Abstract
Purpose
The aim of this meta-analysis was to compare the results of arthroscopic single-bundle and double-bundle anterior cruciate ligament (ACL) reconstruction.
Methods
We systematically searched electronic databases to identify randomised controlled trials (RCTs) in which arthroscopic single-bundle was compared with double-bundle for ACL reconstruction. The search strategy followed the requirements of the Cochrane Library Handbook. The outcomes of these studies were analysed in terms of graft failures, Lysholm score, negative pivot-shift test, KT1000 arthrometer measurements, knee extensor and flexor peak torques, knee extension and flexion deficit, and subjective and objective International Knee Documentation Committee (IKDC) final score. Methodological quality was assessed and data were extracted independently. Standard mean difference (SMD) or odds ratio (OR) with 95 % confidence interval (CI) was calculated by a fixed effects or random effects model. Heterogeneity across the studies was assessed with the I-square and chi-square statistic. Forest plots were also generated.
Results
We identified 17 RCTs comprising 1,381 patients who were treated by arthroscopic single-bundle versus double-bundle ACL reconstruction. The results of meta-analysis of these studies showed that arthroscopic double-bundle reconstruction was associated with a lower risk of graft failures (P = 0.002) and a lower rate of positive pivot-shift test (P < 0.0001). Compared with single-bundle reconstruction, double-bundle reconstruction had a lower KT1000 arthrometer measurement (P < 0.00001), a lower knee extension deficit (P = 0.006) and a higher subjective IKDC score (P = 0.03). There was no statistically significant difference between single-bundle and double-bundle reconstruction in Lysholm score (P = 0.91), knee extensor peak torques (P = 0.97), knee flexor peak torques (P = 0.96), knee flexion deficit (P = 0.30) and objective IKDC score (P = 0.18).
Conclusions
Considering the more favourable outcomes of graft failures, knee joint stability and knee joint function in double-bundle reconstruction, we concluded that arthroscopic double-bundle reconstruction should be considered as the primary treatment in ACL reconstruction.
Introduction
The anterior cruciate ligament (ACL) is one of the most commonly injured ligaments at the knee. Reconstruction of the ACL is a common procedure [1, 2]. The arthroscopic single-bundle technique is widely used for patients who suffered from ACL rupture. Anatomical and biomechanical studies have shown that the ACL comprises two principal bundles, the anteromedial and the posterolateral [3, 4]. The arthroscopic double-bundle technique has recently been used by many surgeons in an attempt to reproduce both the anteromedial bundle and the posterolateral bundle.
A single-bundle reconstruction is performed by producing one single femoral tunnel and one single tibial tunnel. Conventional single-bundle ACL reconstructive procedures focus primarily on reproducing the anteromedial bundle. Two studies demonstrated that single-bundle anteromedial reconstruction alone was insufficient to control the combined rotator load and valgus torque that simulates the pivot-shift test [5, 6]. On the basis of biomechanical studies on human cadavers showing that the posterolateral bundle of the ACL becomes important near full knee extension, especially under anterior tibial and rotator loads [7, 8]. Although much of the evidence supports the use of the double-bundle technique [9, 15, 18, 19, 23], some trials have not found significant differences between clinical outcomes in the patient groups [10, 11, 21, 29]. A previously published meta-analysis which included only four randomised controlled trials (RCTs) showed that there were no clinically significant differences in KT1000 arthrometer and pivot-shift results between single-bundle and double-bundle techniques in 2008 [46]. Therefore, it remains unclear which technique has much more advantages.
The purpose of this paper is to present a meta-analysis of original research studies dealing with arthroscopic single-bundle reconstruction and double-bundle reconstruction of the ACL. We carried out an up-to-date meta-analysis of all available RCTs to establish whether single-bundle or double-bundle is a superior treatment for ACL reconstruction. Our aim was to identify and summarise the best available evidence from RCTs between single-bundle and double-bundle reconstruction of the ACL. We hypothesised that double-bundle ACL reconstruction would be advantageous in restoring the stability and function of the knee joint, compared with single-bundle reconstruction.
Methods
Search strategy
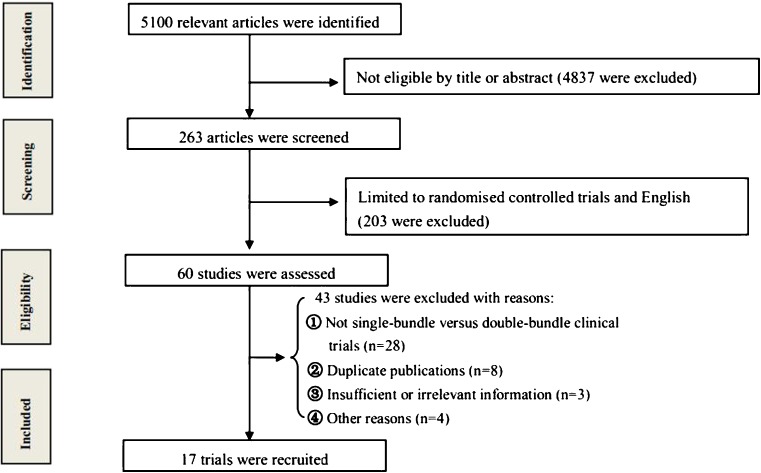
We searched for relevant studies according to the search strategy of the Cochrane Collaboration. Three of the authors independently completed an online search of PubMed, Cochrane Library, EMBASE, BIOSIS and Ovid (last search update 1 May 2012). Computer literature search was conducted using specific search terms (ACL, anterior cruciate ligament, reconstruction, single-bundle and double-bundle). All searches were limited to the English language. Citations that included the search terms in either the title, abstract, article or medical subject heading (MeSH) terms were retained. Additional strategies to identify relevant studies were supplemented with manual searches of major orthopaedic textbooks and bibliographies of the published articles. All of the results were limited by “randomised controlled trials”. Studies without comparisons of the clinical results were excluded from the search result. We pooled the RCT studies comparing arthroscopic single-bundle versus double-bundle in reconstruction of the ACL. A flow chart of the study selection process is presented in Fig. 1.
Fig. 1.
Flow chart of eligibility selection
Inclusion criteria
We identified the articles that met the following criteria: (1) prospective RCTs comparing single-bundle technique with double-bundle technique; (2) primary ACL reconstruction; (3) absence of ligament injury to the contralateral knee; (4) closed growth plates; and (5) the target population consisted of individuals who presented with ACL disruption and needed surgical intervention. Duplicate or multiple publications of the same study were not included. Two reviewers assessed the articles independently to determine if they met the inclusion criteria. Disagreements between reviewers were resolved by consensus.
