Abstract
The aim of the paper is to describe the medial portal technique for anatomical single-bundle anterior cruciate ligament (ACL) reconstruction. Placement of an ACL graft within the anatomical femoral and tibial attachment sites is critical to the success and clinical outcome of ACL reconstruction. Non-anatomical ACL graft placement is the most common technical error leading to recurrent instability following ACL reconstruction. ACL reconstruction has commonly been performed using a transtibial tunnel technique in which the ACL femoral tunnel is drilled through a tibial tunnel positioned in the posterior half of the native ACL tibial attachment site. ACL reconstruction performed using a transtibial tunnel technique often results in a vertical ACL graft, which may fail to control the combined motions of anterior tibial translation and internal tibial rotation which occur during the pivot-shift phenomenon. The inability of a vertically oriented ACL graft to control these combined motions may result in the patient experiencing continued symptoms of instability due to the pivot-shift phenomenon. The medial portal technique in which the ACL femoral tunnel is drilled through an anteromedial or accessory anteromedial portal allows consistent anatomical ACL tunnel placement. This paper describes the advantages of the medial portal technique, indications for the technique, patient positioning, proper portal placement, anatomical femoral and tibial tunnel placement, graft tensioning and fixation.
Introduction
Anatomical placement of an anterior cruciate ligament (ACL) graft is considered critical to the success and clinical outcome of ACL reconstruction. Anatomical ACL graft placement is defined as positioning the ACL femoral and tibial bone tunnels at the centre of the native ACL femoral and tibial attachment sites. Clinical studies have demonstrated that non-anatomical ACL graft placement is the most common technical error leading to recurrent instability following ACL reconstruction [1, 2]. ACL reconstruction has been commonly performed using a transtibial technique in which the ACL femoral tunnel is drilled through a tibial tunnel positioned in the posterior half of the native ACL tibial attachment site. In the transtibial technique, positioning the ACL tibial tunnel in the posterior half of the ACL tibial attachment site is dictated by the need for the arthroscopic drill bit to reach the region of the ACL femoral attachment site and the desire that the ACL graft avoid impingement against the roof of the intercondylar notch when the knee is in full extension. However, the resulting ACL femoral tunnel is often positioned too high and deep in the intercondylar notch, outside of the native ACL femoral attachment site (Fig. 1).
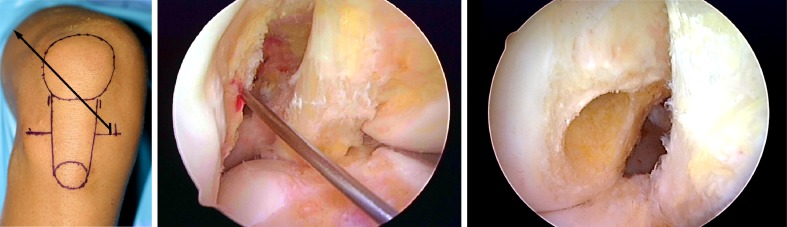
Fig. 1.
Transtibial tunnel technique. a The femoral guide pin is drilled using an ACL femoral offset aimer inserted through a tibial tunnel positioned in the posterior half of the ACL tibial attachment site. b An ACL femoral tunnel drilled through a posteriorly positioned tibial tunnel often results in the ACL femoral tunnel being positioned high relative to the native ACL femoral attachment site. c An ACL graft positioned in a posterior tibial and high femoral tunnel often results in a non-anatomical “vertical” ACL graft. d An example of ACL reconstruction using a transtibial technique
An ACL graft positioned at a posterior tibial and a high-deep femoral attachment site will be vertically oriented in both the coronal and sagittal planes. Biomechanical studies have shown that a vertically oriented ACL graft may resist the motion of anterior tibial translation, but may fail to control the combined motions of anterior tibial translation and internal tibial rotation which occur during the pivot-shift phenomenon [3–6]. The inability of a vertically oriented ACL graft to control these combined motions may result in the patient experiencing continued symptoms of instability and giving-way episodes due to the pivot-shift phenomenon.
The medial portal technique for endoscopic drilling of the ACL femoral tunnel was first developed to address the issues of ACL graft laceration, violation of the posterior wall of the ACL femoral tunnel, divergence of ACL femoral interference screws and tunnel-graft length mismatch associated with bone-patellar tendon-bone autograft ACL reconstructions performed using the transtibial technique. In the medial portal technique described in this paper, the ACL femoral tunnel is drilled through an accessory anteromedial (AAM) portal with the knee flexed to 120° or more (Fig. 2).
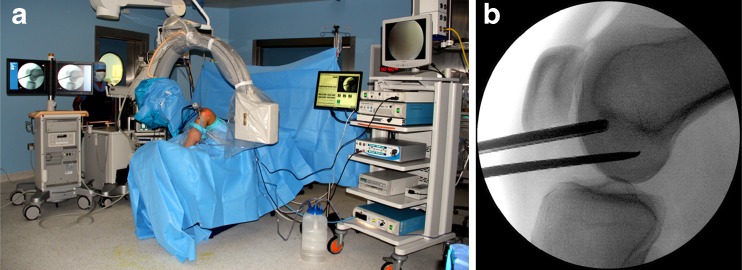
Fig. 2.
a Medial portal technique. The knee is hyperflexed and the femoral tunnel is drilled through a medial portal. b The knee is hyperflexed with the 30° arthroscope positioned in the anteromedial (AM) portal. The ACL femoral tunnel is drilled through a low AAM portal. c View through the AM portal with the knee in hyperflexion. The ACL femoral tunnel is drilled into the centre of the ACL femoral attachment site through a low AAM portal
This approach provides several advantages compared to the traditional transtibial technique:
The ACL femoral tunnel is drilled independently of the tibial tunnel, which allows for consistent placement of the femoral tunnel within the native ACL femoral attachment site.
The angle of the ACL tibial tunnel does not have to be compromised to accommodate drilling of the ACL femoral tunnel. Therefore, the surgeon can opt to drill a steeper and thus longer tibial tunnel. A longer tibial tunnel minimises the potential for graft-tunnel length mismatch and allows longer bone-tendon-bone graft constructions to be used.
Although guides are available, the medial portal technique does not require any special guides or instrumentation.
Inserting an ACL femoral interference fixation screw through the same medial portal which was used to drill the ACL femoral tunnel minimises screw-tunnel divergence.
The medial portal technique provides improved arthroscopic visualisation during ACL femoral tunnel drilling since the femoral tunnel can be drilled under ideal arthroscopic conditions, without the loss of joint distention due to fluid extravasation out of the tibial tunnel.
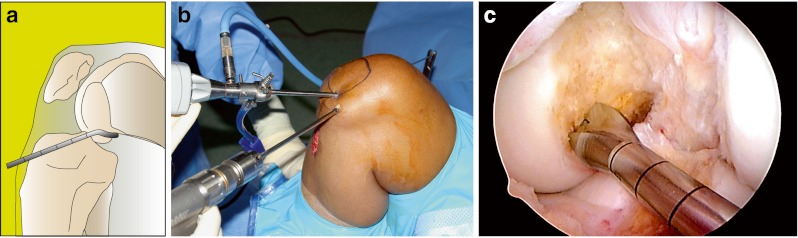
Similar to any surgical technique, there is a learning curve to the medial portal technique for ACL reconstruction. Surgeons making the transition from the transtibial to the medial portal technique may experience some unique issues and challenges not normally encountered when performing an ACL reconstruction using the transtibial technique. In the medial portal technique, the knee must be flexed to 120° or more when a rigid guide pin and drill bit are used to drill the ACL femoral tunnel (Fig. 3). Hyperflexion is necessary to avoid having the femoral guide pin exit the lateral soft tissues too posteriorly. The peroneal nerve is at risk when the femoral guide pin exits the lateral soft tissues in a too posterior position. Alternatively, the knee may be positioned at 90° of flexion and the ACL femoral tunnel drilled using flexible reamers.
Fig. 3.

The right knee is positioned in hyperflexion during drilling of the ACL femoral tunnel. The drill tip femoral guide pin exits the lateral soft tissues in the mid-thigh region and is thus directed away from the peroneal nerve and posterior neurovascular structures
Drilling the ACL femoral tunnel in hyperflexion can potentially compromise arthroscopic visualisation and lead to spatial disorientation in the notch compared to drilling at the more familiar 90° of knee flexion. Other potential problems that can result from drilling the ACL femoral tunnel in hyperflexion include: (1) difficulty passing the endoscopic reamer over the guide pin due to the medial portal tightening in hyperflexion, (2) difficulty visualising the endoscopic reamer due to the reamer dragging the fat pad into the notch and (3) difficulty advancing the endoscopic reamer over the guide wire due to a bend or kink in the guide pin. Drilling the ACL femoral tunnel through a medial portal which is placed too close to the medial femoral condyle can result in iatrogenic injury to the articular cartilage of the medial femoral condyle. Unless special attention is paid to proper portal placement and positioning the knee in hyperflexion while drilling the ACL femoral tunnel, the medial portal technique can result in a short ACL femoral tunnel length which may limit the amount of soft tissue graft inserted into the ACL femoral tunnel when using a cortical femoral fixation device such as the ENDOBUTTON continuous loop (CL) (Smith & Nephew, London, UK). With attention to detail, all of these potential issues and challenges can be overcome.
Indications and contraindications for the medial portal technique
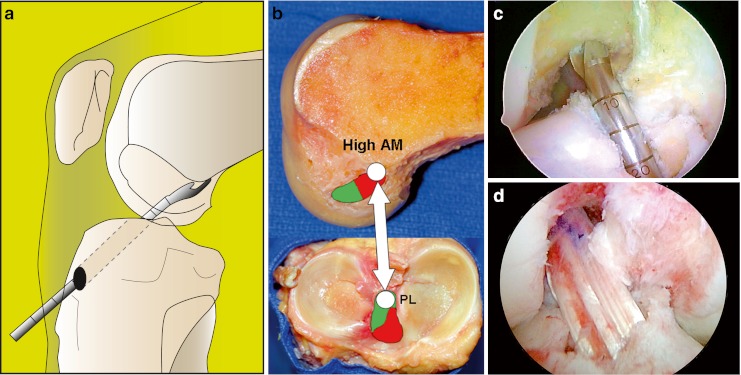
The medial portal technique is versatile and can be used with any ACL graft type and for any primary, revision, single- or double-bundle ACL reconstruction. The medial portal technique is particularly useful in the situation where only one of the ACL bundles is torn and the surgeon wishes to preserve the remaining intact ACL fibres and augment the injured posterolateral (PL) or anteromedial (AM) bundle (Fig. 4).
