Abstract
Background
Revascularization by coronary artery bypass graft (CABG) surgery or percutaneous coronary intervention (PCI) is frequently deferred in patients with chronic kidney disease (CKD) to avoid precipitating end-stage renal disease (ESRD), but reliable estimates of absolute and relative risks of death and ESRD following CABG and PCI are unavailable.
Methods and Results
CKD patients undergoing CABG (n = 4547) or PCI (n = 8620) were identified and tracked using the 5% Medicare sample. The cumulative incidence of ESRD and death were reported for observed events. A Cox model with the Fine-Gray method was used to account for competing risks in assessing relative hazards of death and ESRD. Three-year cumulative incidence of ESRD was lower (CABG, 6.8%; PCI, 5.4%) than death (CABG, 28.3%; PCI, 32.8%). The adjusted hazard ratio of death was higher during the first 3 months after CABG than after PCI (1.25, 95% confidence interval 1.12-1.40, P < 0.001), but lower from 6 months on (0.61, 0.55-0.69). Conversely, risk of ESRD after CABG was higher during the first 3 months (1.59, 1.27-2.01, P < 0.001), but was not statistically significant from 3 months on. The adjusted hazard ratio of combined death or ESRD was similar to death.
Conclusions
Among CKD patients undergoing coronary revascularization, death is more frequent than ESRD. The Incidence of ESRD was lower throughout follow-up after PCI, but long-term risks of death or combined death and ESRD were lower after CABG. Our data suggest better overall clinical outcomes with CABG than with PCI in CKD patients.
Keywords: Angioplasty, coronary disease, kidney, revascularization, surgery
Introduction
Chronic kidney disease (CKD) is associated with high risk of developing and dying from cardiovascular disease.1,2 Elderly CKD patients are 5 to 10 times more likely to die from cardiovascular disease than to develop end-stage renal disease (ESRD).3 This high risk may be partly explained by the more than 50% prevalence and diffuse nature of obstructive coronary atherosclerosis in patients with severe CKD.4
Despite high prevalence and high risk of coronary disease in this population, use of coronary revascularization is paradoxically lower in patients with than without CKD.5 Nevertheless, whether use of coronary artery bypass graft (CABG) surgery and percutaneous coronary intervention (PCI) should be increased and how the choice between these procedures should be optimized in patients with CKD remains uncertain. CABG provides more complete revascularization and reduces mortality in high-risk patients,6 but its benefits relative to PCI may be limited by operative mortality rates 4- to 5-fold higher in patients with advanced CKD than in patients without CKD.7 CABG is also associated with high risk of perioperative acute kidney injury (AKI) when pre-existing CKD is present.8 Even minor episodes of AKI may hasten progression to ESRD, and CABG can negatively affect overall quality of life for patients who become dialysis dependent postoperatively.
Despite studies in the general population suggesting that PCI is inferior to CABG in patients with high-risk coronary anatomy,9 PCI offers a less invasive alternative with potentially lower procedural risks of death and ESRD. Whether CABG or PCI is the best choice for a particular CKD patient depends on the relative strength of that patient’s preference for avoiding dialysis compared with avoiding death, and on the timing and relative risks of each outcome following each procedure. Currently, absence of reliable risk estimates in patients with CKD limits clinicians’ ability to make evidence-based decisions. To address this important knowledge gap, we compared risks of death and ESRD in a contemporary cohort of elderly CKD patients undergoing CABG and PCI.
Methods
Study Population and Follow-Up
Medicare fee-for-service enrollees (enrolled in Medicare Part A and Part B but not in a health maintenance organization) with CKD were identified from the 5% Medicare database, a random sample of all Medicare beneficiaries. Patients undergoing an index revascularization procedure were included if they underwent first CABG or PCI between 2001 and 2007, were Medicare fee-for-service enrollees for > 12 months before the index procedure, were aged 66 years or older, and resided in the United States or its territories. Patients with ESRD, undergoing concomitant valvular surgery, or undergoing CABG and PCI during the same hospitalization were excluded. Patients were followed from the date of the index procedure to the earliest of death, ESRD, subsequent revascularization, 3 years after the index procedure, or December 31, 2008. Date of death and ESRD status were obtained from the Medicare 5% data. Date and onset of ESRD were defined using information from the Centers for Medicare & Medicaid Medical Evidence Report (form CMS-2728), which is required from providers within 45 days of dialysis initiation or transplant.
