Abstract
Purpose
A positive glide is a common finding after ACL reconstructions, especially in women. The aim of this study was to prospectively evaluate the role of Cocker-Arnold’s extra-articular procedure in reducing the incidence of a residual postoperative rotational knee laxity.
Methods
Sixty patients affected by an ACL injury with a +2 (clunk) or +3 (gross shift) pivot-shift test entered this prospective study; they were randomly assigned to group A (control group, hamstrings) or group B (study group, hamstrings plus Cocker-Arnold). Thirty-two patients entered group A and 28 group B. At follow-up, patients underwent clinical evaluation, KT-1000 arthrometer and Lysholm, Tegner, VAS and subjective and objective IKDC form.
Results
At a mean follow-up of 44.6 months, the same expert surgeon reviewed 55 patients (28 group A and 27 group B). The comparison of the results of the evaluation scales used and of the KT-1000 arthrometer did not show statistically significant differences (p > 0.05). Lachman test was negative (S/S) in all the patients of both groups (100 %). A residual positive pivot-shift (glide) was found in 16 patients (57.1 %) of group A and in five patients (18.6 %) of group B (p < 0.05).
Conclusions
The extra-articular MacIntosh procedure modified by Cocker-Arnold in combination with ACL reconstruction significantly reduces the rotational instability of the knee.
Introduction
Today more women are participating in competitive and recreational sports activities, with a concomitant higher incidence of ACL injuries in female athletes [1–7]. Many authors [1, 8–11] have already shown how postoperative results are usually worse in women than men after ACL reconstruction with hamstrings (HS). Even though some authors [12–15] have stated that a greater postoperative knee laxity in women does not necessarily correlate to poorer clinical results, it is a matter of concern as to what will be the clinical outcome of such patients in long-term follow-up.
The role of extra-articular procedures improving postoperative knee stability has been a matter of debate, especially with regard to the rotational component (glide); and while authors such as Roth et al. [16], Strum et al. [17] and Barret et al. [18] found no significant improvements with the use of extra-articular plasty, Lerat et al. [19], Noyes et al. [20] and Zaffagnini et al. [21] found an increased success rate with the addition of an extra-articular procedure.
In order to better understand the real, effective, stabilizing role of extra-articular procedures in ACL reconstruction in females, we carried out a prospective randomized study in which we compared two groups of active female patients treated with autogenous four-strand hamstrings either without or with an extra-articular procedure. We also sought to examine the relationship between postoperative residual laxity and self-reported functional results.
The null hypothesis was that the use of a peripheral plasty in addition to ACL reconstruction with hamstrings provides higher knee stability than ACL reconstruction alone.
Materials and methods
Between January 2005 and December 2006, 124 female patients were operated on for chronic ACL instability at our Orthopaedic Department. Inclusion criteria to enter this study was the presence of a moderate to severe rotatory instability as revealed by a pivot-shift test graded as +2 or +3 (in a laxity scale ranging from score 0 negative, +1 glide, +2 clunk, to +3 gross shift), a minimum interval of two months between trauma and surgery and an age less than 40 years old. Exclusion criteria were previous surgical procedures on the same or on the contralateral knee, with concomitant injury of the internal or the external collateral ligament; concomitant systemic diseases; pre-operative radiological signs of knee arthritis; and imaging evidence of grades III or IV chondral damage on both patellar surface or medial and lateral femoral condyles, according to the International Cartilage Repair Society. On the contrary, the presence of concomitant medial or lateral meniscal lesions was not considered an exclusion criterium. All patients included in the study were pre-operatively evaluated by the same expert surgeon (A.F.).
Out of the 124 operated, 60 patients were recruited to enter this prospective study and were consequently designated by a draw to group A (32 patients, ACL reconstruction with hamstrings) or group B (28 patients, ACL reconstruction with hamstrings plus extra-articular MacIntosh procedure modified by Cocker-Arnold).
The mean age of the patients at the time of surgery was 27 years (range, 15–40 years). In group A the right side was involved in 15 (46.8 %) cases and the left side in 17 (53.2 %), while in group B the right side was involved in 16 (57.1 %) cases and the left side in 12 (42.9 %).