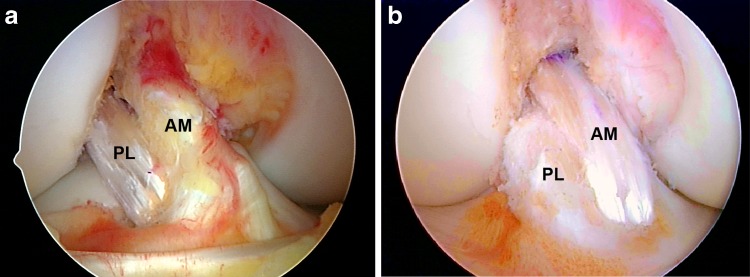
Fig. 4.
a Isolated PL bundle reconstruction. b Isolated AM bundle reconstruction
In the situation of revision ACL surgery, the medial portal technique often allows a new anatomical ACL femoral tunnel to be drilled away from a previous non-anatomical vertical femoral tunnel. This may eliminate the need to remove the original ACL femoral fixation hardware and can bypass a malpositioned or enlarged ACL femoral tunnel, thus avoiding the need for bone grafting of the original femoral tunnel and a two-stage revision (Fig. 5).
Fig. 5.
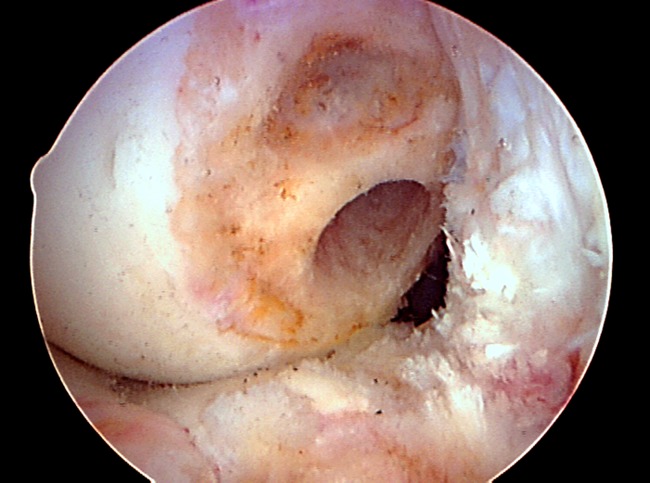
AM portal view at 90°. Failed ACL reconstruction. Probable cause of failure: non-anatomical ACL femoral tunnel placement. Surgical technique: transtibial. The old ACL femoral tunnel is located high above the anatomical ACL femoral attachment site. A new anatomical ACL femoral tunnel was drilled through an AAM portal bypassing the original non-anatomical femoral tunnel
The only contraindication to the medial portal technique when using rigid guide pins and drill bits is the inability to flex the knee to at least 120°. This limitation may be encountered in some obese patients, in which case consideration should be given to drilling the ACL femoral tunnel using an outside-in technique or using flexible reamers.
Patient positioning
It is important to have the ability to achieve full, unrestricted knee flexion during the procedure. The requirement to achieve at least 120° of knee flexion can sometimes present problems when a circumferential leg holder is used and the foot of the operating room table flexed down. Keeping the operating room table flat and using a thigh post and one or two foot rests allows full unrestricted knee flexion and facilitates performance of the procedure.
Apply a thigh length anti-embolism stocking and a foam heel protector to the non-operative leg.
Place a padded pneumatic tourniquet high on the operative leg. Use of the tourniquet is optional depending on the surgeon’s preference, noting that adequate joint visualisation can be obtained using an infusion pump.
Attach a padded thigh post to the operating room table at the level of the pneumatic tourniquet to support the thigh and act as a fulcrum during the application of valgus stress to open the medial compartment (Fig. 6a).
Attach a padded L-shaped foot rest to the rail clamp along the operative side of the operating table. Adjust the position of the distal foot rest to maintain the knee at 90° of flexion during most of the procedure (Fig. 6b).
Place a second foot rest just proximal to the popliteal fossa and adjust it to allow maintenance of the knee in hyperflexion during drilling of the ACL femoral tunnel (Fig. 6b, c). The patient’s foot can be placed under or against the proximal foot rest (Fig. 6c). With the knee in extension, the relative height of the two foot rests can be adjusted such that the knee can be maintained at a known flexion angle during tensioning and fixation of the ACL graft (Fig. 6d).
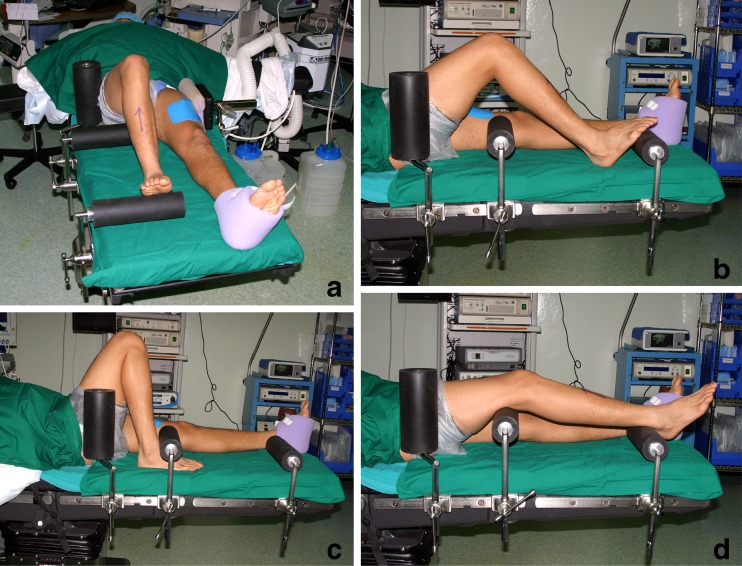
Fig. 6.
a The patient’s pelvis is stabilised on the operating table by the lateral hip positioner and thigh post. b Distal foot rest is adjusted to maintain 90° of knee flexion. c Proximal foot rest is adjusted to maintain hyperflexion during drilling of the ACL. d The proximal and distal foot rest can be adjusted to maintain the desired degree of knee flexion during graft tensioning and fixation
Portal placement
Proper portal placement is critical to the success of the procedure. ACL reconstruction using the medial portal technique is facilitated by using three arthroscopic portals (Fig. 7):
The anterolateral (AL) portal—used as a viewing portal to perform diagnostic arthroscopy and meniscal surgery. This is positioned slightly higher than the normal position for standard arthroscopic procedures.
The AM portal—used as both a working and viewing portal. Again this is in a slightly higher position than usual.
The AAM portal—used as a working portal to insert instrumentation into the notch and for drilling the ACL femoral tunnel.
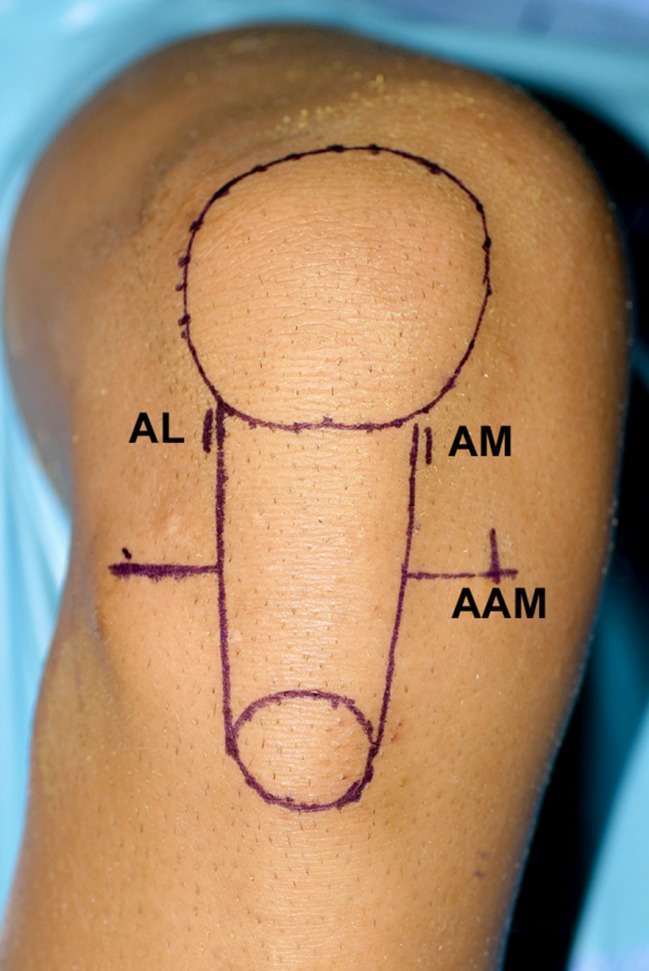
Fig. 7.
Three portals and their relationship to the inferior pole of the patella, medial and lateral borders of the patellar tendon, and the medial and lateral joint lines. AL high anterolateral portal, AM high anteromedial portal, AAM low accessory anteromedial portal
The use of three portals provides the following advantages:
The additional medial portal allows the ACL femoral attachment site to be viewed through the AM portal, while working instrumentation is inserted into the notch through the AAM portal. As will be discussed later, viewing through the AM portal is the preferred method to visualise the ACL femoral attachment site.
Drilling the ACL femoral tunnel through an AAM portal increases the obliquity of the ACL femoral tunnel relative to the lateral wall of the notch, resulting in a longer femoral tunnel length and a more elliptical ACL femoral tunnel aperture compared to drilling the femoral tunnel through the AM portal.
Establishing the anterolateral portal
Establish a high AL portal at the level of the inferior pole of the patella, as close as possible to the lateral border of the patellar tendon using a #11 knife blade. A high AL portal places the arthroscope above the widest part of the fat pad, minimising interference of the visual field in the intercondylar notch when the knee is placed in hyperflexion. A high AL portal also provides a better “look down” view of the ACL tibial attachment site.
Establishing the anteromedial portal
Establishing the AM portal at the correct height above the medial joint line is extremely important to the success of the procedure. Placing the AM portal too close to the medial joint line will lead to instrument crowding when the AM and AAM portals are used simultaneously during notch preparation and ACL femoral tunnel drilling
Place a 30° arthroscope in the AL portal and perform a diagnostic arthroscopy.
