Abstract
Purpose
Although the short- and mid-term outcomes of ACL reconstruction with a hamstring graft are promising, clinical investigations reporting the long-term results after ten years or longer are rare. Therefore we performed a retrospective single-blinded evaluation of ACL reconstruction using a four-stranded single-bundle reconstruction with a semitendinosus tendon graft with extracortical fixation.
Methods/Results
At follow-up patients obtained at least the same level in the clinical outcome scores (Lysholm, IKDC, Tegner) compared to previous studies with a similar follow-up time using a STG graft. Furthermore there was no detectable difference in the incidence of osteoarthritis. Patients having a negative pivot shift test showed significantly fewer signs of radiographic osteoarthritis and better functional assessment scores.
Conclusion
On the basis of our investigation, we conclude that the reconstruction of the ACL by a quadrupled semitendinosus tendon graft with extracortical anchorage can achieve excellent clinical and subjective results after a follow-up of ten years.
Introduction
Reconstruction of the ACL is a well-established procedure worldwide. It is estimated that more than 200,000 ACL reconstructions are performed annually in the United States and the incidence of ACL injury is roughly one in 3,000 per year [1]. There have been significant technical advances during recent decades to treat ACL insufficiency and many studies have documented the successful results of contemporary arthroscopic ACL reconstruction [2]. Therefore several different auto- and allografts have been described. The bone–patellar tendon–bone (BPTB) graft is still one of the most commonly used methods for ACL reconstruction [3]. However, there are several postoperative disadvantages of the BPTB graft, which include anterior knee pain, quadriceps weakness and extension deficit [4]. During the last decade, there has been an increased use of hamstring tendon (HT) autografts. This is because of the lower rate of postoperative morbidity with fewer donor-site complications. However, there are several concerns about the use of HT grafts: failure to achieve immediate rigid fixation to bone, lower stiffness compared with the BPTB graft or the native ACL, risk of increased laxity at medium- to long-term follow-up, tunnel widening, weakness of the hamstring musculature with difficulties controlling internal tibial rotation, and reduced strength in deep flexion [5].
Although the short- and mid-term outcomes of ACL reconstruction with a HT graft are promising, clinical investigations reporting the long-term results after ten years or longer are rare. Furthermore the quadrupled semitendinosus tendon is larger in diameter and provides a stronger graft compared with combined semitendinosus/gracilis (STG) transplants and even patellar tendon [6]. Furthermore compared to a STG graft the gracilis tendon as an important flexor muscle can be saved. Therefore we performed a retrospective single blinded evaluation of ACL reconstruction using a four-stranded single-bundle reconstruction with an ST graft with an extracortical fixation through an Endobutton CL™ (Smith& Nephew, Andover, MA, USA) and a Suture-Disc™ (Aesculap, Tuttlingen, Germany).
Patients and methods
Inclusion and exclusion criteria
Between 01/2000 and 12/2000 the senior author performed ACL reconstructions in 101 consecutive patients. All patients had an ACL rupture diagnosed on clinical examination and confirmed at arthroscopy. In order to achieve a homogenous cohort we excluded patients with significant chondral damage (grade 3 or 4 according to the Outerbridge classification) (n = 8) or concurrent ligamental injuries [previous contralateral ACL injury (n = 6), revision ACL reconstruction (n = 9), medial or lateral collateral ligament repair (n = 6), posterior cruciate ligament insufficiency (n = 5)]. Furthermore patients with meniscal tears requiring fixation (n = 8) needed a different rehabilitation program and were not included. Eight patients (7.8 %) suffered a graft rupture during the follow-up period. Therefore 51 patients were initially eligible to participate in the study (Fig. 1).
Fig. 1.
