Abstract
Purpose
Posterior cruciate ligament (PCL) injury has a reported incidence of 3–20 %. PCL reconstruction is aimed at reducing onset of premature articular degeneration and improving function. Numerous operative techniques have been described with varying degrees of result consistency.
Methods
We evaluated 15 patients treated for isolated primary posterior cruciate ligament injury with a mean follow-up of 4.1 years (range one to nine). Post-reconstruction clinical assessment included the Lysholm and Tegner knee scoring scale, international knee documentation committee (IKDC) ligament evaluation, and KT2000 arthrometer assessment.
Results
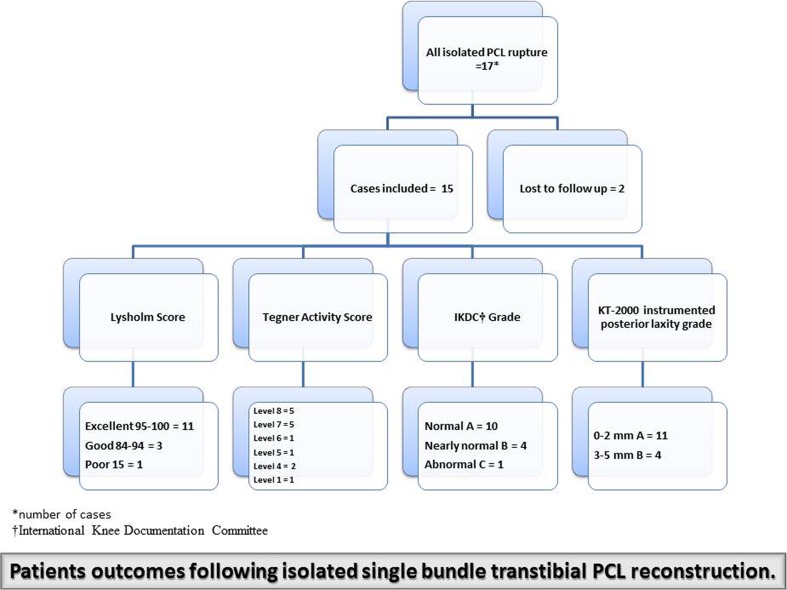
On the Lysholm knee score 11 patients (73 %) had excellent results, three patients (20 %) had good results and one patient (7 %) had a poor result. On the Tegner activity score the majority of patients scored 7–8 with a return to high level sports. At the final follow-up, the post-reconstruction IKDC score was normal or nearly normal (A and B) in 14 (93 %) patients, and abnormal (C) in one (7 %) patient. According to KT-2000 arthrometer measurements at final follow-up review, 11 patients (73 %) were rated as normal (A, 0–2 mm), and four patients (27 %) as nearly normal (B, 3–5 mm). These results were independent of age, mechanism of injury, time elapsed to surgical reconstruction, and length of follow-up.
Conclusions
Despite being a technically demanding procedure, the outcomes reported in this study show that single bundle transtibial arthroscopic PCL repair using four strands hamstring autograft provides satisfactory and consistent functional outcomes.
Introduction
Posterior cruciate ligament (PCL) rupture has a reported incidence between 3 and 20 % [1]. Management of posterior cruciate ligament injuries lags behind that of the anterior cruciate ligament injuries, due to the relative infrequency of these injuries and lack of consensus on treatment protocol [2]. Non-operative treatment has been shown to increase the risk of articular cartilage degeneration and onset of secondary osteoarthroses (OA) [3]. This in turn is associated with poorer functional outcomes [4]. With a debatable retardation in the onset of secondary OA and favourable results obtained with functional non-operative management the most evident advantage of PCL reconstruction is the objective return of good level of function [5]. In selected candidates PCL reconstruction has been shown to yield promising results with up to 80 % return to pre-injury activity levels [6]. Equally, arthroscopic surgical techniques have increased in popularity and PCL reconstruction continues to receive a wide interest in the orthopaedic literature [7]. Nonetheless, the lack of consensus on the most optimal reconstruction technique remains a reality. The debate most frequently relates to double versus single bundle reconstruction, graft choices, and transtibial versus tibial inlay approaches [8–10]. The principal aim of this study was to determine the long-term results based on clinical and functional assessment following arthroscopic single bundle transtibial PCL reconstruction using four strands hamstring tendon autograft. The study reports both objective and subjective outcomes and concentrates on isolated high grade PCL injury which was refractory to an initial period of functional treatment.