With the knee flexed at 90°, establish the AM portal under direct vision using an 18-gauge spinal needle. Insert the spinal needle into the knee joint as close as possible to the medial border of the patellar tendon. Direct the spinal needle towards the intercondylar notch, adjusting the height of the spinal needle above the medial joint line as needed to ensure that it comes to lie parallel to the roof of the intercondylar notch.
Typically, the spinal needle is located at the height of the interior pole of the patella or slightly higher. Placing the spinal needle at this level results in adequate spatial separation between the AM and the AAM portal which is created later and also results in the AM portal lying above the fat pad. The spinal needle position is too low if it enters the knee joint below the level of the roof of the intercondylar notch or passes through the fat pad.
Insert a motorised shaver blade into the knee joint through the AM portal and resect the ligamentum mucosum. This step will release the fat pad and expose the intercondylar notch.
Placement of the accessory anteromedial portal
Proper placement of the AAM portal is also critical to the success of the procedure, as it is the most important factor affecting the length of the ACL femoral tunnel. The medial-lateral placement of the AAM portal determines both the length of the ACL femoral tunnel and the shape of the tunnel’s aperture. Positioning the AAM portal more medially results in a more perpendicular orientation of the femoral drill bit with respect to the lateral wall of the notch and produces a shorter ACL femoral tunnel and a more circular-shaped tunnel aperture (Fig. 8) [7]. However, placing the AAM portal too medially can result in damage to the medial femoral condyle when the AAM portal is used to drill the ACL femoral tunnel.
Fig. 8.
Medial placement of the AAM portal results in a more perpendicular orientation of the spinal needle relative to the lateral wall of the notch. The orientation will produce a more circular-shaped aperture of the ACL femoral tunnel and a shorter femoral tunnel length
Moving the AAM portal more laterally, towards the medial border of the patellar ligament, orientates the femoral bit more obliquely with respect to the lateral wall of the notch and produces a longer ACL femoral tunnel length and a more elliptically shaped tunnel aperture (Fig. 9) [7].
Fig. 9.
A more lateral placement of the AAM portal results in a more oblique orientation of the spinal needle relative to the lateral wall of the notch. This orientation will produce a more elliptically shaped aperture of the femoral tunnel and a longer femoral tunnel length. Based on the ACL graft type and femoral fixation method, the position of the AAM portal is adjusted to achieve the desired ACL femoral tunnel length. For example, if a bone-patellar tendon-bone ACL graft with interference screw fixation of the femoral bone block is used for the ACL reconstruction, the optimal femoral tunnel length can be in the range of 25–30 mm. For this graft type and fixation method, the AAM portal can be positioned more medially compared to an ACL reconstruction performed using a multiple-strand hamstring tendon graft with ENDOBUTTON femoral fixation
When performing hamstring ACL reconstructions with cortical fixation devices such as the ENDOBUTTON CL, it is optimal to achieve a femoral tunnel length of around 40 mm, with the minimum tunnel length being around 35 mm. A 40 mm femoral tunnel allows for 25 mm of the hamstring tendon graft to be inserted into the ACL femoral socket when using a 15 mm ENDOBUTTON CL.
Establishing the accessory anteromedial portal
Use an 18-gauge spinal needle to determine the optimal position for the AAM portal. The AAM portal should be located as low as possible above the medial joint line while avoiding the anterior horn of the medial meniscus. Rotate the arthroscope medially to determine whether the spinal needle is positioned too closely to the medial femoral condyle. Adjust the position of the portal accordingly.
Create the AAM portal using a #11 knife blade, with the cutting edge of the blade oriented away from the anterior horn of the medial meniscus.
Dilate the AAM portal by inserting the tips of the Metzenbaum scissors or a small curved clamp into the incision and spreading the tips in-line with the direction of the portal. This step will ease future instrument passage through the AAM portal.
Preparation of the ACL tibial attachment site
Careful inspection of the remnants of the torn ACL is important. An attempt should be made to preserve large stumps and remnant ACL fibres with intact connections from the tibia to the femur.
Insert a motorised shaver blade into the knee joint through the AM portal and resect the midsection of the ACL. Preserve some of the remaining native ACL fibres at the tibial and femoral attachment sites to aid with anatomical placement of the ACL bone tunnels.
Insert a 90° bipolar thermal probe through the AM portal and mark the borders of the ACL tibial attachment site (Fig. 10). Note that a portion of the ACL tibial attachment site extends anterior to the posterior margin of the anterior horn of the lateral meniscus. The anterior margin of the ACL tibial attachment site lies just posterior to the intermeniscal ligament when the knee is at 30° of flexion, and the posterior margin lies just anterior to a bony ridge connecting the medial and lateral tubercles (spines). If the knee is at 90° the intermeniscal ligament will cover part of the ACL footprint. The medial border of the ACL tibial attachment site is defined by a bony ridge, the medial intercondylar ridge of the tibia, which extends anteriorly from the medial tubercle.
To measure the length of the ACL tibial attachment site, insert a ruler through the AAM portal and measure the length of the ACL tibial attachment site (Fig. 11). One of the goals of ACL reconstruction is to restore the maximum amount of the tibial and femoral attachment sites. Long and wide ACL tibial attachment sites are best restored with larger diameter ACL grafts such as five- and six-strand hamstring tendon grafts, a bone-patellar tendon-bone graft, a quadriceps tendon graft or by performing a double-bundle ACL reconstruction [8].
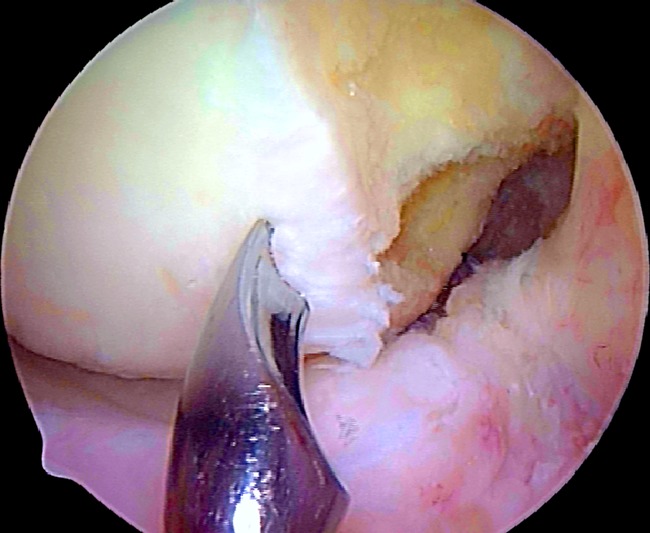
Fig. 10.
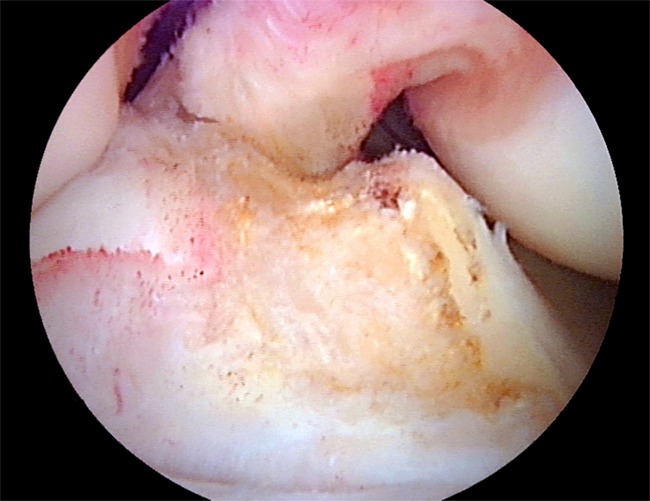
ACL tibial attachment site. The medial and lateral tibial tubercles (spines) with the interconnecting ACL ridge and the medial intercondylar ridge of the tibia are well seen
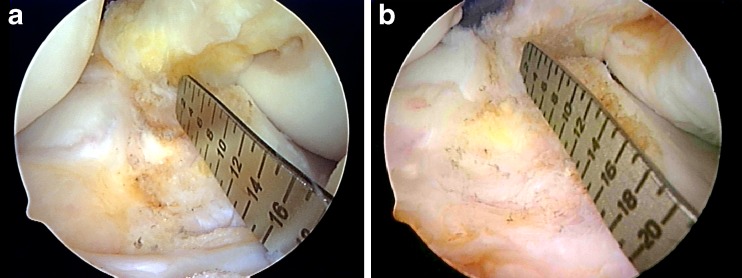
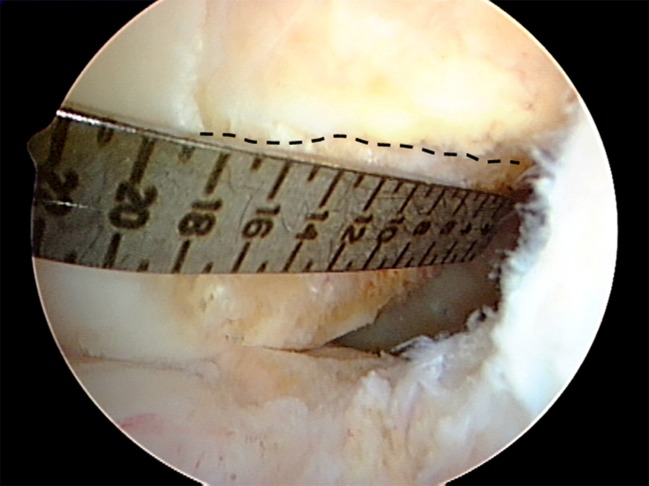
Fig. 11.
Measuring tibial attachment site length. a Short tibial insertion site (13 mm). b Long tibial insertion site (18 mm)
ACL graft placement
Biomechanical studies have demonstrated that a single-bundle ACL graft positioned at the centre of the ACL femoral and tibial attachment sites best controls anterior tibial translation and the combined motions of anterior tibial translation and internal tibial rotation (simulated pivot-shift test) and restores kinematics more closely to those of the normal knee compared to other anatomical ACL graft placements [3–6].
Anatomical ACL femoral tunnel position
Although the clock-face reference method is often used to specify ACL femoral tunnel placement, it has several shortcomings: it ignores the depth of the notch; there is no agreed reference position for the 3 and 9 o’clock locations; it relies on no known anatomical landmarks; and it cannot be used when viewing the ACL femoral attachment site through the AM portal. ACL femoral tunnel placement is more accurately defined and specified using the following methods:
Identification of the native ACL footprint
In most situations, remnants of the native ACL fibres are present at the ACL femoral attachment site and these can aid with anatomical ACL femoral tunnel placement (Fig. 12).
