | Unclear | Yes | Yes | Yes | No |
| Jiang 2000 | No | Unclear | Yes | Yes | Yes | No |
| Shannon 2002 | No | Unclear | Yes | Yes | Yes | No |
| Fan 2004 | No | Unclear | Yes | Yes | Yes | No |
| Kaftandziev 2006 | No | Unclear | Yes | Yes | Yes | No |
| Inan 2007 | No | Unclear | Yes | No | Yes | No |
| Rohde 2007 | No | Unclear | Yes | Yes | Yes | No |
Statistical Analysis
Review Manager 5 (Version 5 for Windows, Cochrane Collaboration, Oxford, UK) was used for all statistical analysis. This software was used to estimate the pooled rates and means of all the statistics using fixed effect models or random effects models, depending on the test of heterogeneity, which is determined by the calculation of I2 using that software. None of the selected studies included in this analysis showed any significance in population heterogeneity, as the I2 values showed that the heterogeneity of each study rarely contributed to the data’s inconsistency. However, care must be taken when those statistics were used to judge the significance. In Inan’s study [12], the result of “time to union” is apparently different from those of the other articles, which favored the use of external fixation, with a small standard derivation and statistical significance. Thus a random effects model was used in spite of the I2 value less than 75% (29%, Chi2=2.82), to gain a more conservative and thus more confident result.
For dichotomous variables, we listed individual and pooled statistics as odds ratio with 95% confidence intervals. For continuous data as time to union, we pooled the weighted mean time to union with associated 95% confidence intervals, and also listed the individual means and standard deviations. As for Inan’s study [12] which mentioned the mean time to union but did not calculate their standard deviations, we used a special method recommended in the Cochrane Handbook to estimate the standard deviations of both therapeutic groups [13]. The standard deviations extracted through that method are listed in Table 2 in italics. Publication bias was assessed using the funnel plot; the funnel plot was largely symmetric (not shown). This result indicated that publication bias may not have played an important role in the observed effect.
Table 2.
Characteristics of the included papers on intramedullary nailing vs. external fixation for treatment of Grade III open tibial fracture.
| Reference | Treatment | No. of subjects | Comparisons | ||||
|---|---|---|---|---|---|---|---|
| Time to Union | Deep Infection | Malunion | Nonunion | ||||
| Holbrook 1989 | Ender nailing vs. EF | EF | 10 | 7.4 months, 5 delayed | 3 after nailing | – | 1 |
| UTN | 6 | 6.8 months, 1 delayed | 1 | – | 1 | ||
| Whitelaw 1990 | Ender rods vs. EF | EF | 14 | 27.9w, 4 delayed | 1 | 4 | 1 |
| UTN | 6 | 24.6w, 1 delayed | 0 | 2 | 0 | ||
| Tornetta 1993 | UTN vs. EF | EF | 14 | 28.3w, 14–38, 2 delayed | 1 | 2 | 0 |
| UTN | 15 | 23w, 12–30, 2 delayed | 1 | 0 | 0 | ||
| Tu 1995 | UTN vs. EF | EF | 18 | – | 2 | 6 | 5 |
| UTN | 18 | – | 4 | 1 | 3 | ||
| Schandelmaier 1997 | UTN vs. Gotzen Fixator | EF | 15 | 37w ±22, 2 delayed | 1, 1 after alteration | 2 | 1 |
| UTN | 17 | 31w ±14 | 1 | 2 | 0 | ||
| Alberts 1999 | UTN vs. Hoffmann Fixators | EF | 10 | – | 3 | – | – |
| UTN | 17 | – | 1 | – | – | ||
| Jiang 2000 | UTN vs. EF | EF | 17 | 31w, 14–39, P<0.05 | 0 | – | 1 |
| UTN | 16 | 23w, 12–30, 1 delayed | 0 | – | 0 | ||
| Shannon 2002 | UTN vs. EF | EF | 17 | 36.9w ±14.8 | 0 | – | 7 |
| UTN | 13 | 32.8w ±12.3 | 1 | – | 2 | ||
| Fan 2004 | UTN vs. EF | EF | 22 | 30.1w | 1 | 4 | 3 |
| UTN | 34 | 25.6w | 0 | 2 | 0 | ||
| Kaftandziev 2006 | UTN vs. EF | EF | 30 | 38.4w, P<0.001 | 6 | 5 | 4 |
| UTN | 18 | 32.8w | 2 | 2 | 2 | ||
| Inan 2007 | UTN vs. Ilizarov fixator | EF | 32 | 19w ±3.7, P=0.039 | 2 | 7 | 0 |
| UTN | 29 | 21w ±3.7, 3 delayed | 3 | 5 | 1 | ||
| Rohde 2007 | UTN vs. EF | EF | 18 | – | 2 | – | 3 |
| UTN | 20 | – | 5 | – | 8 | ||
UTN – unreamed tibial nails; EF – external fixator.
