Abstract
Side-to-side differences in lower extremity biomechanics may be predictive of increased risk of lower extremity injuries in athletes. The purpose of this report is to provide field testing methodology for tests designed to isolate lower extremity asymmetry and to demonstrate the potential for these tests to provide reliable measures. Six athletes (3 females, 3 males), were tested on two consecutive days for activities incorporated into a replicated NFL combine setting. VHP and jump height were measured on a portable force platform as athletes performed maximum effort hops for 10 seconds. The MAT test incorporates two 90° single leg cuts during the trial and was measured as total time for completion. Intraclass correlations (within ICC [3,k], between: ICC [3,1]) were calculated. The VHP test had good to excellent within session reliability for peak power of both the right (ICC = 0.942) and left (ICC = 0.895) sides. Jump height showed excellent within session reliability for both the right (ICC = 0.963) and left (ICC = 0.940) sides. The between session reliability for peak power between jumps was good for the right (ICC = 0.748) and left (ICC = 0.834) sides. Jump height showed good to excellent between session reliability on the right (ICC = 0.794) and left (ICC = 0.909) sides. The MAT test also showed good reliability between days (ICC = 0.825). The results indicate that the VHP test provides reliable assessment of both within and between session jump height and power production. The MAT test also provides good reliability between testing days. Both the VHP test and the MAT test may be useful for clinicians to identify the presence of lower limb asymmetry and potential injury risk factors in athletic populations.
Keywords: functional test, vertical hop test, modified agility T-test, injury prevention
INTRODUCTION
Presently, over seven million athletes participate in organized high school varsity sports.(31) An estimated 380,000 athletes participate in intercollegiate sports, and millions of other athletes of all age levels are participating recreationally. (1) With such a large number of children, adolescents and adults participating in a wide variety of physically demanding activities, sports injuries are a major concern among athletes, athletic organizations, and health care providers. Appropriate diagnosis and treatment following injury are essential to return an athlete quickly and safely to sports. However, before an athlete returns, it is important to determine their level of readiness to meet the functional demands of the sport with minimal risk of re-injury or compensatory injury. (29)
The majority of sports injuries occur in the lower extremities, (8, 10, 11, 17) usually during jumping and cutting maneuvers. (4, 10, 26, 27, 33) Lower extremity asymmetries in strength or functional abilities may be related to an increased risk for lower extremity injury in athletic populations. (15, 20, 29, 32) If these asymmetries in side-to-side mechanics of running, cutting, jumping and landing persist after rehabilitation from a lower extremity injury, the athlete’s risk for injury may be increased for both the rehabilitated and contra-lateral limb. (3, 21, 36, 40) Diagnostic tests that can be used to identify side-to-side functional differences may be useful for the determination of an athlete’s readiness to safely return to sports following a lower extremity injury. (28, 29, 36) Moreover, functional performance tests that measure lower extremity asymmetry may help identify healthy athletes who are at increased risk for lower extremity injury. (15, 20, 32)
Many current functional assessment tests rely on subjective visual evaluations for a general analysis of movement. However, functional tests for evaluation of an athlete’s ability to safely participate in sports should include objective, valid, reliable measurements of sports specific movements. (6, 9, 16, 28, 29, 36) Tests that measure dynamic tasks during cutting and jumping activities are important to assess power, strength, landing kinetics and coordination during high-risk activities. (29) However, a test that objectively measures single leg hop power or the difference between single limb cutting maneuvers was not found in the published literature. Reliable, objective, sports-related functional assessment tools must be developed and utilized for the evaluation of the effectiveness and progression of rehabilitation protocols, determination of readiness to return to sport, (28, 29) and to identify athletes who may be at increased risk for injury. (15, 16) The purpose of this report is to provide field testing methodology for tests designed to isolate lower extremity asymmetry and to demonstrate the potential for these tests to provide reliable measures.
METHODS
Approach to the Problem
The current methodological report provide and approach to apply objective field testing methodology with functional tests designed to isolate lower extremity asymmetry and to demonstrate the potential for these tests to provide reliable measures. These data were collected in a large scale 2-day field setting designed to replicate NFL combine testing procedures. Quantitative measurements, such as the described functional assessment can be beneficial to identify preseason asymmetries that may be predictive of injury or reinjury risk in athletes.(14)
Subjects
Six athletes (3 males, 3 females) were tested on two consecutive days. Informed written consent was obtained from subjects and approved by the Institutional Review Board. After the informed consent was obtained, height and weight were measured and recorded. A questionnaire was utilized to determine prior history of knee injury. Two of the female subjects had ACL reconstructions at least two years prior to testing; one subject had a unilateral ACL reconstruction and the other had bilateral ACL reconstructions. Subjects reported recreational involvement in basketball, football, running, and/or hockey. No subjects reported any current injuries and all were currently out of season for their preferred sporting activities.
