Abstract
Over recent years, double-bundle reconstruction has gained popularity after studies showed significant advantages of adding a second bundle with regard to outcomes and biomechanics; in particular, it resulted in less rotational instability than after reconstruction with a traditional single-bundle technique. As the focus shifted further towards the restoration of the native anatomy, both single-bundle and double-bundle ACL reconstruction were performed in an anatomical fashion and yielded similar results. To date, no consensus has developed as to whether double-bundle reconstruction is better than single-bundle reconstruction or vice versa. However, after surgeons started to individualise their surgical approach to the patient, it has been found that both the anatomical single- and double-bundle techniques have their own set of indications and contraindications. Reconstruction of the ligament should focus on restoration of the native functional and anatomical properties and should take the size, shape and orientation of the ACL into account. When indications and contraindications for the technique used are based on native anatomical characteristics, either a single-bundle or a double-bundle procedure can be performed according to the same double-bundle concept.
Introduction
Rupture of the anterior cruciate ligament (ACL) is one of the most common ligamentous injuries of the knee, with an incidence of 35 out of 100,000 and a two to three times higher risk of injury for females [1]. When left untreated, it can result in recurrent instability, and an inability to return to cutting and pivoting activities. Additionally, the ACL deficient knee is at risk for meniscal injuries and the early onset of degenerative changes of the articular cartilage [2, 3]. The ACL does not have the potential to adequately heal when torn, therefore surgical ACL reconstruction is generally the treatment of choice with the goal of stabilising the knee to minimise the risk of re-injury, allowing for a safe return to sport and—most importantly—avoiding early degenerative changes.
Anatomical ACL reconstruction has been shown to provide improved knee stability when compared to conventional techniques [4]. The definition of anatomical ACL reconstruction is the functional restoration of the ACL to its native dimensions, collagen orientation, and insertion sites [5]. When performing an anatomical ACL reconstruction, it is critical to reproduce the patient’s unique anatomy by reconstructing the insertion site size, orientation, and tensioning patterns of each individual bundle. A bundle specific ACL reconstruction can always be performed whether it is a single-bundle, double-bundle or augmentation procedure [6]. Therefore, each technique has its own indications and contraindications and surgeons should master all techniques depending on the injury pattern and anatomical characteristics of the individual patient. Since each technique can be applied to restore the native double-bundle anatomy, “double-bundle ACL reconstruction” should be regarded as a concept rather than a surgical technique. The goal of each bundle-specific technique should be to restore the patient’s individual anatomy and thereby both functional bundles of the native ligament that serve the knee’s bony morphology. When anatomical ACL reconstruction is customized to the size, shape and orientation of the native ACL of each individual patient, single-bundle and double-bundle reconstruction yield similar subjective and objective clinical outcome measures [7].
The double-bundle concept
Two distinct functional bundles have been identified in the native ACL: the anteromedial (AM) and posterolateral (PL) bundle. These bundles are named for their relative anatomical insertion on the tibia [8–12]. Both bundles are distinguishable and separated by a vascularised septum during early foetal development (already around 20 weeks) [13], suggesting that both bundles are literally a part of native anatomy (Fig. 1).
Fig. 1.