Flowchart of patient selection
Surgical technique
All patients underwent a four-stranded single-bundle reconstruction with an ST graft. After performing a diagnostic arthroscopy verifying a complete ACL tear the semitendinosus tendon was harvested through an oblique approach on the medial side of the proximal tibia over the pes anserinus using a closed tendon stripper (Aesculap™, Tuttlingen, Germany). Then the ST graft was cut in half and the free ends were firmly sutured. In both groups the torn ACL was debrided and the anatomical tibial and femoral footprints were identified and left intact. In line with the study protocol the gracilis tendon was always left in situ and was not harvested. First the tibial tunnel was drilled using a 55° drillguide under arthroscopic view at the posterior part of the middle of the tibial ACL footprint. The tibial starting point was placed more medial than in conventional technique approximately 45° from the mechanical axes in the frontal plane. Care was taken to avoid posterior ligament impingement as the femoral tunnel was drilled through the tibia. The final drilling diameter was matched to the width of the prepared four-stranded ST graft. To create the femoral tunnel a 5-mm offset guide system (Transtibial Femoral ACL Drill Guide™, Arthrex, Naples, FL, USA) was placed transtibially at the posterior margin of the intercondylar notch. With knee flexion of at least 110° a 2.4-mm K-wire was inserted at 10 o’clock (right) or 2 o’clock (left) position with respect to the apex of the notch. After overdrilling the guide-wire with a 4.5-mm Endobutton drill through the femur to emerge on the lateral aspect of the thigh the final femoral tunnel was created by cannulated drills matched to the diameter of the prepared graft. Then the graft was placed and the femoral side was secured with an Endobutton CL™ (Smith& Nephew, Andover, MA, USA). Final tibial fixation was achieved with a Suture-Disc™ (Aesculap, Tuttlingen, Germany) at 30° of flexion after cycling under a manual tension of approximately 60 N.
Rehabilitation
A brace-free postoperative protocol for rehabilitation was used. Range of motion of the knee and isometric muscle exercises were started the day after the operation and gradually progressed on the basis of closed kinetic chain exercises. Knee flexion of more than 90° and walking with full weight bearing was allowed one month postoperatively. Indoor cycling and swimming were permitted after four weeks and running after 12 weeks. High demand pivoting sports activities were allowed after approximately 12 months.
Clinical assessment at follow-up
The final examination was performed by two independent and blinded observers (N.A.S., S.B). Both knees of the patient were covered with a stockinette to prevent any information about the operated side and the incisions. The side-to-side anterior laxity was measured using the KT-1000 knee arthrometer (MEDmetric Corporation, San Diego, CA, USA) with the knee at 20° and 60° flexion. An anterior displacement force of 134 N was applied for the tibia of both the injured and the normal uninjured leg. The differences were noted in millimeters. For overall evaluation the International Knee Documentation Committee (IKDC), Lysholm and Tegner activity scores were used. Furthermore subjective evaluation was assessed by a numeric rating scale (NRS) from 0 (very unsatisfied) to 10 (very satisfied).
Radiological assessment
Standard unilateral weight-bearing radiographic examinations in the anteroposterior view with the knee in 30° flexion and in lateral view were classified according to IKDC guidelines as follows: A, normal; B, minimal changes and barely detectable joint space narrowing; C, moderate changes and joint space narrowing of up to 50 %; D, severe changes and more than 50 % joint space narrowing. This grading has been shown to be reliable and reproducible with longitudinal data [7]. The radiographs were obtained twice, immediately after the index procedure and at follow-up. According to the requirements of the local ethics committee weight bearing radiographs of the contralateral limb could not be performed.
The tibial and femoral tunnel were studied directly postoperatively and at final follow-up and were adjusted for magnification. The margins of the bone tunnels could be identified as a thin line on the immediate postoperative radiography and were easy to identify at follow-up. The diameter of the femoral tunnel was measured at one centimetre proximal to the ACL origin and the tibial diameter one centimetre distal to the ACL insertion on the AP and lateral view. Tunnel enlargement was quantified as a ratio between the largest and the narrowest diameter of the tunnel and was compared at the two time points; immediate postoperative radiograph and at follow-up in each patient.
