Abstract
Purpose
The aim of the study was to compare three different procedures performed by the same surgeon: mono-bundle patellar tendon reconstruction (bone-patellar tendon-bone, BPTB), double-bundle hamstring reconstruction (DBH) and mono-bundle patellar tendon combined with extra-articular reconstruction (Lemaire) (BPTB + L).
Methods
A total of 75 patients (25 in each group) were evaluated at a mean follow-up of 25 months. Laxity was assessed pre- and post-operatively with Telos™ stress radiographs (15 kg). The amount of anterior tibial translation (ATT) corrected by the surgery was quantified. Secondary outcomes were International Knee Documentation Committee (IKDC) scores, pivot shift grading, pain complaints, sensory deficits, subsequent surgical procedures, return to sports and patients’ ability to kneel or squat on their affected knee.
Results
Absolute correction of ATT for the internal compartment was not statistically significant [analysis of variance (ANOVA), p = 0.377]. For the external compartment BPTB + L (8.2 mm) showed superiority over DBH (5.6 mm) and BPTB (4.1 mm) (ANOVA, p = 0.0001, Tukey’s test). Kneeling was better in the DBH group (ANOVA, p = 0.0001, Tukey’s test). In 22 patients it felt normal, while only in seven in the BPTB and eight in the BPTB + L groups. Sensory deficits were present in 11 patients from the DBH group, while in 17 in the BPTB and 19 in the BPTB + L groups (ANOVA, p = 0.052). Mean IKDC values, presence of anterior knee pain, subsequent operations, ability to squat and return to sports were not statistically different between groups.
Conclusions
Absolute correction of ATT was not statistically different for the medial compartment, but the patellar tendon reconstruction combined with the extra-articular procedure achieved the best lateral compartment ATT correction. Sensory deficits and kneeling seem to be worse in the groups where the patellar tendon is harvested.
Introduction
Considerable controversy exists about the best procedure for anterior cruciate ligament (ACL) reconstruction. Numerous publications focusing on the number of bundles (mono- or double-bundle reconstruction) have been published recently as a result of this controversy [1–4].
The graft choice has also been extensively debated. The main controversy lies in the choice between the hamstrings or the patellar tendon. Many conflicting publications exist with no real consensus. Improved long-term stability in the patellar tendon group and decreased sensory deficits in the hamstrings group are some of the tendencies shown in these studies [5–11].
Addition of an extra-articular procedure to the standard intra-articular reconstruction is another important item. The extra-articular procedure adds stability to the procedure, but it is not an anatomical procedure and some complications such as stiffness and lateral pain with degenerative changes are described. Most of the publications focus on these extra-articular procedures for revision surgery, thus preventing conclusions on the efficacy and results in the primary setting. Also, few comparative data including these procedures exist [8, 12–14].
Finally, outcome measures are recorded in different ways in different studies, making it even more difficult to compare techniques [15]. The choice of procedure is based primarily upon the surgeon’s preference and experience.
The primary purpose of this study is to evaluate and compare three different procedures in ACL reconstruction—double-bundle hamstring (DBH), mono-bundle patellar tendon (bone-patellar tendon-bone, BPTB) and mono-bundle patellar tendon combined with an extra-articular reconstruction (Lemaire) (BPTB + L) with respect to stability. In our hypothesis, DBH and BPTB + L should perform better regarding restoration of stability (i.e. should achieve the greater correction and the lower post-operative anterior tibial translation values).
Secondary goals included comparing International Knee Documentation Committee (IKDC) scores, pivot shift grading, rates of return to sports, development of anterior knee pain, new surgical procedures needed, post-operative sensory deficits, and ability to kneel and crouch after the procedures. In our hypothesis IKDC scores should be similar, and the development of anterior knee pain, post-operative sensory deficits, and ability to kneel and crouch should be worst in the groups using the patellar tendon as the graft source.