Pre-operatively all patients were clinically evaluated with the Lachman test [22] which was graded (S/S) as: 0, negative; +1, negative but with a slightly longer endpoint; +2, positive. The pivot-shift test [19] was also tested and graded as 0, negative; +1, glide; +2, clunk; +3, gross shift). All patients had a normal range of motion. Patients were also given the Lysholm knee score [15, 23], Tegner activity level [24] and International Knee Documentation Committee (IKDC) 2000 forms [25]. Joint laxity was assessed with the KT-1000 arthrometer (MED Metric Corp., San Diego, CA, USA) by measuring the side-to-side (S/S) differences in displacement at manual maximum (MM) testing.
All patients considered in this study were involved in sports activity either as professionals or as amateurs. They all gave their informed consent to participate in the study.
Surgical technique
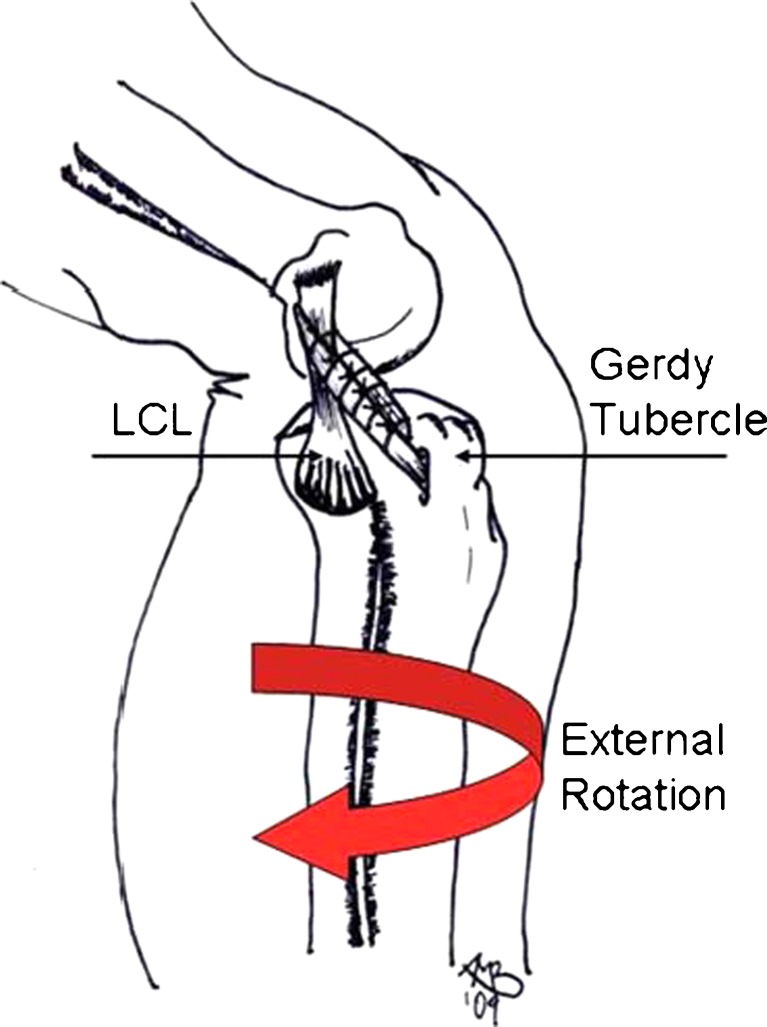
In patients of both groups, the ACL reconstruction consisted of an anatomical Out-In technique, with autogenous semitendinosus and gracilis tendons passed from the femoral toward the tibial side and securely fixed with biomechanically proven nonabsorbable fixation devices [26, 27]. While the recovery of knee stability in patients of group A was entirely achieved by reconstruction of the torn ACL with four-strand hamstring tendons, the patients of group B were operated on with an additional extraarticular MacIntosh modified Coker-Arnold procedure. After slightly extending the lateral femoral incision (used to pass the new ACL ligament through) toward the Gerdy’s tubercle, a strip of iliotibial tract, approximately 8–10 cm long and 1 cm wide, was obtained from the iliotibial band. The strip was then proximally cut free and passed under the lateral collateral ligament (LCL) in an anterior-to-posterior direction, then looped back on itself and sutured to the Gerdy’s tubercle with #0 Vycril suture, while the knee was flexed and in maximal external rotation. The iliotibial tract was also sutured to the LCL for additional stability (Fig. 1).