Outcome measures
The outcome measures of this meta-analysis included graft failures, Lysholm score, negative pivot-shift test, KT1000 arthrometer, knee extensor and flexor peak torques (Biodex/Cybex dynamometer at 60°/s), knee extension and flexion deficit, and subjective and objective International Knee Documentation Committee (IKDC) score. Graft failures were defined as reoperation after ACL reconstruction. Function evaluation was performed with knee motion deficit (extension and flexion), Lysholm scale and IKDC. The Lysholm scale ranges from 0 to 100, with 0 representing the worst results and 100 representing optimal results [31]. According to the objective IKDC scale, a normally functioning knee is graded as A, a near-normally functioning knee is graded as B, a fairly functioning knee is graded as C and a poorly functioning knee is graded as D [32]. We took the number of individuals with normal objective IKDC graded as A. The subjective IKDC score was also pooled and evaluated in this meta-analysis. The stability of the knee joint was evaluated by knee isokinetic peak torques (extensor and flexor), pivot-shift test and KT1000 arthrometer. The pivot-shift test was categorised as normal (negative), nearly normal (1+), abnormal (2+) and severely abnormal (3+). We recorded the number of individuals with negative pivot-shift test for meta-analysis. Side-to-side difference in anterior tibial translation was assessed with the KT1000 arthrometer (MEDmetric, San Diego, CA, USA) at 134 N [33]. The data were extracted by two reviewers independently to ensure that they were accurate. When there was any disagreement, a consensus was reached by discussion within the review team.
Methodological quality assessment
Each study was independently assessed by two of the reviewers. In order to ensure the methodological quality of the studies that were included in the meta-analysis, the Consolidated Standards of Reporting Trials (CONSORT) checklist and scoring system was used [34]. Each study that met the inclusion criteria was appraised with use of this 22-point checklist. Every study was assigned a quality rating, with scores of 18–22 representing excellent study quality, 13–17 good quality, 8–12 fair quality and 7 or less poor quality. To avoid unnecessary bias, the reviewers were blinded to the study’s title, author and institution of origin. Conflicts were resolved through consensus.
Statistical analysis
In each study the odds ratio (OR) with 95 % confidence intervals (CIs) was calculated for dichotomous outcomes. For continuous outcome measures, the standard mean difference (SMD) and the associated 95 % CIs were evaluated for all studies. We tested for heterogeneity using both the chi-square and I-square test. For the I-square statistic, a value of less than 25 % is considered to reflect low heterogeneity, 50 % moderate heterogeneity and 75 % high heterogeneity. Generally, we defined study heterogeneity as a significant test of heterogeneity (I2 > 50 %) and differences in the treatment effects across studies. I-square was used to estimate total variation across studies. All data were combined with the fixed effects model as there was no evidence of statistical heterogeneity between studies for any of our outcome measures. A random effects model was used when significant heterogeneity was detected. For our outcome measures, a P value of <0.05 was considered statistically significant. A funnel plot was created to assess for publication bias. This plot for studies demonstrates the relationship between the sample size of the studies and the precision in estimating the treatment effect. Bias can be seen if the plot is widely skewed [35].
Results
Study identification
There were 263 potentially relevant papers. Most of these studies were not suitable for our analysis because they included case reports, biomaterial studies, biomechanical studies, non-randomised cohort studies, retrospective studies and other study subjects irrelevant to our question. By limiting the search to only RCTs, 20 clinical trials met our inclusion criteria (level I evidence) [11–29, 43]. Three of these studies had to be excluded from the meta-analysis because of inadequacy of data details [11, 29, 43]. Accordingly, there were 17 publications left [12–28]. A total of 1,381 patients undergoing ACL reconstruction were identified: 722 in the single-bundle group and 659 in the double-bundle group. However, when anatomical single-bundle was restricted, only six RCTs were left comprising 449 patients: 189 in the anatomical single-bundle group and 260 in the double-bundle group. The assessment results for eligible trials by use of the CONSORT checklist showed that the score ranged from 12 to 19. According to the CONSORT checklist, four studies achieved an excellent rating (score 18–22), 12 studies attained a good rating (score 13–17) and one study had a fair quality (score 8–12), with a mean score 15.8. The demographic information and detailed characteristics of the included studies are listed in Tables 1 and 2.
Table 1.
Demographic information of included studies
| Studies, first author | Publication year | Numbers (SB/DB) | Follow-up duration (mean, months) | No. of ineffective at follow-up (SB/DB) | CONSORT score |
|---|---|---|---|---|---|
| Lee [12] | 2012 | 21/21 | 24 | 3/2 | 14/22 |
| Núñez [13] | 2012 | 25/30 | 24 | 2/1 | 18/22 |
| Ochiai [14] | 2012 | 44/40 | 24 | 0/0 | 15/22 |
| Araki [15] | 2011 | 10/10 | 24 | 0/0 | 16/22 |
| Hussein [16] | 2011 | 78/131 | 51 | 0/0 | 19/22 |
| Hemmerich [17] | 2011 | 17/15 | 5 | 0/3 | 13/22 |
| Zaffagnini [18] | 2011 | 39/40 | 103 | 0/0 | 14/22 |
| Suomalainen [23] | 2011 | 71/67 | 24 | 11/6 | 17/22 |
| Aglietti [19] | 2010 | 35/35 | 24 | 0/0 | 19/22 |
| Ibrahim [20] | 2009 | 150/50 | 29 | 102/0 | 16/22 |
| Wang [21] | 2009 | 32/32 | 16 | 0/0 | 14/22 |
| Järvelä [22] | 2008 | 52/25 | 24 | 31/3 | 16/22 |
| Siebold [25] | 2008 | 35/35 | 19 | 0/0 | 17/22 |
| Streich [26] | 2008 | 25/24 | 24 | 0/0 | 15/22 |
| Järvelä [24] | 2008 | 25/35 | 27 | 4/3 | 16/22 |
| Muneta [27] | 2007 | 34/34 | 25 | 0/0 | 18/22 |
| Järvelä [28] | 2007 | 30/35 | 14 | 5/5 | 12/22 |
SB single-bundle, DB double-bundle
Table 2.