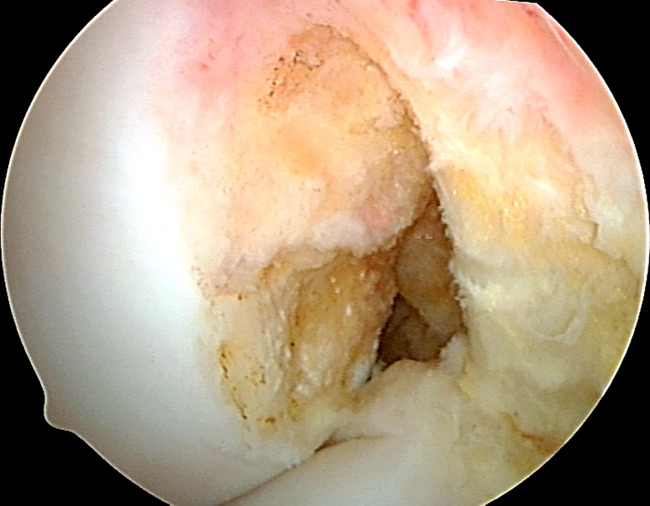
Fig. 12.
AM portal view at 90° of flexion. Remnants of the native ACL fibres at the ACL femoral attachment site are clearly seen
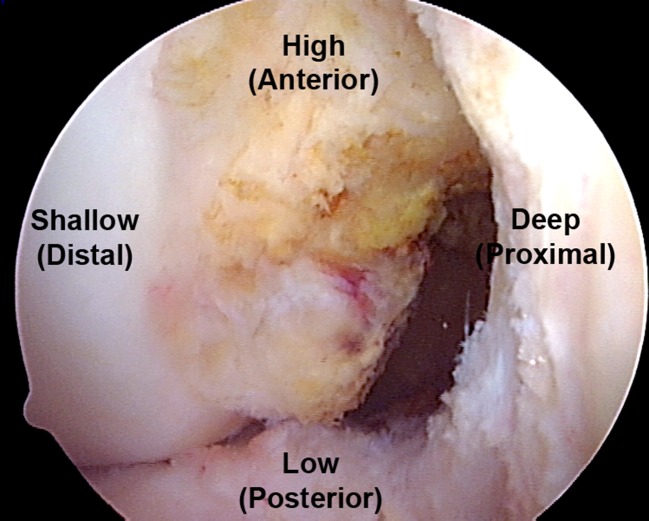
The view of the intercondylar notch and the ACL femoral attachment site changes significantly depending on the arthroscopic portal used. Viewing the ACL femoral attachment site through the AM portal provides an orthogonal view of the lateral wall of the notch, allowing accurate assessment of the ACL femoral tunnel position in both the shallow-deep and high-low directions (Fig. 13).
Fig. 13.
AM portal view at 90° of flexion (arthroscopic position). In the arthroscopic terminology, directions along the lateral wall of the intercondylar notch are referred to as: high or superior, low or inferior, shallow and deep. The directions using the corresponding anatomical terminology (shown in parentheses) which references the knee in the extended position are: anterior, posterior and distal. Remnant ligament fibres of the native ACL are seen along the lower third of the lateral wall of the notch
As a result, the AM portal is the preferred portal for viewing the anatomical ACL femoral attachment site. Viewing the ACL femoral attachment site through the AM portal also eliminates the need to perform a routine notchplasty for visualisation purposes. Avoid using a curette, motorised shaver blade or burr to initially perform a notchplasty or to completely remove all of the soft tissue remnants from the lateral wall of the notch as this destroys the remaining native ACL fibres and underlying bony landmarks.
To use the native ACL footprint method:
View the lateral wall of the notch with the scope in the AM portal. Insert a 90° bipolar thermal probe through the AAM and mark the borders of the native ACL femoral attachment site.
Insert a 45° angle microfracture awl through the AAM and mark the centre of the ACL femoral attachment site.
Using the lateral intercondylar and bifurcate ridges
When soft tissue remnants are not present at the native ACL femoral attachment site, the underlying bony morphology of the ACL femoral attachment site can provide useful anatomical landmarks to assist with anatomical ACL femoral tunnel placement. Anatomical studies have demonstrated that the ACL femoral attachment site is defined by two osseous ridges [9]. The lateral intercondylar ridge (“resident’s ridge”) runs at approximately a 30–35° angle with respect to the long axis of the femoral shaft and represents the upper or superior limit of the ACL femoral attachment site. The lateral intercondylar ridge has been shown to be present and visible in 88–100 % of chronic ACL-deficient knees [10, 11]. When present, the lateral intercondylar ridge is critical to anatomical ACL femoral tunnel placement since the ACL femoral attachment site always lies below or inferior to this ridge. In some knees it may be possible to identify a second bony ridge, the lateral bifurcate ridge, which separates the attachment sites of the AM and PL bundle fibres [9]. It is important to remember that because the cross-sectional area of the PL and AM bundles is variable from patient to patient, the location of the bifurcate ridge, when present, does not necessarily represent the true centre of the ACL femoral attachment site (Fig. 14).
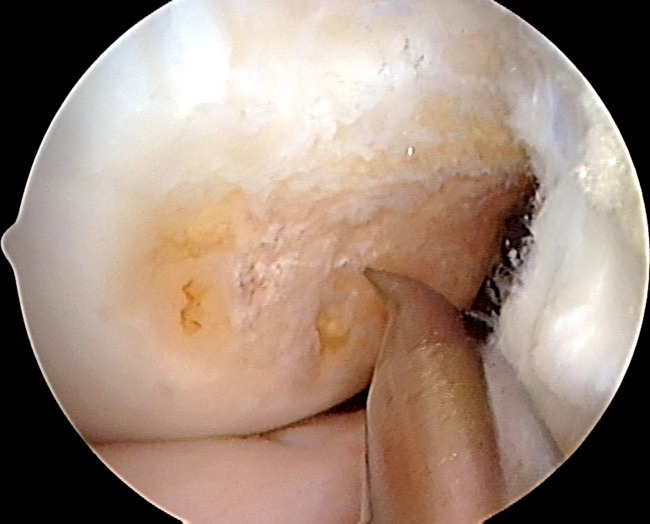
Fig. 14.
View through the AM portal at 90° of flexion. The lateral intercondylar and bifurcate ridges are clearly visible
To use the lateral intercondylar and bifurcate ridges method:
Use a bipolar 90° thermal probe to remove soft tissue along the lower third of the lateral wall of the notch.
With the knee at 90° of flexion, identify the lateral intercondylar ridge and the margin of the lower articular cartilage border. The lateral intercondylar ridge is most easily identified by starting the dissection in the lower part of the footprint and working in the superior (high) direction. A distinct end point will be encountered as the thermal probe contacts the ridge. The centre of the ACL femoral attachment site in the high-low direction is located halfway between these two landmarks (Fig. 15).
Identify the bifurcate ridge as a shelf or prominence perpendicular to the intercondylar ridge in the mid part of the footprint insertion area.
Position the tip of a 30° or 45° angle microfracture awl through the AAM and mark the centre of the ACL femoral attachment site at a point just deep to the bifurcate ridge and at the mid high-low position as described.
Fig. 15.
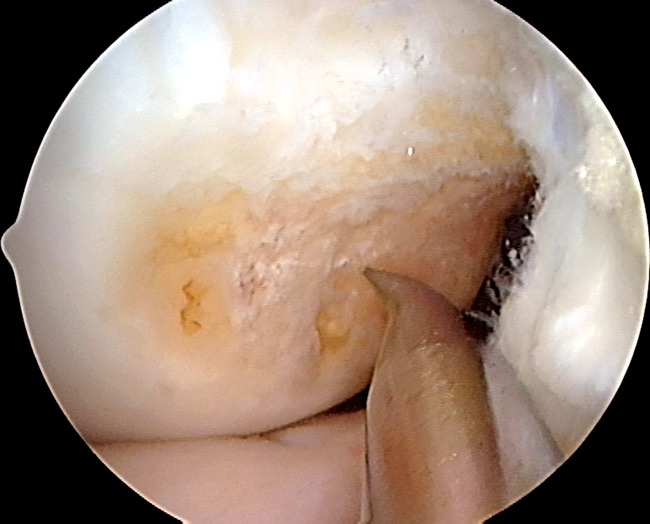
AM portal view at 90°. Microfracture awl tip is positioned halfway between the lateral intercondylar ridge and the inferior (low) articular cartilage margin
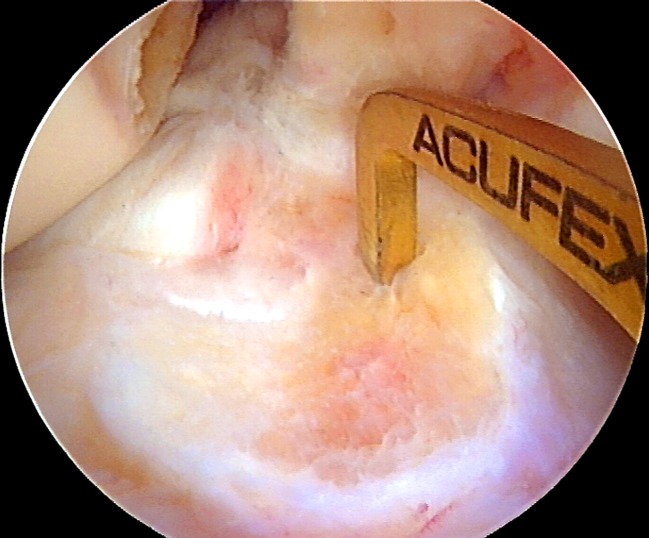
Using a ruler
A curved ruler allows the surgeon to individualise the location of the ACL femoral tunnel based on the specific anatomy of the patient. Bird et al. [12] validated this technique for finding the midbundle position showing that a point 50 % along the lateral wall of the notch as described below accurately identifies the midbundle position. This approach allows for “à la carte” or patient-specific surgery to be performed versus the “one size fits all” approach associated with the use of offset ACL femoral aimers.
With the knee at 90° of flexion, place the arthroscope in the AM portal to view the ACL femoral attachment site.
