Abstract
Purpose
Based on biomechanical cadaver studies, anatomical double-bundle reconstruction of the anterior cruciate ligament (ACL) was introduced to achieve better stability in the knee, particularly in respect of rotatory loads. Previously, the success of ACL reconstruction was believed to be mainly dependent on correct positioning of the graft, irrespective of the number of bundles for which computer-assisted surgery was developed to avoid malpositioning of the tunnel. The aim of this study was to compare rotational and translational stability after computer-navigated standard single-bundle and anatomical double-bundle ACL reconstruction.
Methods
The authors investigated 42 consecutive patients who had undergone the single-bundle or double-bundle ACL reconstruction procedure using autogenous hamstring tendon grafts and ENDOBUTTON fixation in patients who had been followed up for a minimum of 24 months. Post-operative anteroposterior and rotational laxity was measured with the KT3000 and compared between groups.
Results
Both surgical procedures significantly improve rotational and translational stability compared to the preoperative ACL-deficient knee (P<0.05). No significant differences were registered between groups with regard to anteroposterior displacement of the tibia. The International Knee Documentation Committee (IKDC) and Lysholm scores were significantly higher in the double-bundle group. However, the results were excellent in both groups.
Conclusions
The use of computer-assisted ACL reconstruction, which is a highly accurate method of graft placement, could be useful for inexperienced surgeons to avoid malposition. Long-term results of at least five years are needed to determine whether double-bundle ACL reconstruction, which was associated with improved rotational laxity and significantly better IKDC and Lysholm scores compared to the standard single-bundle ACL reconstruction procedure, exerts an influence in terms of avoiding osteoarthritis or meniscus degeneration.
Introduction
The incidence of anterior cruciate ligament (ACL) injuries has significantly increased in recent times, and reconstruction of the ACL is one of the most frequently performed procedures in orthopaedic surgery. Previously, it was assumed that the clinical success of ACL reconstruction depends on correct positioning of the graft tunnel when replacing only one portion of the ACL, the anteromedial (AM) bundle. However, large prospective series and meta-analyses conducted recently have shown that, despite correct tunnel placement, a significant number of patients experience persistent instability in the knee at follow-up especially in respect of rotational stability and also have abnormal International Knee Documentation Committee (IKDC) scores in as many as one fifth of patients who had undergone single-bundle ACL reconstruction [1]. Anatomical studies have shown that the ACL consists of two major functional bundles, namely the AM and the posterolateral (PL) bundle [2]. Several in vivo and in vitro studies have demonstrated the inability of single-bundle ACL reconstruction to restore intact knee rotational stability [3]. Although anatomical double-bundle reconstruction of the ACL is frequently performed at the present time, its superiority over the single-bundle procedure has not yet been proven in clinical studies. Otherwise, recent investigations [4] have shown that an incorrectly positioned tunnel is the main reason for graft failure and persistent joint instability after ACL reconstruction irrespective of the number of reconstructed grafts for which computer-assisted orthopaedic surgery (CAOS) has been introduced to improve the accuracy of tunnel placement. Currently, the computer-navigated single-bundle and double-bundle ACL reconstruction procedures have not yet been compared in respect of rotational/translational laxity and functional outcome. The aim of this study was to perform such a comparison for a minimum clinical follow-up period of two years.