Comorbid Conditions
CABG, PCI, procedural characteristics, and dates were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and Current Procedural Terminology codes on Medicare inpatient claims, outpatient institutional claims, revenue claims, and line items of Part B physician/supplier claims (Supplementary Table 1). Because all CABGs are inpatient procedures, only inpatient PCIs were included in the analysis to ensure comparability.
Comorbid conditions were defined by qualifying ICD-9-CM diagnosis codes on at least 1 Part A inpatient, skilled nursing facility, or home health claim, or on 2 Part A outpatient or Part B claims on different days during the time period from 12 months preceding the index procedure to discharge. Supplementary Table 1 lists ICD-9-CM diagnosis codes for each comorbid condition.
Statistical Analysis
Baseline characteristics are presented as n (%) with differences assessed using χ2 tests. Because death and ESRD were considered to be competing risks with each other in this study, the cumulative incidence method was used to report the observed event probabilities of ESRD and death. Visual inspection revealed that the proportionality between risk of ESRD and death was questionable, and a piecewise Cox regression model was used with the Fine-Gray method10 to handle competing risk and adjust for all demographic and comorbid conditions listed in Table 1. Subgroup analyses with age cut-off at 80 years were performed. Sensitivity analyses were conducted by restricting the CABG and PCI comparison to subgroups of patients undergoing multi-vessel intervention, off-pump CABG, CABG with internal mammary graft, and PCI with drug-eluting stent. Descriptive analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC). The Fine-Gray Cox model was implemented in R package. P < 0.05 was considered significant.
Table 1.
Baseline Patient Characteristics
| Characteristic | CABG | PCI | P |
|---|---|---|---|
| n | 4547 | 8620 | |
| Age, yr | < 0.001 | ||
| 66-69 | 874 (19.2) | 1370 (15.9) | |
| 70-74 | 1279 (28.1) | 2063 (23.9) | |
| 75-79 | 1330 (29.3) | 2298 (26.7) | |
| ≥ 80-up | 1064 (23.4) | 2889 (33.5) | |
| Men | 3028 (66.6) | 4838 (56.1) | < 0.001 |
| Race | 0.009 | ||
| White | 4045 (89.0) | 7532 (87.4) | |
| Black | 298 (6.6) | 692 (8.0) | |
| Other | 204 (4.5) | 396 (4.6) | |
| Year | < 0.001 | ||
| 2001 | 581 (12.8) | 1033 (12.0) | |
| 2002 | 653 (14.4) | 1051 (12.2) | |
| 2003 | 660 (14.5) | 1143 (13.3) | |
| 2004 | 636 (14.0) | 1227 (14.2) | |
| 2005 | 607 (13.4) | 1301 (15.1) | |
| 2006 | 778 (17.1) | 1509 (17.5) | |
| 2007 | 632 (13.9) | 1356 (15.7) | |
| Comorbid conditions | |||
| Congestive heart failure | 2569 (56.5) | 4719 (54.7) | 0.05 |
| Dysrhythmia | 3012 (66.2) | 4636 (53.8) | < 0.001 |
| Myocardial infarction | 2191 (48.2) | 4526 (52.5) | < 0.001 |
| Cardiac (other) | 2653 (58.4) | 4198 (48.7) | < 0.001 |
| CVA/TIA | 1599 (35.2) | 2224 (25.8) | < 0.001 |
| PVD | 2361 (51.9) | 4390 (50.9) | 0.28 |
| Anemia | 2256 (49.6) | 3626 (42.1) | < 0.001 |
| Cancer | 631(13.9) | 1302 (15.1) | 0.06 |
| COPD | 1656 (36.4) | 2808 (32.6) | < 0.001 |
| Diabetes | 2559 (56.3) | 4567 (53.0) | < 0.001 |
| Gastrointestinal disease | 512 (11.3) | 1016 (11.8) | 0.37 |
| Hypertension | 4337 (95.4) | 8181 (94.9) | 0.23 |
| Liver disease | 91 (2.0) | 153 (1.8) | 0.36 |
Values are n (%).