Methods
This study was a retrospective observational analysis on a series of patients who underwent primary posterior cruciate ligament reconstruction for isolated grade III and above PCL injuries. This was a single centre study and all operations were performed by the same surgeon, the senior author SA, using the same surgical technique. The second investigator QQ assisted and performed parts of the operations under SA supervision. In order to preserve homogeneity of cases, patients with concomitant postero-lateral corner injury, other ligamentous or meniscal injury, or osteoarthritis grade III-IV were excluded. We recorded postoperative complications, clinical and functional outcome measures. In total there were 17 patients with isolated PCL rupture, all were male with an average age of 25 years (range 19–40 years). The average follow-up time was four years (range one to nine years). Two patients were lost to follow up and excluded from the study leaving a total of 15 cases. The mechanisms of injury consisted of contact sports in 11 patients (73 %), motorcycle collision in three patients (20 %) and skiing injury in one patient (7 %). The average interval between injury and surgical treatment was 15.5 months (range two–74 months). The indications for surgical reconstruction of PCL consisted of magnetic resonance (MR) scan evidence of posterior cruciate ligament complete rupture, symptoms of instability with normal daily activities and inability to play sports in addition to symptoms being refractory to a period of non-operative treatment. Postoperatively all patients were reviewed in the outpatient clinic according to our local practice at six weeks, three, six, nine and 12 months and then at an annual interval. Patients were recalled for an assessment for the purpose of this study which included clinical examination and knee function evaluation. Patient derived outcomes were recorded with the Lysholm score and Tegner activity score. In addition, patients were objectively assessed using the International Knee Documentation Committee (IKDC) standard assessment and instrumented posterior knee laxity using KT-2000 arthrometer (MED metric™) [11]. Each case was awarded an overall grade according to IKDC standards (Grades A, B, C and D). In order to minimize bias, all evaluations were made by the same investigator.
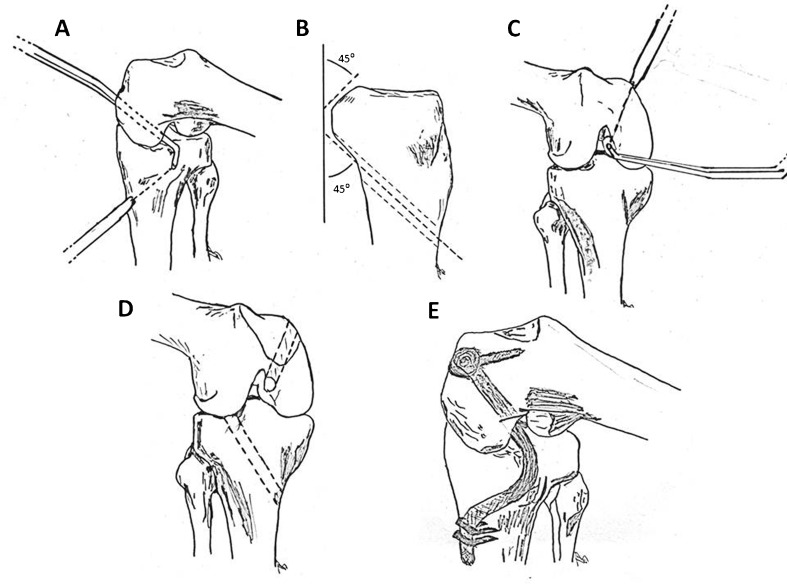
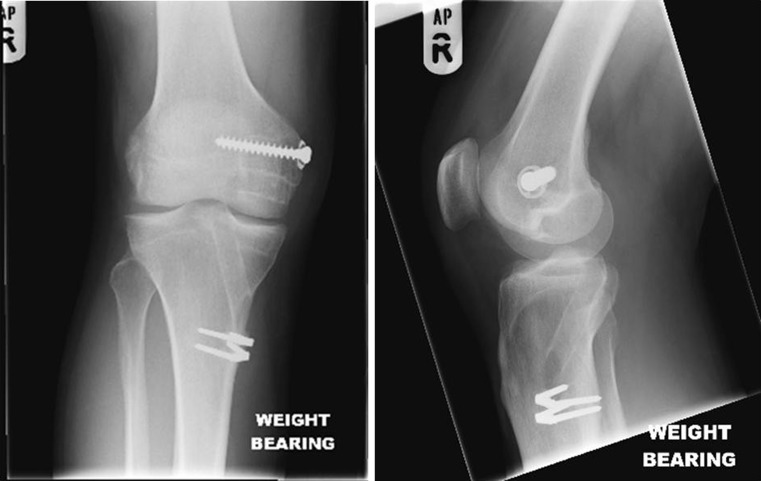
The operative technique consisted of routine examination under anaesthetic and arthroscopy for the confirmation of diagnosis and any other concomitant injuries using standard antero-lateral and antero-medial portals. A postero-lateral portal was created to resect the torn posterior cruciate ligament and define the tibial and femoral PCL footprints. Through a vertical incision on the proximal medial tibia, 24 cm of hamstring tendons (gracilis and semitendinosis) were obtained as free grafts. Using a drilling guide (Linvotec™ tibial drilling guide), the tibial tunnel was made over a guide wire. The aiming guide was positioned on the PCL footprint on the posterior tibia under direct 70° arthroscope and the drill sleeve positioned on the anteromedial aspect of the proximal tibia. Dual control was utilised as the guide position and pin insertion were monitored with an image intensifier. A cannulated reamer was used to create the tibial tunnel, with a curette positioned through the postero-lateral portal to protect the posterior neurovascular substructures. Tunnel edges were chamfered with PCL instruments rasps, and the resulting 45° angled tibial tunnel