Methods
In all, 75 patients, 25 for each of the three groups formed, were recruited from a total of 196 ACL reconstructions performed in 2005 by the senior surgeon (DD). All patients had been operated on for an ACL tear. They had been investigated preoperatively by clinical examination, magnetic resonance imaging and bilateral Telos™ (15 kg) stress radiographs. Previous knee surgery, associated lesions of other ligaments, other known diseases, injury to the opposite knee and pre-existing arthritis in the affected knee constituted the exclusion criteria. Patients with greater laxity (gross pivot shift and side-to-side Telos difference greater than 9 mm) had been allocated to the BPTB-L group. For the remaining patients, the decision to perform mono- or double-bundle procedures was determined by the graft chosen, and graft choice was based on sports participation: those who practised jumping sports with no internal rotation were allocated to the hamstrings group, and those who played sports with internal rotation (soccer and high-level skiing) had a BPTB procedure. This strategy was used with the intent to weaken the muscles most used during the preferred sport to a lesser extent, allowing patients to recover in better condition as soon as possible [16]. For the hamstring technique, the femoral fixation needed a double tunnel because of the absence of any fixation device [17], while for the patellar tendon a single-bundle technique was used.
The three types of surgery were:
Double-bundle hamstring loop technique (DBH) [17]: A double-bundle ACL reconstruction is performed under arthroscopy. The semitendinosus and gracilis tendons are harvested maintaining their tibial insertion intact and sutured to each other to make a double-stranded 25-cm long graft. One single tibial tunnel of 8 mm, one 6-mm femoral anteromedial (AM) and one 6-mm femoral posterolateral (PL) tunnels are drilled. The graft is pulled first into the tibial tunnel, looped through the femoral posterolateral and anteromedial tunnels, and back through the tibial tunnel keeping the native position between AM and PL bundles. Fixation is achieved in full extension with a 9/25 mm (Ligafix® 60 SBM 9/25 mm) absorbable interference screw into the tibia. No femoral fixation is needed since the graft is passed in a loop through both tunnels and supported by the femoral external cortex.
Single-bundle BPTB: After graft harvesting, the procedure is performed under arthroscopy. One tibial and one femoral tunnel are drilled, preserving the native ACL stump as a landmark. The femoral tunnel is perforated from outside in, at the 10 o’clock position. The graft is passed from the femur into the tibia. Press-fit fixation is employed on the femur, and a 9/25 mm (Ligafix® 30 SBM 9/25 mm) absorbable interference screw is used to achieve fixation on the tibial side at 10° of knee flexion.
Mono-bundle BPTB associated with a modified Lemaire’s extra-articular reconstruction (BPTB + L): The BPTB part of the procedure is carried out as described above and reinforced by an extra-articular modified Lemaire’s procedure [18, 19], performed with a free gracilis tendon. The gracilis tendon is harvested and detached from its tibial insertion, prepared on a side table. Through a lateral incision, the graft is then passed in a loop into a semicircular tunnel located at the isometric point just above the lateral collateral ligament femoral insertion, and the two strands pass under the lateral collateral ligament. One strand is passed into a tunnel at Gerdy’s tubercle and then sutured back to the other strand.
Post-operative care was identical for all three groups and included hospital stay for three days. Physiotherapy for full range of motion was started immediately. After hospital discharge, the patients were referred to a rehabilitation service. Visits to the assistant surgeon were at 45 days, three months and seven months after the surgery, when return to sports was allowed. The rehabilitation protocol prescribed was identical in all groups.
All patients were evaluated with a mean follow-up of two years. An independent orthopaedic surgeon (WV) evaluated all patients clinically and radiographically. Clinical data collected included IKDC objective and subjective forms. Sex, side of lesion, age, time from injury to surgery and follow-up were recorded for comparison. All patients were submitted again to Telos™ stress radiographs at approximately 20° of knee flexion and with 15 kg of anterior translation for both knees (the operated and the other normal knee) and the absolute and side-to-side (SS) anterior tibial translation (ATT) were recorded.