ASHD, atherosclerotic heart disease; CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; CVA/TIA, cerebrovascular accident/transient ischemic attack; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease.
Research conducted by the United States Renal Data System is classified as exempt under institutional review board regulations.
Results
Baseline Characteristics
We identified 4574 CKD patients who underwent CABG and 8620 who underwent PCI during the study period. CKD stage was unspecified (ICD-9-CM code 585.9) or missing in 86.0% of CABG and 87.5% of PCI patients, and identified as stage 3-5 in 506 (11.1%) CABG and 881 (10.2%) PCI patients; P = 0. 03. CABG patients were more likely to be younger (23.4% vs. 33.5% aged ≥ 80 years, P < 0.001), male (66.6% vs. 56.1%, P < 0.001), and white (89.0% vs. 87.4%, P = 0.009; Table 1). Dysrhythmia (66.2% vs. 53.8%, P < 0.001), diabetes (56.3% vs. 53.0%, P < 0.001), and chronic obstructive pulmonary disease (36.4% vs. 32.6%, P < 0.001) were more common in CABG than PCI patients. History of myocardial infarction was less common in CABG patients (48.2% vs. 52.5%, P < 0.001).
Stents were used in most PCIs (Table 2); only 826 (9.6%) were performed with angioplasty alone. Drug-eluting stents were the most common stent types, used in 3660 (42.4%) cases. Most PCIs were single-vessel interventions; 1958 (22. 7%) involved 2 or more vessels. Three or more vessels were bypassed in 3641 (80.1%) CABG surgeries. Most CABGs (81.8%) used internal mammary grafts.
Table 2.
Procedural Characteristics
| Characteristic | Number | Percent |
|---|---|---|
| PCI (n = 8620) | ||
| Number of Vessels | ||
| 1 | 6662 | 77.3 |
| ≥ 2 | 1958 | 22.7 |
| Number of stents | ||
| PTCA only | 826 | 9.6 |
| 1 | 6828 | 79.2 |
| ≥ 2 | 966 | 11.2 |
| Type of stent | ||
| Bare metal | 4134 | 48.0 |
| Drug eluting | 3660 | 42.5 |
| CABG (n = 4547) | ||
| Number of vessels | ||
| Unknown | 19 | 0.4 |
| 1 | 194 | 4.3 |
| 2 | 693 | 15.2 |
| 3 | 1651 | 36.3 |
| ≥ 4 | 1990 | 43.8 |
| Off- pump | 732 | 16.1 |
| Internal mammary artery graft | 3721 | 81.8 |
CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention; PTCA, percutaneous transluminal coronary angiography.
Outcomes
In-hospital death was more frequent after CABG than after PCI (7.1% vs. 3.9%, P < 0.001). Cumulative incidence of death was higher during the first 14 months after CABG than after PCI, was similar at month 15 (CABG, 19.6%; PCI, 19.5%), and was subsequently lower in CABG patients. The incidence of ESRD remained higher after CABG throughout follow-up. However, ESRD occurred much less frequently than death (cumulative incidence of death at 36 months: CABG, 28.3%; PCI, 32.8%), and differences in cumulative incidence of ESRD at 36 months were small (CABG, 6.8%; PCI, 5.4%) (Table 3).
Table 3.
Cumulative Incidence of Death, ESRD or Combined Death or ESRD
| Outcome
|
||||||
|---|---|---|---|---|---|---|
| Death | ESRD | Death or ESRD | ||||
| Month | CABG | PCI | CABG | PCI | CABG | PCI |
| 0 | 0.000 | 0.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| 3 | 0.124 | 0.099 | 0.033 | 0.019 | 0.157 | 0.118 |
| 6 | 0.156 | 0.132 | 0.038 | 0.024 | 0.195 | 0.157 |
| 12 | 0.183 | 0.175 | 0.044 | 0.030 | 0.227 | 0.205 |
| 24 | 0.232 | 0.258 | 0.056 | 0.040 | 0.288 | 0.298 |
| 36 | 0.283 | 0.328 | 0.068 | 0.054 | 0.352 | 0.382 |
CABG, coronary artery bypass graft; ESRD, end-stage renal disease; PCI, percutaneous coronary intervention.