Characteristics of the 17 studies used in the meta-analysis
| Studies, first author | Randomised method | Graft material of SB | Graft material of DB | Weight-bearing time after surgery |
|---|---|---|---|---|
| Lee [12] | Not mentioned | Autologous STG | Autologous STG | As tolerated |
| Núñez [13] | A random list of numbers | Autologous STG | Autologous STG | Not mentioned |
| Ochiai [14] | Not mentioned | Autologous STG | Autologous STG | First 2 weeks |
| Araki [15] | Closed envelopes | Autologous STG | Autologous STG | Not mentioned |
| Hussein [16] | Computer software | Autologous STG | Autologous STG | As tolerated |
| Hemmerich [17] | METLAB analysis | Autologous STG | Autologous STG | Not mentioned |
| Zaffagnini [18] | Computer-generated | Patellar tendon | Autologous STG | First 2 weeks |
| Suomalainen [23] | Closed envelopes | Autologous STG | Autologous STG | Immediately after surgery |
| Aglietti [19] | Not mentioned | Autologous STG | Autologous STG | Not mentioned |
| Ibrahim [20] | Closed envelopes | Autologous STG | Autologous STG | Immediately after surgery |
| Wang [21] | Not mentioned | Autologous STG | Autologous STG | Second day after surgery |
| Järvelä [22] | Closed envelopes | Autologous STG | Autologous STG | Immediately after surgery |
| Siebold [25] | Computer | Autologous STG | Autologous STG | First week |
| Streich [26] | Not mentioned | Autologous ST | Autologous ST | 1 months after surgery |
| Järvelä [24] | Closed envelopes | Autologous STG | Autologous STG | Immediately after surgery |
| Muneta [27] | Odd and even number | Autologous STG | Autologous STG | 3 days after surgery |
| Järvelä [28] | Closed envelopes | Autologous STG | Autologous STG | Immediately after surgery |
SB single-bundle, DB double-bundleST semitendinosus tendon, STG semitendinosus and gracilis tendons, METLAB MathWorks, Natick, MA, USA
Functional outcome
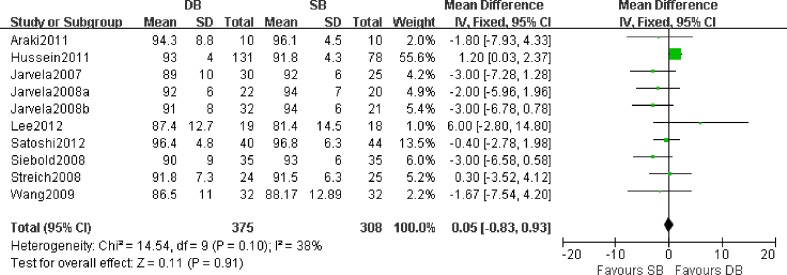
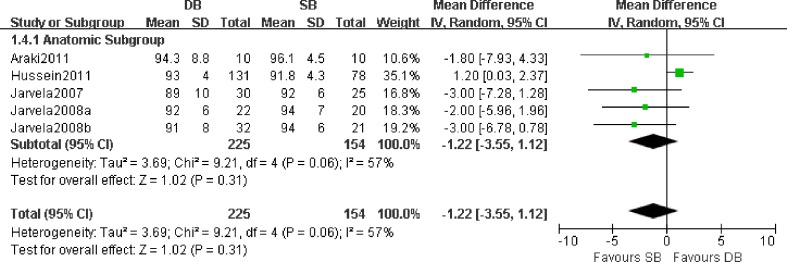
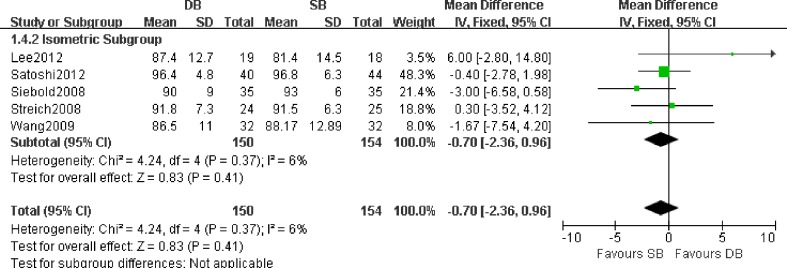
Ten studies with a total of 683 patients who were available at the time of the latest follow-up included Lysholm data that were suitable for meta-analysis [12, 14–16, 21, 22, 24–26, 28]. Figure 2 shows the results of Lysholm score at the follow-up. With a fixed effects model, the results showed that there was no significant difference between the two groups in Lysholm functional score (SMD 0.05; 95 % CI −0.83 to 0.92; P = 0.92). The forest plot showed higher Lysholm scores with single-bundle reconstruction than with double-bundle reconstruction, but the difference was not statistically significant. Heterogeneity across the studies was not considered not significant (P = 0.10; I2 = 38 %). Figures 3 and 4 show that there was no significant difference between double-bundle and single-bundle concerning Lysholm score in the anatomical subgroup (P = 0.31) with a random effects model (P = 0.06; I2 = 57 %) and in the isometric subgroup (P = 0.41) with a fixed effects model (P = 0.37; I2 = 6 %).
Fig. 2.
Forest plot of Lysholm score. Individual studies are listed on the left with Lysholm score (mean and standard deviation) as well as number of patients in each study group. A visual representation of the standard mean difference for each study is plotted on the right with a diamond. The large black diamond at the bottom represents the pooled treatment effect of all studies. It lies on the midline, representing no significant difference (P = 0.91) with a fixed effects model. DB double-bundle, SB single-bundle, Järvelä 2008a the study of reference [22], Järvelä 2008b the study of reference [24]
Fig. 3.
Forest plot of Lysholm score in the anatomical subgroup. The pooled treatment effect, with a random effects model, demonstrates no significant difference between double-bundle (DB) and single-bundle (SB) (P = 0.31)
Fig. 4.
Forest plot of Lysholm score in the isometric subgroup. The pooled treatment effect, with a fixed effects model, demonstrates no significant difference between double-bundle (DB) and single-bundle (SB) (P = 0.41)
Ten studies with a total of 823 patients who were available at the time of the latest follow-up provided the objective IKDC final score for meta-analysis [12, 16, 19, 20, 22–25, 27, 28]. Figure 5 shows the number of individuals with normal objective IKDC final score at the follow-up. With a random effects model, the pooling of data showed that there was no significant difference between the single-bundle and double-bundle techniques (OR 1.56; 95 % CI 0.82–2.95; P = 0.18). The forest plot showed double-bundle reconstruction had better objective IKDC final score, and the difference was statistically significant. Heterogeneity across the studies was considered significant (P < 0.0001; I2 = 76 %). Similarly, there was no significant difference in the anatomical subgroup (OR 1.51; 95 % CI 0.49–4.70; P = 0.47) and isometric subgroup (OR 1.57; 95 % CI 0.71–3.48; P = 0.27).
Fig. 5.