Materials and methods
Computer-navigated (Vector Vision ACL, v.1.0, Brainlab AG, Feldkirchen Germany), single-bundle and double-bundle ACL reconstruction using semitendinosus (ST) and/or gracilis (GT) tendon autografts were compared retrospectively in respect of clinical results, rotational and translational laxity in 42 consecutive patients over a minimum follow-up of 24 months. The navigation system is an image-free, wireless system that does not require preoperative computed tomography. The current version of the navigation system shows the intra-articular position of tibial and femoral tunnels. Of the patients, 20 received single-bundle reconstruction (SB group) and 22 double-bundle reconstruction (DB group). All patients fulfilled the following inclusion criteria: (1) primary ACL reconstruction, (2) at arthroscopy, no significant articular cartilage erosion higher than grade II according to the Outerbridge classification, (3) absence of injury to ligaments in the contralateral knee and (4) no accompanying injury to the posterior cruciate ligament (PCL) or other ligaments. Patients with concomitant meniscal injuries were not excluded. The decision to perform single- or double-bundle ACL reconstruction was made intraoperatively on the basis of the quality, length and size of the tendons, and the size and diameter of the lateral femoral condyle. The median age of the patients at the time of surgery was 28.1 years (range 16.1– 46.4 years) in the SB group and 29.0 years (range 19.2–43.7 years) in the DB group. The DB group consisted of 12 men and ten women and the SB group of 11 men and nine women. The median interval between injury and surgery was 15.3 months (range 1.1–36.4 months). The median follow-up period was 36.4 months (range 24.0–45.8 months) in the SB group and 31.3 months (range 25.2–49.0 months) in the DB group. All ACL reconstructions were performed by the senior co-author. Clinical and radiological data were registered on a professional electronic database. At follow-up, the examination for assessment included the Lachman test and the pivot shift test. For quantitative measurement, anterior laxity at a standard manual force of 134 N was measured on a KT3000 arthrometer (MEDmetric Corporation, San Diego, CA, USA). All manual tests were repeated three times to ascertain reliable data. The results of the arthrometer investigation were recorded as a side-to-side difference between the injured and the intact knee [5]. The IKDC [6], Lysholm score [7] and Tegner activity score [8] were used for subjective clinical assessment. All clinical examinations were performed by one blinded examiner. Post-operatively, all cases underwent X-ray and 64-row CT scan to evaluate the tibial tunnel placement and the graft. The correct position of the femoral and tibial tunnels and the ENDOBUTTON on the lateral aspect of the distal femoral compact bone, was analysed by an experienced and independent radiologist. All operations were performed under lumbar anaesthesia using a tourniquet and standard arthroscopy-assisted two incision techniques. A complete diagnostic arthroscopy was performed to confirm the ACL tear followed by treatment of meniscal injury if required. Following graft harvesting, for single-bundle reconstruction, we quadrupled the ST and the GT to create a bunch exceeding 7~8 mm in diameter and 120 mm in length. The mean diameter of the proximal end of the graft was 7.5 ± 0.5 mm (range 7–9 mm). The proximal ends were fixed using an ENDOBUTTON CL (Smith&Nephew), and the distal ends were fixed using a bio-interference screw (Smith&Nephew).
For double-bundle reconstruction, depending on the length and strength of the tendon, the ST and if necessary the GT were harvested. Both tendons were doubled or tripled to a diameter of more than 5.0 mm. Thicker grafts were used for the AM bundle and thinner ones for the PL bundle. The mean diameter of the proximal end of the AM and PL bundles was 6.6 ± 1.1 mm (range 6.0–7.5 mm) and 5.4 ± 0.8 mm (range 5.0–7.0 mm), respectively.