The native anterior cruciate ligament (ACL) consists of two functionally separate bundles: the anteromedial (AM) bundle (solid line) and posterolateral (PL) bundle (dashed line)
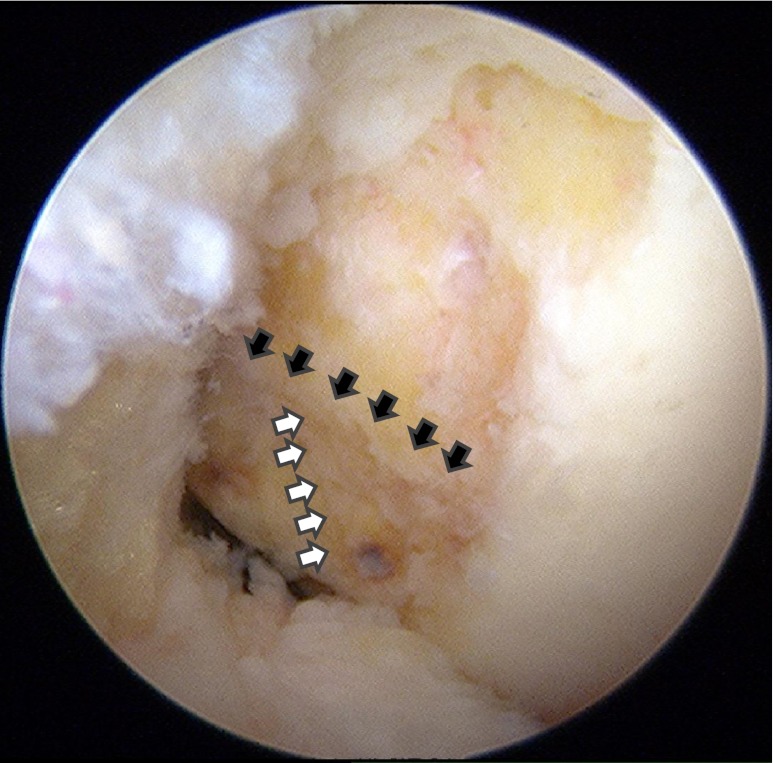
The tibial AM bundle insertion site is aligned with the anterior horn of the lateral meniscus and has a close relationship with the medial and lateral tibial spine. The tibial PL insertion is in the respective posterolateral position to the AM bundle [14]. The AM bundle originates from the proximal portion of the medial wall of the lateral femoral condyle, while the PL bundle lies more distally, near the weight bearing articular cartilage surface [15, 16]. Both bundles insert posterior to the intercondylar ridge. On the femoral side, the most prominent anatomical osseous landmark is the intercondylar ridge which is the anterior border of the femoral insertion site. In 80 % of all cases, a second ridge, the bifurcate ridge, can also be identified. This ridge separates the origins of the AM and PL bundle and runs perpendicular to the intercondylar ridge [17, 18] (Fig. 2).
Fig. 2.
Osseous landmarks on the medial wall of the lateral femoral condyle can be used to identify the insertion sites of the anteromedial (AM) and posterolateral (PL) bundles. The lateral intercondylar ridge (black arrows) is the most anterior border of the anterior cruciate ligament (ACL) insertion site. The bifurcate ridge (white arrows) runs perpendicular to the intercondylar ridge and separates the AM from the PL insertion site
The distinction between the two bundles is not solely made based on anatomy. AM and PL bundles have a synergistic but different function throughout the entire range of motion (ROM) of the knee. In a fully extended knee, both AM and PL are taut, with PL is at its maximum. PL limits rotation of the tibia on the femur up to 60–90° of knee flexion, after which PL loosens [19]. Although AM primarily resists anterior translation of the tibia, at low flexion angles (0–30°) the PL also contributes. The AM bundle is under maximum tension when the knee is flexed between 45° and 60° [20] (Fig. 3).
Fig. 3.
In a fully extended knee (a), both anteromedial (AM) (solid line) and posterolateral (PL) (dashed line) bundles are taut. In flexion (b) however, the PL (dashed line) loosens to allow rotation
The goal of anatomical ACL reconstruction is to restore the native ACL anatomy as closely as possible and consequently to approximate normal knee biomechanics. Four fundamental principles should be observed to achieve this goal. The first is to carefully observe and objectify the patient’s native anatomy. The second is to individualise each surgery with respect to the patient’s anatomy. The third is to place the tunnels, and grafts in the centre of the patient’s native footprints. The fourth is to re-establish knee biomechanics by tensioning the grafts to mimic the functional properties of the native ACL as closely as possible [5].
The double-bundle concept is founded on the distinct anatomical and functional differences between the AM and PL bundle that comprise the ACL. A clear understanding of this concept is vital to mastering and applying anatomical ACL reconstruction in a customised manner to each individual patient’s anatomy and injury pattern.
Preoperative assessment
The first and foremost step towards diagnosing an ACL tear is to obtain a complete history and physical examination. Not only will this help to diagnose the presence of a tear, but also in differentiating between partial and complete tears [21].