Fig. 1.
Extra-articular MacIntosh modified Coker-Arnold procedure
Rehabilitation protocol
The postoperative protocol was the same for all patients of both groups. The knee was locked in full extension with the use of a brace, in order to protect the reconstructed ACL, to facilitate its integration within the bone tunnels and thus avoiding the bone tunnel enlargement. Partial weightbearing was allowed the second postoperative day, with the use of two crutches, as well as isometric exercises and hamstrings stretching. Recovery of range of motion was started at the end of the second postop week, when the brace was unlocked to 0–90°. At the beginning of the second postop month the brace was completely removed, and the patient started a progressive program of muscular strengthening and recovery of the remaining degrees of flexion. Return to sports activity was allowed starting from the fifth postop month.
Follow-up evaluation
All patients were followed-up at a mean of 44.6 months (range, 36–50). Out of the 60 patients pre-operatively considered in this study, 55 were available for final follow-up: 28 patients for group A and 27 for group B. An independent examiner (A.V.), not involved in any of the surgical procedures, performed the physical examination of all patients. Subjectively, patients reported a visual analog scale score (VAS score of 0, no pain; 10, unbearable pain) and were asked to judge the clinical outcome of the surgical procedure they had undergone. Objectively, they underwent physical examination using the Lachman test, pivot-shift test, and evaluation of ROM (side-to-side). Moreover they underwent the Tegner scale, the Lysholm knee score and IKDC 2000 score, and were given the manual maximum KT-1000 arthrometer test.
Statistical method
Statistical analysis was performed using SAS software (version 9.1). The results between the two groups have been compared through the Wilcoxon test and the chi-square test; the relationship between variables have been assessed through logistic models. A P value of less than 0.05 (5 %) was interpreted as being a significant difference between variables.
Results
All patients were called for follow-up at a mean of 44.6 months (range, 36–50). No postoperative complications (such as infection, deep venous thrombosis or nerve injuries) were detected in either of the two groups.
Group A, without extra-articular procedure
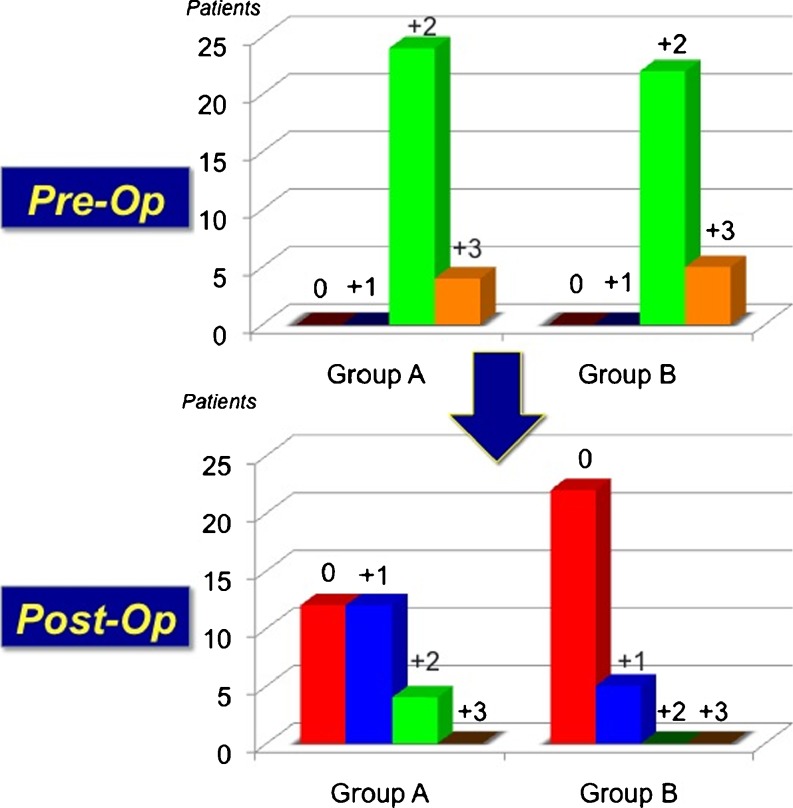
Out of the 32 patients of group A, four patients were not available for follow-up: two patients (6.2 %) because of a reported re-rupture of the ACL (which occurred in one case during a soccer match and in the other case during a volleyball match), and the other two (6.2 %) because of living too far away from our city. As a consequence, we followed-up 28 patients of this group. The mean follow-up was 43.1 months (range, 36–50). The mean age of this group was 28 years (range, 15–40 years). Six patients (21.4 %) underwent a medial partial selective meniscectomy, three patients (10.7 %) an external partial meniscectomy, and two patients (7.1 %) a concomitant medial and lateral partial meniscectomy. Subjectively, the