Navigation
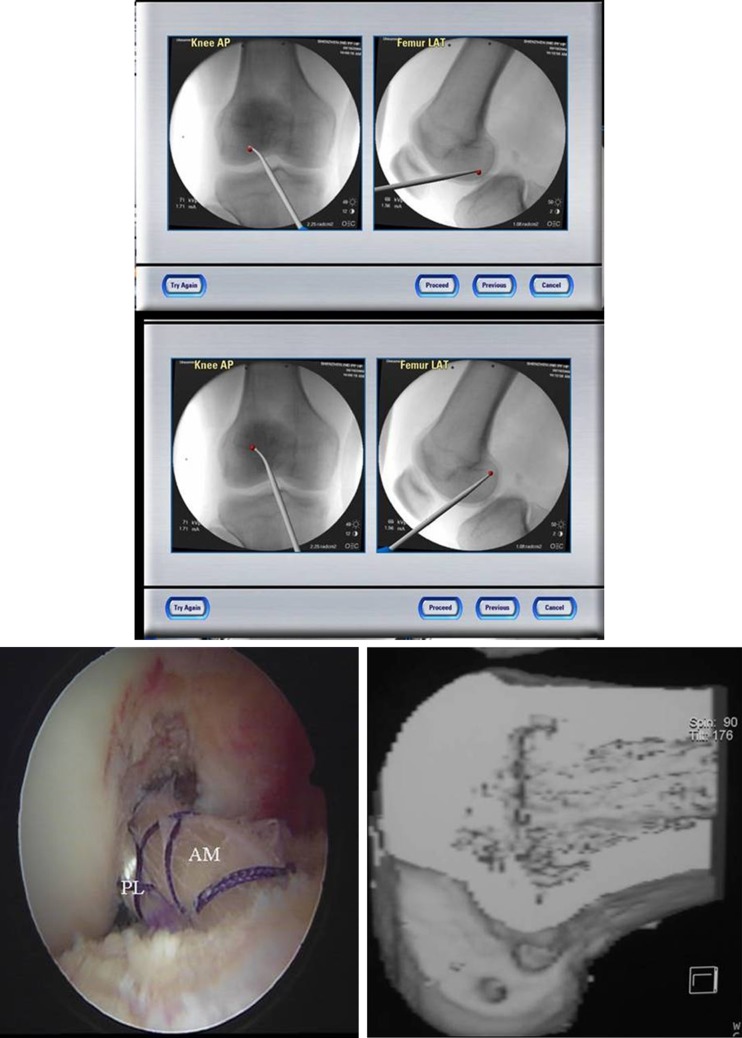
Two K-wires of 2.5-mm diameter were placed in the distal portion of the femur and the proximal portion of the tibia, and rigid bodies with reflective markers were attached (Fig. 1). Patient data and the size of the tendon graft were entered into the computer. The extra-articular and intra-articular aspects as well as the kinematics of the knee joint were registered by the system using a straight pointer. The extra-articular landmarks included the tibial tuberosity, the anterior edge of the tibia, and the medial and lateral points of the tibial plateau. Intra-articular landmarks included the anterior edge of the PCL on the tibial plateau, the anterior horn of the lateral meniscus, the spine of the medial intercondylar tubercle, the medial notch wall, the anterior notch outlet, the lateral notch wall, the ACL insertion area on the femur, the 12 o’clock “over-the-top” position and the lateral over-the-top position. Using a special tibial aimer with attached markers, the exact location of the tibial and femoral tunnels could be selected on the basis of real-time information about the tibial plateau as seen on the OrthoPilot map [19] (Fig. 2). The tibial and femoral tunnels were then made under arthroscopic visualisation and navigation.
Fig. 1.
Arthroscopy of the left knee. K-wires (arrow 1) with rigid bodies (arrow 2) and reflected markers (arrow 3) are placed at the distal part of the femur and proximal part of the tibia to provide a connection to the OrthoPilot navigation system
Fig. 2.
Real-time information for optimal ACL tunnel position on the tibial plateau on the OrthoPilot navigation system monitor. The view at the top of the tibial plateau shows the optimal ACL insertion with a distance of 8 mm in front of the PCL and with a distance of 46 % from the medial side of the tibial plateau
SB group
Following preparation of the tibial tunnel through the centre of the AM bundle, the femoral tunnel of the AM bundle was created by a guide pin using a transtibial tunnel technique, which was drilled to a point 5 mm anterior to the over-the-top position of the femur at the 10 o’clock position for the right knee (or 2 o’clock for the left knee). The graft was passed through, and the ENDOBUTTON was flipped and fixed to the lateral cortex of the femur with the knee at 30° of flexion and the foot in neutral rotation. The distal end of the bundle was fixed by a bio-interference screw. After fixation, we applied 80 N of tension to the required stability in 30° flexion. At the end of the procedure, stability was measured using a Lachman test exactly at the same angle as that used preoperatively.
DB group
The tibial tunnels were made in the same manner with the aid of the navigator, while the femoral tunnels were made with the parallel guide, at 11 and 9.30 o’clock positions for the right and 1 and 2.30 o’clock positions for the left knee. The PL bundle was first passed through the tibial and femoral tunnels. The fixation procedure was the same as that used in the SB group.
Statistical methods
To investigate differences in KT3000 values between the single- and the double-bundle procedure, an analysis of variance for the pre–post differences in KT3000 of the operated leg accounting for the factor treatment (single- or double-bundle) as well as for age, body mass index (BMI), sex, side (the injured leg is the dominant leg: yes/no), type of accident (non-contact/contact), type of graft (ST—ST/GT) and mechanism of accident (rotation/extension) was calculated. For each of the scores measured after treatment (IKDC, Lysholm and Tegner) and the decrease in internal rotation, a similar analysis of variance with the factor treatment and the covariables of sex, age, side, type and mechanism of accident were performed. All P values ≤0.05 were considered to be statistically significant. All analyses were performed using the SPSS 14.0 System.