The mechanism of injury may help to distinguish which bundle has ruptured as the AM bundle is frequently torn with high-energy trauma, while the PL bundle may be torn with more subtle, rotational mechanisms [21]. Insufficiency of the AM bundle usually results in antero-posterior instability similar to a complete rupture, while insufficiency of the PL bundle may result in instability with pivoting or turning. During physical examination this may become evident, i.e., the presence of a positive pivot shift with an intact end point on Lachman test suggests a PL bundle injury, while isolated injuries to the AM bundle will show increased anterior translation without a firm end point on Lachman test and a negative pivot-shift examination [14].
Conventional radiographic evaluation of both the injured and un-injured knee is fundamental in the initial assessment for degenerative changes, physeal status, leg alignment, associated fractures or avulsions and possible deformities.
High quality magnetic resonance imaging (MRI) plays a critical role in diagnostics and pre-operative planning [22]. MRI can confirm the diagnosis of an ACL injury [23] and—more importantly—it also allows the surgeon to examine the rupture pattern [24, 25], measure the native ACL insertion site dimensions, inclination angles and thickness of the quadriceps and patellar tendon as potential grafts, evaluate for additional ligamentous or bony injuries, and evaluate meniscus and cartilage status [26] (Fig. 4).
Fig. 4.
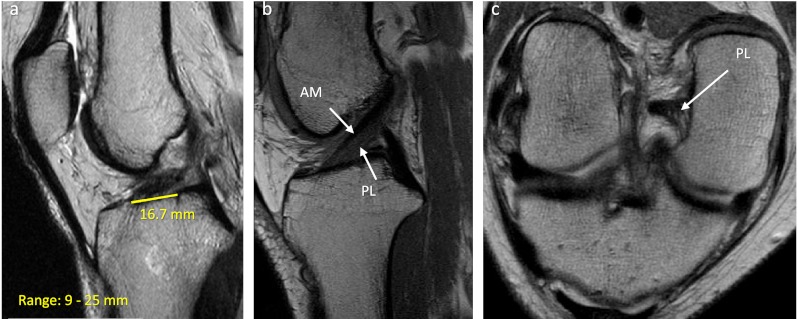
Both for diagnostic purposes and pre-surgical planning, a complete evaluation with MRI is invaluable. Regular coronal, axial and sagittal cuts should be obtained to confirm the diagnosis and look for concomitant injuries. Additionally, on the regular sagittal cuts, measurements of the insertion site length (a), inclination angle, total anterior cruciate ligament (ACL) length and quadriceps and patellar tendon thickness can be obtained. For a more precise evaluation, oblique sagittal and coronal cuts can be obtained by scanning in the same plane as the trajectory of the entire ACL. These images are particularly helpful in identifying the individual bundles (b) and potential partial bundle tears (c)
However, even with clinical and radiological assessment, the exact injury pattern of an ACL tear and individual anatomy can only be definitively established arthroscopically. Consequently, the ultimate decision to perform a single-bundle or a double-bundle ACL reconstruction can only be made intraoperatively.
Surgery
Following induction of general anaesthesia a complete knee examination is repeated to assess the ligamentous function without the patient potentially muscle guarding. Specifically, pivot-shift test results may differ significantly from what is found during office examination [27].
Three portal technique
A three-portal approach has been shown to provide the best visualisation of the native insertion sites, which is of the utmost importance for anatomical ACL reconstruction [28, 29] (Fig. 5). A “high” anterolateral portal (LP) is positioned above Hoffa’s fat pad, thus minimising the need to traverse the fat pad and allowing for evaluation of the tibial insertion site of the ACL. The central portal (CP) and medial portal (MP) are then created under direct vision through the LP using a spinal needle. The final position of the CP and MP varies as the orientation of the intercondylar notch may vary. Through the CP, the spinal needle should be in the central portion of the notch in the coronal plane and in the lower third of the notch in the proximal to distal direction. The MP is ideally located superior to the medial joint line approximately two centimetres medial to the medial border of the patellar tendon. In establishing the MP, careful attention should be taken to avoid iatrogenic damage to the cartilage of the medial femoral condyle [28, 29].