Procedures
Subjects performed two functional tasks (VHP and MAT tests) in a local high school gymnasium. Before testing, all subjects were instructed how to perform the two tests, followed by a demonstration by the same researcher. If a task was not performed according to instructions or data was unable to be recorded, the subject immediately stopped and rested, and the test was repeated. After the test, subjects were given 2 minutes to recover. This recovery was given between VHP jumping sets, MAT runs, and when transferring between tests.
The VHP test was measured on a portable force platform (Figure 1; Accupower AMTI, Watertown, MA) and recorded with AccuPower Software (Frappier Accleration, Fargo ND). Subjects were instructed to repeatedly hop on one leg “as high as possible while remaining under control” for ten seconds (Figure 2). The start leg was determined by random selection and the subject balanced on the leg until the subjects were given a cue by the investigator to begin the hopping task. The jump time, force upon landing, and power during take-off was measured and recorded during each 10 second VHP test. If a subject did not fully contact the force plate, the trial was terminated and the test was repeated. After the subject completed testing on one leg, the test was then repeated on the opposite leg.
Figure 1.
Portable platform with subject in testing position.
Figure 2.

An athlete performing the vertical hop power (VHP) test. The athlete jumped for 10 seconds, and the first three consecutive hops that reached at least 70% of the initial jump height were recorded. (For subject safety, the force platform was surrounded by a wooden step level to the force plate height to increase the surface area for jumps. If a subject landed on the wooden step the test was immediately stopped and new trial was performed.)