Because the risks of death and ESRD were not proportional over time (Figure 1), piecewise Fine-Gray Cox models were constructed to account for the time dependency of risk and competing-risk data (Table 4). In adjusted analyses, the relative risk of death declined over time and was consistent with increased risk of perioperative death but greater long-term reduction in death after CABG than after PCI. Hazard ratios (HRs) (95% confidence interval [CI]) were 1.25 (1.12-1.40), ≤ 3 months; 1.03 (0.83-1.28), > 3-≤6 months; 0.61 (0.55-0.69), > 6-36 months. During the first 3 months, risk of ESRD was 1.59-fold higher (95% CI 1.27-2.01) after CABG, but non-significantly lower from 3 months to the end of follow-up (HR 0.97, 95% CI 0.77-1.21). Consistent with the much greater absolute risk of death than of ESRD, relative risks of the combined outcome favored PCI during the first 3 months and CABG during the remainder of follow-up. HRs (95% CI) for CABG vs. PCI were 1.30 (1.17-1.43), ≤ 3 months; 0.99 (0.81-1.20), > 3-≤ 6 months; 0.66 (0.60-0.73), > 6-36 months.
Figure 1.
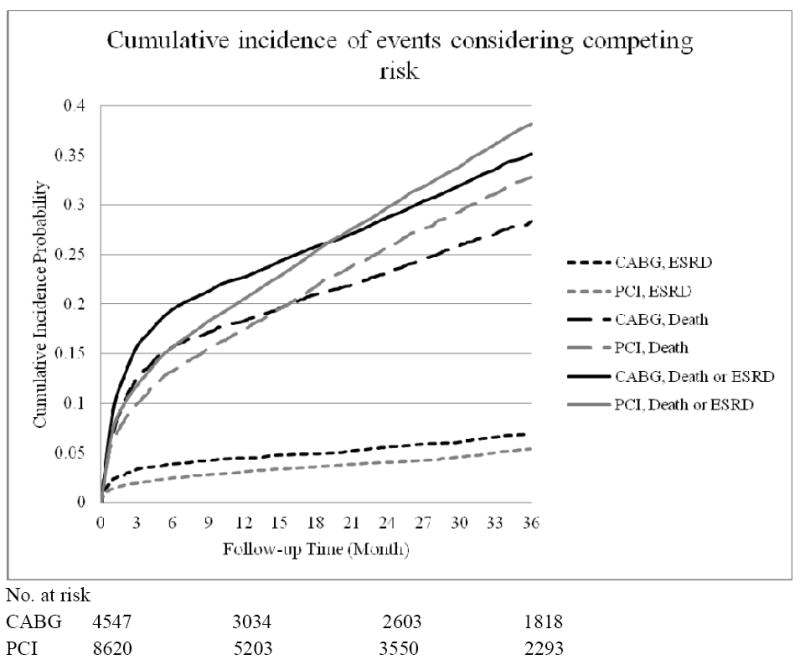
Cumulative incidence for death, ESRD, and death or ESRD after accounting for competing risks. CABG, coronary artery bypass graft; ESRD, end-stage renal disease; PCI, percutaneous coronary intervention.
Table 4.