Bend the ruler to approximately a 45° angle at the 24 mm mark to allow it to lie flat along the lateral wall of the notch.
Insert the ACL ruler into the knee joint through either the AL or the AAM portal (Fig. 16). Inserting the ruler through the AL portal allows a microfracture awl to be inserted through the AAM portal, giving the surgeon the ability to measure and simultaneously mark the ACL femoral attachment site. However, due to the height of the AL portal above the lateral joint line, in some knees it may be more difficult to position the ACL ruler lower down the sidewall of the notch at the ACL femoral attachment site. In this situation, it may be advantageous to insert the ruler through the AAM. The lower position of the AAM portal allows the ruler to be easily positioned at the ACL femoral attachment site.
If remnant fibres of the ACL are clearly visible, measure the length of the ACL femoral attachment site along the long axis of the footprint using the ACL ruler (Fig. 17).
To create an ACL femoral tunnel located in the centre of the ACL femoral attachment site, the centre of the ACL femoral tunnel should be located at a shallow-deep position that is 50 % of the measured length of the ACL femoral attachment site (Fig. 18). The high-low placement of the ACL femoral tunnel should be halfway between the top and bottom of the footprint, effectively six millimetres above the low border of the articular margin when the knee is at 90°.
If there are no remnant fibres of the ACL clearly visible, insert the ruler into the notch until the tip is positioned at the proximal (deep) border of the articular cartilage. The proximal cartilage border represents the deep point of the ACL femoral attachment site. The length of the side wall of the notch is measured where the ACL ruler touches the shallow margin of the articular cartilage (Fig. 19) [12].
-
Insert a 45° microfracture awl through the AAM portal and use it to mark the location of the femoral tunnel. The centre of the femoral tunnel should be located at a shallow-deep position that is 50 % of the measured distance from the deep aspect of the ACL femoral attachment site to the shallow articular cartilage margin. The high-low position of the ACL femoral tunnel is located halfway between the lateral intercondylar ridge and the low (posterior) articular cartilage border (Fig. 20). Effectively this is six millimetres above the low border of the articular margin when the knee is at 90°.
Note:At 90° of flexion, in order to avoid any tendency to position the start point of the femoral tunnel too shallow, it is important to ensure the ruler start or ‘0’ point is held at the proximal margin of the articular cartilage. Any movement of the ruler as the scope is moved should be avoided.
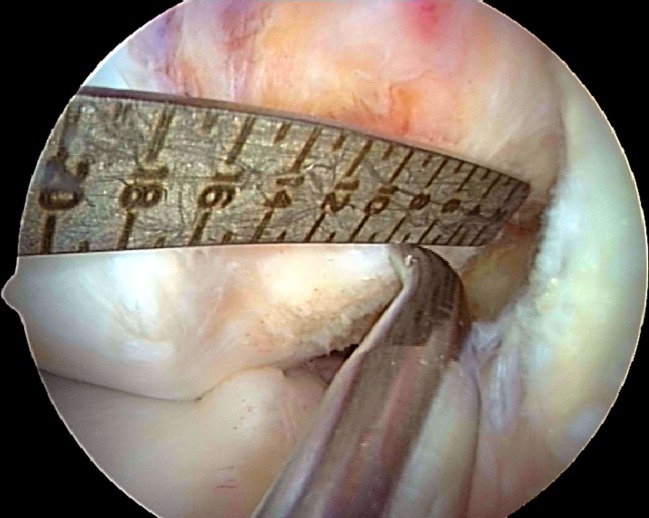
Fig. 16.
View through the AM portal at 90° of flexion. The ACL ruler has been bent to lie flat along the lateral wall of the intercondylar notch. The ruler is inserted through the AL portal and is positioned to lie parallel to the wall of the notch just below the lateral intercondylar ridge (dotted line)
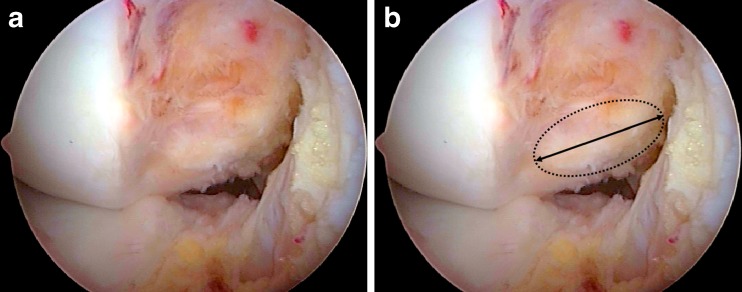
Fig. 17.
AM portal view at 90° of flexion. Remnant fibres of the native ACL are seen along the lateral wall of the notch. The ACL femoral attachment site is shown by the dotted ellipse. The length of the ACL femoral attachment site length is measured along its long axis (black line)
Fig. 18.
AM portal view at 90° of flexion, same knee as shown in Fig. 17. The ACL ruler is inserted through the AL portal and the 45° microfracture awl through the AAM portal. In this case, the ACL femoral attachment site length measures 14 mm, so the centre of the ACL femoral tunnel is placed at the 7 mm mark
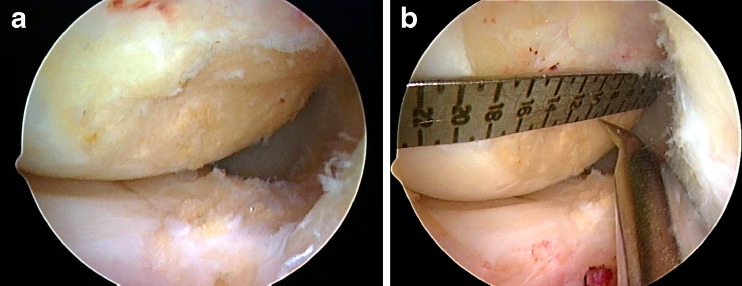
Fig. 19.
Chronic ACL-deficient knee. AM portal view at 90° of flexion. a The lateral intercondylar ridge is clearly seen. However, there are no remnants of the native ACL fibres visible. b The ACL ruler is inserted through the AL portal. The length of the lateral wall of the notch measures 18 mm. A 45° microfracture awl is inserted through the AAM portal and is used to mark the ACL femoral attachment site at 9 mm, which represents 50 % of the measured lateral wall length
Fig. 20.
AM portal view at 90°. The tip of the 45° microfracture awl is placed halfway between the lateral intercondylar ridge and the low (posterior) articular cartilage margin and 50 % of the length of the ACL femoral attachment site as measured using the ACL ruler. Note that in this particular case, the centre of the ACL femoral attachment site lies slightly deep (proximal) to the lateral bifurcate ridge
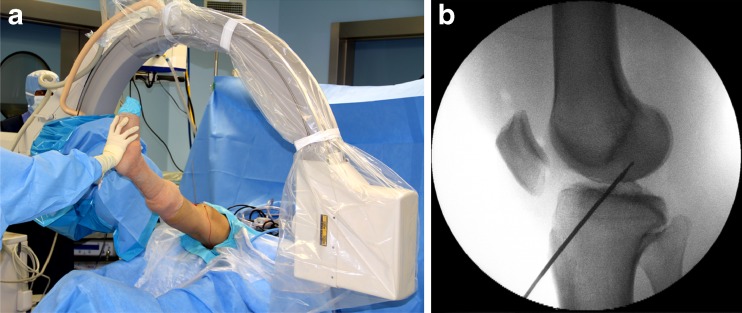
Using intra-operative fluoroscopy
At present, intra-operative fluoroscopy is the most accurate method to measure and document ACL femoral tunnel placement [13, 14]. Fluoroscopy gives the surgeon the ability to intra-operatively measure and change the ACL femoral tunnel position, and also serves as a quality control for the ACL femoral tunnel position.
With the knee at 90° of flexion and the 45° microfracture awl positioned at the chosen ACL femoral tunnel location, a sterile draped digital C-arm is used to take a true lateral radiograph of the knee. A true lateral radiograph is one in which the inferior and deep margins of the medial and lateral femoral condyles overlap (Fig. 21a, b).
The grid system described by Bernard and Hertel is used to measure the position of the ACL femoral tunnel (Fig. 22a, b) [15]. This method is easy to use, is reproducible and has been shown to be independent of knee size, shape and the distance between the X-ray tube and the patient [15].
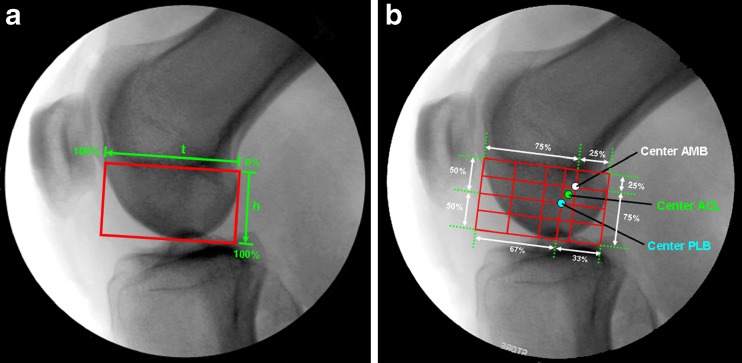
Fig. 21.
a Intra-operative C-arm. b True lateral image of the knee. The microfracture awl is positioned at the centre of the ACL femoral attachment site
Fig. 22.
a Bernard and Hertel grid. b The centre of the AM and PL bundles are shown according to the data of Columbet et al. [16]. In this study, the centre of the AM bundle was found to lie at a point 25 % along Blumensaat’s line (t) and 25 % along line h. The centre of the PL bundle was located at a point 33 % along line t and 50 % along line h
How to draw the Bernard and Hertel grid:
Draw a tangent to the roof of the intercondylar notch (Blumensaat’s line). Draw two lines perpendicular to that line, one at the intersection of the tangent line with the shallow border of the lateral femoral condyle and the other with intersection of the tangent line and the deep border of the lateral femoral condyle. The lateral femoral condyle can be identified by an indentation (Grant’s notch) and the fact that the medial femoral condyle extends more distal.
Draw another line parallel to Blumensaat’s line and tangent to the inferior border of the condyles. Measurements are made as percentages along Blumensaat’s line (t), which represents the maximum sagittal diameter of the lateral femoral condyle, and line h, which represents the maximum intercondylar notch height.