provided a smoother turn of the graft (Fig. 1). The tunnel opens at the isometric point under direct vision of a 70° arthroscope and image intensifier control. Similarly the femoral tunnel guide pin was inserted under dual control, with the entry point aimed at the centre of the PCL stump. A cannulated reamer was used over the guide pin while employing a curette to protect the anterior cruciate ligament (ACL) and chondral surfaces. The intra-articular openings of the tunnel were chamfered, an important step to prevent damage of the graft. The two tendons were looped into four strands and railroaded as a single bundle from the tibia to the femoral tunnel with the help of a suture passer and traction suture. The looped ends of the graft were fixed to a fully threaded cancellous screw and ligament washer. Standard tensioning was applied to the distal free end of the graft with a traction suture and cycled through flexion and extension. Once the graft settled the tibial fixation was achieved with two barbed staples (Smith & Nephew™) (Fig. 1). Graft position was confirmed under arthroscopic direct vision. Postoperative rehabilitation patients were provided continuous passive motion (CPM) for 12 hours then discharged from hospital at about 24 hours when mobilising independently on crutches. The physiotherapy was commenced initially with static hamstring and quadriceps exercises and close chain kinetic exercises for six weeks. Open chain kinetic exercises were introduced at that point, and a more resistant and intensive programme of muscle building exercises was carried out. No brace was used and patients were allowed full range of movement by two to three weeks. Patients were allowed to commence jogging at three months and light sporting activities at six months. Contact sports were usually delayed until nine to 12 months postoperatively. Figure 2 shows a single bundle transtibial PCL reconstruction tunnel position and graft fixation on a one-year postoperative plain radiograph.
Fig. 1.
Graphic illustrations of PCL reconstruction technique. a Drill guide used to determine position and orientation of guide pin and tibial tunnel. b Graft turning point on the posterior aspect of the tibia. c Drill guide used to determine position and orientation of guide pin and femoral tunnel. d Femoral and tibial tunnel position, chamfering tunnel entrances prevents graft attrition. e Final graft position and fixation
Fig. 2.
Post-reconstruction plain film radiographs at one year
In the absence of pre-operative clinical and functional knee scores, the statistical analysis looked at the relationship between post reconstruction clinical and functional outcomes and other variables, namely, length of follow-up and time interval between injury and reconstruction. Lysholm Score, Tegner activity score, IKDC score and KT2000 arthrometer assessment were considered dependent variables. Length of follow-up and time interval to surgery were considered independent variables. The confounding variables identified were age and mechanism of injury. The relationships between Lysholm Score, Tegner activity scroe, length of follow-up and time interval to surgery were evaluated using multiple linear regression analysis. Relationships between IKDC score and KT2000 arthrometer assessment, length of follow-up and time interval to surgery were evaluated using a multiple binary logistic regression. Both confounding variables were taken into account and adjusted for. The significance level was set at 5 % and the analyses were performed with SAS software version 9.2™ (PROC REG, PROC LOGISTIC).