The Identification of Relevant Studies
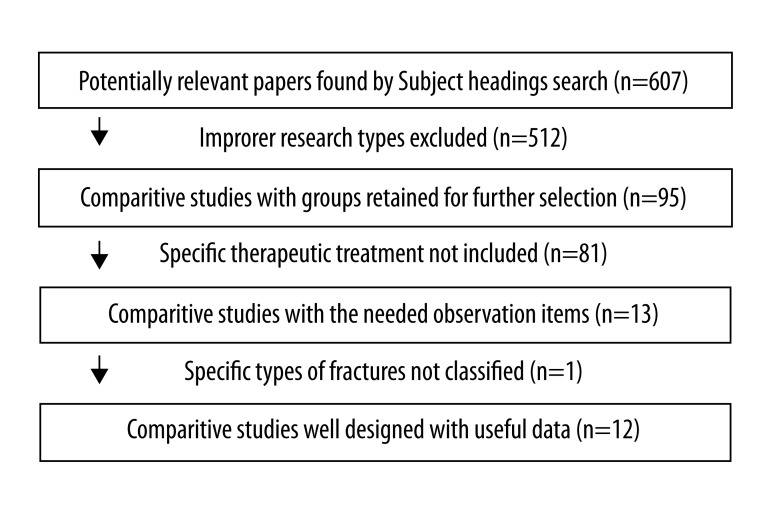
There are altogether 607 articles with the relevant MeSH terms; 512 were excluded for not meeting the proper study types according to criteria (i), 81 were excluded for not meeting the specific therapeutic measures according to criteria (ii), and only 13 articles were considered to be eligible according to criteria (iii) and (iv).
Henley et al. reported a case series of 174 patients who had accepted either unreamed interlocking intramedullary nails or half-pin external fixators, 101 of whom were diagnosed as Gustilo grade III open fractures, but the time to union and nonunion/malunion/deep infection rates were not added up respectively [14]. Thus this article had to be excluded from the meta-analysis, leaving 12 applicable articles.
The entire selection process is shown in a flow diagram (Figure 1).
Figure 1.
Flow diagram of literature retrieval.
All the included studies were comparative research works whose subjects were Ender nailing (Holbrook, Whitelaw) or unreamed interlocking tibial nailing as the intramedullary method [12,15–20], and Ilizarov apparatus (Inan), Gotzen Fixator (Schandelmaier), Hoffman fixators (Alberts) or other kind of “external fixator” as the external fixation method, which may be unilateral, bilateral, or ring-formed [12,21–25]. A summary of these eligible articles is listed in Table 2.
Primary Outcome
After careful consideration a total of 4 observation items were selected as primary outcomes in our analysis.. These items involved either therapeutic or prognostic problems, all of great clinical significance.
Deep infection, including osteomyelitis, was an important observation item because, for both intramedullary nailing and external fixation patients who had a grade III open fracture, further contamination of the deep wound was always the first thing a surgeon endeavors to avoid to prevent amputation or even more severe results. This is especially important for an intramedullary nailing patient, as thorough exposure of the marrow cavity is needed, which may increase the risk of infection.
Malunion is defined as: 1) valgus; 2) varus, both with an angulation of more than 5 degrees in the coronal or sagittal plane; 3) malrotations; and 4) limb length discrepancy, larger than 1.5 centimeters. Malunion acts as a most important outcome among the factors affecting the post-cure quality of life. Nonunion is described as any fracture that was so delayed that a secondary operation was inevitable, or a fracture not healed until 270 days after the operation. Both the malunion status and the definition of nonunion have objective indices to make an exact evaluation (eg, length, time and degree of angle) in such manner as the intra- and inter-observer errors are minimized.