Results
At follow-up, all patients were satisfied with the result. No patient complained about continued attacks of “giving way”, persistent joint effusion, or a flexion or extension deficit. No major complications such as venous thromboses, pulmonary embolism, wound healing problems or intra-articular infections were encountered post-operatively in either group. With regard to post-operative side-to-side anterior laxity measured with the KT3000 arthrometer, no statistically significant difference in the pre–post reduction in KT3000 values was registered between treatments (Table 1). With regard to the type of graft, no statistical influence on KT1000 values or subjective findings was observed for quadrupled ST or ST/GT grafts. Otherwise, the patient’s age, BMI, gender, side or type of accident had no impact on KT3000 values. Concerning the results of the pivot shift test, better results were registered in the DB group than in the SB group (Table 1). The IKDC and Lysholm scores were significantly higher in the DB group. Both groups achieved excellent or good results (Table 2). The Tegner score showed no statistically significant difference between the SB and the DB groups. Post-operative radiographs revealed no malpositioning of the tibial or femoral tunnels—such as far anterior placement of the tunnel—in either group. No tunnel merging occurred in the DB group. The “flipped” ENDOBUTTON was correctly positioned on the lateral side of the distal femoral compact bone in all patients.
Table 1.
Functional outcome of computer-navigated single- and double-bundle ACL reconstruction after 2 years of follow-up
| SB | DB | P value | |
|---|---|---|---|
| Pivot shift testing − | 16 | 19 | NS |
| Pivot shift testing + | 4 | 3 | P=0.033 |
| Pivot shift testing ++ | 0 | 0 | |
| KT3000 side-to-side difference (mm) | 0.31±0.68 | 0.40±0.52 | NS |
Table 2.
Clinical outcome (Tegner, IKDC and Lysholm scores) of computer-navigated single- and double-bundle ACL reconstruction after 2 years of follow-up
| SB | DB | P value | |
|---|---|---|---|
| Tegner | 7 (range 5–9) | 7 (range 5–9) | NS |
| IKDC | 87.7±9.6 | 90.3±8.7 | P=0.039 |
| Lysholm | 91.2±7.2 | 92.5±9.0 | P=0.042 |
Discussion
The most important finding in this study was that patients who received a computer-navigated hamstring autograft double-bundle ACL reconstruction had significantly better rotational laxity as seen on pivot shift testing and navigated measurements, as well as excellent subjective satisfaction, compared to the single-bundle ACL procedure.
Although ACL reconstruction is one of the most frequently performed procedures in orthopaedic surgery, it does not consistently provide a good outcome: graft failure rates of 16–25 % have been reported during the first year [9]. Generally, orthopaedic surgeons are confronted with two problems that affect the functional outcome of primary ACL reconstruction: (1) The first is correct placement of the femoral tunnel, which is the most crucial aspect of ACL reconstruction and a major challenge. A reconstructed graft placed too far anteriorly on the femoral condyle may lead to reduced flexion and instability in the knee joint, whereas a graft positioned too far posteriorly may result in reduced extension and early graft failure. Incorrect placement of the tibial and femoral tunnels is the main reason for technical failure in ACL reconstruction [10]. (2) The second problem is persistent instability of the knee after single-bundle ACL reconstruction despite correctly positioned tunnels [11]. The influence of the “mini” pivot shift phenomenon, a measurable positive pivot shift sign too low to introduce any subjective symptoms of instability but high enough to indicate degeneration of the meniscus and degenerative osteoarthritis, has been extensively and controversially discussed [12]. In the past, conventional ACL reconstruction procedures have focused on replacing the AM bundle by a single-bundle technique while ignoring the PL bundle [13]. The “multiple-bundle” configuration of the ACL, subdivided into AM and PL bundles and each having different functions in knee kinematics, was first described more than 20 years ago by Ferretti et al. [14]. In biomechanical cadaver studies, Mae et al. [15] and Yagi et al. [16] showed that anatomical ACL double-bundle reconstruction provides better anteroposterior and rotational knee stability; furthermore, two bundles can replicate the native ACL ligament more closely than a single bundle in terms of knee stability. Subsequently, anatomical double-bundle ACL reconstruction became one of the most popular and widely discussed topics in orthopaedic surgery. Currently, double-bundle techniques are extensively used for reconstruction of the ACL and have been described by several authors [17]; two year outcomes have been reported by some. Nevertheless, clinical evidence to show that the double-bundle is superior to the single-bundle technique for ACL reconstruction has not yet been provided. The two procedures have been compared in five randomised controlled trials (RCTs), two quasi-RCTs and two prospective comparative cohort studies. In a meta-analysis, Meredick et al. [4] reported a mean side-to-side difference of 0.52 mm closer to normal on the KT1000 arthrometer in patients who underwent double-bundle reconstruction compared to those who received single-bundle reconstruction. In fact, the KT1000 arthrometer measures anterior knee laxity in 1-mm increments of precision and the IKDC considers a post-operative