Fig. 5.
A three portal technique provides the best visualisation of and access to the anterior cruciate ligament (ACL) insertion sites. First, a high LP is created, then—under arthroscopic visualisation of a spinal needle—the central portal (CP) and medial portal (MP) are created
Indications and contraindications
Diagnostic arthroscopy is performed first to assess for concomitant injuries and to confirm the ACL‘s rupture pattern by cautious evaluation of the ACL remnant. A single-bundle tear is an indication for a bundle augmentation technique, provided that the intact bundle is fully functional.
If both bundles are torn, the remnants are then carefully dissected with the use of a shaver and thermal device to mark the native insertion sites of both the AM and PL bundle.
Intra-operative measurements are then obtained with an arthroscopic bendable ruler (Smith & Nephew Endoscopy, Andover, MA) to assess the size of both the tibial and femoral native insertion sites (Fig. 6). Although the indication for either single-bundle or double-bundle reconstruction is primarily dependent on this measurement, surrounding anatomical properties should also be taken into account. To this end, the notch size is measured and documented. Specific measurements that are obtained include the insertion site lengths, AM and PL bundle widths as well as notch height and width.
Fig. 6.
Intra-operative measurements are taken to make an objective assessment of the individual anatomy. Tibial insertion site length (a) and width (b) provide information on the native anterior cruciate ligament (ACL) size and primarily dictate the surgical technique used for reconstruction. Notch height (c) and width (d) measurements provide information as to how much room there is for the surgery to be performed without iatrogenic damage and for the eventual graft(s) to function without impingement. These measurements are the final step in the decision-making process regarding what reconstructive technique to apply
Based on the insertion site measurements, a total tibial insertion site length of less than 14 mm is an indication for single-bundle reconstruction [30]. A single graft will usually be sufficient to restore 60–80 % of the size of the native ACL, while a double graft would probably exceed the size of the insertion site. Provided that the graft is positioned anatomically on both the tibia and femur (“PL to PL” and “AM to AM”), this single-bundle graft will acquire the functional properties of the native double-bundle ligament.
Relative contraindications for a double-bundle ACL reconstruction include open physes, severe bone bruising, a narrow notch (<14 mm), a shallow notch (<14 mm), severe arthritic changes (grade 3 or greater), or multiligamentous injuries [31]. Open physes and severe bone bruising are conditions that probably benefit from less iatrogenic damage by less tunnel drilling, and severe arthritic changes may worsen more rapidly by constraining the knee with two bundles. A small notch, whether it be shallow or narrow, does not easily accommodate a double-bundle ACL reconstruction as a narrow notch poses a technical challenge for placing both femoral tunnels anatomically and a shallow notch may cause early failure due to potential graft impingement.
Techniques
Bundle augmentation
In cases of a partial ACL rupture, bundle augmentation may be appropriate. Meticulous care should be given to preserve the remaining intact bundle while dissecting the compromised ACL’s anatomy using a thermal device. The centre of the femoral insertion for the ruptured bundle is identified, and the centre of the planned tunnel is marked with an angled awl. In cases of single-bundle augmentation drilling with a flexible reamer may be desirable as a more spherical aperture is produced and may not compromise the remaining intact ACL bundle. The distance to the lateral cortex is determined and the tunnel size is increased to the desired dimensions. A tibial guide is centred within the tibial insertion of the ruptured bundle. The tibial tunnel is reamed and dilated to the desired dimensions. Graft passage is visualised arthroscopically to assure anatomical positioning, and position of suspensory fixation is confirmed with fluoroscopy. The graft is finally tensioned and fixed as dictated by the reconstructed bundle.
Anatomical single-bundle ACL reconstruction
As mentioned, if applied for the correct indication and according to the double-bundle concept, a single-bundle ACL reconstruction restores the functional double-bundle anatomy of the native ligament.