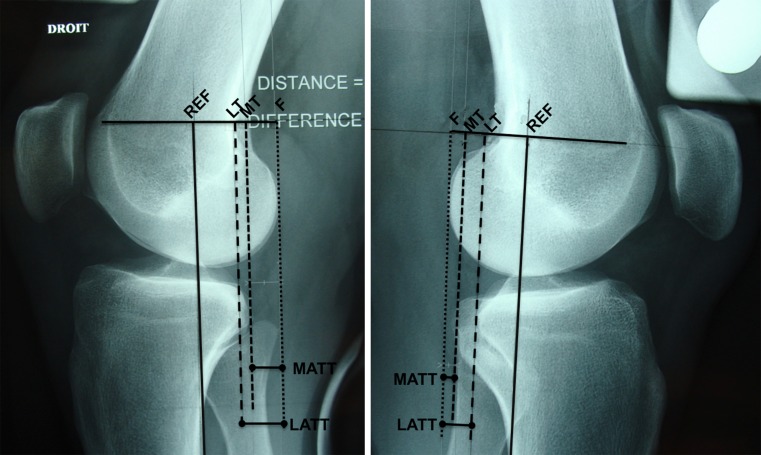
For Telos™ stress radiograph interpretation [17, 20, 21], two lines were drawn on the radiographs tangential to the posterior border of the upper tibial medial and lateral plateaux. Another line was drawn parallel to the above lines and tangential to the most posterior part of each femoral condyle (assuming perfect superimposition of both femoral condyles). The distance between the femoral and tibial lines on the medial side was called the medial anterior tibial translation (MATT) and the distance on the lateral side the lateral anterior tibial translation (LATT) (Fig. 1).
Fig. 1.
A reference line (REF) is drawn tangential to the tibial posterior cortex. Two lines are drawn tangential to the posterior border of the upper tibial medial (MT) and lateral (LT) plateaux, parallel to the reference line. Another line is drawn parallel to the above lines and tangential to the most posterior part of the femoral condyles (F). The distance between the femoral and tibial lines on the medial side was called the medial anterior tibial translation (MATT) and the distance on the lateral side the lateral anterior tibial translation (LATT)
MATT and LATT values for the operated knee were calculated pre- and post-operatively, and the difference between the pre- and post-operative settings calculated and compared between groups. The SS (normal to affected) pre- and post-operative MATT and LATT differences were also compared between groups.
For all patients, objective and subjective IKDC scores were calculated. Pivot shift of the preoperative status was obtained based on the medical record. Post-operative pivot shift was evaluated objectively by the independent observer at the final visit.
During the final evaluation, patients were instructed to kneel and walk on their knees over a hard surface in front of the examiner for a few metres. Afterwards, they were asked to subjectively classify it as impossible, difficult, unpleasant or normal (following the described knee walking test [22, 23]). They were also requested to crouch and classify subjectively as possible with pain, possible without pain, or impossible. The patients were asked to classify return to sports according to the pre-lesion level as return to the same level or return to an inferior level, regardless of which sport the patient practised. Changing the sport practised was considered as return to an inferior level.
Anterior knee pain was recorded as present or absent. Sensory deficits (hypoaesthesia) were also recorded as present or absent. When sensory loss was present, the knee was divided into eight zones, and each zone was tested individually [20]. This was recorded and the mean number of hypoaesthesia zones was calculated for each group.
Statistical analysis
Statistical analysis was performed using SPSS 14®. For quantitative data, the analysis of variance (ANOVA) test was used, and the post hoc analysis was performed with Tukey’s test. Qualitative data were analysed with the chi-square test or Fisher’s exact test. Paired samples were compared with the t test for paired samples. For all tests, the p value was accepted as significant if inferior to 0.05.
Patient profiles
There was a clear predominance of men in the sample. The DBH group showed the most equal distribution. Table 1 shows the distribution. Patients were older in the DBH group (mean 33.2 years), followed by the BPTB patients (27.52 years), and the youngest ones were those in the BPTB + L group (21.4 years) (ANOVA, p = 0.0001). Post hoc analysis with Tukey’s test confirmed that the three groups were different. Follow-up was very similar among the three groups, and the differences in delay from injury until surgery were not statistically significant between groups (ANOVA, p = 0.872). Values are shown in Table 2.
Table 1.
Sex distribution among the groups
| Procedure | Sex | Total | |
|---|---|---|---|
| Female | Male | ||
| DBH | 11 | 14 | 25 |
| BPTB | 8 | 17 | 25 |
| BPTB + L | 5 | 20 | 25 |
| Total | 24 | 51 | 75 |
DBH double-bundle hamstring, BPTB bone-patellar tendon-bone, BPTB + L bone-patellar tendon-bone associated with modified Lemaire procedure
Table 2.