Statistics
All data were tested for normal distribution by means of the Kolmogorov-Smirnov test. Homogeneity of the variances was ascertained by Levene’s F-test. We used the Wilcoxon signed-rank test to compare paired continuous variables. Comparisons between the subgroups were performed with the Mann-Whitney U test. Linear regression analysis was performed to assess the relative contribution of selected variables on linear outcomes. Multiple regression analysis was used to assess the relative contribution of selected variables on dichotomous outcomes. All tests were carried out in two directions and a p-value <0.05 was regarded as significant. The statistical evaluation was performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA).
The study was approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1975 Declaration of Helsinki. All persons gave their informed consent prior their inclusion in the study.
Results
Demographic data
According to the above mentioned criteria 51 were initially eligible to participate in the study. Despite extensive searches six patients could not be located, one died from unrelated causes, and four patients declined to participate in the clinical evaluation. Therefore 40 patients (12 female, 28 male) were available for clinical and radiological follow-up at a median of ten years (range, nine to 11 years) after the index operation. The median age at surgery was 29 years (range, 18–52 years). The majority of injuries occurred during sports activity: soccer (n= 20), skiing (n = 9), handball (n = 3) and basketball (n = 3). In two patients, injury occurred at work and in three patients during other activities.
Clinical examinations (range of motion, KT-1000, pivot-shift)
At ten-year follow-up a flexion deficit of more than 10° compared to the uninvolved contralateral side was observed in one patient. None showed a lag of extension.
The Lachman test was negative (grade 0) in 32 patients (80 %), seven patients (17 %) had a grade 1 test results and one (3 %) had a grade 2 test result. On pivot shift testing 36 patients (90 %) had a grade 0 test result, four patients (10 %) had a glide, none a had a grade 2 test result.
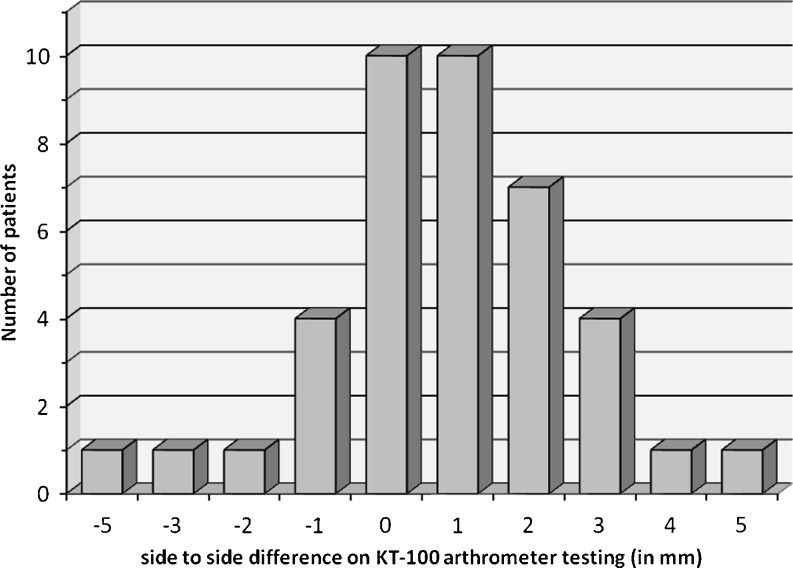
Instrumental laxity testing showed a mean KT-1000 (134 N) side-to-side difference of 0.78 ± 1.85 mm (range, −5 to +5 mm). Thirty-one patients (78 %) demonstrated an anterior laxity difference of less than 3 mm. Six patients (15 %) showed a difference between 3 and 5 mm. Three operated (7 %) knees showed a negative anterior laxity of more than 1 mm compared to the uninvolved contralateral knee (Fig. 2).
Fig. 2.