The summary mean time to union was calculated within these articles by using a random effects model, as mentioned above. As some of the articles did not exactly mention that item, or did not detail the full parameters of the time, authors were contacted to get more detailed data, and 3 articles were finally selected for this analysis. Other observation items that encountered the same problem were similarly processed.
In Schandelmaier’s study, 2 bone infection cases was recorded, but 1 of them was described as occurring after the surgery procedure was altered to intramedullary nailing, thus that bone infection case was removed from the external fixation group, leaving 14 overall patients and 1 occurrence. Two malunion cases in Inan’s study were also removed from the unreamed tibial nailing group. The first case occurred because of a technical error at the beginning of the surgeon’s learning curve; the second case was a patient with multiple injuries whose vital signs dramatically worsened, so the operation had to be completed immediately. These were not reflections of the therapeutic effects of the method itself and were therefore not suitable to be included in the analysis.
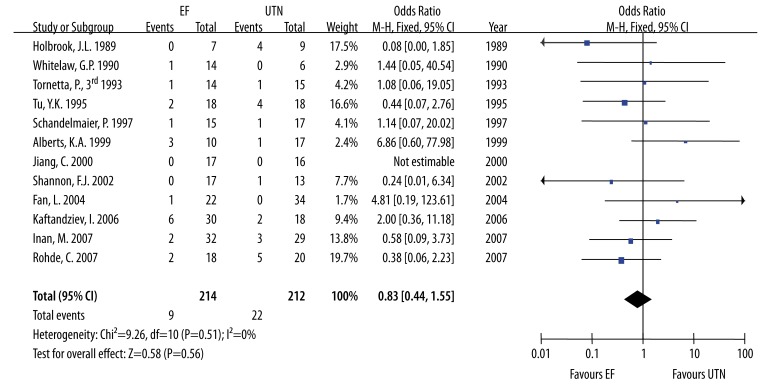
The external fixation group showed a tendency of better results in the pooled odds ratio of deep infection rate compared with the intramedullary nailing group (Figure 2). The pooled odds ratio was 0.83 and 95% confidence interval was 0.44 to 1.55. All 12 studies (n=426, including 33 in Jiang’s study, 2000) reported a deep infection rate, 5 of which favor external fixation and 6 favor intramedullary tibial nailing group, but none had sufficient statistical power. In Jiang’s study, no deep infection cases were observed in both groups until the follow-up survey ended, so it was not possible to estimate its effect on the pooled odds ratio. Effect sizes varied in different studies and no single study alone could show significant statistical difference. The heterogeneity between studies may be not important, as the I2 calculated was 0%.
Figure 2.
Forest plot of deep infection rate.
Similarly, the comparison of malunion rate between both groups was also calculated, and preference for unreamed intramedullary tibial nailing method was inferred from this calculation (odds ratio 2.06, 95% confidence interval 1.05 to 4.06). Indeed, only 7 of the studies (n=282) mentioned and listed malunion incidence. Heterogeneity was non-significant (I2=0%) and a fixed effect model was applied to calculate the pooled odds ratio (Figure 3).
Figure 3.
Forest plot of malunion rate.
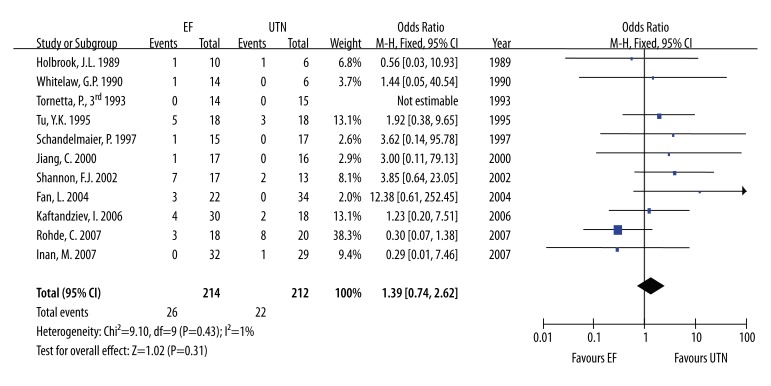
Figure 4 shows no significant difference between the 2 groups in nonunion rate; 11 of the studies (n=399, including 29 in Tornetta’ study, 1993) counted the nonunion cases but Tornetta’s study had observed no nonunion case, the weight of which was therefore not estimated; 3 of those studies had a tendency of the preference for external fixation and 7 potentially favored unreamed tibial nailing. Heterogeneity may not be important (I2=1%).