Age, follow-up and time from injury to surgery according to the group
| Age (years) | Follow-up (months) | Time from injury to surgery (months) | ||
|---|---|---|---|---|
| DBH | Mean | 33.2 | 24.9 | 16.54 |
| Min. | 22 | 18 | 2 | |
| Max. | 43 | 31 | 120 | |
| BPTB | Mean | 27.5 | 25.4 | 12.96 |
| Min. | 14 | 18 | 1 | |
| Max. | 42 | 30 | 84 | |
| BPTB + L | Mean | 21.4 | 25.6 | 10.78 |
| Min. | 14 | 14 | 3 | |
| Max. | 34 | 33 | 30 | |
DBH double-bundle hamstring, BPTB bone-patellar tendon-bone, BPTB + L bone-patellar tendon-bone associated with modified Lemaire procedure
Associated procedures were exclusively procedures on the meniscus (medial, lateral or both) and could include suture or meniscectomy. In the DBH group 12 patients were submitted to an associated procedure, in the BPTB group ten patients and in the BPTB + L group 15 patients. This difference was not statistically significant (chi-square, p = 0.363).
Results
Anterior tibial translation
ATT improved in all three groups after surgery (Table 3). Mean ATT for the internal compartment improved from 10.41 to 4.67 mm, a 5.74-mm decrease. For the external compartment the mean ATT decrease was 6 mm, from 15.21 to 9.21 (t test for paired samples, p = 0.0001).
Table 3.
Pre- and post-operative ATT
| Pre-op | Post-op | Paired difference (pre- to post-op) | Sig. (2-tailed) | ||||
|---|---|---|---|---|---|---|---|
| Mean | 95 % Confidence interval of the difference | ||||||
| Lower | Upper | p | |||||
| DBH | MATT | 9.40 | 3.92 | 5.48 | 4.504 | 6.456 | .0001 |
| LATT | 13.12 | 7.44 | 5.68 | 4.685 | 6.675 | .0001 | |
| BPTB | MATT | 9.72 | 4.36 | 5.36 | 4.218 | 6.502 | .0001 |
| LATT | 15.48 | 11.36 | 4.12 | 3.210 | 5.030 | .0001 | |
| BPTB + L | MATT | 12.12 | 5.72 | 6.40 | 5.010 | 7.790 | .0001 |
| LATT | 17.4 | 8.84 | 8.20 | 6.906 | 9.494 | .0001 | |
DBH double-bundle hamstring, MATT medial anterior tibial translation, LATT lateral anterior tibial translation, BPTB bone-patellar tendon-bone, BPTB + L bone-patellar tendon-bone associated with modified Lemaire procedure
ATT values for the internal compartment were greater in the preoperative evaluation in the BPTB + L group than in the other two groups (ANOVA, p = 0.008, Tukey’s test). ATT preoperative values for the external compartment were also different between groups: the BPTB + L and BPTB groups showed significantly higher values than the DBH group (ANOVA, p = 0.001, Tukey’s test). Group-specific improvements are shown in Table 3.
Internal compartment SS difference (normal to ACL insufficient) in the preoperative setting was similar among groups: DBH 7.12 mm, BPTP 7.00 mm and BPTB + L 8.20 mm (ANOVA, p = 0.294). For the external compartment values for SS difference were similar for DBH (7.64 mm) and BPTB (8.24), but the BPTB + L group showed increased difference (10.16 mm) (ANOVA, p = 0.005, Tukey’s test).
When the absolute decrease in ATT value from the preoperative to the post-operative setting was considered, internal compartment mean values were not statistically different for all three groups: 5.48 mm for DBH, 5.36 for BPTB and 6.40 for BPTB + L (ANOVA, p = 0.377). Comparing the external compartment mean values, however, the BPTB + L (8.20 mm) group was superior to the other two (ANOVA, p = 0.0001, Tukey’s test). The BPTB (4.12 mm) and DBH groups (5.58 mm) were not different.
In the comparative analysis between the post-operative SS (normal to operated) difference for the ATT values for the external compartment, results showed that the BPTB group was significantly less corrected by surgery than the other two groups. Mean difference values were 4.16 mm for the BPTB group, 1.84 mm for the BPTB + L group and 1.92 mm for the DBH group. The two last groups were not different in the statistical analysis (ANOVA, p = 0.0001, Tukey’s test). For the internal compartment, again, no differences were shown (ANOVA, p = 0.698). Mean values were 2.00 mm (DBH), 1.56 mm (BPTB) and 1.80 mm (BPTB + L).