mean VAS score was 0.96 ± 0.8 (range 0–3); 20 patients (71.4 %) judged their clinical outcome as excellent and eight patients (28.6 %) judged theirs as good. At physical examination, the Lachman test was judged as negative in 20 patients (71.4 %), and as +1 in eight patients (28.6 %). The pivot-shift test was judged negative in 12 patients (42.9 %) and positive in 16 patients (57.1 %), in specific, a grade +1 pivot-shift test was detected in 12 patients (42.9 %) and in the other four patients (14.2 %) a grade +2 was found (Fig. 2). However, all patients reported a satisfactory feeling of stability in the operated knee, despite the result of the pivot-shift test detected at physical examination. Final range of motion was complete (S/S) in all patients. The average score of the Tegner scale decreased from a pre-operative value of 7.4 ± 1.24 to 6.7 ± 1.35 at follow-up; the mean value of the Lysholm scale raised from 56.3 ± 3.12 to 94.5 ± 6.65. The mean value of the objective IKDC form at follow-up was 93.7 ± 3.38, specifically, 21 patients (75 %) entered level A and seven patients (25 %) level B. The subjective IKDC score improved from 72 ± 2.3 points (range, 51–100 points) to 87 ± 1.8 points (range, 54–100 points). The mean anterior laxity difference between the involved knee and the contralateral healthy knee dropped from 10.2 ± 0.77 mm to 2.8 ± 0.77 mm at maximum manual handling.
Fig. 2.
Pre- and post-operative Pivot-Shift values
Group B, with extra-articular procedure
Out of the 28 patients of group B, one patient was not able to be present because he moved away for work purposes. As a consequence, we followed-up 27 patients of this group. The mean follow-up was 45.2 months (range, 38–50). The mean age of this group was 26 years (range, 15–40 years).
Seven patients (25.9 %) underwent an internal partial selective meniscectomy, and three patients (11.1 %) an external partial meniscectomy. Subjectively, the mean VAS score was 1 ± 0.86 (range 0–3); 19 patients (70.3 %) judged their clinical outcome as excellent and eight patients (29.7 %) judged theirs as good. At physical examination, the Lachman test was judged as negative in 16 patients (59.3 %) and as +1 in 11 patients (40.7 %). The pivot-shift test was judged as negative (grade 0) in 22 patients (81.4 %) and as positive (grade + 1) in five patients (18.6 %) (Table 1). All patients of group B reported a satisfactory feeling of stability in the operated knee. Final range of motion was complete (S/S) in all patients. The average score of the Tegner scale decreased from a pre-operative value of 7.9 ± 0.88 to 7.5 ± 1.15 at follow-up; the mean value of the Lysholm scale raised from 53.4 ± 4.22 to 95.8 ± 3.99. The mean value of the objective IKDC form at follow-up was 94.2 ± 3.33; 22 patients (81.4 %) entered level A and five patients (18.6 %) level B. The subjective IKDC score improved from 71 ± 1.2 points (range, 49–99 points) to 89 ± 1.5 points (range, 61–100 points). The mean anterior laxity difference between the involved knee and the contralateral healthy knee dropped from 10.9 ± 0.7 mm to 2.7 ± 0.89 mm at maximum manual handling.