Crude and Adjusted Associations of Revascularization Strategy With Outcomes During Follow-Up from a Competing-Risk Model
| Death | ESRD | Death or ESRD | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | |
| Crude | ||||||
| CABG vs. PCI* ≤ 3 m | 1.26 (1.13-1.40) | < 0.001 | 1.75 (1.40-2.20) | < 0.001 | 1.35 (1.22-1.48) | < 0.001 |
| CABG vs. PCI > 3-≤ 6 m | 1.02 (0.83-1.25) | 0.85 | NA | NA | 1.01 (0.84-1.23) | 0.90 |
| CABG vs. PCI† > 6-36 m | 0.64 (0.58- 0.72) | < 0.001 | 1.08 (0.86-1.34) | 0.513 | 0.69 (0.63-0.77) | <0.001 |
| Adjusted | ||||||
| CABG vs. PCI* ≤ 3 m | 1.25 (1.12-1.40) | < 0.001 | 1.59 (1.27-2.01) | < 0.001 | 1.30 (1.17-1.43) | < 0.001 |
| CABG vs. PCI >3-≤ 6 m | 1.03 (0.83-1.28) | 0.77 | NA | NA | 0.99 (0.81-1.20) | 0.88 |
| CABG vs. PCI† > 6-36 m | 0.61 (0.55-0.69) | < 0.001 | 0.97 (0.77-1.21) | 0.78 | 0.66 (0.60-0.73) | < 0.001 |
Results using cutoffs of ≤ 3 months, > 3-≤ 6 months and > 6-36 months (death, combined death/ESRD), and intervals of
≤ 3 months and
> 3-36 months (ESRD). Covariates in the model included age, sex, race, year of procedure performed, congestive heart failure, dysrhythmia, myocardial infarction, other cardiac disease, cerebrovascular accident/transient ischemic attack, peripheral vascular disease, anemia, cancer, chronic obstructive pulmonary disease, diabetes, gastrointestinal disease, hypertension, and liver disease.
CI, confidence interval; HR, hazard ratio; NA, not applicable.
Subgroup Analysis
Risks of ESRD after CABG vs. PCI were qualitatively similar between patients aged < 80 years and ≥ 80 years, high during the first 3 months (HR 1.57, 95% CI 1.21-2.04 for patients aged < 80 years; HR 1.67, 95% CI 1.04-2.69 for patients aged ≥ 80 years), but not significantly lower from 3 months on (HR 0.98, 95% CI 0.77-1.26 for patients aged < 80 years; HR 0.88, 95% CI 0.51-1.52 for patients aged ≥ 80 years). In contrast, early risks of death during the first 3 months after CABG vs. PCI were qualitatively higher in patients aged < 80 years (HR 1.34, 95% CI 1.16-1.55) than in patients aged ≥ 80 years (HR 1.12, 95% CI 0.93-1.34). Late risks of death after 6 months favored CABG slightly more in patients aged < 80 years (HR 0.59, 95% CI 0.51-0.68) than in patients aged ≥ 80 years (HR 0.65, 95% CI, 0.54-0.78).
Sensitivity Analysis
Outcomes of CABG vs. PCI were qualitatively similar in comparisons restricted to patients undergoing multi-vessel intervention, CABG with internal mammary graft, or PCI with drug-eluting stent (data not shown). Early and late risks of death were qualitatively similar in a comparison of off-pump CABG with PCI. HRs (95% CI) were 1.23 (0.98-1.55), ≤ 3 months; 0.76 (0.61-0.95), > 6-36 months. Early risk of ESRD (1.20 [0.72-2.00], ≤ 3 months) appeared to be attenuated and risks of late progression were similar (1.11 [0.71-1.72]), > 3-36 months).
Discussion
We analyzed outcomes after coronary revascularization in a large, contemporary cohort of Medicare patients with CKD. We found that risks of early mortality and ESRD are higher after CABG than after PCI, but long-term survival is better. In contrast, the relative risk of ESRD was significantly higher after CABG. However, absolute risk of ESRD was low (3.3% at 3 months, 6.8% at 3 years) compared with the risk of death at 3 years after CABG (28.3%) and PCI (32.8%). Risk of the combined outcome of death or ESRD closely mirrored risk of death.
Coronary artery disease is highly prevalent in the CKD population,4,11 and risk of developing and dying from cardiovascular disease is high.2 Nevertheless, revascularization procedures are underused.5,12 Absence of randomized studies comparing CABG and PCI in this population, together with concerns that coronary revascularization, especially CABG, may precipitate progression to ESRD, are likely important factors underlying low use. These factors may also influence the choice between CABG and PCI, since avoiding dialysis dependence and avoiding death may be equally important to CKD patients. To our knowledge, however, the relative risks of ESRD after CABG and after PCI have not been previously estimated.