Figure 4.
Forest plot of nonunion rate.
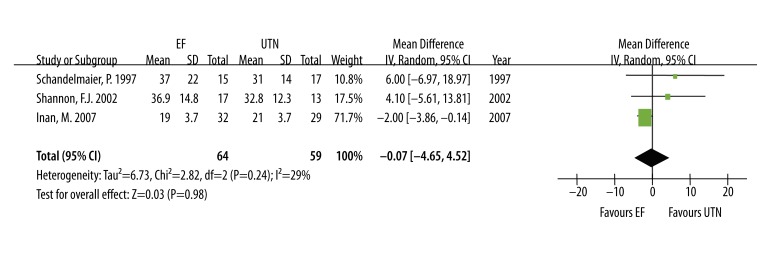
Figure 5 shows no potential tendency of preference for time to union in the external fixation group or in the unreamed intramedullary tibial nailing group, with the 95% confidence interval astride the midline, using a random effects model. Although the heterogeneity test showed no importance (I2=29%, largest within this analysis) within the 3 articles (n=123) that calculated and recorded the mean time to union, inconsistency can still be noticed by looking carefully into those clinical results. Even when a fixed effects model was also applied to evaluate this outcome, the result still showed nonsufficient statistical power (mean difference −1.63, 95%CI −3.44 to 0.18). The estimated results for time to union were almost the same in the external fixation group and in the unreamed intramedullary nailing group (mean difference −0.07, 95%CI −4.65 to 4.52).
Figure 5.
Forest plot of time to union.
In all the studies, no subgroup of different sex, age or race had been divided from the whole population, nor were any differences in sex, age, race or mechanisms of injury reported. The baseline conditions of the subjects were thought to be homogeneous, which ensured the continuity of these results when applying them to the general population.
Discussion
This meta-analysis summarized the available evidence for the use of unreamed intramedullary nailing or external fixators to treat severe open tibial fractures (Gustilo grade III and above). With the use of an exhaustive search strategy and a comprehensive study protocol, the results of 12 comparative clinical studies were pooled to obtain a universal principle in the therapeutic choice. Our analysis obtained a better result from 7 trials for unreamed tibial nailing than external fixation in malunion rate. This result was independent from the other observation items. Beside this, the analysis showed no significant preference in the other 3 observed items. The results suggest that the therapeutic choice is determined by several independent factors which must be considered jointly if a rational decision is to be made.
Deep infection status of patients was recorded in almost all articles included in this analysis, for it is important in prediction of a patient’s prognosis of limb salvage and function reserve [26]. Indeed, both of the 2 therapeutic methods may be affected by either superficial or profound infection (eg, external fixators’ pin site infection, internal fixations’ incision infestation, and extensive wound contaminations which may result in secondary sepsis of all Gustilo grade III open fractures). Making this choice is always a dilemma. Generally, pin site care and prevention of infection is of priority for external fixation patients, which usually manifest a high incidence but low severity [27]. Traditional open reduction and internal fixation methods always need more rigorous infection control measures during the treatment of severe open fractures, as thorough exposure to the fracture site and extensive soft tissue dissection is also needed throughout the operation [28]. Regarding intramedullary nailing, the hazard is even more serious because bone cavity is exposed, which may give rise to osteomyelitis. Besides, the therapeutic efficacy of the antibiotics administered prophylactically during the perioperative period may be diminished with the existence of the implant material such as nails, plates, etc. [29].
Malunion rate of the 2 therapies is the only observation item which gave sufficient statistical evidence to present a difference, whose forest plot showed partiality for intramedullary nailing. For open reduction and internal fixation methods, exact alignment under direct vision is always an inherent advantage compared with external fixation. Malunion rate of intramedullary nailing methods is also controlled at a fairly acceptable level compared with other therapies [30]. The external fixation methods, although having easy application and lower cost, must overcome the difficulties in accurate anatomical reduction and anomaly prevention with a limited exposure of the wound site. Once the healing procedure begins, the final bony healing can be achieved in both groups despite the alignment condition, suggesting that the bone healing could not discriminate between right and wrong for the alignment pattern, and the importance of primary achievement of a good alignment.