Forest plot of objective IKDC score. The pooled treatment effect, represented by the black diamond, demonstrates no significant difference (P = 0.18)
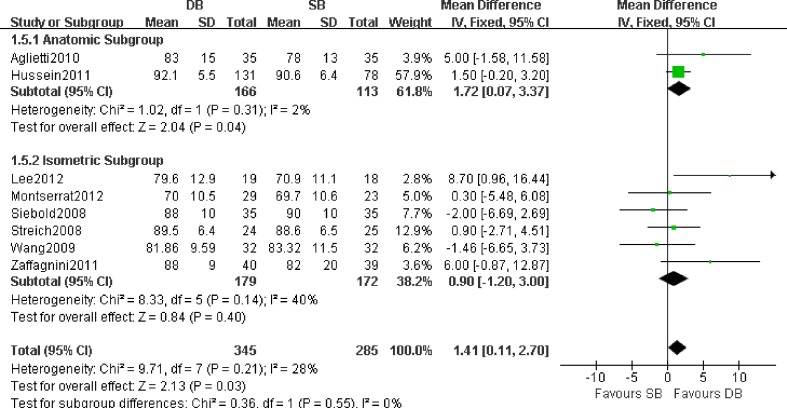
Subjective IKDC score was reported in eight studies with 630 patients [12, 13, 16, 18, 19, 21, 25, 28]. Figure 6 shows that for subjective IKDC score at the follow-up, with a fixed effects model, the results analysed suggested a significant difference between the single-bundle and double-bundle groups (SMD 1.41; 95 % CI 0.11–2.70; P = 0.03). Heterogeneity was not significant across the studies (P = 0.21; I2 = 28 %). There was a significant difference in the anatomical subgroup (SMD 1.72; 95 % CI 0.07–3.37; P = 0.04). However, there was no significant difference in the isometric subgroup (SMD 0.90; 95 % CI −1.20 to 3.00; P = 0.40).
Fig. 6.
Forest plot of subjective IKDC score. The pooled treatment effect, represented by the black diamond, demonstrates a significant difference favouring double-bundle (DB) (P = 0.03)
As to knee extension and flexion deficit, 279 patients in two studies were included [16, 25]. Figure 7 shows the results of knee extension deficit and Fig. 8 shows those of knee flexion deficit. With a fixed effects model, there was a significant difference between the two groups in knee extension deficit (SMD −0.37; 95 % CI −0.63 to −0.11; P = 0.006). Heterogeneity across the studies was not considered significant (P = 0.42; I2 = 0 %). However, there was no significant difference between the two groups (SMD −0.40; 95 % CI −1.15 to 0.35; P = 0.30) according to the results of knee flexion deficit. Heterogeneity across the studies was not considered significant (P = 0.60; I2 = 0 %).
Fig. 7.
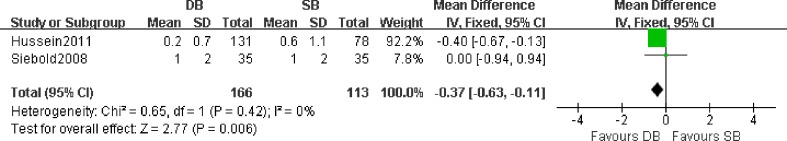
Forest plot of knee extension deficit. The pooled treatment effect, represented by the black diamond, demonstrates a significant difference favouring double-bundle (DB) (P = 0.006)
Fig. 8.
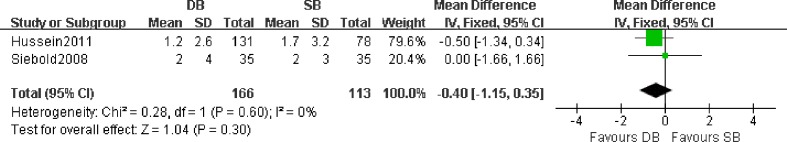
Forest plot of knee flexion deficit. The pooled treatment effect, represented by the black diamond, demonstrates no significant difference (P = 0.30)
Stability of knee joint
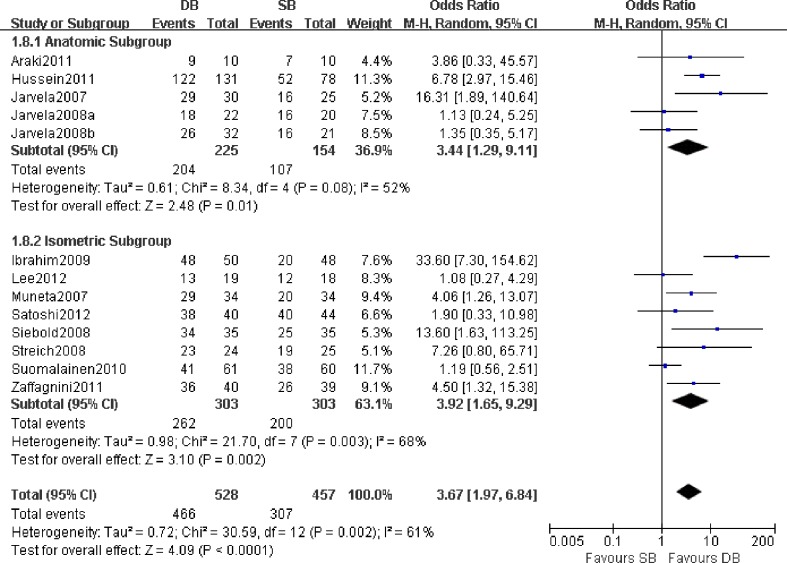
Results of the pivot-shift test were reported in 13 studies with a total of 985 patients for meta-analysis [12, 14–16, 18, 20, 22–28]. Figure 9 shows the number of individuals with negative pivot-shift test at the follow-up. With a random effects model, the results showed a significant difference in negative pivot-shift tests between the two groups (OR 3.67; 95 % CI 1.97–6.84; P < 0.0001). The forest plot demonstrated a significant difference favouring the double-bundle technique. Heterogeneity was significant across the studies (P = 0.002; I2 = 60 %). Similarly, there was a significant difference in the anatomical subgroup (OR 3.44; 95 % CI 1.29–9.11; P = 0.01) and isometric subgroup (OR 3.92; 95 % CI 1.65–9.29; P = 0.002).
Fig. 9.
Forest plot of negative pivot-shift test. The pooled treatment effect, represented by the black diamond, demonstrates a significant difference favouring double-bundle (DB) with a higher negative rate (P < 0.0001)
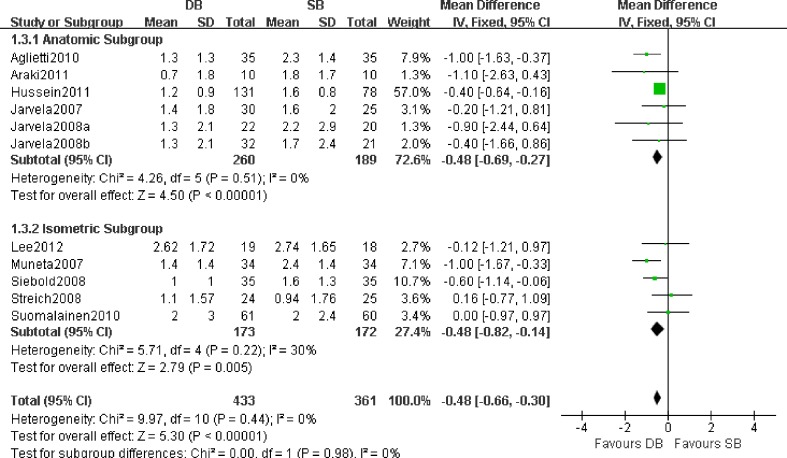
Eleven studies including 794 patients provide the KT1000 arthrometer (MEDmetric, San Diego, CA, USA) results at the follow-up [12, 15, 16, 19, 22–28]. Figure 10 shows the results of KT1000 arthrometer measurements. The results from a fixed effects model showed a significant difference between the two groups (SMD −0.48; 95 % CI −0.66 to −0.30; P < 0.00001). The forest plot showed that the double-bundle group had an advantage with KT1000 arthrometer postoperatively. Heterogeneity across the studies was not considered significant (P = 0.44; I2 = 0 %). Similarly, there was a significant difference in the anatomical subgroup (SMD −0.48; 95 % CI −0.69 to −0.27; P < 0.00001) and isometric subgroup (SMD −0.48; 95 % CI −0.82 to −0.14; P = 0.005).