side-to-side difference of up to 2 mm as normal. Meredick et al. registered statistically significant but clinically insignificant data. With regard to rotational stability, their findings showed no statistically significant difference in pivot shift when comparing clinical outcomes after single-bundle versus double-bundle ACL reconstruction. Interestingly, the pivot shift test yielded diverse, but no clinical differences in all of the studies. The reliability and sensitivity of the pivot shift phenomenon are influenced by several factors. The execution of the test may vary, depending on the manoeuvre and the examiner [18]. Moreover, the pivot shift test is a subjective assessment. Manually applied forces and displacements are inconsistent and difficult to assess. The speed of the procedure, the angle of hip abduction during the test and the magnitude of force applied to the knee depend on the investigator and the test used [19]. Post-operatively, we found a significant reduction in laxity in both groups. Translational stability was graded as excellent by subjects of both groups. At the two year clinical follow-up, a statistically non-significant side-to-side difference of 0.12 mm was noted in the SB group compared to 0.11 mm in the DB group. With regard to rotational stability, a significantly higher post-operative reduction in internal rotation was observed in the DB group than in the SB group (15 and 7°, respectively; P<0.001). Whether a major reduction in internal rotation provides better clinical results has not yet been proven. In a biomechanical cadaver study on intact knees, Zurfluh et al. showed a mean internal rotation of 10, 13.6 and 17° at knee flexions of 20, 60 and 90°. However, the reported data represent the mean reduction in internal rotation at the same angle of measurement in different knees, using the two methods of reconstruction. Better rotational stability may prevent and reduce degenerative osteoarthritis; long-term results are required to confirm this thesis. Subjective findings were significantly better in the DB group, whereas both groups achieved excellent and satisfactory results. Accurate computer-navigated placement of the tunnel is an essential prerequisite to achieve a good clinical outcome with the procedure. Several studies have shown that an incorrectly placed tunnel is the main reason for graft failure and is frequently associated with instability of the knee joint after ACL reconstruction [11]. The question remains as to whether the use of four tunnels in a double-bundle construct rather than two in a single-bundle repair would increase the rate of failure. These problems could probably be avoided and the precision of tunnel placement enhanced by the use of computer-assisted navigation [20]. In the published orthopaedic literature, computer-assisted surgery has been reported to raise the accuracy of tunnel placement and reduce the rate of revision surgery. Picard et al. [21] presented a randomised prospective study comparing the accuracy of tunnel placement performed using a traditional arthroscopic ACL reconstruction technique and a surgical navigation technique. Two experienced surgeons in ACL reconstruction randomly used traditional arthroscopic guides or navigated assisted guides to drill a tunnel in 20 identical foam knees. The distances from the ideal tunnel placement to the femoral and tibial tunnels were 4.2 ± 1.8 and 4.9 ± 2.3 mm, respectively, for the traditional arthroscopic technique and 2.7 ± 1.9 and 3.4 ± 2.3 mm, respectively, for the computer-assisted ACL reconstruction. With no need for intraoperative X-rays, highly effective in evaluating the global performance of the reconstructed knee, anteroposterior (AP), internal rotation (IR) and external rotation (ER) rotation of the tibia documentation [22] as well as precise assistance in tunnel placement, computer navigation could become routine in the future. The principal advantage of this study was that all ACL reconstructions were performed by a single experienced surgeon [23]. The primary limitation of the study was its retrospective design. A further limitation was the small number of patients. However, in view of the fact that experience with computer-navigated ACL single-bundle and double-bundle reconstruction has not yet been reported in the published literature, the size of our patient group is comparable to that of other studies reporting the results of double-bundle reconstruction.
Perspective
Computer-assisted ACL reconstruction is an accurate means of graft placement and yields favourable clinical results. Computer guidance enabled the tibial and femoral tunnels to be systematically positioned within the anatomical area and, as regards the tibial area, within the anterior third near to the medial tibial spine, without femoral notch impingement. The use of computer-assisted ACL reconstruction could be useful for inexperienced surgeons to avoid malposition. A long observation period would be needed to determine the relevance of double-bundle ACL reconstruction in terms of improving osteoarthritis or meniscus degeneration. To improve the quality of results, it thus seemed necessary to increase the accuracy of tunnel positioning, and computer-assisted surgical navigation has made this feasible. It is also mandatory to have sufficient experience in ligament surgery and in surgical navigation if inconsistency is to be avoided, although it remains possible to cross over from the navigation protocol to a conventional method.