Results
At final review clinic on the Lysholm knee score 11 patients (73 %) had excellent results (95–100), three patients (20 %) had good results (84–94) and one patient (7 %) had a poor score (15). Median postoperative Lysholm knee score was 95 (range 15–100). On the Tegner activity score ten patients (67 %) scored 7–8 with a return to competitive level sports, four patients (26 %) scored 4–6 with a return to heavy labour and moderate sports, and one patient (7 %) scored 1 with a return to sedentary work. Median post-reconstruction Tegner activity score was 7 (range 1–8). Table 1 provides a profile of all the PCL rupture cases included in this study along with a summary of the clinical and functional outcome measures. The adjusted associations between Lysholm score, Tegner activity score and the length of follow-up and time interval to reconstruction are presented in Table 2. Using multiple linear regression analysis no statistically significant association between these variables was found; estimated regression coefficient (estimated beta value) and 95 % confidence intervals are outlined in Table 2.
Table 1.
Profile of all posterior cruciate ligament (PCL) cases and summary of clinical and functional outcomes
| Case | Age (years) | Injury | Side | Mechanism of injury | Length of follow-up (months) | Interval to surgery (months) | Lysholm scale | Tegner activity score | % of perceived normality | IKDC scorea | Arthrometer assessed AP translation gradeb |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | PCL | Left | Rugby | 58 | 17 | 95 | 8 | 100 % | A | A |
| 2 | 38 | PCL | Left | Football | 12 | 12 | 91 | 6 | 75 % | B | A |
| 3 | 27 | PCL | Right | Motor bike | 82 | 5 | 84 | 5 | 80 % | C | B |
| 4 | 26 | PCL | Right | Football | 36 | 22 | 100 | 7 | 100 % | A | A |
| 5 | 38 | PCL | Right | Football | 77 | 74 | 95 | 4 | 80 % | B | A |
| 6 | 20 | PCL | Right | Rugby | 24 | 14 | 99 | 7 | 85 % | A | B |
| 7 | 21 | PCL | Right | Ski | 25 | 18 | 100 | 8 | 100 % | A | A |
| 8 | 38 | PCL | Left | Rugby | 72 | 27 | 99 | 8 | 95 % | A | A |
| 9 | 28 | PCL | Right | Rugby | 50 | 6 | 99 | 7 | 95 % | A | A |
| 10 | 35 | PCL | Left | Rugby | 16 | 7 | 94 | 8 | 85 % | A | A |
| 11 | 22 | PCL | Right | Football | 19 | 2 | 100 | 7 | 100 % | A | A |
| 12 | 24 | PCL | Left | Motor bike | 39 | 4 | 95 | 4 | 80 % | B | A |
| 13 | 19 | PCL | Right | Motor bike | 14 | 7 | 95 | 8 | 100 % | A | A |
| 14 | 38 | PCL | Right | Football | 75 | 8 | 15 | 1 | 40 % | B | A |
| 15 | 30 | PCL | Right | Football | 41 | 12 | 99 | 7 | 85 % | A | B |
a International Knee Documentation Committee standard assessment scores
b KT-2000 arthrometer (MED metric™) antero-posterior translation graded according to IKDC standards (Grades: A 0–2 mm, B 3–5 mm, C 6–10 mm and D >10 mm)
Table 2.