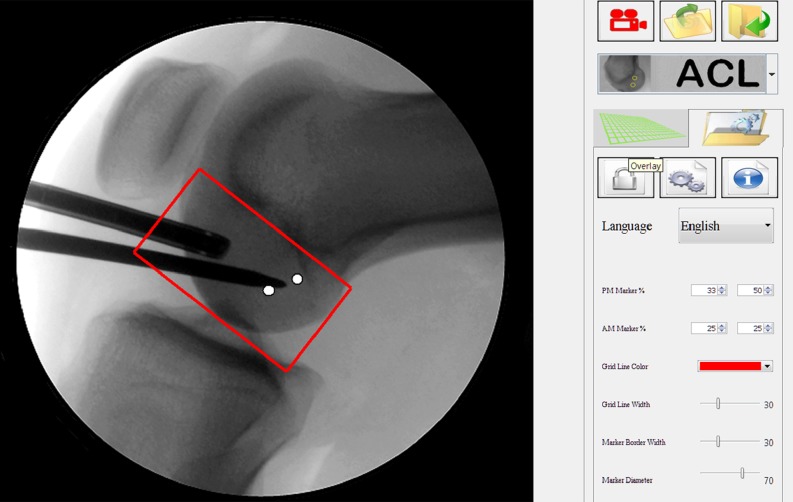
Intra-operatively, the ACUFEX DIRECTOR APPLICATION Anatomic Guide (Smith & Nephew, London, UK) software can be used to plot the Bernard and Hertel grid on the C-arm image. Alternatively the images can be saved to an image capture unit and the grid applied later as a quality control check (Fig. 23). The microfracture awl position can be adjusted under arthroscopic and fluoroscopic guidance until the desired position is obtained.
Fig. 23.
The ACUFEX DIRECTOR APPLICATION Anatomic Guide software was used to plot the location of the AM and PL bundles (white circles) based on the data of Columbet et al. [16]. The software also allows other coordinates for the centre of the AM and PM bundles to be selected. In this example, the tip of the microfracture awl is positioned halfway between the centre of the AM and PL bundles (white circles). This location would position the ACL femoral tunnel in the centre of the ACL femoral attachment site
Using any or all of the above guidelines eliminates the need to use an offset ACL femoral aimer and referencing off the “over-the-top” position (which is different to the start point of the ruler measurement) to determine the femoral tunnel placement. Offset ACL aimers can constrain the location of the femoral guide pin and can lead to non-anatomical placement of the ACL femoral tunnel. The above guidelines allow the surgeon to select and verify the location of the ACL femoral tunnel position using established anatomical and radiographic landmarks.
Drilling the femoral tunnel
After selecting and confirming the desired location for the ACL femoral tunnel, use a 45° microfracture awl to mark the location along the lateral wall of the notch.
-
Insert a 0° mm offset guide through the AAM portal and place it at the desired location for the ACL femoral tunnel. Slowly flex the knee to 120° or higher. Increasing the degree of knee flexion increases the ACL femoral tunnel length.
Note:Hyperflexion of the knee results in a loss of joint distension due to external compression of the knee joint capsule by the soft tissues of the thigh. This can result in bleeding and a loss of joint visualisation due to encroachment of the fat pad into the notch. To maintain adequate joint distension and visualisation, it is necessary to increase the fluid pressure up to 120 mmHg while working in the notch with the knee in hyperflexion. Decrease the pump pressure to the normal setting after the ACL femoral tunnel has been drilled and the knee is extended back to 70–90° of flexion. If the fat pad still obscures visualisation, limited resection of the fat pad should be performed using a motorised shaver blade inserted through the AAM.
Insert a 2.7 mm drill tip graduated guide pin through the 0 mm offset aimer and use a small mallet to tap the drill tip part of the guide pin into the pilot hole created by the microfracture awl (Fig. 24).
Keeping the tip of the 2.7 mm drill tip guide pin in the pilot hole, slowly angle the handle of the 0° mm offset aimer laterally and tap the guide pin into the lateral wall of the notch until the drill tip part of the guide pin is fully buried into the bone. This manoeuvre increases the obliquity of the guide pin relative to the lateral wall of the notch, resulting in a longer femoral tunnel length and a more elliptically shaped tunnel aperture (Fig. 24) [7]. An elliptically shaped tunnel covers more of the ACL femoral attachment site and more closely reproduces the anatomy of the native ACL attachment site versus a circular-shaped femoral tunnel [7].
Slowly drill the 2.7 mm drill tip graduated guide pin through the lateral femoral condyle until the resistance of the lateral femoral cortex is encountered.
-
Note the depth mark on the graduated drill tip passing pin at the point of maximum resistance. This distance will provide a good estimate of the ACL femoral tunnel length. If the resulting ACL femoral tunnel length is significantly less than desired, it is possible to increase the femoral tunnel length by reversing the guide pin back to the entry point, angling the offset aimer more laterally and increasing the knee flexion angle. These manoeuvres can often redirect the drill tip guide pin more proximally up the femoral shaft, producing a longer femoral tunnel length.
Note:Do not use power to initially insert the femoral guide pin into the bone. The guide pin will skive off the pilot hole if power is initially used. Guide pin breakage can also occur if an attempt is made to simultaneously angle and drill the femoral guide pin into the bone under power. To prevent guide pin breakage, ensure that the drill tip portion of the guide pin is fully inserted into the bone before using power to drill the pin through the bone.
-
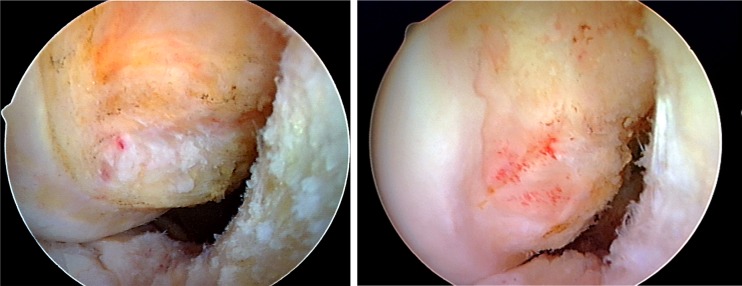
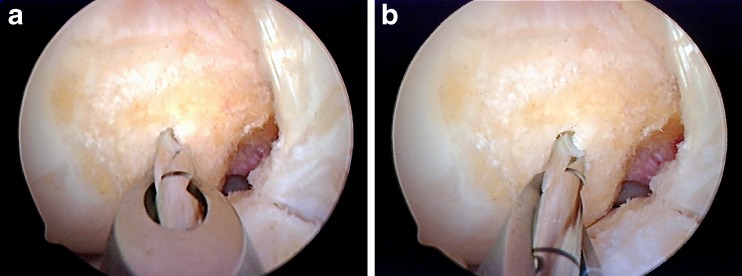
Drill the ACL femoral socket using an endoscopic drill bit that corresponds to the diameter of the ACL graft (Fig. 25a, b).
Note:If an ENDOBUTTON CL implant is used as the ACL femoral fixation device, use a 4.5 mm ENDOBUTTON drill bit to drill a tunnel through the lateral femoral cortex. Measure the length of the femoral tunnel by noting the mark on the ENDOBUTTON drill bit at the time of cortical breakthrough. The ACL femoral tunnel length can also be measured by slowly withdrawing the ENDOBUTTON drill bit until the fluted part of the drill bit is felt to engage the lateral femoral cortex. The distance at the femoral tunnel entrance is noted and 10 mm (the length of the fluted part of the 4.5 mm ENDOBUTTON drill bit) is subtracted to obtain the ACL femoral tunnel length.
Note: Knowing the length of the ACL femoral tunnel allows the femoral socket to be drilled all the way to the femoral cortex. Drilling the femoral socket close to the lateral femoral cortex will allow room for the ENDOBUTTON fixation device to flip in all situations, eliminating the need to calculate how deep to drill the femoral socket.
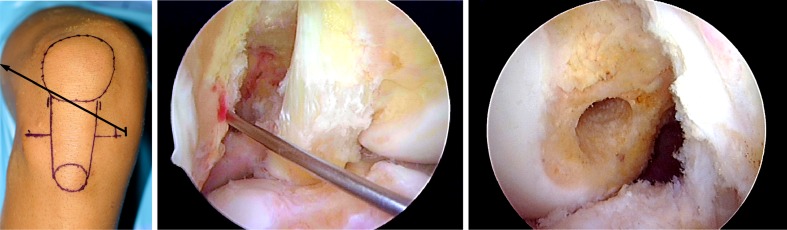
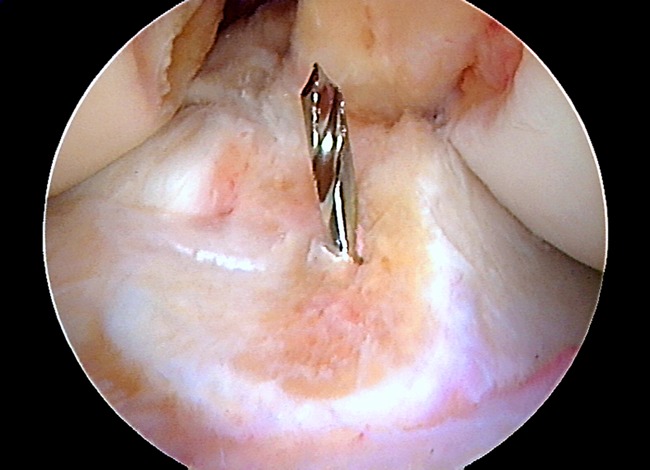
Fig. 24.