The time to union is mainly determined by local blood supply, soft tissue coverage, proper wound care, and systemic nutritional support [31]. Theoretically speaking, open reduction and internal fixation usually achieve more exact alignment, and the deep site of the bone trauma can be debrided more thoroughly, but problems like periosteal damage, excessive removal of adjacent soft tissue, and longer surgery procedure are generally inevitable. A relatively “simple” external fixation procedure may avoid those hazards easily. Therefore the difference of time to union may exist due to these reasons. After all, the time to union may not be the first thing a surgeon considers. Once good alignment and firm restitution are achieved, a slight time delay may also be acceptable.
Limitations
This meta-analysis was an update of many previous ones. The first author who noticed the value of such a systemic review was G. F. Dervin [32]. As no significant result was concluded but a potential was revealed, M. Bhandari et al. summarized the relevant articles once again for a new systemic review, but many controversial issues still remained [33]. As was shown in Table 1, all of the 9 articles included in our meta-analysis did not meet the adequate randomization criteria. The subjects treated in those studies were most commonly allocated based on even/odd patient number, or just the preference of the physician. Many of the articles were designed retrospectively, not prospectively. No allocation concealment measures were taken in all of the studies, but we still believed that lack of complete blinding may not greatly affect the treatment outcome. Biases may derive from the issues mentioned above and may affect the conclusion of a final and fixed, statistically powerful result. So more randomized controlled trials are still in urgent need to gain better experimental design and larger sample size, thus achieve a better result.
We also noticed that in some doctors’ point of view, the more severe a fracture is, the more preference the external fixation method usually gains. That phenomenon was determined by the character of external fixation that it only needs minimum exposure and can therefore dodge possible deep infection. And that idea only comes from doctors’ subjective experience. Indeed, good results of unreamed intramedullary nailing for severe open fractures of the tibia were also reported fairly well [34]. For the articles included in our analysis, we cannot exclude that kind of bias based on the surgeon’s prejudice either. So a detailed stratification and randomized grouping in order to make equal chance of the two methods may be needed to avoid, or decrease such problem at least.
In Shannon’s research, the longest follow up period for nonunion was 32 weeks, 12 weeks the shortest and 20 weeks as an average. After that period of time the patients were altered from external fixation to open reduction and internal fixation, and then gained union. The dilemma of this situation is mainly the short span of follow up period, which cannot support the advantage of intramedullary method or the disadvantage of the external fixation method strong enough. The inclusion or exclusion of this article did not influence the final result of the pooled odds ratio, though. But this also showed a trend that the external fixation was used as a transitional method and intramedullary nailing as a definitive method in many occasions [35,36].
Conclusions
Due to the limitations of the studies and biases of undetermined reasons, this meta-analysis did not give a definitive result of preference for either of the 2 methods except for the malunion rate, which cannot determine the choice of treatment. In fact, without a guideline of the treatment for severe open tibial fracture, alteration of the therapeutic methods was frequently seen in clinical practice [35,37–39]. External fixation might be a temporary solution and an intramedullary nailing fixation method was regarded as an ultimate one. For those who had a primary unreamed intramedullary tibial nail but encountered deep infection that may threaten the limb function and salvage, the external fixation may also be a remedy. The purpose of achieving a consensus for the treatment of Gustilo grade III open tibial fractures was to try to make the primary surgical procedure the best one and avoid reoperation necessitated by nosocomial errors. Use of adjunctive therapies was also reported by some surgeons (eg, surgical suture osteosynthesis, which also gained ideal curative effect) [40]. With discretion, if a surgeon attached the utmost importance to avoiding malunion, then the unreamed tibial nailing may be the first choice, but if the wound is clearly contaminated, the clinical risk of deep infection must be evaluated before internal fixation methods can be applied. A more detailed stratification and classification of the fractures is needed to make the conclusion more precise, as a great difference may exist within the subgroups of Gustilo grade III fractures.