Lysholm and Tegner activity scores
| Measure | Length of follow-upa | P-value | Time interval to reconstructiona | P-value |
|---|---|---|---|---|
| Lysholm score | −0.23 (−0.77, 0.30) | 0.3578 | 0.45 (−0.26, 1.19) | 0.1922 |
| Tegner activity score | −0.03 (−0.07, 0.01) | 0.1541 | 0.007 (−0.06, 0.07) | 0.8347 |
aValues are estimated beta (β^) and 95 % confidence intervals (95 % CI) obtained with multiple linear regression model adjusted for age and mechanism of injury
At the final follow-up, the post-reconstruction IKDC score was normal or nearly normal (A and B) in 14 (93 %) patients, and abnormal (C) in one (7 %) patient. No one had severely abnormal IKDC grade (D). KT-2000 arthrometer measured the instrumented posterior laxity which was classified by IKDC standards: normal (A, 0–2 mm), nearly normal (B, 3–5 mm), abnormal (C, 6–10 mm), and severely abnormal (D, >10 mm). At final follow-up, 11 patients (73 %) were rated as normal, and four patients (27 %) as nearly normal. The adjusted associations between the objective knee assessment scores (IKDC, KT 2000 arthrometer) and the length of follow-up and time interval to reconstruction are presented in Table 3. The association between IKDC scores, KT 2000 arthrometer assessment and length of follow-up were of borderline significance—odds ratios (OR) 1.04 (95 % CI 0.97, 1.12) and 1.05 (95 % CI 0.96, 1.15), respectively. Equally an association was observed between IKDC scores, KT 2000 arthrometer assessment and time interval to reconstruction—OR 0.977 (95 % CI 0.90, 1.05) and 0.96 (95 % CI 0.81, 1.14), respectively. The statistical significance in both analyses was diminished due to small sample size.
Table 3.
International Knee Documentation Committee (IKDC) score and KT2000 arthrometer assessment
| Measure | Length of follow-upa | P-value | Time interval to reconstructiona | P-value |
|---|---|---|---|---|
| IKDC | 1.04 (0.97, 1.12) | 0.1925 | 0.977 (0.90, 1.05) | 0.5354 |
| KT2000 | 1.05 (0.96, 1.15) | 0.2534 | 0.96 (0.81, 1.14) | 0.6868 |
a Values are odds ratios (OR) and 95 % confidence interval (95 % CI) obtained with binary logistic regression model adjusted for age and mechanism of injury
There were no intra-operative complications; two patients developed serous wound discharge and delay in wound healing in the early period (two to six weeks), and this settled down completely without the need for antibiotic therapy; one patient developed complex pain syndrome and was referred to specialist pain clinic. At approximately one year, two patients required metal work removal due to soft tissue irritation on the medial femoral condyle. Figure 3 outlines patients outcomes in each scoring category.
Fig. 3.
Post-reconstruction clinical and functional outcomes
Discussion
Arthroscopic posterior cruciate ligament reconstruction is a surgically demanding procedure aimed at restoring normal knee kinematics and function. Isometric reconstruction and potential risk of injury to the posterior neurovascular bundles create potential complications. In this study, we evaluated the performance of single bundle transtibial hamstring autograft PCL reconstruction in a patient population with isolated grade III and above PCL injury. We found satisfactory long-term clinical and functional results without significant complications. There is a paucity in the level of evidence present in the relevant literature, and studies on isolated PCL injury are rare and often with small sample size. The largest sample size study we identified reported on 32 cases [5]. Although it is difficult to simply compare our outcomes with other studies especially when different graft material and surgical technique are utilised, certain parameters surrounding this PCL reconstruction need to be considered.
Studies which used similar graft material, graft preparation and surgical technique showed comparable results [6]. In a recent review Hammoud and colleagues reported satisfactory results in isolated PCL reconstruction with a return to pre-injury activity level of 50–82 % [6]. Several graft options are available for PCL reconstruction: hamstring, patellar, Achilles, synthetic, and cadaveric grafts [7]. The surgical reconstruction described relied on the use of autologous four strand hamstring graft because of its strength, its biological bulk and the belief that it has a greater resistance at the killer bend [12]. Lim and colleagues in a series looking at 22 PCL reconstructions using Achilles tendon allograft at a mean follow up of 33 months found similar satisfactory clinical and functional outcome [13]. Despite the paucity of high level evidence supporting double versus single bundle reconstruction, a recent large cohort study failed to demonstrate a difference in the clinical and functional outcome between the two techniques [8]. There is also a lack of prospective studies supporting superiority of transtibial versus tibial inlay techniques; the evidence available suggests satisfactory results in both approaches and choice is often due to surgeons experience [10]. According to the available literature, better results with double bundle tibial inlay PCL reconstruction are only found in multiligaments injury cases [5, 8]. Chamfering the sharp edges of the bone at the entrance of the tunnels in our experience helps reduce risk of reconstruction failure by graft abrasion without the need to alter the graft position angulation or tibial tunnel route suggested in other studies [12]. The key safety approach in doing this procedure is to operate under a double control, with direct view using a 70 degree arthroscope and intra-operative image intensifier control. The latter is highly recommended in order to not only achieve optimal isometric graft position but also minimise the risks to posterior neurovascular structures during tibial tunnel preparation [7]. In this series the use of image an intensifier and arthroscope allowed the surgeons to monitor instruments as they are positioned in the posterior aspect of the knee, thus producing a more accurate guide pin position while reducing the risk to neurovascular structures.