Pivot shift
Pre- and post-operative results are shown in Tables 4 and 5, respectively. In order to allow statistical analysis, the post-operative results were divided into A (equal) and B (glide, gross and marked), and comparison was performed between each two groups (DBH vs BPTB, DBH vs BPTB + L and BPTB vs BPTB + L) using Fisher’s exact test, but no significance was observed (Fisher’s exact test, p = 0.289, p = 1 and p = 0.138, respectively).
Table 4.
Preoperative pivot shift results (compared to the contralateral non-injured side)
| Group | Pivot pre-op | Total | |||
|---|---|---|---|---|---|
| Glide | Gross | Marked | Impossible | ||
| BPTB | 19 | 2 | 0 | 4 | 25 |
| BPTP + L | 1 | 14 | 6 | 4 | 25 |
| DBH | 14 | 5 | 0 | 6 | 25 |
| Total | 34 | 21 | 6 | 14 | 75 |
DBH double-bundle hamstring, BPTB + L bone-patellar tendon-bone associated with modified Lemaire procedure, BPTB bone-patellar tendon-bone
Table 5.
Post-operative pivot shift results (compared to the contralateral non-injured side)
| Group | Pivot post-op | Total | ||
|---|---|---|---|---|
| Equal | Glide | Marked | ||
| BPTB | 18 | 5 | 2 | 25 |
| BPTP + L | 23 | 2 | 0 | 25 |
| DBH | 22 | 2 | 1 | 25 |
| Total | 63 | 9 | 3 | 75 |
DBH double-bundle hamstring, BPTB + L bone-patellar tendon-bone associated with modified Lemaire procedure, BPTB bone-patellar tendon-bone
IKDC
The total mean IKDC was 88.4 in the post-operative set. Group DBH mean score was 89.1, group BPTB 90.1 and group BPTB + L 86. There was no statistical difference between the groups (ANOVA, p = 0.224). Objective IKDC was again statistically not different between groups when comparing patients classified as IKDC A versus those classified as B and C. No patients were classified as D (chi-square, p = 0.49) (Table 6).
Table 6.
IKDC results according to group distribution
| Procedure | Objective IKDC | Total | ||
|---|---|---|---|---|
| A | B | C | ||
| DBH | 18 | 5 | 2 | 25 |
| BPTB | 14 | 9 | 2 | 25 |
| BPTB + L | 16 | 8 | 1 | 25 |
| Total | 48 | 22 | 5 | 75 |
DBH double-bundle hamstring, BPTB bone-patellar tendon-bone, BPTB + L bone-patellar tendon-bone associated with modified Lemaire procedure
Return to sports
Return to sports was possible at the same level as before the injury in 20 patients in the DBH group, 20 in the BPTB group and 16 in the BPTB + L group. This difference was not statistically significant (chi-square, p = 0.324). One patient in the DBH group and one patient in the BPTB + L group abandoned the practice of sports after the surgery, and the remainder returned to sports at an inferior level.
Anterior knee pain
Six patients in the DBH group complained of anterior knee pain. The BPTB and BPTB + L groups had nine patients each. This was not statistically different (chi-square, p = 0.576).
Post-operative procedures
One patient in the DBH group was submitted to an arthroscopic resection of a cyclops lesion and another to resection of a protuberant tendon remnant in the external femoral cortex. In the BPTB group, one cyclops lesion resection and one meniscectomy were performed. In the BPTB + L group, two meniscectomies were performed, and one patient developed deep venous thrombosis.
Sensory deficits
Eleven patients in the DBH group complained of sensory deficit. This same complaint was present in 17 patients in the BPTB group and 19 patients in the BPTB + L group (chi-square, p = 0.052). When analysing the number of zones in which hypoaesthesia was present in those who had it, the mean number of zones was 1 in the DBH group, 1.76 in the BPTB group and 1.84 in the BPTB + L group (ANOVA, p = 0.0001). Tukey’s test set for 0.05 showed that the DBH group was different from the other two groups.
Kneeling and crouching
Walking on the knees was normal in 22 patients in the DBH group, seven in the BPTB group and eight in the BPTB + L group (chi-square, p = 0. 0001). The BPTB and BPTB + L groups were not different (chi-square, p = 0.75). In the remaining patients it was difficult, unpleasant or impossible. Crouching was possible with no pain in 18 patients in the DBH group, 17 in the BPTB group and 17 in the BPTB + L group (chi-square, p = 0.939). It was possible with pain in the remainder, and only one patient in the BPTB group considered it impossible.