Footnotes
Source of support: Self financing
References
- 1.Melvin JS, et al. Open tibial shaft fractures: I. Evaluation and initial wound management. J Am Acad Orthop Surg. 2010;18(1):10–19. doi: 10.5435/00124635-201001000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Allen JC, Jr, et al. The effect of retained intramedullary nails on tibial bone mineral density. Clin Biomech (Bristol, Avon) 2008;23(6):839–43. doi: 10.1016/j.clinbiomech.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Pieske O, et al. Clinical benefit of hydroxyapatite-coated pins compared with stainless steel pins in external fixation at the wrist: A randomised prospective study. Injury. 2010 doi: 10.1016/j.injury.2010.03.030. [DOI] [PubMed] [Google Scholar]
- 4.Wani N, et al. Role of early Ilizarov ring fixator in the definitive management of type II, IIIA and IIIB open tibial shaft fractures. Int Orthop. 2010;41(10):1031–36. doi: 10.1007/s00264-010-1023-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madadi F, et al. Epidemiology of adult tibial shaft fractures: a 7-year study in a major referral orthopedic center. in Iran Med Sci Monit. 2010;16(5):CR217–21. [PubMed] [Google Scholar]
- 6.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24(8):742–46. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Kakar S, Tornetta P., III Open fractures of the tibia treated by immediate intramedullary tibial nail insertion without reaming: a prospective study. J Orthop Trauma. 2007;21(3):153–57. doi: 10.1097/BOT.0b013e3180336923. [DOI] [PubMed] [Google Scholar]
- 8.Melvin JS, et al. Open tibial shaft fractures: II. Definitive management and limb salvage. J Am Acad Orthop Surg. 2010;18(2):108–17. doi: 10.5435/00124635-201002000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Gray AC, et al. The stress response to bilateral femoral fractures: a comparison of primary intramedullary nailing and external fixation. J Orthop Trauma. 2009;23(2):90–97. doi: 10.1097/BOT.0b013e31819194c6. discussion 98–99. [DOI] [PubMed] [Google Scholar]
- 10.Bhandari M, Schemitsch EH. Bone formation following intramedullary femoral reaming is decreased by indomethacin and antibodies to insulin-like growth factors. J Orthop Trauma. 2002;16(10):717–22. doi: 10.1097/00005131-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Gustilo RB, Gruninger RP, Davis T. Classification of type III (severe) open fractures relative to treatment and results. Orthopedics. 1987;10(12):1781–88. [PubMed] [Google Scholar]
- 12.Inan M, et al. Treatment of type IIIA open fractures of tibial shaft with Ilizarov external fixator versus unreamed tibial nailing. Arch Orthop Trauma Surg. 2007;127(8):617–23. doi: 10.1007/s00402-007-0332-9. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011] The Cochrane Collaboration. 2011;2011 Available from www.cochrane-handbook.org. [Google Scholar]
- 14.Henley MB, et al. Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: a prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma. 1998;12(1):1–7. doi: 10.1097/00005131-199801000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Rohde C, et al. Gustilo grade IIIB tibial fractures requiring microvascular free flaps: external fixation versus intramedullary rod fixation. Ann Plast Surg. 2007;59(1):14–17. doi: 10.1097/SAP.0b013e31803403c8. [DOI] [PubMed] [Google Scholar]
- 16.Shannon FJ, Mullett H, O’Rourke K. Unreamed intramedullary nail versus external fixation in grade III open tibial fractures. J Trauma. 2002;52(4):650–54. doi: 10.1097/00005373-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Tu YK, et al. Unreamed interlocking nail versus external fixator for open type III tibia fractures. J Trauma. 1995;39(2):361–67. doi: 10.1097/00005373-199508000-00029. [DOI] [PubMed] [Google Scholar]
- 18.Tornetta P, III, et al. Treatment of grade-IIIb open tibial fractures. A prospective randomised comparison of external fixation and non-reamed locked nailing. J Bone Joint Surg Br. 1994;76(1):13–19. [PubMed] [Google Scholar]
- 19.Holbrook JL, Swiontkowski MF, Sanders R. Treatment of open fractures of the tibial shaft: Ender nailing versus external fixation. A randomized, prospective comparison. J Bone Joint Surg Am. 1989;71(8):1231–38. [PubMed] [Google Scholar]