Our study demonstrated clinical results of similar nature with comparable length of follow-up to studies utilising graft material with bone plug for PCL reconstruction [14]. The use of graft material which incorporates bone plug is well documented in the literature. Its advocates postulate the ability to provide better graft fixation and longstanding stability. It is important to highlight however that bone plug fixation is subject to limiting factors, namely, plug length and diameter. It has been previously shown that bone plugs displacement or fractures are the most common failure modes [15]. This plethora of cadaveric and biomechanical studies supports the use of soft tissue fixation with backup fixation [15, 16]. The average interval of time between the injury and reconstructive surgery in this study was of 15.5 months. Although no other study had previously looked at the impact of this variable, it is widely accepted that earlier reconstruction may be associated with better outcomes overall due to the preservation of posterior soft tissue tensile integrity [7]. Our study showed no significant relationship between timing of surgery and clinical and functional outcomes. Our postoperative rehabilitation consisted of a standard fast track programme without the use of a knee brace or support. Despite this rapid rehabilitation, our results were consistent with the often recommended protected postoperative rehabilitation [17].
The results reported in our study demonstrate a very good overall restoration of knee kinematics and function on both objective and subjective scales. Results of subjective perception of normality level in relation to the contralateral uninjured side were 100 % in five patients, 80–99 % in eight patients, 60–79 % in one patient and 40 % in one patient, with a mean perceived percentage of normality on the operated knee of 87 %. The patient with the lowest Lysholm score (15) and Tegner activity score (1) still reported good results in the objective assessment IKDC grade B, and KT-2000 arthrometer measurement rated normal. In contrast the single case with an abnormal IKDC grade scored 84/100 on the Lysholm score and 5 (work-heavy labour) on the Tegner activity score. In relation to occupational history, none of the patients were heavy manual workers. There were eight of 15 sedentary workers and six light manual workers. Post PCL reconstruction, 11 patients remained at the pre-injury level of occupation, one patient improved on their pre-injury level and two reduced their level of occupation. In addition, ten patients regularly played contact sports and four light sports such as tennis and skiing. At the final review clinic, 12 patients continued in their chosen sport, whereas two patients reduced their level of sporting pursuit. One case was unable to play sports due to complex regional pain syndrome. In this series one patient was noted to have pain, patchy discolouration, cold sensitivity and swelling on the operated knee at three months postoperatively. This same patient went on to develop complex regional pain syndrome and was eventually referred to a pain management clinic. Although his symptoms were shown to improve, the functional result was still overall poor. Of note, this case had a very stable knee, demonstrated normal (A) measurement on the KT 2000 arthrometer assessment and was graded nearly normal (B) on the IKDC standard assessment.
The principal weaknesses in this study are the small sample size and the lack of pre-operative data on the injured knee clinical and functional status. Based on our results however, we conclude that it is possible to achieve satisfactory objective and subjective outcomes with arthroscopic posterior cruciate ligament reconstruction using four strand hamstrings tendon graft even in the long term. Arthroscopic single bundle transtibial PCL reconstruction offers similar clinical and functional outcomes to other techniques previously described. Taking into account the limitations of our study, larger prospective studies are needed to delineate the differences between the various treatment approaches and ultimately make firmer recommendations on future treatment options.
Acknowledgments
Conflict of interest
No competing interests declared and no external funds received.
Contributor Information
Tarek Boutefnouchet, Phone: +44-780-9677302, Email: tboutefnouchet@hotmail.com.
Malek Bentayeb, Email: malek2toi@hotmail.com.
Qutub Qadri, Email: Qutub.Qadri@dgoh.nhs.uk.
Salman Ali, Email: msaorthopaedics@btconnect.com.