Instrumental side-to-side laxity (KT-1000; 134N; 20°)
Self-reported data (Tegner activity score, IKDC, Lysholm score)
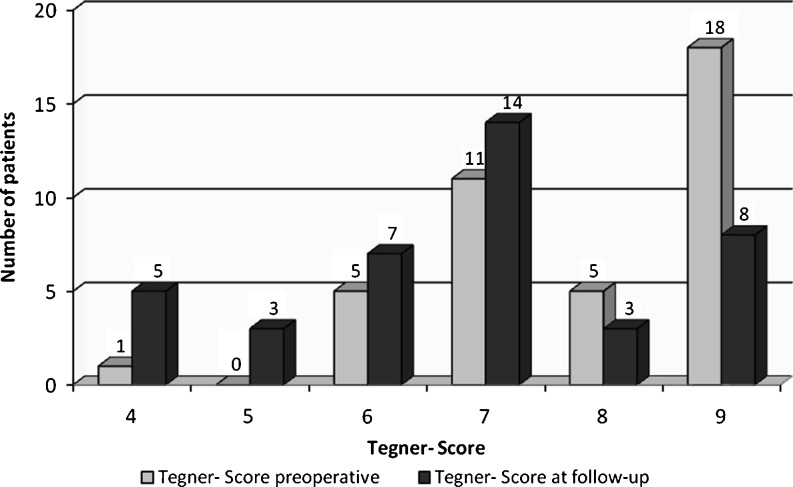
The evaluation of the Tegner activity score showed a significant decrease from 8 points (median, range 4–9) preoperatively to 7 points (median, range 4–9) postoperatively. 22 patients (55 %) were able to return to their preoperative activity level, while 18 patients (45 %) decreased their activity (Fig. 3).
Fig. 3.
Evaluation of the Tegner activity score
At ten-year follow-up the mean IKDC evaluation score revealed 90.3 ± 8.6 points. Eight patients (20 %) had a score of 100 points. The full IKDC assessment showed that 29 knees (72.5 %) had a normal overall IKDC grade (A). The remaining 11 patients (27.5 %) were graded as “nearly normal” (B). No joint was “abnormal” or “severely abnormal” (grade C or D).
The mean Lysholm score was 93.2 ± 7.8 (range 66–100) at follow-up. Twenty-eight patients (70 %) were rated as very good (91–100 points), nine (23 %) as good (84–90 points) and three patients (7 %) as fair (65 to 83 points). None was assessed as poor (<65 points).
While there was no correlation between the functional clinical scores (IKDC, respectively, Lysholm score) and the anteriorposterior translation measured by the KT-1000 arthrometer we found a significant relationship between the pivot shift and the clinical assessment scores. Patients having a negative pivot shift demonstrated significantly better results in the IKDC subjective and Lysholm scores than patients having a rotational instability in the pivot shift test (p < 0.001).
According to the numeric rating scale (NRS) the satisfaction with the operative result was 9 (median, range 4–10). Thirty-four patients (85 %) were very satisfied (NRS, 8–10) and six patients (15 %) were satisfied (NRS, 4–7) with the result of the operation. None was dissatisfied (NRS, 0–3).
Further surgical interventions
There were no intra- or postoperative complications during the inpatient period. Five patients (13 %) had revision surgery during follow-up period. Three patients had a medial menisectomy, two patients had removal of the suture disc due to local mechanical irritation.
As described above there were eight re-ruptures (8 %) of the initially reconstructed ACL grafts (n = 101) due to adequate trauma. One re-rupture occurred during the first year postoperative and two at two years of follow-up. Six of the eight patients had revision reconstruction with patellar autograft during follow-up period.