AM portal view in hyperflexion. a The femoral drill tip passing pin is oriented perpendicular to the lateral wall of the notch. This guide pin orientation will result in a short femoral tunnel length and a more circular shape of the ACL femoral tunnel aperture. b The 0° offset aimer has been angled laterally which results in the femoral guide pin being oriented more obliquely to the lateral wall of the notch. A more oblique orientation of the guide pin will increase the length of the ACL femoral tunnel and produce a more elliptically shaped femoral tunnel aperture [7]
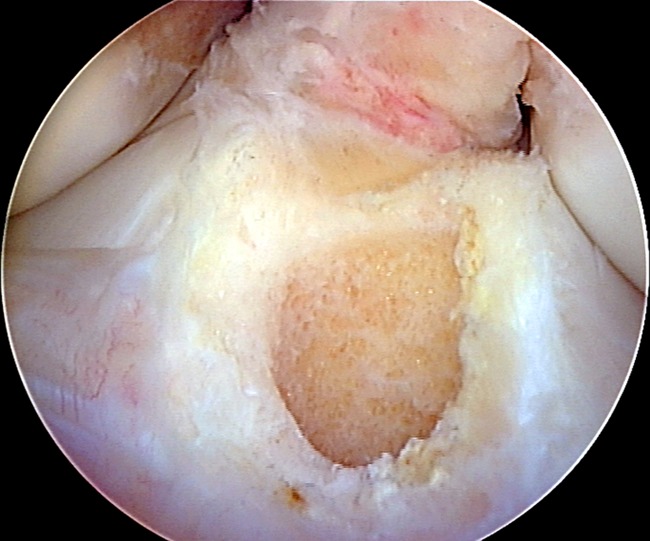
Fig. 25.
a AM portal view in hyperflexion. The endoscopic drill bit is inserted into the intercondylar notch through the AAM portal and is seen to lie at the centre of the ACL femoral attachment site. b AM portal view at 90°. The elliptically shaped aperture of the ACL femoral tunnel is centred in the ACL femoral footprint
Damage to the medial femoral condyle which can be caused by an endoscopic reamer introduced through the AAM portal can be avoiding by using the “passing pin manoeuvre” described by Siebold et al. [17]. Due to their smaller diameter, this technique is rarely necessary in the case of hamstring tendon ACL grafts. Iatrogenic damage to the cartilage of the medial femoral condyle is more likely to occur in the situation where a ten millimetre drill bit is used to drill the femoral socket for a bone-patellar tendon-bone or bone-quadriceps tendon graft. In this manoeuvre, the femoral guide pin is drilled out through the lateral soft tissues in the usual fashion. To avoid damage to the articular cartilage from the endoscopic reamer, the drill tip end of the femoral guide pin is reversed until the tip of the guide pin is visible in the intercondylar notch.
The guide pin is then angled away from the medial femoral condyle and the cannulated endoscopic reamer inserted over the guide pin into the notch. Once the endoscopic reamer has safely bypassed the medial femoral condyle, the tip of the guide pin is reinserted into its original hole in the lateral wall of the notch. Having safely bypassed the medial femoral condyle, the femoral socket can be drilled in the conventional fashion. To withdraw the endoscopic reamer, the passing pin is withdrawn from the femoral tunnel, and the reamer manoeuvred into the notch away from the medial femoral condyle and the reamer safely removed from the joint.
If a three-portal technique has been used, fluid flow and visualisation in the notch with the knee in hyperflexion can be facilitated by introducing a motorised shaver blade through the AL portal. The suction on the shaver can be used to maintain fluid flow and to suction bone debris created during the drilling of the ACL femoral tunnel, thus maintaining a clear visual field. The shaver can also be used to resect any portions of the fat pad restricting passage of the endoscopic reamer or obstructing visualisation in the notch.
Load a #2 or #5 polyester suture into the slotted end of the 2.7 mm drill tip passing pin and pass the free ends of the suture out through the lateral soft tissues, leaving the looped end of the suture in the ACL femoral tunnel.
Chamfer the edges of the ACL femoral tunnel with an ACL chamfer rasp to minimise abrasion of the ACL graft.
In chronic cases with notch osteophytes or in patients with small width notches, a limited wallplasty at the shallow border of the notch is performed using a small curved compound gouge (Fig. 26). If required, the wallplasty should be performed after the ACL femoral tunnel has been drilled to avoid lateralising the position of the ACL femoral tunnel. Use a motorised shaver blade to contour and flatten the wall of the notch.
Fig. 26.
Chronic ACL-deficient knee with osteophytes along the lateral wall of the intercondylar notch. After drilling the ACL femoral tunnel, a curved compound gouge is used to excise the osteophytes along the lateral wall and widen the width of the intercondylar notch
Drilling the tibial tunnel
The tibial tunnel is performed with the knee at 70–90° of flexion. While viewing through the AM or AL portal, insert an ACL tibial guide set at a 55° angle with a tip aimer through the AM or AAM portal into the knee joint. Position the tip of the aimer 2–3 mm anterior to the posterior margin of the anterior horn of the lateral meniscus and slightly medial to midline of the ACL tibial attachment site (Fig. 27).
Mark the ACL tibial aimer bullet with a surgical marker at the desired tibial tunnel length.
Position the bullet medial to the crest of the tibia, in the middle of the skin incision used to harvest the ACL graft. Raise or lower the handle of the tibial guide aimer until the mark on the bullet is located at the end of the aimer handle when the bullet is flush with the anterior cortex of the tibia. These steps allow a tibial tunnel of a known length to be drilled, thus allowing the issue of graft-tunnel length mismatch to be addressed.
-
Drill a 2.4 mm drill tip guide pin into the tibia until the resistance of the aimer tip is encountered.
Note: Avoid drilling the tibial guide pin completely into the knee joint as this will result in the guide pin hitting the tip of the tibial aimer and deflecting away from its intended target. Instead, remove the tibial aimer from the joint and use a small mallet to tap the 2.4 mm drill tip guide pin until it is visible in the joint.
Fig. 27.
The tip of the ACL tip aimer is positioned slightly anterior to the posterior margin of the anterior horn of the lateral meniscus and slightly medial to the midline of the tibial footprint
In general, the tip of the tibial passing pin should lie one to two millimetres anterior to the posterior margin of the anterior horn of the lateral meniscus and slightly medial to the midline of the ACL tibial attachment site (Fig. 28). The most common error made when converting from the transtibial tunnel technique to the AM portal technique is to position the tibial guide pin in the posterior half of the ACL tibial attachment site.
Fig. 28.
The tibial guide pin is positioned slightly anterior to the posterior margin of the anterior horn of the lateral meniscus and slightly medial to the midline of the insertion site
Note:Placement of the tibial guide pin posterior to the posterior margin of the anterior horn of the lateral meniscus will result in a non-anatomical tibial tunnel positioned in the region of the PL bundle. Positioning the tibial guide pin too far laterally in the ACL tibial attachment site can result in impingement of the ACL graft against the lateral wall of the notch.
Due to the large degree of variability of the intercondylar notch roof angle and the amount of knee hyperextension from patient to patient, it is extremely helpful to use fluoroscopy to confirm correct anterior-posterior placement of the ACL tibial guide pin.
-
Place the knee in maximum extension and obtain a true lateral radiographic view of the knee (Fig. 29).
Note:For soft tissue grafts, which will be centred along the line of the guide pin, the tibial guide pin should lie approximately 4–5 mm posterior to Blumensaat’s line. For bone-patellar tendon-bone grafts the tibial guide pin placement can be approximately 2–3 mm posterior to Blumensaat’s line since the patellar tendon graft fibres are offset from the bone block and will come to lie posterior to the line of the guide pin.
Fig. 29.
The C-arm is used to take a lateral radiograph of the knee in full hyperextension
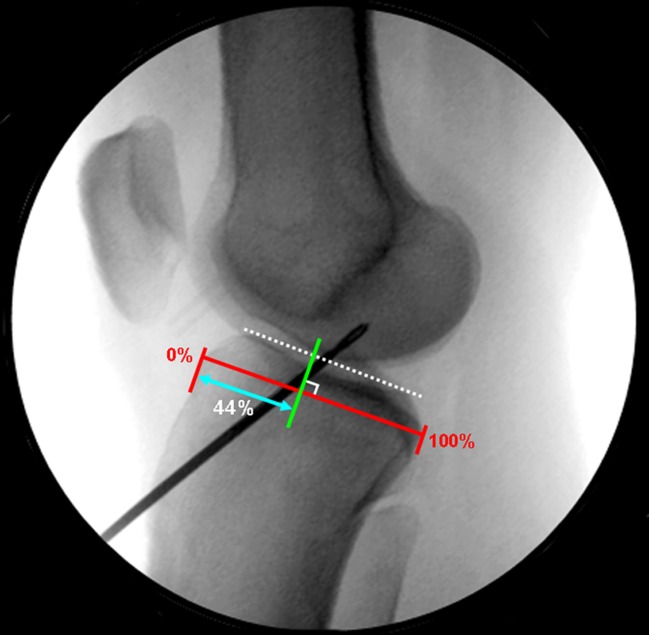
Measuring the ACL tibial guide pin position
The ACUFEX DIRECTOR APPLICATION Anatomic Guide software can be used to accurately analyse and measure the position of the ACL tibial guide pin in the sagittal plane.
Measure the tibial guide pin position using the method of Amis and Jakob (Fig. 30) [18]. The goal is to place the tibial guide pin in the centre of the ACL tibial insertion site, which has been shown to lie at 41–44 % along the Amis-Jakob line [19].
With proper placement of the tibial guide pin confirmed, use a fully fluted cannulated drill bit sized equal to the measured diameter of the ACL graft to drill the tibial tunnel (Fig. 31).
Small adjustments in the final position of the ACL tibial tunnel can be made by first using a 5 mm drill bit to drill the initial tibial tunnel. Adjustments to the final tibial tunnel position can be made by maintaining and repositioning the tibial guide pin eccentrically in the tibial tunnel using a small clamp. The tibial guide pin can be moved in the desired direction and the tibial tunnel drilled sequentially by one millimetre increments up to the desired size of the tunnel using an endoscopic drill bit.
In the situation where the tibial guide pin is malpositioned more than three to four millimetres, the tibial guide pin can be exchanged leaving the original malpositioned guide pin in place, repositioning the tip of the ACL tibial aimer at the desired intra-articular location and changing the external starting point of the aimer on the tibia. Leaving the original guide pin in place prevents the new guide pin from tracking up the path of the original guide pin.
Fig. 30.
Amis-Jakob line [18]. The medial joint line is marked by the dotted white line. The Amis-Jakob line (red line) passes through the posterior corner of the widest part of the medial tibial plateau (square posterior border) parallel to the medial joint line. The anterior tibial cortex represents 0 % and the posterior tibial cortex 100 % of the sagittal width of the tibia. The tibial guide pin position is calculated by dropping an orthogonal line (green line) from the point where the tibial guide pin crosses the medial joint line onto the Amis-Jakob line. The distance from the anterior tibial cortex (0 %) to the orthogonal projection onto the Amis-Jakob line (blue line with arrowheads) is represented as a percentage of the total length of the Amis-Jakob line. The tibial guide pin in this case is located at 44 % along the Amis-Jakob line, which places the guide pin in the centre of the ACL tibial attachment site
Fig. 31.