Fig. 10.
Forest plot of KT1000 arthrometer measurements. The large black diamond at the bottom represents the pooled treatment effect of all studies. It lies exclusively to the left and does not cross the midline, representing a lower KT1000 arthrometer measurement favouring double-bundle (DB) with a significant difference (P < 0.00001)
Referring to the knee isokinetic extensor and flexor strength, only 121 patients in three articles were reported [12, 15, 21]. With a fixed effects model, Figs. 11 and 12 show that no significant differences were found for the incidence of extensor peak torques (SMD 0.09; 95 % CI −5.07 to 5.26; P = 0.97) and flexor peak torques (SMD −0.10; 95 % CI −3.96 to 3.76; P = 0.96) between the two groups. Heterogeneity across the studies was not considered significant (P = 0.94; I2 = 0 % and P = 0.61; I2 = 0 %).
Fig. 11.
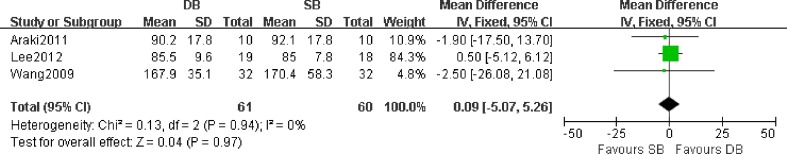
Forest plot of knee extensor peak torques. The pooled treatment effect, represented by the black diamond, demonstrates no significant difference (P = 0.97)
Fig. 12.
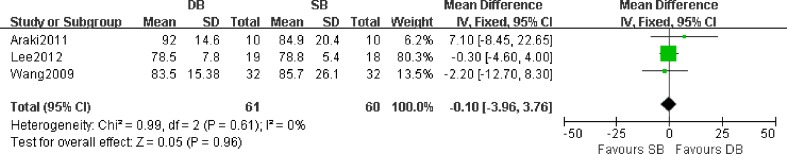
Forest plot of knee flexor peak torques. The pooled treatment effect, represented by the black diamond, demonstrates no significant difference (P = 0.96)
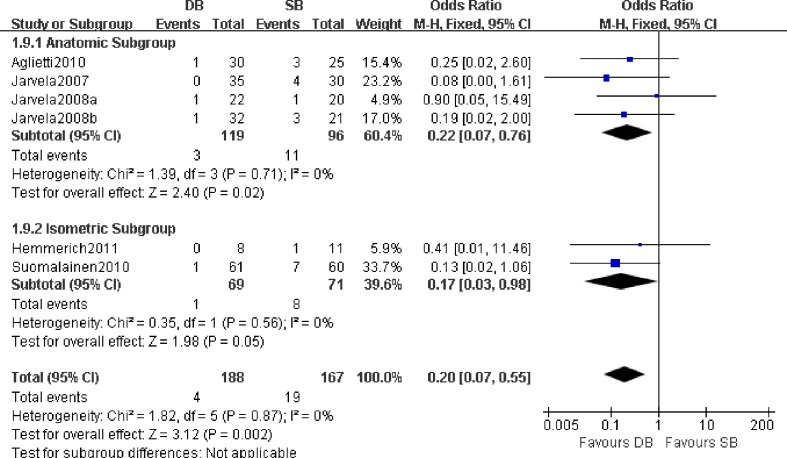
Graft failures
With regard to graft failures, six publications with a total of 355 patients reported the outcome at the end of follow-up [14, 17, 19, 22–24, 28]. Figure 13 shows the results of meta-analysis. Järvelä [28] reported the number of patients who undergo graft failure in both groups, but these patients were excluded from the statistical analysis of their study. However, we must include the patients in our study when we analyse the data. Graft failures of ACL reconstruction were more common in the single-bundle group compared with the double-bundle group, and the difference was statistically significant (OR 0.20; 95 % CI 0.07–0.55; P = 0.002). Heterogeneity was not significant across the studies (P = 0.87; I2 = 0 %). Similarly, there was a significant difference in the anatomical subgroup (OR 0.22; 95 % CI 0.07–0.76; P = 0.02) and isometric subgroup (OR 0.17; 95 % CI 0.03–0.98; P = 0.05).
Fig. 13.
Forest plot of graft failure. The pooled treatment effect, represented by the black diamond, demonstrates a significant difference favouring double-bundle (DB) with a lower rate of graft failure (P = 0.002)
Sensitivity analysis and publication bias
Sensitivity analysis was used in this meta-analysis to assess the robustness of results. Sensitivity analysis revealed that with low-quality (CONSORT score = 12) studies excluded, the summary OR/SMD, 95 % CIs and P values for negative pivot-shift, Lysholm score and KT1000 arthrometer (as these outcomes were reported in most of the studies of this meta-analysis) were still similar to the results before they were excluded, as presented in Table 3.
Table 3.