A single femoral tunnel is positioned midway between the centre of the AM and PL insertion sites. The distance to the lateral cortex is determined and the femoral tunnel is reamed and dilated to the desired size. The tibial insertion site is then carefully dissected to identify both the AM and PL bundles. The desired position of a single tibial tunnel is midway between the centres of the AM and PL bundles. A tip-to-tip guide is placed in the desired position and a guide pin is passed retrograde through a longitudinal incision over the anteromedial proximal tibia. The tunnel is then reamed and dilated to the desired dimensions. Graft passage is performed using a loop suture and beath pin. The loop suture is passed through the femoral tunnel and retrieved from the tibial tunnel. The graft is then passed retrograde through the tibial tunnel until seated appropriately within the femoral tunnel. The PL section of the graft is marked to allow for appropriate orientation of the graft in both the femoral and tibial tunnel. A suture is placed through the PL section intra-articularly, allowing the surgeon to manoeuvre the graft intra-articularly to its ideal position. The graft is oriented to allow for this section to be located in the PL position on the femoral and tibial sides. By anatomically positioning the fibres within the femoral and tibial insertions, a single-bundle reconstruction can be performed while applying the double-bundle concept. The position of suspensory fixation is confirmed using fluoroscopy. The graft is then tensioned and fixed in 15–20° of flexion.
Anatomical double-bundle ACL reconstruction with soft tissue grafts
Anatomical double-bundle ACL reconstruction can be performed using either soft tissue grafts or grafts with an additional bone block. In case of soft tissue double-bundle reconstruction, separate AM and PL tunnels are drilled at the native femoral and tibial insertion sites. A thermal device is used to identify both the AM and PL insertions sites. These soft tissue remnants, along with bony landmarks such as the lateral intercondylar ridge and the bifurcate ridge are useful for identifying the individual bundle insertions. The femoral PL tunnel should be created first in the centre of the PL insertion site with a Steadman awl, and then a guide wire is advanced through the lateral cortex. Traditionally, rigid guide-wires and reamers are used to place and drill the tunnels; however, this instrumentation often requires knee hyperflexion in order to avoid iatrogenic damage to nearby structures. Often, flexible reamers may be desired as these devices do not require knee hyperflexion. Moreover, they decrease the susceptibility for posterior cortical violation by altering the drill exit point and an increase in tunnel length [32].
Attention is then turned to the tibial side before drilling the femoral AM tunnel. Depending on individual anatomy and surgical preference, the femoral AM tunnel may be drilled with a transtibial or medial portal technique. Rarely can the tibial AM tunnel be used (∼10 % of cases); but frequently, the tibial PL tunnel can be used (∼50 %), and nearly always, the MP can be used (>95 %). The tibial insertion site is carefully dissected measured in a similar manner to the femoral anatomy. A vertical incision of 3–4 cm is made along the proximal antero-medial aspect of the leg. The planned tibial tunnels are placed in the centre of the AM and PL bundles. A tibial tip-to-tip guide is set to 45° and placed in the centre of the PL bundle, and a guide-wire is then advanced. Another guide-wire is similarly advanced to the centre of the AM insertion with the tip guide now set to 55°. To assure an adequate bone bridge between the tunnels, the tunnel entrance should be 2 cm apart on the tibial extra-articular cortex. To assure that no notch impingement is presented, the knee is then brought into full extension. The relationship between the K-wire and the roof of the intercondylar notch should be evaluated with the knee in full extension to avoid notch impingement of the ACL graft.
Prior to passing the grafts, a beath pin is passed through the femoral tunnels and the suture loop is retrieved through the tibia PL and AM tunnels, respectively. To assure appropriate placement of each passing suture, arthroscopic examination is performed. The PL graft is passed through the tibial tunnel and into the femoral tunnel prior to AM graft passage. Correct positioning of suspensory fixation outside the lateral femoral cortex is confirmed prior to graft tensioning. Fixation at full extension for the PL graft and at 45° of flexion for the AM graft is performed.