The tibial tunnel is elliptically shaped and in this case almost completely restores the cross-sectional area of the ACL tibial attachment site
Graft insertion into the tibial and femoral tunnels
Use an arthroscopic probe or grasper to retrieve the suture loop that was left in the ACL femoral tunnel and pull the suture out of the knee joint through the tibial tunnel. Pass the passing sutures for the ACL graft through the suture loop and pass them out of the lateral thigh. The ACL graft is passed into the knee joint using the graft passing sutures.
When a femoral bone-patellar tendon-bone or bone-quadriceps tendon ACL graft is used for the ACL reconstruction, the length of the femoral bone block should not exceed 20–22 mm in length, as longer bone blocks may present difficulties during graft passage. Unlike the transtibial technique where the ACL femoral and tibial bone tunnels are collinear, drilling the ACL femoral tunnel through a medial portal results in divergence of the two tunnels. As a result, the femoral bone block of the ACL graft must rotate in the notch away from the PCL to enter the ACL femoral tunnel (Fig. 32). If the femoral bone block is longer than 20–22 mm, it may be difficult to get it to rotate in the notch and enter the femoral tunnel. It is often helpful to use an arthroscopic probe as a pulley to redirect the angle of the femoral bone block sutures in the direction of the ACL femoral tunnel.
Fig. 32.
Passing femoral bone block. An arthroscopic probe can be used to assist with rotation of the femoral bone block into the ACL femoral tunnel
ACL graft tensioning and tibial fixation
The correct angle of flexion for tensioning the ACL graft, based on the location of the ACL femoral tunnel, is shown in Table 1.
For multiple-strand hamstring tendon ACL grafts, use a graft tensioning device applied to opposite ends of the ACL graft limbs and apply 10–15 N of force per strand (40–80 N total).
For multiple-strand hamstring tendon ACL grafts, cycle the knee from 0 to 90° for a minimum of 30 cycles with an 80 N preload applied to the ACL graft using a graft tensioning device.
Fix the multiple-strand hamstring tendon ACL graft at the flexion angle shown in Table 1 with the graft tensioned to 10–15 N per strand (40–80 N).
Insert the 30° arthroscope into the AL or AM portal and check for wall and roof impingement of the ACL graft (Fig. 33).
Table 1.
Correct angle of knee flexion for tensioning of the ACL graft for different femoral tunnel positions
| Femoral tunnel position | Tension the ACL graft at |
|---|---|
| Near the centre of the AM attachment site | 45° |
| Near the centre of the ACL attachment site | 20° |
| Near the centre of the PL bundle | 0° |
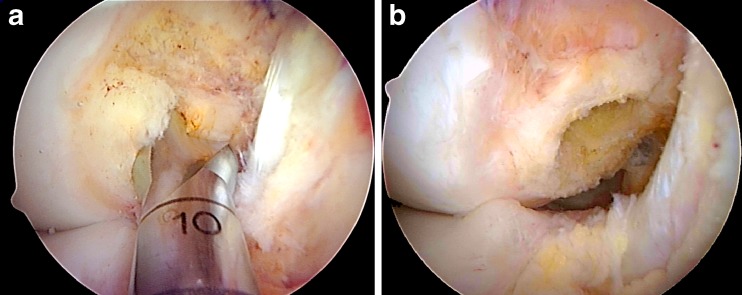
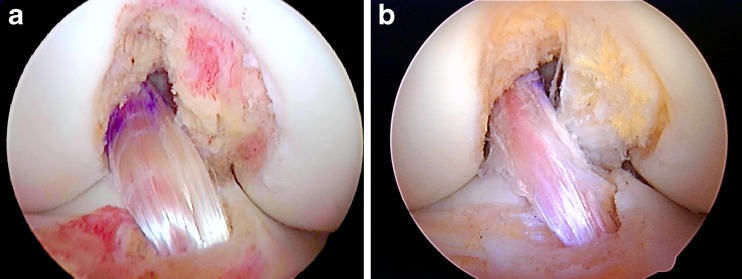
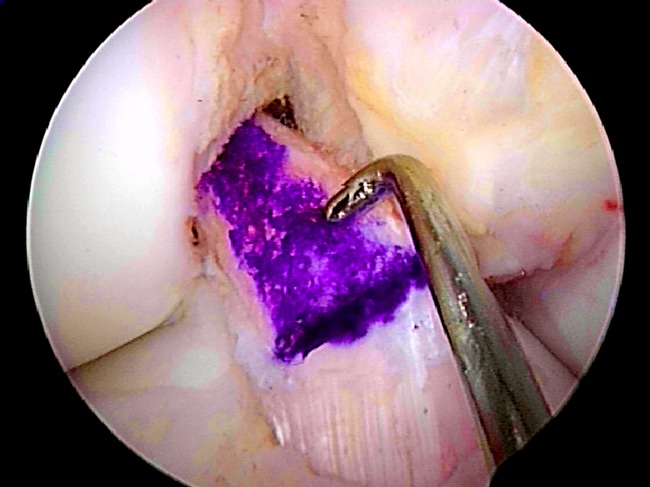
Fig. 33.
a Six-strand (9.5 mm) hamstring ACL graft, b 10 mm bone-patellar tendon-bone ACL graft
Closure
Finally the knee stability is tested and all wounds are closed. Dressings are applied and the patient is returned to the recovery area. Full weight-bearing as tolerated is allowed immediately, but cycling is restricted until six weeks at the earliest in order to avoid cyclical creep on the graft
Conclusion
Anatomical ACL reconstruction requires an understanding of ACL insertion anatomy and an understanding of the various methods currently used to identify the anatomy and to identify the true insertion points. We have outlined the importance of the AM viewing portal to better understand the insertion anatomy and we have outlined a variety of methods for accurately determining the midbundle femoral and tibial attachment points. This detailed description should enable surgeons to be confident in their anatomical understanding of ACL reconstructive surgery.
References
- 1.Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 2.Marchant B, Noyes F, Barber-Westin S, Fleckenstein C. Prevalence of nonanatomical graft placement in a series of failed anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38:1987–1996. doi: 10.1177/0363546510372797. [DOI] [PubMed] [Google Scholar]
- 3.Kato Y, Ingham JM, Kramer S, Smolinski P, Saito P, Fu F. Effect of tunnel position for anatomic single-bundle ACL reconstruction on knee biomechanics in a porcine model. Knee Surg Sports Traumatol Arthrosc. 2010;18:2–10. doi: 10.1007/s00167-009-0916-8. [DOI] [PubMed] [Google Scholar]
- 4.Driscoll MD, Isabell GP, Conditt MA, Ismaily BS, Jupiter DC, Noble PC, Lowe WR. Comparison of 2 femoral tunnel locations in anatomic single-bundle anterior cruciate ligament reconstruction: a biomechanical study. Arthroscopy. 2012;28:1481–1489. doi: 10.1016/j.arthro.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A, Musahl V, Steuber V, Kendoff D, Choi D, Allen AA, Pearle AD, Altchek DW. Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy. 2011;27:380–390. doi: 10.1016/j.arthro.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Steiner ME, Battaglia TC, Heming JF, Rand JD, Festa A, Baria M. Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:1912–1919. doi: 10.1177/0363546509340407. [DOI] [PubMed] [Google Scholar]
- 7.Hensler D, Working Z, Illingworth K, Thorhauer E, Tashman S, Fu F. Medial portal drilling: effects on the femoral tunnel aperture morphology during anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2011;93:2063–2071. doi: 10.2106/JBJS.J.01705. [DOI] [PubMed] [Google Scholar]
- 8.Siebold R. The concept of complete footprint restoration with guidelines for single- and double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:699–706. doi: 10.1007/s00167-010-1376-x. [DOI] [PubMed] [Google Scholar]
- 9.Ferretti M, Ekdahl M, Shen W, Fu F. The topography of the femoral insertion of the anterior cruciate ligament: an anatomical study. Arthroscopy. 2007;23:1218–1225. doi: 10.1016/j.arthro.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Van Eck C, Morse K, Lesniak B, Kropf E, et al. Does the lateral intercondylar ridge disappear in ACL deficient patients. Knee Surg Sports Traumatol Arthrosc. 2010;18:1184–1188. doi: 10.1007/s00167-009-1038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shino K, Suzuki T, Iwahashi T, Mae T, et al. The resident’s ridge as an arthroscopic landmark or anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1164–1168. doi: 10.1007/s00167-009-0979-6. [DOI] [PubMed] [Google Scholar]
- 12.Bird J, Carmont M, Dhillon M, Smith N, Brown C, Thompson P, Spalding T. Validation of a new technique to determine midbundle femoral tunnel position in anterior cruciate ligament reconstruction using 3-D computed tomography analysis. Arthroscopy. 2011;27:1259–1267. doi: 10.1016/j.arthro.2011.03.077. [DOI] [PubMed] [Google Scholar]
- 13.Lobenhoffer P, Bernard M, Agneskirchner J. Quality assurance in cruciate ligament surgery. Arthroscopie. 2003;16:202–208. doi: 10.1007/s00142-003-0230-2. [DOI] [Google Scholar]
- 14.Passler H, Hoher J. Intraoperative quality control of the placement of bone tunnels for the anterior cruciate ligament. Unfallchirurg. 2004;107:263–272. doi: 10.1007/s00113-004-0745-7. [DOI] [PubMed] [Google Scholar]
- 15.Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg. 1997;10:14–22. [PubMed] [Google Scholar]
- 16.Columbet P, Robinson J, Christel P, Franceschi J-P, et al. Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy. 2006;22:984–992. doi: 10.1016/j.arthro.2006.04.102. [DOI] [PubMed] [Google Scholar]
- 17.Siebold R, Benetos I, Sartory N, He Z, et al. How to avoid the risk of intraoperative cartilage damage in anatomic four tunnel double bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:64–67. doi: 10.1007/s00167-009-0967-x. [DOI] [PubMed] [Google Scholar]
- 18.Amis A, Jakob R. Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthrosc. 1998;6(Suppl 1):S2–S12. doi: 10.1007/s001670050215. [DOI] [PubMed] [Google Scholar]
- 19.Staubli HU, Rauschning W. Tibial attachment area of the anterior cruciate ligament in the extended knee position. Anatomy and cryosections in vitro complemented by magnetic resonance arthrography in vivo. Knee Surg Sports Traumatol Arthrosc. 1994;2:138–146. doi: 10.1007/BF01467915. [DOI] [PubMed] [Google Scholar]