Sensitivity analysis of this meta-analysis
| Outcomes | No. of studies | No. of patients | OR/SMD (95 % CI) | P value | |
|---|---|---|---|---|---|
| No studies excluded | Negative pivot-shift test | 13 | 985 | 3.67 (1.97–6.84) | <0.0001 |
| Lysholm score | 10 | 683 | 0.05 (−0.83 to 0.93) | 0.91 | |
| KT1000 arthrometer | 11 | 794 | −0.48 (−0.66 to −0.30) | <0.00001 | |
| Excluded studies of low-quality (CONSORT score = 12) | Negative pivot-shift test | 12 | 930 | 3.37 (1.79–6.34) | 0.0002 |
| Lysholm score | 9 | 628 | 0.18 (−0.71 to 1.08) | 0.69 | |
| KT1000 arthrometer | 10 | 739 | −0.49 (−0.67 to −0.31) | <0.00001 |
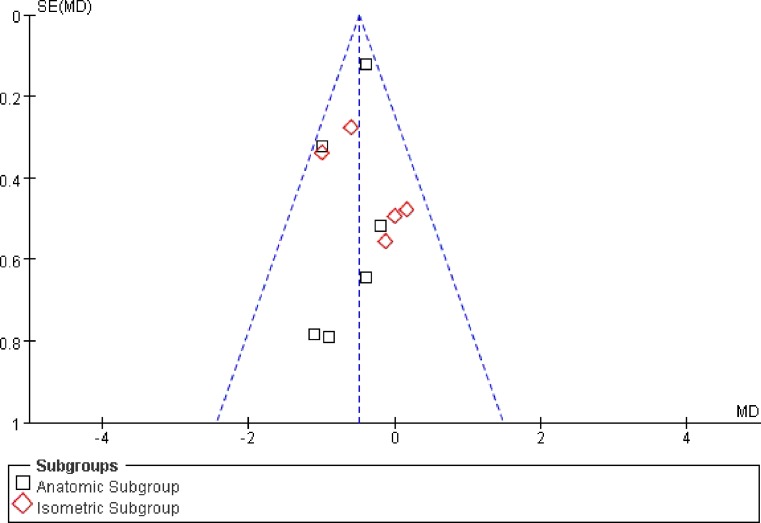
For the purpose of assessing publication bias, funnel plots were used in our study. Funnel plots can be used for reviews with sufficient numbers of included studies. Figure 14 shows a funnel plot of the 11 studies pooled for KT1000 arthrometer measurements reporting the standard difference in means as a measure of treatment effect. The x-axis represents the standard difference in means as a measure of treatment effect, whereas the y-axis represents a measure of study size. The plot demonstrates some mild asymmetry, but all studies fall within the 95 % CI axis for a given standard error. However, there is minimal evidence of publication bias.
Fig. 14.
Funnel plot showing minimal publication bias of KT1000 arthrometer measurements
Discussion
The ACL plays an important role in the motion of the knee joint, and it is the primary restraint to anterior tibial displacement. The exact incidence of ACL injuries is unknown. However, an estimated 80,000 ACL tears occur annually in the USA [36]. Surgical repair of the ACL is a fairly common necessity in knee injuries, especially with good to excellent outcomes. In an attempt to more closely recreate native anatomy and better replicate natural ACL function, anatomical double-bundle ACL reconstruction is popular with many surgeons. The earliest published discussions of double-bundle ACL reconstruction are from the 1980s [37, 38]. Since then, many studies reported that double-bundle reconstruction of the ACL reproduced better stability of a native knee [9, 22, 39–42]. Meta-analysis studies are considered to represent a high level of evidence when high-quality RCTs are combined in an appropriate fashion. To our knowledge, the latest systematic review including 13 studies concluded that the double-bundle may be better than the single-bundle ACL reconstruction technique in rotational stability but not for function, translation and complications [30]. However, there were some obvious limitations in the systematic review. First and most important, isometric and anatomical single-bundle reconstructions were taken together for analysis, so the comparison is not fair and of course the double-bundles do better. Second, the last search date was 27 April 2011, and many new RCTs have been published since [12–14, 16, 17, 23]. Third, a quasi-randomised trial and a prospective comparative study met the inclusion criteria. Therefore, the statistical power of the systematic review would be impaired. In this up-to-date meta-analysis, we statistically combined the results of all available evidence from RCTs to answer the question of whether the double-bundle reconstruction technique is a superior treatment for ACL ruptures. Based on the analysis of the latest RCTs [12–28], this study shows that there is no significance with Lysholm score, objective IKDC score, flexion deficit and knee isokinetic peak torques (flexor and extensor) between the two techniques, which corresponds with the previous studies. We also found that double-bundle reconstruction is superior to single-bundle reconstruction in graft failures, subjective IKDC score, extension deficit, pivot shift tests and KT1000 measurements.
There is a problem in most published articles comparing single- and double-bundle ACL reconstruction: one or both surgical techniques are not performed anatomically (transtibial single-bundle versus anatomical double-bundle) [12–14, 17, 18, 20, 21, 23, 25–27]. As a consequence, the results were controversial, mainly focused on single-bundle reconstruction. Whether the surgical technique of single-bundle reconstruction is anatomical or not is determined by the method used to create the femoral tunnel. The transtibial technique is defined as isometric reconstruction, and if the femoral tunnel and tibial tunnel are placed independently, mainly by a transportal technique, we define that as an anatomical reconstruction. It has been established that the true insertion site of the ACL on the femur is actually on the wall of the intercondylar notch and not on the roof [22]. However, the transtibial technique using the o’clock method can easily lead to a high and anterior position of the femoral tunnel, which will generate misconceptions because of the three-dimensional nature of the intercondylar notch, where the clock face can be put anywhere along the anterior to posterior axis [47, 48]. Moreover, cadaveric studies showed that the transtibial approach is not accurate both in single-bundle and double-bundle ACL reconstruction [49]. The problem was considered in this meta-analysis, so we believe that our results will be more meaningful.
Lysholm score, knee motion deficit (extension and flexion), and subjective and objective IKDC score were used in this study to evaluate the functional outcomes in ACL reconstruction. With regard to the subjective IKDC score, our pooled results showed that double-bundle reconstruction was superior to single-bundle reconstruction (P = 0.03). The forest plot showed that the double-bundle group has more advantages compared with the single-bundle group. Kondo et al. [42] and Aglietti et al. [19] reported that anatomical double-bundle reconstruction revealed some tendency towards superiority over the single-bundle reconstruction. Lee et al. [12] reported that the double-bundle group was superior to the single-bundle group in IKDC subjective score at the two-year follow-up. Not surprisingly, Hussein et al. [16] reported similar results. In contrast, Siebold et al. [25] reported that the average subjective IKDC score was higher in the single-bundle group than in the double-bundle group (90 points versus 88 points). The subjective IKDC score may be affected by the subjective view of different patients, so different results are possible and understandable.
As to Lysholm score and objective IKDC score, this meta-analysis shows no statistically significant difference with Lysholm score (P = 0.91) and objective IKDC score (P = 0.18) between the two groups, which is in accordance with most of the published studies [18, 19, 21, 22, 24–26]. The results of Sastre et al. [43] also suggested that there was no significant difference in Lysholm score between the two techniques, while Muneta et al. [27] reported that average points on the Lysholm knee scale were higher in the double-bundle group (94.5 points) compared with the single-bundle group (93.8 points). Because data on standard deviation were not given, the Lysholm score of this study was not included in this meta-analysis. Conversely, Araki et al. [15] demonstrated that the single-bundle group had a higher Lysholm score than the double-bundle group. However, no significant difference was found between the groups in the two studies. In this meta-analysis, we gathered the number of individuals with normal objective IKDC score (graded as A) at the follow-up. Järvelä [28] reported that the single-bundle group had more individuals with normal objective IKDC score than the double-bundle group, but it was equally good in both groups at follow-up. By contrast, Sastre et al. [43] found a statistically significant difference in favour of the double-bundle technique in terms of objective IKDC at the two-year follow-up. Generally, most studies reported there was no significant difference in terms of objective IKDC score between the two techniques. Likewise, similar results with Lysholm and objective IKDC score were seen in our study.