Double-bundle ACL reconstruction with quadriceps tendon with bone block
When performing a double-bundle-ACL reconstruction using a quadriceps tendon with bone block, a single femoral tunnel is prepared. The femoral tunnel is positioned midway between the AM and PL insertion sites. The distance from the medial wall to the lateral cortex and the desired tunnel dimensions are then determined. The femoral tunnel is reamed to a depth of at least 20 mm and dilated to allow for graft passage while maintaining the tightest possible fit. The tibial tunnels are created as previously described. The quadriceps bone block is passed through the MP into the femoral tunnel. Once the block is appropriately placed within the femoral tunnel, confirmation of suspensory fixation outside the lateral cortex is obtained with fluoroscopy. It is important with a single femoral tunnel that the PL and AM section of the soft tissue graft are anatomically positioned. Flexible loop wires are passed retrograde through the AM and PL tibial tunnels and retrieved from the CP, while sutures from the AM and PL soft tissue grafts are retrieved out the CP as well. First, the PL graft is passed under arthroscopic visualisation to assure appropriate placement relative to the AM graft. The AM graft is then passed under arthroscopic visualisation. Lastly, the PL graft is tensioned and secured in full extension while the AM graft is fixed in 45° of flexion.
Postoperative care and rehabilitation
Immediately after surgery, the knee is immobilised with a brace. Patients are discharged with adequate pain medication and a cooling device the same day.
All bundle-specific techniques follow the same rehabilitation protocol. During the first week(s), focus should be placed to minimise pain, reduce swelling and restore full ROM and quadriceps muscle strength. The day after surgery patients begin to perform ankle pumps, quadriceps sets, straight leg raise, gastrocnemius and hamstring stretches and heel slides. At the end of the first week, continuous passive motion (CPM) is initiated with full progression to full extension.
Generally crutches and brace are weaned after six weeks, depending on the progress made. Once quadriceps muscle strength resumes, straight line walking can be initiated at six weeks with progression to jogging in a straight line and a stationary bike around three months. Pivoting and cutting exercises are not initiated until at least six months and return to sport is generally no sooner than nine months postoperatively. A functional ACL brace for sports is recommended until the patient is two years from their ACL reconstruction.
Patient progression through the rehabilitation phases is dependent on the patient’s readiness as assessed by the physical therapist and the operating surgeons with performance on rehabilitation tests, clinical findings in the office, and even evaluation on MRI to assess graft healing.
Complications
Both anatomical single-bundle and double-bundle procedures have the same potential general complications including wound infection, haemarthrosis, arthrofibrosis, effusion, neurovascular injury, tunnel widening, tibial or femoral fractures and DVT. The double-bundle technique is technically more complex and may therefore be more prone to complications in inexperienced hands. For this reason, the double-bundle concept should be first solidified in a single-bundle approach before attempting a double-bundle reconstruction.
Discussion
The traditional single-bundle ACL reconstruction technique has several advantages associated with its application for treatment of ACL tears as it is simple, quick and does not require the knee to be flexed beyond 90°. However, while outcomes were suboptimal and the understanding of the anatomy and kinematics of the native ACL expanded, new recommendations developed with keen regard to anatomical placement of bone tunnels. When studies did confirm nearly normal knee joint kinematics when the bone tunnels were placed in the centre of the native ACL insertion site [33–37], emphasis shifted further towards the restoration of anatomy. This increased understanding of the anatomy also resulted in the recognition and attempted restoration of the double-bundle anatomy of the ACL, by adding a second bundle graft. Multiple studies have shown equivalent or superior knee stability after double-bundle ACL reconstruction, when compared with single-bundle ACL reconstruction [33, 38–43]. However, when placed anatomically and customised to the patient’s individual anatomy, there does not seem to be a difference between a single-bundle and a double-bundle technique [4, 7]. Rather than just adding a second bundle, restoration of normal anatomy is required to restore normal function of the knee.
In summary, ACL surgery should be performed according to the double-bundle concept. This concept relies on the functional anatomy of the ACL, which dictates the surgical procedure by accounting for size, shape, tensioning patterns and orientation of the native ligament. A surgeon should master a variety of diagnostics, objective measurements and surgical techniques to be able to customise the treatment to the patient’s specific needs.
Contributor Information
Bart Muller, Email: bart.muller@live.nl.
Marcus Hofbauer, Email: marcus.hofbauer@meduniwien.ac.at.
Jidapa Wongcharoenwatana, Email: amorithe@hotmail.com.