Discussion
As a result of selection bias, patients were different from the outset. There were differences concerning especially sex, age and degree of laxity (ATT). Age differences compromise the comparison between groups. Follow-up and delay from injury until surgery were similar.
The absolute ATT improved for both compartments in all three groups after surgery. Correction of ATT was not statistically different for the medial compartment between the three groups, but the patellar tendon reconstruction combined with the extra-articular procedure achieved the best lateral compartment ATT correction.
Preoperative differences hindered the comparison between the groups’ absolute values. Decreased ATT values from the preoperative to the post-operative setting, however, allowed direct comparison between them, and there was superior LATT correction in the BPTB-L group, while the study failed to prove any difference between the BPTB and DBH groups and failed to prove any differences for the medial compartment (MATT).
When analysing the difference from the normal opposite knee ATT values to the post-operative ATT values of the operated knee, the BPTB group showed the greatest value, meaning inferior correction. The DBH and BPTB-L groups were similar, but it should be reiterated that the BPTB-L group had the greatest preoperative values, and the fact that it reached a similar value to the DBH group could be understood as a superior correction. For the medial compartment, again, no differences could be found. Similarity between medial tibial translation values, in our opinion, is due to the fact that all procedures included an intra-articular reconstruction.
We believe that this mismatch (BPTB-L superior in one analysis and BPTB inferior in the other) is attributed to the study design and small sample. Probably, a greater sample and equal groups from the beginning of the study could show that the three groups were different in relation to LATT correction.
The mean post-operative IKDC was very similar among the three groups. Preoperative values were not available, which in some way compromised further conclusions, but this agrees with the rest of the literature [5, 21, 22] and shows that most of the procedures are equivalent. Equally, objective IKDC showed similar results among the groups, again confirming the trends in the literature.
Anterior knee pain mechanisms are not completely understood. The patellar tendon procedures are supposed to produce more pain, but this is not universally accepted. In our sample, there was no significant statistical difference between the groups, but a larger sample could have shown different results. Also, anterior knee pain was assessed as present or absent, and no quantitative measurement was made.
The number of associated procedures was similar between groups, which correlates with similar mechanisms of trauma, and also similar delay until surgery. This similarity also favours comparison between groups and procedures. Post-operative interventions were also similar between groups and corresponded to common procedures following ACL reconstruction. One patient in the DBH group was submitted to a resection of the tendon remnants in the external femoral cortex, and this is unique to the way the graft is passed (in a loop) through the femur.
When analysing the presence or absence of sensory deficits, the p value obtained in the ANOVA test for the differences between the groups was borderline. We agree with the literature [5, 23] and believe that patellar tendon reconstructions with a standard approach, in which the incision is bigger than in hamstring procedures, should cause more sensory deficits. A bigger sample should confirm this. When analysing the number of zones in which hypoaesthesia was present, there was a clear predominance of the BPTB and BPTB-L groups.
Also, in our hypothesis, the association of a lateral incision for the extra-articular reconstruction should worsen the sensory deficits. This was not confirmed by the post-operative assessment.
The DBH group performed much better when walking on the knees than the BPTB and BPTB-L groups. This is expected, as the anterior scar produced by these procedures prevents attempts of kneeling over the affected side. Crouching was similar between groups.
Return to sports was not different between the groups. Two main biases should be considered, however: first, the BPTB-L group consisted of younger patients, which could improve their ability to return to sports and affect results; second, the BPTB-L group represented a group with greater laxity in the preoperative setting, which could compromise their ability to return to sports. Also, the size of the sample should be taken into account, and a larger sample could evidence some differences.
Conclusion
There are intrinsic differences between the three procedures. Absolute correction of ATT is not different for the medial compartment between the three groups, but the patellar tendon reconstruction combined with a Lemaire extra-articular procedure achieved the best lateral compartment ATT correction. Sensory deficits and the ability to kneel seem to be worse in the groups in which the patellar tendon is harvested.
Following the trends in the literature, our study has shown that superior stability is achieved by the addition of an extra-articular procedure, and this can be used in the primary setting when treating patients with increased instability and who are involved in high demand sports. On the other hand, one should be cautious when performing procedures using the patellar tendon in individuals who may be subjected to kneeling and crouching during their sport or work activities.