- 20.Fan L, et al. Application of unreamed intramedullary nailing and external fixation for Gustilo grade III tibial shaft fracture: A comparative study. J Bone Joint Injury. 2004;19(2):125–27. [Google Scholar]
- 21.Alberts KA, Loohagen G, Einarsdottir H. Open tibial fractures: faster union after unreamed nailing than external fixation. Injury. 1999;30(8):519–23. doi: 10.1016/s0020-1383(99)00143-6. [DOI] [PubMed] [Google Scholar]
- 22.Schandelmaier P, et al. Superior results of tibial rodding versus external fixation in grade 3B fractures. Clin Orthop Relat Res. 1997;(342):164–72. [PubMed] [Google Scholar]
- 23.Whitelaw GP, et al. Ender rods versus external fixation in the treatment of open tibial fractures. Clin Orthop Relat Res. 1990;(253):258–69. [PubMed] [Google Scholar]
- 24.Jiang C, Tang MJ, Shi ZM. Treatment of Open Tibial Fractures: Comparison of Non-reamed Interlocking Intramedullary Nail and External Fixator. China J Orthop & Trauma. 2000;13(1):14–15. [Google Scholar]
- 25.Kaftandziev I, Pejkova S, Saveski J. Operative treatment of III grade open fractures of the tibial diaphysis. Prilozi. 2006;27(1):121–31. [PubMed] [Google Scholar]
- 26.Yokoyama K, et al. Risk factors for deep infection in secondary intramedullary nailing after external fixation for open tibial fractures. Injury. 2006;37(6):554–60. doi: 10.1016/j.injury.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 27.Bibbo C, Brueggeman J. Prevention and management of complications arising from external fixation pin sites. J Foot Ankle Surg. 2010;49(1):87–92. doi: 10.1053/j.jfas.2009.07.026. [DOI] [PubMed] [Google Scholar]
- 28.McCann PA, et al. Complications of definitive open reduction and internal fixation of pilon fractures of the distal tibia. Int Orthop. 2011;35(3):413–18. doi: 10.1007/s00264-010-1005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamel A, et al. Internal device decreases antibiotic’s efficacy on experimental osteomyelitis. J Child Orthop. 2008;2(3):239–43. doi: 10.1007/s11832-008-0102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.el Moumni M, et al. The incidence of non-union following unreamed intramedullary nailing of femoral shaft fractures. Injury. 2009;40(2):205–8. doi: 10.1016/j.injury.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 31.Phieffer LS, Goulet JA. Delayed unions of the tibia. J Bone Joint Surg Am. 2006;88(1):206–16. doi: 10.2106/00004623-200601000-00026. [DOI] [PubMed] [Google Scholar]
- 32.Dervin GF. Skeletal fixation of grade IIIB tibial fractures. The potential of metaanalysis. Clin Orthop Relat Res. 1996;(332):10–15. doi: 10.1097/00003086-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Bhandari M, et al. Treatment of open fractures of the shaft of the tibia. J Bone Joint Surg Br. 2001;83(1):62–68. doi: 10.1302/0301-620x.83b1.10986. [DOI] [PubMed] [Google Scholar]
- 34.Tielinen L, Lindahl JE, Tukiainen EJ. Acute unreamed intramedullary nailing and soft tissue reconstruction with muscle flaps for the treatment of severe open tibial shaft fractures. Injury. 2007;38(8):906–12. doi: 10.1016/j.injury.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 35.Sechriest VF, II, Lhowe DW. Prolonged femoral external fixation after natural disaster: successful late conversion to intramedullary nail aboard the USNS Mercy hospital ship. Am J Disaster Med. 2008;3(5):307–12. [PubMed] [Google Scholar]
- 36.Emara KM, Allam MF. Ilizarov external fixation and then nailing in management of infected nonunions of the tibial shaft. J Trauma. 2008;65(3):685–91. doi: 10.1097/TA.0b013e3181569ecc. [DOI] [PubMed] [Google Scholar]
- 37.Bhandari M, et al. Intramedullary nailing following external fixation in femoral and tibial shaft fractures. J Orthop Trauma. 2005;19(2):140–44. doi: 10.1097/00005131-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 38.Megas P, et al. The treatment of infected nonunion of the tibia following intramedullary nailing by the Ilizarov method. Injury. 2010;41(3):294–99. doi: 10.1016/j.injury.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 39.Taylor KF, McHale KA. Ilizarov external fixation salvage of failed intramedullary fixation of tibia with nail retention. Am J Orthop (Belle Mead NJ) 2004;33(9):461–67. [PubMed] [Google Scholar]
- 40.Gao YS, et al. Stabilizing severely open fractures of the tibia with a surgical suture: an alternative and feasible method for osteosynthesis. Med Sci Monit. 2010;16(11):CS143–47. [PubMed] [Google Scholar]