Freddie H. Fu, Phone: +1-412-6053265, FAX: +1-412-6870802, Email: ffu@upmc.edu
References
- 1.Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6):622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Maletius W, Messner K. Eighteen- to twenty-four-year follow-up after complete rupture of the anterior cruciate ligament. Am J Sports Med. 1999;27(6):711–717. doi: 10.1177/03635465990270060501. [DOI] [PubMed] [Google Scholar]
- 3.Heijink A, Gomoll AH, Madry H, Drobnič M, Filardo G, Espregueira-Mendes J, et al. Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):423–435. doi: 10.1007/s00167-011-1818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40(3):512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 5.van Eck CF, Schreiber VM, Liu TT, Fu FH. The anatomic approach to primary, revision and augmentation anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1154–1163. doi: 10.1007/s00167-010-1191-4. [DOI] [PubMed] [Google Scholar]
- 6.van Eck CF, Lesniak BP, Schreiber VM, Fu FH. Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy. 2010;26(2):258–268. doi: 10.1016/j.arthro.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 7.Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Individualized anterior cruciate ligament surgery: a prospective study comparing anatomic single- and double-bundle reconstruction. Am J Sports Med. 2012;40(8):1781–1788. doi: 10.1177/0363546512446928. [DOI] [PubMed] [Google Scholar]
- 8.Palmer I. On the injuries to the ligaments of the knee joint: a clinical study. 1938. Clin Orthop Relat Res. 2007;454:17–22. doi: 10.1097/BLO.0b013e31802c7915. [DOI] [PubMed] [Google Scholar]
- 9.Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73(2):260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 10.Arnoczky SP. Anatomy of the anterior cruciate ligament. Clin Orthop Relat Res. 1983;172:19–25. [PubMed] [Google Scholar]
- 11.Odensten M, Gillquist J. Functional anatomy of the anterior cruciate ligament and a rationale for reconstruction. J Bone Joint Surg Am. 1985;67(2):257–262. [PubMed] [Google Scholar]
- 12.Girgis FG, Marshall JL, Monajem A (1975) The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res (106):216–231 [DOI] [PubMed]
- 13.Ferretti M, Ekdahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23(11):1218–1225. doi: 10.1016/j.arthro.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 14.van Eck CF, Lesniak BP, Schreiber VM, Fu FH. Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy. 2010;26(2):258–268. doi: 10.1016/j.arthro.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 15.Harner CD, Baek GH, Vogrin TM, Carlin GJ, Kashiwaguchi S, Woo SL. Quantitative analysis of human cruciate ligament insertions. Arthroscopy. 1999;15(7):741–749. doi: 10.1016/S0749-8063(99)70006-X. [DOI] [PubMed] [Google Scholar]
- 16.Mochizuki T, Muneta T, Nagase T, Shirasawa S-I, Akita K-I, Sekiya I. Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(4):356–361. doi: 10.1016/j.arthro.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 17.Ferretti M, Ekdahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23(11):1218–1225. doi: 10.1016/j.arthro.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Purnell ML, Larson AI, Clancy W. Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med. 2008;36(11):2083–2090. doi: 10.1177/0363546508319896. [DOI] [PubMed] [Google Scholar]
- 19.Gabriel MT, Wong EK, Woo SL-Y, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22(1):85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 20.Chhabra A, Starman JS, Ferretti M, Vidal AF, Zantop T, Fu FH. Anatomic, radiographic, biomechanical, and kinematic evaluation of the anterior cruciate ligament and its two functional bundles. J Bone Joint Surg Am. 2006;88(Suppl 4):2–10. doi: 10.2106/JBJS.F.00616. [DOI] [PubMed] [Google Scholar]
- 21.Zantop T, Brucker PU, Vidal A, Zelle BA, Fu FH. Intraarticular rupture pattern of the ACL. Clin Orthop Relat Res. 2007;454:48–53. doi: 10.1097/BLO.0b013e31802ca45b. [DOI] [PubMed] [Google Scholar]
- 22.Araujo P, van Eck CF, Torabi M, Fu FH (2012) How to optimize the use of MRI in anatomic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. Aug 15 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 23.Steckel H, Vadala G, Davis D, Fu FH. 2D and 3D 3-tesla magnetic resonance imaging of the double bundle structure in anterior cruciate ligament anatomy. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1151–1158. doi: 10.1007/s00167-006-0185-8. [DOI] [PubMed] [Google Scholar]