References
- 1.Yasuda K, Tanabe Y, Kondo E, Kitamura N, Tohyama H. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(9 Suppl):S21–S34. doi: 10.1016/j.arthro.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 2.Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N. Comparison between single- and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med. 2010;38(1):25–34. doi: 10.1177/0363546509347096. [DOI] [PubMed] [Google Scholar]
- 3.Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):500–507. doi: 10.1007/s00167-006-0254-z. [DOI] [PubMed] [Google Scholar]
- 4.Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):137–145. doi: 10.1016/j.arthro.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86-A(10):2143–2155. [PubMed] [Google Scholar]
- 6.Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med. 2001;29(6):722–728. doi: 10.1177/03635465010290060901. [DOI] [PubMed] [Google Scholar]
- 7.Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(2):214–220. doi: 10.1177/03635465020300021201. [DOI] [PubMed] [Google Scholar]
- 8.Anderson AF, Snyder RB, Lipscomb AB., Jr Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med. 2001;29(3):272–279. doi: 10.1177/03635465010290030201. [DOI] [PubMed] [Google Scholar]
- 9.Webster KE, Feller JA, Hameister KA. Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):86–91. doi: 10.1007/s001670100191. [DOI] [PubMed] [Google Scholar]
- 10.Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 11.Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25(10):1139–1174. doi: 10.1016/j.arthro.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 12.Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009;37(4):707–714. doi: 10.1177/0363546508328114. [DOI] [PubMed] [Google Scholar]
- 13.Lerat JL, Mandrino A, Besse JL, Moyen B, Brunet-Guedj E. Effect of external extra-articular ligament plasty on the results of anterior cruciate ligament reconstruction with patellar tendon, a 4 years follow-up. Rev Chir Orthop Reparatrice Appar Mot. 1997;83(7):591–601. [PubMed] [Google Scholar]
- 14.Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73(6):882–892. [PubMed] [Google Scholar]
- 15.van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy. 2010;26(9 Suppl):S2–S12. doi: 10.1016/j.arthro.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Condouret J, Cohn J, Ferret J-M, Lemonsu A, Vasconcelos W, Dejour D, Potel J-F, et al. Isokinetic assessment with two years follow-up of anterior cruciate ligament reconstruction with patellar tendon or hamstring tendons. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8 Suppl):375–382. doi: 10.1016/j.rco.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Prado RK, Ntagiopoulos PG, Fucs PMB, Severino NR, Dejour D. A new technique in double-bundle anterior cruciate ligament reconstruction using implant-free femoral fixation. Int Orthop. 2012;36(7):1479–1485. doi: 10.1007/s00264-012-1488-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dejour H, Dejour D, Aït Si Selmi T. Chronic anterior laxity of the knee treated with free patellar graft and extra-articular lateral plasty: 10-year follow-up of 148 cases. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(8):777–789. [PubMed] [Google Scholar]
- 19.Lemaire M (1967) Rupture ancienne du ligament croisé antérieur du genou; fréquence, clinique, traitement (46 cas). J Chirurgie 311–320
- 20.Beldame J, Bertiaux S, Roussignol X, Lefebvre B, Adam J-M, Mouilhade F, Dujardin F. Laxity measurements using stress radiography to assess anterior cruciate ligament tears. Orthop Traumatol Surg Res. 2011;97(1):34–43. doi: 10.1016/j.otsr.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Jacobsen K. Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand. 1976;47(3):335–334. doi: 10.3109/17453677608992002. [DOI] [PubMed] [Google Scholar]
- 22.Kartus J, Magnusson L, Stener S, Brandsson S, Eriksson BI, Karlsson J. Complications following arthroscopic anterior cruciate ligament reconstruction. A 2-5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):2–8. doi: 10.1007/s001670050112. [DOI] [PubMed] [Google Scholar]
- 23.Laxdal G, Sernert N, Ejerhed L, Karlsson J, Kartus JT. A prospective comparison of bone-patellar tendon-bone and hamstring tendon grafts for anterior cruciate ligament reconstruction in male patients. Knee Surg Sports Traumatol Arthrosc. 2007;15(2):115–125. doi: 10.1007/s00167-006-0165-z. [DOI] [PubMed] [Google Scholar]