Our finding of increased short-term mortality but overall reduction in mortality with CABG compared with PCI is consistent with a previous study of CKD patients who underwent coronary angiography,13 and extends these observations to a contemporary cohort of patients treated with drug-eluting stents, off-pump surgery, and other recent innovations. The findings differ from a recent analysis of the Arterial Revascularization Therapy Study (ARTS), which found no difference in survival among randomized CABG and PCI patients with CKD.14 The small sample (290 patients), mild degree of CKD in randomized patients, and exclusion of patients with high-risk coronary disease may underlie the contrasting findings. Larger, randomized studies are clearly warranted. In their absence, our analysis provides reassurance that the potential benefits of CABG relative to PCI seen in the general population9 remain in the CKD population.
To our knowledge, no prior study has estimated the relative risks of ESRD after CABG and PCI in CKD patients. Our finding that short-term risk of ESRD increases after CABG is consistent with high incidence of post-CABG AKI8 in CKD patients. However, of note, absolute probability of ESRD at 3 years was only 6.8% after CABG and 5.4% after PCI. Thus, despite accelerated perioperative progression to ESRD, absolute early and long-term risks of ESRD were low for most patients who survived and remained dialysis independent throughout follow-up. These probabilities also compare favorably with the roughly 2% to 3% annual incidence of ESRD observed in a recent analysis of unselected Medicare patients with CKD.15
Of note, overall incidence of ESRD was more than 4 times lower than incidence of death. Similarly, despite a higher risk of death and ESRD during the first 3 post-procedural months, long-term risk of the combined outcome was significantly lower after CABG than after PCI. Our results thus suggest that CABG is associated with better overall outcomes than PCI in CKD patients. Our data suggest that CABG is the preferred revascularization procedure for elderly patients with CKD; however, PCI might be favored if the focus is short-term mortality and maximizing avoidance of ESRD.
Strengths of our study include a large cohort, extensive adjustment for comorbidity, and a nationally representative sample. Limitations should also be noted. Selection bias for choice of revascularization procedure may have occurred in this retrospective observational study. Administrative data were used, and clinical information such as left-ventricular ejection fraction, coronary angiographic findings, and functional class were not available. We were unable to estimate glomerular filtration rate, and therefore we cannot rule out the possibility that differences in the severity of CKD between the PCI and CABG groups could partly account for the observed differences in outcomes, particularly for progression to ESRD. However, previous studies have demonstrated high specificity for advanced CKD when diagnostic codes are used to define the presence of CKD, and it is likely that the majority of patients in both groups had at least moderately impaired renal function with a high risk of progression to ESRD.16 Therefore, differences in the severity of CKD between the PCI and CABG groups large enough to qualitatively modify the observed associations with death or ESRD are unlikely. However, additional studies in cohorts with information on baseline glomerular filtration rate are clearly warranted. Several baseline factors such as age and number of diseased vessels were unequally distributed between treatment groups. We also lacked data on use of renal- or cardio-protective medications. Although multivariable models and sensitivity analyses provided consistent results, we cannot rule out the possibility of residual confounding. Lastly, the study population was limited to patients eligible for Medicare and patients undergoing outpatient PCI (accounting for 95.4% of all PCIs), and the results may not be generalizable to younger CKD patients or to patients eligible for outpatient revascularization.
In conclusion, we compared outcomes of CABG and PCI in elderly patients with CKD. We found that absolute incidence of ESRD is much lower than incidence of death, and that long-term risks of death or combined death and ESRD are lower following CABG. In contrast, overall risk of ESRD is higher after CABG (and attributable to the first 3 postoperative months). These findings will allow CKD patients and their physicians to better assess risks of critical outcomes and incorporate them into clinical decisions before proceeding with coronary revascularization, and they have important implications for patient care.
Supplementary Material
Acknowledgments
Data for this analysis were provided by the United States Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government. The authors thank USRDS colleagues Shane Nygaard, BA, for manuscript preparation and Nan Booth, MSW, MPH, ELS, for manuscript editing.
Funding Sources
This study was performed as a deliverable under Contract No. HHSN267200715003C (National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland), Dr. Herzog Principal Investigator. Dr. Charytan was supported by the American Society of Nephrology (Carl S. Gottschalk Award) and NIDDK 5R21DK089368-02.
Footnotes
Disclosures
None.