Table 1.
Methodology used to value the difference between the two groups referring to the variable, the statistic value and the related type I error
| Variable | Methodology | Value | P |
|---|---|---|---|
| Pivot-shift | Wilcoxon | 2.7397 | 0.0031 |
| Lachman | Chi-square | 1.2528 | 0.263 |
| Tegner | Wilcoxon | 0.5157 | 0.302 |
| Lysholm | Wilcoxon | 1.8443 | 0.062 |
| Sub. IKDC | Wilcoxon | 1.7837 | 0.087 |
| Obj. IKDC | Wilcoxon | 0.2753 | 0.391 |
| KT-1000 MM | Wilcoxon | 2.3549 | 0.402 |
| VAS | Wilcoxon | 0.1499 | 0.4404 |
Comparison of data (Table 1) between the two groups shows similar results in regard to all the variables considered except for the pivot-shift test, which was negative (grade 0) in the vast majority of patients of group B (81.4 % vs. 42.9 of group A). Analysis of the logistics model clearly shows how the "postop pivot-shift" variable was highly correlated (p = 0.001) to the group in which patients belonged.
Discussion
The most important finding of this study was the statistically significant better results we gathered in the group of female patients operated on for ACL reconstruction in which a peripheral plasty was added with the aim to further reduce the rotatory instability of the knee. In fact, because of the results published by many authors showing less successful results in female patients than in male patients [1, 9, 11], we carried out this study in order to well define the effectiveness that an additional extra-articular tenodesis might have in preserving the reconstructed ACL, and reducing the postoperative rotatory instability in female patients. In this study we aimed to assess the efficacy of an additional extra-articular plasty in reducing the potential postoperative rotational laxity. The hardest part of this study was to gather a homogenous group of patients to follow. The entity of joint laxity had the potential for being very wide among the female patients we wanted to examine; for this reason we decided to accurately examine the patients before the operation and to consider only those patients whose pre-operative rotational laxity was graded as +2 or greater. The same author evaluated all the patients selected for this study by testing the rotational instability of the knee with the pivot-shift test. This selection criteria was done with the aim of having a homogeneous group of patients to follow up. The lack of this type of selection would have made the group of patients very heterogeneous with low evidence-based reliability. As described above we carefully followed the inclusion/exclusion criteria in order to avoid potential bias due to concomitant lesions, such as internal or external collateral injuries or chondral damages. The rational of combining intra- and extra-articular procedures in ACL reconstruction is to restrict the internal rotation of the reconstructed knee, thus providing more stability in the knee in the rotational axis and preventing the ACL graft from undergoing further excessive stress. Many studies have already investigated the role of such extra-articular procedures [16, 17, 19–21, 28, 29]. Anderson et al. [30], as well as Roth et al. [16], showed no improvement by the addition of an extra-articular procedure. Completely different conclusions were shown by Lerat et al. [19] and Noyes et al. [20], which showed the results of two prospective studies with significantly better results in patients with an extra-articular procedure. More recently, Monaco et al. [30], using a navigator system demonstrated that the addition of a lateral extra-articular tenodesis procedure to a standard single bundle ACL reconstruction was more effective in reducing the internal rotation of the tibia, when compared with a standard single bundle ACL reconstruction or with an anatomic double bundle reconstruction. In our experience, we registered two cases of failure among patients without peripheral tenodesis and no cases among patients with the extra-articular procedure. The results of our study show no significant differences between the two groups with regard to subjective postoperative feeling of knee stability or objective evaluation scales performed. However, patients of group B showed a significantly higher percentage of negative (grade 0) pivot-shift test results compared to group A, which might be due to the presence of the additional extra-articular procedure performed. Moreover, while two patients of group A experienced a rerupture, this data did not occur among patients of group B. Among the evaluation scales used, while the Lysholm and the IKDC showed significant better results at follow-up, the Tegner scale showed lower results in both groups, although without a significant difference between the two groups. This might be due to the fact that not all the patients included in this study were regularly practicing sports activity and the score they chose was a consequence of residual fear to return to the pre-operative sport activity level. The main drawback of the study is certainly represented by the highly subjective capability of judging the pivot-shift test; however, because of the lack of standardized objective tests that exist to test the rotatory instability of the knee, our best option was to have an independent expert examiner who blindly followed-up all the patients. Moreover, despite the hypothesized arthritic degeneration potentially arising from the use of an extra-articular procedure, we did not assess the radiological degeneration of the knee at follow-up; however, we never clinically reported signs of femoro-patellar symptoms.