- 24.Siebold R, Fu FH. Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy. 2008;24(11):1289–1298. doi: 10.1016/j.arthro.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 25.Steckel H, Vadala G, Davis D, Musahl V, Fu FH. 3-T MR imaging of partial ACL tears: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1066–1071. doi: 10.1007/s00167-007-0337-5. [DOI] [PubMed] [Google Scholar]
- 26.Illingworth KD, Hensler D, Working ZM, Macalena JA, Tashman S, Fu FH. A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am J Sports Med. 2011;39(12):2611–2618. doi: 10.1177/0363546511420128. [DOI] [PubMed] [Google Scholar]
- 27.Karlsson J, Irrgang JJ, van Eck CF, Samuelsson K, Mejia HA, Fu FH. Anatomic single- and double-bundle anterior cruciate ligament reconstruction, part 2: clinical application of surgical technique. Am J Sports Med. 2011;39(9):2016–2026. doi: 10.1177/0363546511402660. [DOI] [PubMed] [Google Scholar]
- 28.Araujo PH, van Eck CF, Macalena JA, Fu FH. Advances in the three-portal technique for anatomical single- or double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1239–1242. doi: 10.1007/s00167-011-1426-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen SB, Fu FH. Three-portal technique for anterior cruciate ligament reconstruction: use of a central medial portal. Arthroscopy. 2007;23(3):325.e1–325.e5. doi: 10.1016/j.arthro.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 30.Pombo MW, Shen W, Fu FH. Anatomic double-bundle anterior cruciate ligament reconstruction: where are we today? Arthroscopy. 2008;24(10):1168–1177. doi: 10.1016/j.arthro.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 31.Shen W, Forsythe B, Ingham SM, Honkamp NJ, Fu FH. Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am. 2008;90(Suppl 4):20–34. doi: 10.2106/JBJS.H.00919. [DOI] [PubMed] [Google Scholar]
- 32.Steiner ME, Smart LR. Flexible instruments outperform rigid instruments to place anatomic anterior cruciate ligament femoral tunnels without hyperflexion. Arthroscopy. 2012;28(6):835–843. doi: 10.1016/j.arthro.2011.11.029. [DOI] [PubMed] [Google Scholar]
- 33.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL-Y. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(5):660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto Y, Hsu W-H, Woo SL-Y, Van Scyoc AH, Takakura Y, Debski RE. Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med. 2004;32(8):1825–1832. doi: 10.1177/0363546504263947. [DOI] [PubMed] [Google Scholar]
- 35.Yasuda K, Tanabe Y, Kondo E, Kitamura N, Tohyama H. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(9 Suppl):S21–S34. doi: 10.1016/j.arthro.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 36.Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SLY. Knee stability and graft function following anterior cruciate ligament reconstruction: Comparison between 11 o’clock and 10 o’clock femoral tunnel placement. 2002 Richard O’Connor Award paper. Arthroscopy. 2003;19(3):297–304. doi: 10.1053/jars.2003.50084. [DOI] [PubMed] [Google Scholar]
- 37.Scopp JM, Jasper LE, Belkoff SM, Moorman CT. The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy. 2004;20(3):294–299. doi: 10.1016/j.arthro.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 38.Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y. Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br. 2004;86(4):515–520. [PubMed] [Google Scholar]
- 39.Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006;22(3):240–251. doi: 10.1016/j.arthro.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 40.Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N. Single-and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res. 2007;454:108–113. doi: 10.1097/BLO.0b013e31802baaf4. [DOI] [PubMed] [Google Scholar]
- 41.Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 42.Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):500–507. doi: 10.1007/s00167-006-0254-z. [DOI] [PubMed] [Google Scholar]
- 43.Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):137–145. doi: 10.1016/j.arthro.2007.11.013. [DOI] [PubMed] [Google Scholar]