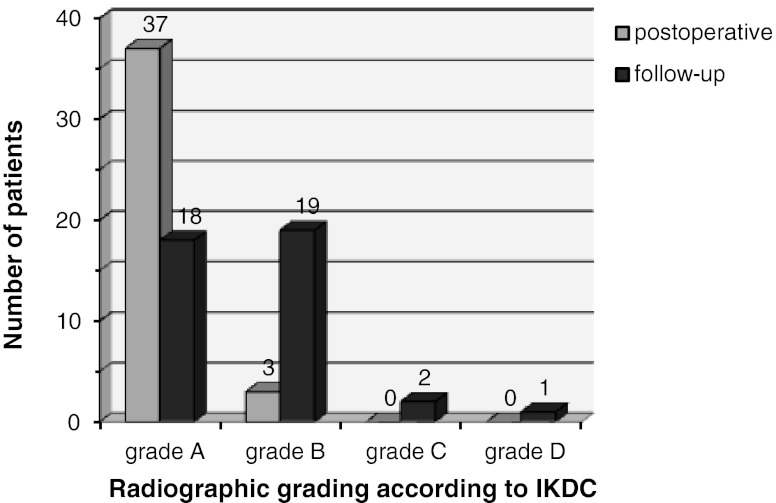
Radiological examination
According to the IKDC guidelines there was a significant aggravation in the radiographic grading over time. As shown in Fig. 4, 20 (50 %) altered the radiological OA grade during follow-up. To assess the relative contributions of age, BMI, gender, functional outcome, time from injury to index operation, initial or secondary meniscal surgery, KT-1000 and pivot shift a statistical analysis was performed. While no correlation was found for age, gender, time from injury to initial surgery, primary and subsequent meniscal surgery, functional outcome or the KT-1000 arthrometer, there was a significant relationship between a positive pivot shift at follow-up and the radiographic grading of OA. Furthermore. poorer radiographic grading was associated with a higher BMI.
Fig. 4.
Radiographic grading according to IKDC guidelines
At follow-up, radiographic evaluation showed a tunnel widening in 32 patients (80 %). Even if there was a significant increase in the mean of the tunnel diameter (p = 0.000), patients with femoral or tibial tunnel widening showed no worse outcomes, neither concerning functional (Lysholm, IKDC KT-1000) nor radiological status.
Discussion
This retrospective case study was able to demonstrate excellent clinical and subjective results for patients undergoing ACL reconstruction with an autologous four-stranded semitendinosus tendon after a ten-year follow-up. The surgical technique applied in this clinical investigation used the quadrupled semitendinosus tendon, which is larger in diameter and provides a stronger graft compared with combined semitendinosus/gracilis (STG) transplants and even patellar tendon [8]. Furthermore compared to a STG graft the gracilis tendon as an important flexor muscle can be saved.
Many authors report only single or double hamstring techniques [8, 9], others provide results with combined semitendinosus and gracilis transplants [10, 11] or report outcomes for patients with shorter follow-up time [4, 12]. Mid- or even long-term results of ACL reconstruction with quadrupled semitendinosus tendon alone are very rare [16]. This study reports minimum ten-year follow-up results after a standardised arthroscopic ACL reconstruction, which is—as far as the authors are aware—one of the longest follow-up periods in the literature evaluating this special technique.
Comparing our results for the stability at the KT-1000 to those in the literature our patients had lower side-to side differences than similar studies [13]. Even though the technique applied in our investigation is similar to others evaluating ACL reconstruction [16], we can only speculate on possible explanations for the confounding parameters. Maybe positioning the femoral tunnel in a more horizontal way influences the stability, even in the sagittal plane [14]. Nor can we quote any correlation between the side-to-side difference and the measured clinical parameters as the Lysholm or the IKDC scores. Furthermore no relationship could be found with the activity score according to Tegner. We speculate that in patients having a stable knee the amount of sagittal translation has no influence on their daily activity or their physical performance. Even if we reconstructed the ACL with an ST graft alone the patients obtained at least the same level in the clinical outcome scores compared to studies with a similar follow-up time using an STG graft [15, 16]. This is in line with the review by Samuelsson et al. [17]. They could not quote any differences between the selected graft and the self reported data including the Lysholm score.