In conclusion, the combination of an extra-articular MacIntosh procedure modified by Cocker-Arnold with ACL reconstruction seems to significantly reduce the rotational instability of the knee.
Acknowledgement
We would like to acknowledge Dr. Gianluca Mastrantonio for the statistical analysis and Mrs. Angela Mitchell for the technical support in performing the study.
References
- 1.Noojin FK, Barrett GR, Hartzog CW, Nash CR. Clinical comparison of intraarticular anterior cruciate ligament reconstruction using autogenous semitendinosus and gracilis tendons in men versus women. AmJ Sports Med. 2000;28(6):783–789. doi: 10.1177/03635465000280060301. [DOI] [PubMed] [Google Scholar]
- 2.Besier TF, Lloyd DG, Cochrane JL, Ackland TR. External loading of the knee joint during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33:1168–1175. doi: 10.1097/00005768-200107000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Bjordal JM, Arnly F, Hannestad B, Strand T. Epidemiology of anterior cruciate ligament injuries in soccer. Am J Sports Med. 1997;25:341–345. doi: 10.1177/036354659702500312. [DOI] [PubMed] [Google Scholar]
- 4.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 5.Ferrari JD, Bach BR, Jr, Bush-Joseph CA, Wang T, Bojchuk J. Anterior cruciate ligament reconstruction in men and women: an outcome analysis comparing gender. Arthroscopy. 2001;17:588–596. doi: 10.1053/jars.2001.24686. [DOI] [PubMed] [Google Scholar]
- 6.Ferretti A, Papandrea P, Conteduca F, Mariani PP. Knee ligament injuries in volleyball players. Am J Sports Med. 1992;20:203–207. doi: 10.1177/036354659202000219. [DOI] [PubMed] [Google Scholar]
- 7.Toth AP, Cordasco FA. Anterior cruciate ligament injuries in the female athlete. J Gend Specif Med. 2001;4:25–34. [PubMed] [Google Scholar]
- 8.Biau DJ, Katsahian S, Kartus J, et al. Patellar tendon versus hamstring tendon autograft for reconstructing the anterior cruciate ligament: a metaanalysis based on individual patient data. Am J Sports Med. 2009;37(12):2470–2478. doi: 10.1177/0363546509333006. [DOI] [PubMed] [Google Scholar]
- 9.Gobbi A, Domzalski M, Pascual J. Comparison of anterior cruciate ligament reconstruction in male and female athletes using the patellar tendon and hamstring autografts. Knee Surg Sports Traumatol Arthrosc. 2004;12:534–539. doi: 10.1007/s00167-003-0486-0. [DOI] [PubMed] [Google Scholar]
- 10.Salmon LJ, Refshauge KM, Russell VJ, Roe JP, Linklater J, Pinczewski LA. Gender differences in outcome after anterior cruciate ligament reconstruction with hamstring tendon autograft. Am J Sports Med. 2006;34(4):621–629. doi: 10.1177/0363546505281806. [DOI] [PubMed] [Google Scholar]
- 11.Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament: a comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(4):444–454. doi: 10.1177/03635465990270040701. [DOI] [PubMed] [Google Scholar]
- 12.Barrett GR, Noojin FK, Hartzog CW, Nash CR. Reconstruction of the anterior cruciate ligament in females: a comparison of hamstring versus patellar tendon autograft. Arthroscopy. 2002;18:46–54. doi: 10.1053/jars.2002.25974. [DOI] [PubMed] [Google Scholar]
- 13.Hill PF, Russell VJ, Salmon LJ, Pinczewski LA. The influence of supplementary tibial fixation on laxity measurements after anterior cruciate ligament reconstruction with hamstring tendons in female patients. Am J Sports Med. 2005;33(1):94–101. doi: 10.1177/0363546504268036. [DOI] [PubMed] [Google Scholar]