References
- 1.Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186–191. doi: 10.1007/s00402-002-0471-y. [DOI] [PubMed] [Google Scholar]
- 2.Wind WM, Jr, Bergfield JA, Parker RD. Evaluation and treatment of posterior cruciate ligament injuries. revisited. Am J Sports Med. 2004;32(7):1765–1775. doi: 10.1177/0363546504270481. [DOI] [PubMed] [Google Scholar]
- 3.Richter M, Bosch U, Wipermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30(5):718–727. doi: 10.1177/03635465020300051601. [DOI] [PubMed] [Google Scholar]
- 4.Kim SJ, Park IS, CHeon YM, Ryu SW. Double bundle technique: endoscopic posterior cruciate ligament reconstruction using tibialis posterior allograft. Arthroscopy. 2004;20(10):1090–1094. doi: 10.1016/j.arthro.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Kim YM, Lee CA, Matava MJ. Clinical results of arthroscopic single bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2011;39:425–434. doi: 10.1177/0363546510374452. [DOI] [PubMed] [Google Scholar]
- 6.Hammoud S, Reinhardt KR, Marx RG. Outcomes of posterior cruciate ligament treatment: a review of the evidence. Sports Med Arthrosc. 2010;18(4):280–291. doi: 10.1097/JSA.0b013e3181eaf8b4. [DOI] [PubMed] [Google Scholar]
- 7.Fanelli GC, Beck JD, Edson CJ. Current concepts review: the posterior cruciate ligament. J Knee Surg. 2010;23(2):61–72. doi: 10.1055/s-0030-1267466. [DOI] [PubMed] [Google Scholar]
- 8.Kim SJ, Jung M, Moon HK, Kim SG, Chun YM. Anterolateral transtibial posterior cruciate ligament reconstruction combined with anatomical reconstruction of posterolateral corner insufficiency: comparison of single-bundle versus double-bundle posterior cruciate ligament reconstruction over a 2- to 6-year follow-up. Am J Sports Med. 2011;39(3):481–489. doi: 10.1177/0363546510385398. [DOI] [PubMed] [Google Scholar]
- 9.Höher J, Scheffler S, Weiler A. Graft choice and graft fixation in PCL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):297–306. doi: 10.1007/s00167-003-0408-1. [DOI] [PubMed] [Google Scholar]
- 10.May JH, Gillette BP, Morgan JA, Krych AJ, Stuart MJ, Levy BA. Transtibial versus inlay posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg. 2010;23(2):73–79. doi: 10.1055/s-0030-1267468. [DOI] [PubMed] [Google Scholar]
- 11.Wang D, Jones MH, Khair MM, Miniaci A. Patient-reported outcome measures for the knee. J Knee Surg. 2010;23(3):137–151. doi: 10.1055/s-0030-1268691. [DOI] [PubMed] [Google Scholar]
- 12.Huang TW, Wang CJ, Weng LH, Chan YS. Reducing the "killer turn" in posterior cruciate ligament reconstruction. Arthroscopy. 2003;19(7):712–716. doi: 10.1016/S0749-8063(03)00394-3. [DOI] [PubMed] [Google Scholar]
- 13.Lim HC, Bae JH, Wang JH, Yang JH, Seok CW, Kim HJ, Kim SJ. Double-bundle PCL reconstruction using tibial double cross-pin fixation. Knee Surg Traumatol Arthrosc. 2010;18(1):117–122. doi: 10.1007/s00167-009-0812-2. [DOI] [PubMed] [Google Scholar]
- 14.Cooper DE, Stewart D. Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up. Am J Sports Med. 2004;32(2):346–360. doi: 10.1177/0363546503261511. [DOI] [PubMed] [Google Scholar]
- 15.Lim HC, Bae JH, Wang JH, Bae TS, Kim CW, Hwang JH, Yoon JY. The biomechanical performance of bone block and soft-tissue posterior cruciate ligament graft fixation with interference screw and cross-pin techniques. Arthroscopy. 2009;25(3):250–256. doi: 10.1016/j.arthro.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 16.Wang CJ, Chen HH, Chen HS, Huang TW. Effects of knee position, graft tension, and mode of fixation in posterior cruciate ligament reconstruction: a cadaveric knee study. Arthroscopy. 2002;18(5):496–501. doi: 10.1053/jars.2002.32326. [DOI] [PubMed] [Google Scholar]
- 17.Fanelli GC. Posterior cruciate ligament rehabilitation: how slow should we go? Arthroscopy. 2008;24(2):234–235. doi: 10.1016/j.arthro.2007.09.009. [DOI] [PubMed] [Google Scholar]