Niki et al. [44] found that knee extension deficit was an important predisposing factor for postoperative anterior knee pain in the early postoperative period. Concerning deficit of motion (extension and flexion), although we got the better statistical result favouring the double-bundle group in extension deficit, combined with subjective IKDC score results, we only conclude that there was a potential advantage in the double-bundle group compared with the single-bundle group in functional outcome, because the number of patients is small and the data are only from two studies.
The pivot-shift results, KT1000 measurements and isokinetic peak torques (flexor and extensor) were used in this study to evaluate the stability for ACL reconstruction. This meta-analysis demonstrated that the double-bundle technique was superior to the single-bundle technique in negative pivot-shift testing of the knee joint (P < 0.0001), which corresponds with the latest systematic review in favour of double-bundle reconstruction. In our study, many RCTs included were published in recent years [12–14, 16, 17, 23, 26], which were not included in the review [30]. It shows that double-bundle reconstruction has a lower risk of positive pivot-shift testing than single-bundle reconstruction. Finding no difference in pivot-shift results, Meredick et al. [46] concluded that their pivot-shift results did not support the theoretical advantage of double-bundle ACL reconstruction. In contrast, recently published RCTs and our study show that the superior rotational stability of the double-bundle group might protect the knee from a new injury, particularly in sports that involve pivoting. The pivot-shift results have particular clinical relevance, because the test was designed to evaluate knee rotational instability. Kondo et al. [42] in a prospective comparative study of 328 patients reported that anatomical double-bundle had significantly better results than single-bundle in terms of pivot shift. Rotational stability indicated that 93.1 % of the double-bundle group and 66.7 % of the single-bundle group had a negative pivot-shift result (P < 0.001) [16]. Cadaveric and biomechanical studies had proved that double-bundle ACL reconstruction was better for control of knee rotational instability [5, 45]. The result of our study is also in accordance with previous studies [15, 16, 18, 19, 22–28]. KT1000/2000 arthrometry is the most reliable parameter for measurement of anterior translation available. Differing from the previous review, this meta-analysis showed that there was a statistically significant difference with KT1000 between the two groups (P < 0.00001), with the double-bundle group being more stable. Muneta et al. [27] reported that anterior stability evaluated with the KT1000 arthrometer was superior in the double-bundle group to that in the single-bundle group, average 2.4 mm versus 1.4 mm, while Järvelä et al. [24] reported no group difference with anterior stability of the knee. In addition, they found that the correlation between the tunnel enlargement in the anteromedial tunnel and the anterior laxity of the knee was significant in both groups on the tibial side and femoral side. According to their findings, the greater the tunnel enlargement was, the worse the result was in terms of KT1000 measurements. Yasuda et al. [39] also reported that side-to-side KT2000 measurements of anatomical double-bundle ACL reconstruction showed significantly better results than in the single-bundle procedure. Considering the previous studies and our meta-analysis, we believe that the double-bundle technique is a safe and reliable technique for ACL reconstruction in anterior stability of the knee.
To our knowledge, the majority of previous studies reported few graft failures among either group. In comparison with single-bundle reconstruction, double-bundle reconstruction was proved to be advantageous in terms of graft failures in this meta-analysis (P = 0.002). Järvelä et al. [22] reported that one patient required a revision ACL reconstruction in the single-bundle group compared with one patient in the double-bundle group. In addition, revision ACL reconstructions were performed on those four patients in the single-bundle group in the study of Järvelä [28]. It seems that the double-bundle technique is more advantageous with respect to graft failures of ACL reconstruction.
Our study has some limitations to be considered. First, the follow-up periods were different in the included studies of this meta-analysis. Furthermore, several patients were lost to follow-up [12, 13, 17, 23, 24, 28]. This might weaken the strength of the results. Second, the sample size in some studies was small, which could increase the publication bias. As we know, any meta-analysis is subject to publication bias, regardless of using a funnel plot to evaluate the publication bias. Third, the quality of the primary studies can affect the strength of the conclusion of this study. Some studies did not have complete reporting, and this decreases the quality assessment in meta-analysis. Furthermore, the reports included in the literature of this meta-analysis are all English studies. Because of language restrictions, some RCTs in other languages were not evaluated in this meta-analysis. Notwithstanding these limitations, this meta-analysis does suggest there are more advantages of double-bundle reconstruction compared with single-bundle reconstruction of the ACL.
Conclusions
The current evidence in this meta-analysis does support the hypothesis that double-bundle ACL reconstruction would be advantageous in restoring stability and in functional outcome and in decreasing the risk of graft failures, compared with single-bundle reconstruction. The results indicated that arthroscopic double-bundle reconstruction should be considered as the primary treatment in ACL reconstruction.
Acknowledgments
Conflicts of interest
None.
Footnotes
Xue Li and Chang-peng Xu contributed equally to this study.