Another important finding of our investigation was the influence of rotational stability on the incidence of osteoarthritis and the functional subjective outcome. Patients having a negative pivot shift test showed significantly less signs of radiographic osteoarthritis and better functional assessment scores independent of reconstruction. This is in line with the results published by Jonsson et al. [18] and others [19] who suggested a positive pivot shift test as a predictor of later osteoarthritis based on the results of long-term radiographic evaluations. Also Kocher et al. reported a significant relationship between the pivot shift test grades and patient satisfaction, whereas anterior posterior laxity did not influence the patient subjective assessment two years postoperatively [20]. In view of these observations it seems to be clear that one of the main targets of any outcome evaluation of ACL treatment should be the precise documentation of transverse plane rotatory stability.
The radiographic evaluation showed no or only mild evidence of osteoarthritis in 92 % of our patients and 50 % of the patients deteriorated during follow-up. This rate and degree of arthritic change after ACL reconstruction compares favourably with other studies treating ACL-deficient knees. Shelbourne et al. [21] reported 97 % normal or near- normal radiographs in ACL-reconstructed patients five to 15 years after reconstruction, provided both menisci were intact and articular surfaces were normal at the time of surgery.
As bone tunnel widening seems to be significantly associated with hamstring autografts and especially with extracortical fixation techniques such as endobutton fixation compared with other fixation techniques including transfix and interference screw fixation, we specifically focussed on that. Our results confirm the outcomes reported in the literature after shorter periods of follow-up [22, 23]. In 80 % of the patients even after ten years a tunnel widening of more than 50 % could be detected compared to the status of the postoperative radiograph. Patients with tunnel widening did not show worse functional or stability results which confirms the results in the literature [22, 24]. Obviously, bone tunnel widening seems to be associated with this kind of fixation technique, but has no impact even on the longer-term clinical outcome after ACL reconstruction.
As there are several studies reporting on limitations in the range of motion following ACL reconstruction with HT autografts we were unable to detect that in our collective. Only one patient (2.5 %) had a deficit in knee flexion of 10°. In the study published by Liden et al. 35 % of their investigated 36 patients had a limitation of flexion seven years after reconstruction with a combined STG graft [25]. In contrast Keays et al. [10] could only quote a flexion deficit in 3 % of their cases. Our graft failure rate with 7 % is within the level reported in the literature ranging from 0 % to 10 % with quadrupled hamstring techniques [9, 11, 22].
Some limitations of our study need to be addressed. A challenge when performing long-term follow-up studies is the number of patients lost to follow-up or dropouts. The number of 40 patients and a follow-up rate of over 75 % allow a representative outcome evaluation. Even when assuming a worst case scenario and a complete failure of all patients (22 %) who were lost of follow-up, the outcomes obtained hereby are still convincing and confirm the results reported in the literature after shorter periods of follow-up. Another limitation might be the reliability of the classification of the radiographs, which may be the subject of individual interpretations.
On the basis of our investigation, we conclude that the reconstruction of the ACL by a quadrupled semitendinosus tendon graft with an extracortical anchorage can achieve excellent clinical and subjective results after a follow-up of ten years. Consequently, we believe that it is a safe alternative for the active patient with ACL deficiency.