References
- 1.Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 3.Collins AJ, Li S, Gilbertson DT, Liu J, Chen SC, Herzog CA. Chronic kidney disease and cardiovascular disease in the Medicare population. Kidney Int. 2003;64(Suppl 87):S24–31. doi: 10.1046/j.1523-1755.64.s87.5.x. [DOI] [PubMed] [Google Scholar]
- 4.Joki N, Hase H, Nakamura R, Yamaguchi T. Onset of coronary artery disease prior to initiation of haemodialysis in patients with end-stage renal disease. Nephrol Dial Transplant. 1997;12:718–723. doi: 10.1093/ndt/12.4.718. [DOI] [PubMed] [Google Scholar]
- 5.Chertow GM, Normand SL, McNeil BJ. “Renalism”: inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency. J Am Soc Nephrol. 2004;15:2462–2468. doi: 10.1097/01.ASN.0000135969.33773.0B. [DOI] [PubMed] [Google Scholar]
- 6.Bravata DM, Gienger AL, McDonald KM, Sundaram V, Perez MV, Varghese R, Kapoor JR, Ardehali R, Owens DK, Hlatky MA. Systematic review: the comparative effectiveness of percutaneous coronary interventions and coronary artery bypass graft surgery. Ann Intern Med. 2007;147:703–716. doi: 10.7326/0003-4819-147-10-200711200-00185. [DOI] [PubMed] [Google Scholar]
- 7.Yeo KK, Li Z, Yeun JY, Amsterdam E. Severity of chronic kidney disease as a risk factor for operative mortality in nonemergent patients in the California coronary artery bypass graft surgery outcomes reporting program. Am J Cardiol. 2008;101:1269–1274. doi: 10.1016/j.amjcard.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Chertow GM, Lazarus JM, Christiansen CL, Cook EF, Hammermeister KE, Grover F, Daley J. Preoperative renal risk stratification. Circulation. 1997;95:878–884. doi: 10.1161/01.cir.95.4.878. [DOI] [PubMed] [Google Scholar]
- 9.Hannan EL, Racz MJ, Walford G, Jones RH, Ryan TJ, Bennett E, Culliford AT, Isom OW, Gold JP, Rose EA. Long-term outcomes of coronary-artery bypass grafting versus stent implantation. N Engl J Med. 2005;352:2174–2183. doi: 10.1056/NEJMoa040316. [DOI] [PubMed] [Google Scholar]
- 10.Fine J, Gray RJ. A proportional hazards model for the subdistribiton of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 11.Ohtake T, Kobayashi S, Moriya H, Negishi K, Okamoto K, Maesato K, Saito S. High prevalence of occult coronary artery stenosis in patients with chronic kidney disease at the initiation of renal replacement therapy: an angiographic examination. J Am Soc Nephrol. 2005;16:1141–1148. doi: 10.1681/ASN.2004090765. [DOI] [PubMed] [Google Scholar]
- 12.Charytan D, Mauri L, Agarwal A, Servoss S, Scirica B, Kuntz RE. The use of invasive cardiac procedures after acute myocardial infarction in long-term dialysis patients. Am Heart J. 2006;152:558–564. doi: 10.1016/j.ahj.2006.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reddan DN, Szczech LA, Tuttle RH, Shaw LK, Jones RH, Schwab SJ, Smith MS, Califf RM, Mark DB, Owen WF., Jr Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol. 2003;14:2373–2380. doi: 10.1097/01.asn.0000083900.92829.f5. [DOI] [PubMed] [Google Scholar]
- 14.Ix JH, Mercado N, Shlipak MG, Lemos PA, Boersma E, Lindeboom W, O’Neill WW, Wijns W, Serruys PW. Association of chronic kidney disease with clinical outcomes after coronary revascularization: the Arterial Revascularization Therapies Study (ARTS) Am Heart J. 2005;149:512–519. doi: 10.1016/j.ahj.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Foley RN, Murray AM, Li S, Herzog CA, McBean AM, Eggers PW, Collins AJ. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol. 2005;16:489–495. doi: 10.1681/ASN.2004030203. [DOI] [PubMed] [Google Scholar]
- 16.Winkelmayer WC, Schneeweiss S, Mogun H, Patrick AR, Avorn J, Solomon DH. Identification of individuals with CKD from Medicare claims data: a validation study. Am J Kidney Dis. 2005;46:225–232. doi: 10.1053/j.ajkd.2005.04.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