References
- 1.Zelle BA, Brucker PU, Feng MT, Fu FH. Anatomical double-bundle anterior cruciate ligament reconstruction. Sports Med. 2006;36:99–108. doi: 10.2165/00007256-200636020-00001. [DOI] [PubMed] [Google Scholar]
- 2.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35:223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 3.Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;106:216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 4.Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73:260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 5.Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84-A:907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kanamori A, Zeminski J, Rudy TW, Li G, Fu FH, Woo SL. The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy. 2002;18:394–398. doi: 10.1053/jars.2002.30638. [DOI] [PubMed] [Google Scholar]
- 7.Mae T, Shino K, Miyama T, Shinjo H, Ochi T, Yoshikawa H, Fujie H. Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy. 2001;17:708–716. doi: 10.1053/jars.2001.25250. [DOI] [PubMed] [Google Scholar]
- 8.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 9.Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 10.Park SJ, Jung YB, Jung HJ, Jung HJ, Shin HK, Kim E, Song KS, Kim GS, Cheon HY, Kim S. Outcome of arthroscopic single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a preliminary 2-year prospective study. Arthroscopy. 2010;26:630–636. doi: 10.1016/j.arthro.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Kanaya A, Ochi M, Deie M, Adachi N, Nishimori M, Nakamae A. Intraoperative evaluation of anteroposterior and rotational stabilities in anterior cruciate ligament reconstruction: lower femoral tunnel placed single-bundle versus double-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:907–913. doi: 10.1007/s00167-009-0757-5. [DOI] [PubMed] [Google Scholar]
- 12.Lee S, Kim H, Jang J, Seong SC, Lee MC. Comparison of anterior and rotatory laxity using navigation between single- and double-bundle ACL reconstruction: prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2012;20:752–761. doi: 10.1007/s00167-012-1880-2. [DOI] [PubMed] [Google Scholar]
- 13.Núñez M, Sastre S, Núñez E, Lozano L, Nicodemo C, Segur JM. Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort-a randomized trial with 2 years of follow-up. Arthroscopy. 2012;28:929–935. doi: 10.1016/j.arthro.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 14.Ochiai S, Hagino T, Senga S, Saito M, Haro H. Prospective evaluation of patients with anterior cruciate ligament reconstruction using a patient-based health-related survey: comparison of single-bundle and anatomical double-bundle techniques. Arch Orthop Trauma Surg. 2012;132:393–398. doi: 10.1007/s00402-011-1443-x. [DOI] [PubMed] [Google Scholar]
- 15.Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, Hoshino Y, Matsushita T, Matsumoto T, Nagamune K, Kurosaka M. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. 2011;35:439–446. doi: 10.1007/s00264-010-1110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3– to 5–year follow-up. Am J Sports Med. 2012;40:512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 17.Hemmerich A, van der Merwe W, Batterham M, Vaughan CL. Knee rotational laxity in a randomized comparison of single- versus double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:48–56. doi: 10.1177/0363546510379333. [DOI] [PubMed] [Google Scholar]
- 18.Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19:390–397. doi: 10.1007/s00167-010-1225-y. [DOI] [PubMed] [Google Scholar]
- 19.Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N. Comparison between single- and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med. 2010;38:25–34. doi: 10.1177/0363546509347096. [DOI] [PubMed] [Google Scholar]
- 20.Ibrahim SA, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H. Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br. 2009;91:1310–1315. doi: 10.1302/0301-620X.91B10.21886. [DOI] [PubMed] [Google Scholar]
- 21.Wang JQ, Ao YF, Yu CL, Liu P, Xu Y, Chen LX. Clinical evaluation of double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: a prospective, randomized and controlled study. Chin Med J (Engl) 2009;122:706–711. [PubMed] [Google Scholar]
- 22.Järvelä T, Moisala AS, Sihvonen R, Järvelä S, Kannus P, Järvinen M. Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med. 2008;36:290–297. doi: 10.1177/0363546507308360. [DOI] [PubMed] [Google Scholar]
- 23.Suomalainen P, Moisala AS, Paakkala A, Kannus P, Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med. 2011;39:1615–1622. doi: 10.1177/0363546511405024. [DOI] [PubMed] [Google Scholar]
- 24.Järvelä T, Moisala AS, Paakkala T, Paakkala A. Tunnel enlargement after double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study. Arthroscopy. 2008;24:1349–1357. doi: 10.1016/j.arthro.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:137–145. doi: 10.1016/j.arthro.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 26.Streich NA, Friedrich K, Gotterbarm T, Schmitt H. Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc. 2008;16:232–238. doi: 10.1007/s00167-007-0480-z. [DOI] [PubMed] [Google Scholar]
- 27.Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy. 2007;23:618–628. doi: 10.1016/j.arthro.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc. 2007;15:500–507. doi: 10.1007/s00167-006-0254-z. [DOI] [PubMed] [Google Scholar]
- 29.Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y. Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br. 2004;86:515–520. [PubMed] [Google Scholar]
- 30.Kongtharvonskul J, Attia J, Thamakaison S, Kijkunasathian C, Woratanarat P, Thakkinstian A (2012) Clinical outcomes of double- vs single-bundle anterior cruciate ligament reconstruction: a systematic review of randomized control trials. Scand J Med Sci Sports. doi: 10.1111/j.1600-0838.2011.01439.x [DOI] [PubMed]
- 31.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 32.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 33.Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R. Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am. 1985;67:720–726. [PubMed] [Google Scholar]
- 34.Moher D, Schulz KF, Altman DG, CONSORT Group The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials 2001. Explore (NY) 2005;1:40–45. doi: 10.1016/j.explore.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, Garrick JG, Hewett TE, Huston L, Ireland ML, Johnson RJ, Kibler WB, Lephart S, Lewis JL, Lindenfeld TN, Mandelbaum BR, Marchak P, Teitz CC, Wojtys EM. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Mott HW. Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin Orthop Relat Res. 1983;172:90–92. [PubMed] [Google Scholar]
- 38.Zaricznyj B. Reconstruction of the anterior cruciate ligament of the knee using a doubled tendon graft. Clin Orthop Relat Res. 1987;220:162–175. [PubMed] [Google Scholar]
- 39.Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006;22:240–251. doi: 10.1016/j.arthro.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 40.Radford WJ, Amis AA. Biomechanics of a double prosthetic ligament in the anterior cruciate deficient knee. J Bone Joint Surg Br. 1990;72:1038–1043. doi: 10.1302/0301-620X.72B6.2147184. [DOI] [PubMed] [Google Scholar]
- 41.Fujita N, Kuroda R, Matsumoto T, Yamaguchi M, Yagi M, Matsumoto A, Kubo S, Matsushita T, Hoshino Y, Nishimoto K, Araki D, Kurosaka M. Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy. 2011;27:906–913. doi: 10.1016/j.arthro.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 42.Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T. Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med. 2008;36:1675–1687. doi: 10.1177/0363546508317123. [DOI] [PubMed] [Google Scholar]
- 43.Sastre S, Popescu D, Núñez M, Pomes J, Tomas X, Peidro L. Double-bundle versus single-bundle ACL reconstruction using the horizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2010;18:32–36. doi: 10.1007/s00167-009-0844-7. [DOI] [PubMed] [Google Scholar]
- 44.Niki Y, Hakozaki A, Iwamoto W, Kanagawa H, Matsumoto H, Toyama Y, Suda Y. Factors affecting anterior knee pain following anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1543–1549. doi: 10.1007/s00167-011-1746-z. [DOI] [PubMed] [Google Scholar]
- 45.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 46.Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 47.Hensler D, Illingworth K, Fu FH. Principle consideration in anatomic ACL reconstruction. Arthroscopy. 2010;26:1414–1415. doi: 10.1016/j.arthro.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 48.Shen W, Forsythe B, Ingham SM, Honkamp NJ, Fu FH. Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am. 2008;90(Suppl 4):20–34. doi: 10.2106/JBJS.H.00919. [DOI] [PubMed] [Google Scholar]
- 49.Giron F, Cuomo P, Edwards A, Bull AMJ, Amis AA, Aglietti P. Double-bundle “anatomic” anterior cruciate ligament reconstruction: a cadaveric study of tunnel positioning with a transtibial technique. Arthroscopy. 2007;23:7–13. doi: 10.1016/j.arthro.2006.08.008. [DOI] [PubMed] [Google Scholar]