- 14.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 15.Lavoie P, Fletcher J, Duval N. Correlation between patients’ satisfaction and objective measurement of knee stability after ACL reconstruction using a patellar tendon autograft. Knee. 2001;8:19–24. doi: 10.1016/S0968-0160(00)00076-4. [DOI] [PubMed] [Google Scholar]
- 16.Roth JH, Kennedy JC, Lockstadt H, et al. Intra-articular reconstruction of the anterior cruciate ligament with and without extra-articular supplementation by transfer of the biceps femoris tendon. J Bone Joint Surg. 1987;69(2):275–278. [PubMed] [Google Scholar]
- 17.Strum GM, Fox JM, Ferkel RD, et al. Intraarticular versus intraarticular and extraarticular reconstruction for chronic anterior cruciate ligament instability. Clin Orthop. 1989;245:188–198. [PubMed] [Google Scholar]
- 18.Barrett GR, Richardson KJ. The effect of added extraarticular procedure on results of ACL reconstruction. Am J Knee Surg Winter. 1995;8(1):1–6. [PubMed] [Google Scholar]
- 19.Lerat JL, Chotel F, Besse JL, et al. Les résultats après 10 à 16 ans du traitement de la laxité chronique antérieure du genou par une reconstruction du ligament croisé antérieur avec une greffe de tendon rotulien associée à une plastie extra-articulaire externe. A propos de 138 cas. Rev Chir Orthop Reparatrice Appar Mot. 1998;84(8):712–727. [PubMed] [Google Scholar]
- 20.Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73(6):882–892. [PubMed] [Google Scholar]
- 21.Zaffagnini S, Marcacci M, Lo Presti M, et al. Prospective and randomized evaluation of ACL reconstruction with three techniques. A clinical and radiographic evaluation at 5 year follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1060–1069. doi: 10.1007/s00167-006-0130-x. [DOI] [PubMed] [Google Scholar]
- 22.Torg J, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 23.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 24.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–44. [PubMed] [Google Scholar]
- 25.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 26.Ferretti A, Conteduca F, Labianca L, et al. Evolgate fixation of doubled flexor graft in acl reconstruction: biomechanical evaluation with cyclic loading. Am J Sports Med. 2005;33(4):574–582. doi: 10.1177/0363546504269721. [DOI] [PubMed] [Google Scholar]
- 27.Ferretti A, Conteduca F, Morelli F, et al. The evolgate, a method to improve the pull-out strength of interference screw in tibial fixation of ACL reconstruction with DGST. Arthroscopy. 2003;19(9):936–940. doi: 10.1016/j.arthro.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Arnold C, Van Bell C, Rogers V, et al. The relationship between serum relaxin and knee joint laxity in female athletes. Orthopedics. 2000;25:669–673. doi: 10.3928/0147-7447-20020601-18. [DOI] [PubMed] [Google Scholar]
- 29.Bak K, Jorgensen U, Ekstrand J, et al. Results of reconstruction of acute ruptures of the anterior cruciate ligament with an iliotibial band autograft. Knee Surg Sports Traumatol Arthrosc. 1999;7:111–117. doi: 10.1007/s001670050132. [DOI] [PubMed] [Google Scholar]
- 30.Anderson AF, Snyder RB, Lipscomb AB., Jr Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med. 2001;29:272–279. doi: 10.1177/03635465010290030201. [DOI] [PubMed] [Google Scholar]
- 31.Monaco E, Labianca L, Conteduca F, et al. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1168–1174. doi: 10.1007/s00167-007-0368-y. [DOI] [PubMed] [Google Scholar]