Acknowledgment
This study received financial support from the Emerging Scientist Project of Shenzhen Second People’s Hospital and the Guangdong Province Medical Research Fund (the project number is B2012320) and Guangdong Province outstanding youth innovative talent training program (Seedling project, the project number is 2012LYM_0120).
Contributor Information
Daping Wang, Phone: +86-755-83791866, FAX: +86-755-83356952, Email: szhzwm@126.com.
Yanjun Zeng, Phone: +86-10-67391809, FAX: +86-10-67391809, Email: yjzeng@bjut.edu.cn.
References
- 1.Aglietti P, Giron F, Buzzi R, et al. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective randomized clinical trial. J Bone Joint Surg Am. 2004;86:2143–2155. [PubMed] [Google Scholar]
- 2.Gabriel MT, Wong EK, Woo SL, et al. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 3.Aglietti P, Giron F, Cuomo P, et al. Single- and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res. 2007;454:108–113. doi: 10.1097/BLO.0b013e31802baaf4. [DOI] [PubMed] [Google Scholar]
- 4.Meredick RB, Vance KJ, Appleby D, et al. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 5.Amis A, Bull AMJ, Lie DT. Biomechanics of rotational instability and anatomic anterior cruciate ligament reconstruction. Oper Tech Orthop. 2005;15:29–35. doi: 10.1053/j.oto.2004.10.009. [DOI] [Google Scholar]
- 6.Hefti F, Müller W. Current state of evaluation of knee ligament lesions. The new IKDC knee evaluation form. Orthopade. 1993;22:351–362. [PubMed] [Google Scholar]
- 7.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–153. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 8.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 9.Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 10.George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2026–2037. doi: 10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
- 11.Laxdal G, Kartus J, Hansson L, et al. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:34–42. doi: 10.1016/j.arthro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 12.Lopomo N, Zaffagnini S, Bignozzi S, et al. Pivot-shift test: analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res. 2010;28:164–169. doi: 10.1002/jor.20966. [DOI] [PubMed] [Google Scholar]
- 13.Yagi M, Kuroda R, Nagamune K, et al. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 14.Ferretti A, Conteduca F, De Carli A, et al. Osteoarthritis of the knee after ACL reconstruction. Int Orthop. 1991;15(4):367–371. doi: 10.1007/BF00186881. [DOI] [PubMed] [Google Scholar]
- 15.Mae T, Shino K, Miyama T, et al. Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy. 2001;17:708–716. doi: 10.1053/jars.2001.25250. [DOI] [PubMed] [Google Scholar]
- 16.Yagi M, Wong EK, Kanamori A, et al. Biochemical analysis of an anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 17.Marcacci M, Molgora AP, Zaffagnini S, et al. Anatomic double-bundle anterior cruciate ligament reconstruction with hamstrings. Arthroscopy. 2003;19:540–546. doi: 10.1053/jars.2003.50129. [DOI] [PubMed] [Google Scholar]
- 18.Domzalsk M, Grzelak P, Gabos P. Risk factors for anterior cruciate ligament injury in skeletally immature patients: analysis of intercondylar notch width using magnetic resonance imaging. Int Orthop. 2010;34(5):703–707. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Legnani C, Ventura A, Terzaghi C, et al. Anterior cruciate ligament reconstruction with synthetic grafts. A review of literature. Int Orthop. 2010;34(4):465–471. doi: 10.1007/s00264-010-0963-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kodali P, Yang S, Koh J. Computer-assisted surgery for anterior cruciate ligament reconstruction. Sports Med Arthrosc. 2008;16:67–76. doi: 10.1097/JSA.0b013e318175d189. [DOI] [PubMed] [Google Scholar]
- 21.Picard F, DiGioia AM, Moody J, et al. Accuracy in tunnel placement for ACL reconstruction. Comparison of traditional arthroscopic and computer-assisted navigation techniques. Comput Aided Surg. 2001;6:279–289. doi: 10.3109/10929080109146093. [DOI] [PubMed] [Google Scholar]
- 22.Colombet P, Robinson J, Christel P, et al. Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res. 2007;454:59–65. doi: 10.1097/BLO.0b013e31802baf56. [DOI] [PubMed] [Google Scholar]
- 23.Araki D, Kuroda R, Kubo S, et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. 2011;35(3):439–446. doi: 10.1007/s00264-010-1110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]