References
- 1.National Institutes of Health (NIH) (2007) Prognosis and predictors of ACL reconstruction—a multicenter cohort study. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), Vanderbilt University, United States. Available at: http://clinicaltrials.gov/ct2/show/NCT00463099. Accessed March 1, 2011
- 2.Prodromos CC, Han YS, Keller BL, Bolyard RJ. Stability results of hamstring anterior cruciate ligament reconstruction at 2- to 8-year follow-up. Arthroscopy. 2005;21(2):138–146. doi: 10.1016/j.arthro.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Hospodar SJ, Miller MD. Controversies in ACL reconstruction: bone-patellar tendon-bone anterior cruciate ligament reconstruction remains the gold standard. Sports Med Arthrosc. 2009;17(4):242–246. doi: 10.1097/JSA.0b013e3181c14841. [DOI] [PubMed] [Google Scholar]
- 4.Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;7(9):CD005960. doi: 10.1002/14651858.CD005960.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reinhardt KR, Hetsroni I, Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41(2):249–262. doi: 10.1016/j.ocl.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Chen L, Cooley V, Rosenberg T. ACL reconstruction with hamstring tendon. Orthop Clin North Am. 2003;34:9–18. doi: 10.1016/S0030-5898(02)00016-0. [DOI] [PubMed] [Google Scholar]
- 7.LaValley MP, McAlindon TE, Chaisson CE, Levy D, Felson DT. The validity of different definitions of radiographic worsening for longitudinal studies of knee osteoarthritis. J Clin Epidemiol. 2001;54(1):30–39. doi: 10.1016/S0895-4356(00)00273-0. [DOI] [PubMed] [Google Scholar]
- 8.Beynnon BD, Johnson RJ, Fleming BC, Pekka K, Kaplan M, Samni J, et al. Anterior cruciate ligament replacement: comparison of bone- patellar tendon-bone grafts with two-strand hamstring grafts. J Bone Joint Surg Am. 2002;84A:1503–1513. doi: 10.2106/00004623-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson K, Anderberg P, Hamberg P, Löfgren AC, Brendenberg M, Westman I, et al. A comparison of quadrupled semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001;83:348–354. doi: 10.1302/0301-620X.83B3.11685. [DOI] [PubMed] [Google Scholar]
- 10.Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med. 2007;35(5):729–739. doi: 10.1177/0363546506298277. [DOI] [PubMed] [Google Scholar]
- 11.Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34(12):1933–1940. doi: 10.1177/0363546506290726. [DOI] [PubMed] [Google Scholar]
- 12.Gobbi A, Domzalski M, Pascual J, Zanazzo M. Hamstring anterior cruciate ligament reconstruction: is it necessary to sacrifice the gracilis? Arthroscopy. 2005;21:275–280. doi: 10.1016/j.arthro.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009;37(4):707–714. doi: 10.1177/0363546508328114. [DOI] [PubMed] [Google Scholar]
- 14.Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o’clock and 10 o’clock femoral tunnel placement. 2002 Richard O’Connor Award paper. Arthroscopy. 2003;19:297–304. doi: 10.1053/jars.2003.50084. [DOI] [PubMed] [Google Scholar]
- 15.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 16.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon–bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38(3):448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 17.Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25:1139–1174. doi: 10.1016/j.arthro.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 18.Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand. 2004;75(5):594–599. doi: 10.1080/00016470410001484. [DOI] [PubMed] [Google Scholar]
- 19.Streich NA, Zimmermann D, Bode G, Schmitt H. Reconstructive versus non-reconstructive treatment of anterior cruciate ligament insufficiency. A retrospective matched-pair long-term follow-up. Intern Orthop. 2011;35:607–613. doi: 10.1007/s00264-010-1174-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 21.Shelbourne K, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28(4):446–452. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 22.Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 23.Buelow JU, Siebold R, Ellermann A. A prospective evaluation of tunnel enlargement in anterior cruciate ligament reconstruction with hamstrings: extracortical versus anatomical fixation. Knee Surg Sports Traumatol Arthrosc. 2002;10:80–85. doi: 10.1007/s00167-001-0267-6. [DOI] [PubMed] [Google Scholar]
- 24.Clatworthy MG, Annear P, Bulow JU, Bartlett RJ. Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc. 1999;7:138–145. doi: 10.1007/s001670050138. [DOI] [PubMed] [Google Scholar]
- 25.Lidén M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35(5):740–748. doi: 10.1177/0363546506298275. [DOI] [PubMed] [Google Scholar]