The MAT test (Figure 3) was developed from the standard T-test (Figure 4) in order to evaluate lower extremity side-to-side differences in cutting and running maneuvers. The T-test is a timed performance test frequently utilized for sports that require quick starts, dynamic changes in direction, and efficient movement. However, the standard agility T-test combines left and right directional changes. While this is functionally ideal for individuals who require cutting from both sides, it is not useful to evaluate and compare a potential unilateral deficit. Therefore, we modified the agility T-test to include cuts and shuffles to only one side. (29) The start leg for the MAT test was randomly assigned. The subject was initially guided through the course by the primary investigator, emphasizing the importance of performing a shuffling movement and not to run or use crossover steps during the lateral movement portions of the test. The subjects informed the investigator when they were ready to begin the test. All trials were electronically timed with a stopwatch. After the subjects felt they had an adequate rest (approximately 2 minutes), the other direction was tested. The total time was recorded for each leg. Only one trial was performed per leg.
Figure 3.
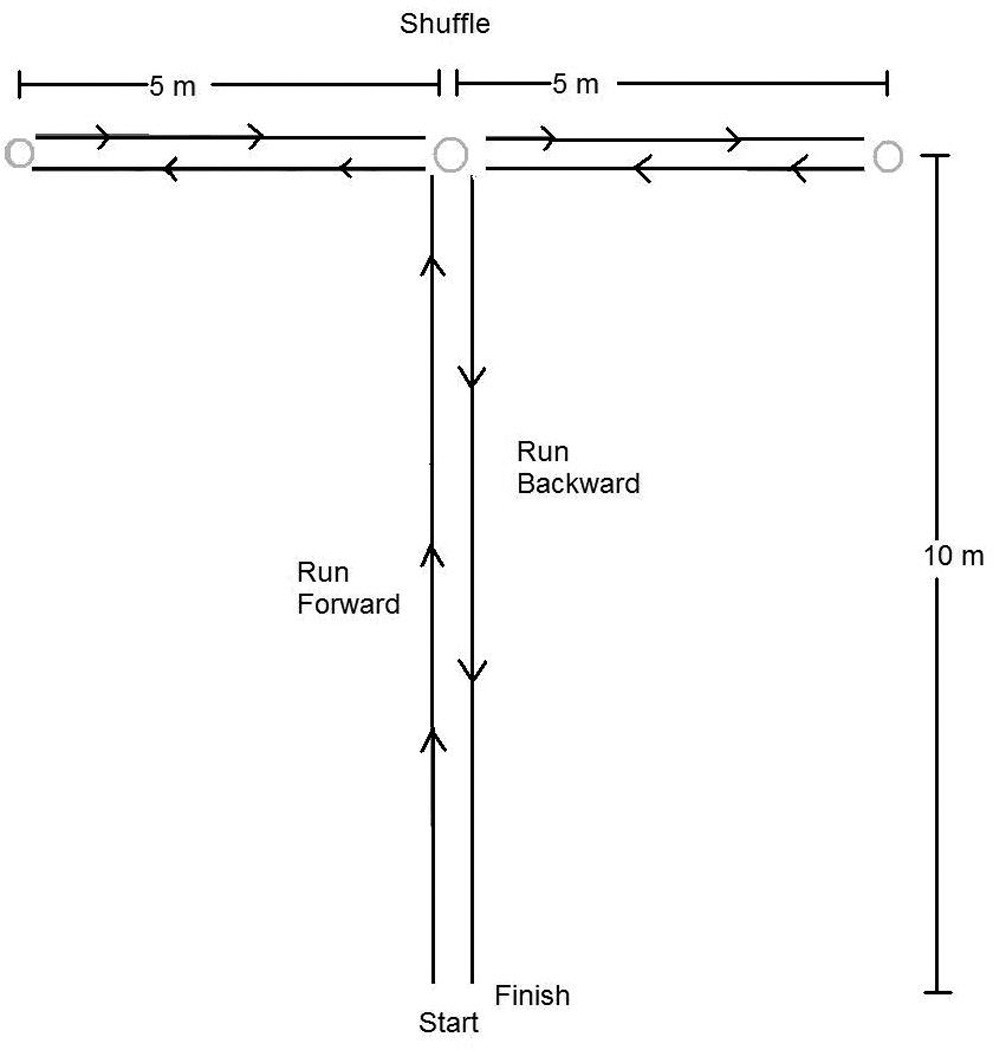
In the agility T-test, a subject runs 10 meters forward before making a perpendicular cut. The subject then shuffles 5 meters left, reaches a cone, shuffles 10 meters right, reaches another cone, and then shuffles 5 meters left. The subject then makes another perpendicular cut and ends the test running 10 meters backwards. (Pauloe, 1996)
Figure 4.
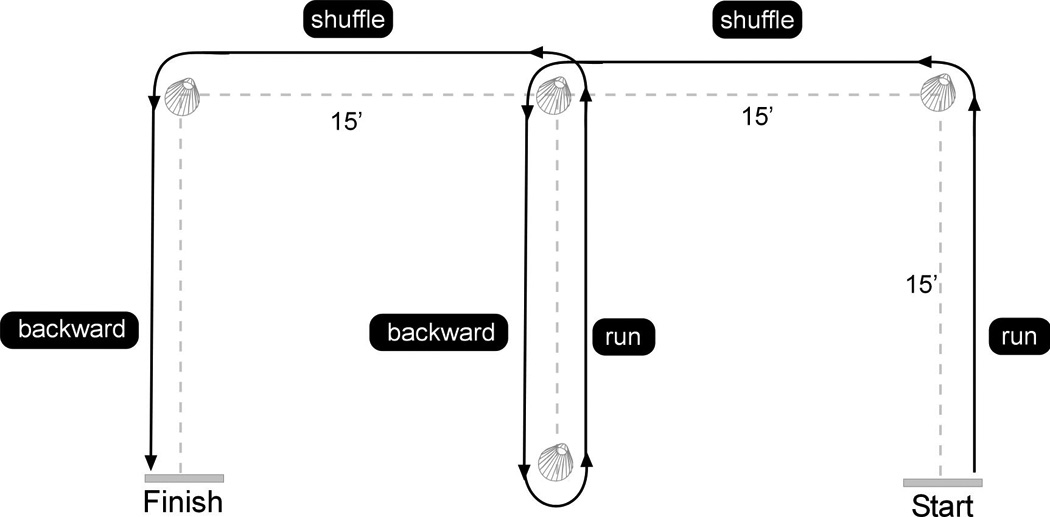
A diagram of the modified agility T-test (MAT). The subject starts at one of the bottom side cones and runs forward 15 meters. The subject makes a perpendicular cut at the cone and shuffles for another 15 meters. At the following cone, the subject runs around it and shuffles back 15 meters. Upon reaching the bottom center cone, the subject runs forward and then when they are back at the center top cone, shuffles for 15 more meters. The subject runs backward 15 meters for the finish. The test starts from one bottom side cone and then the other direction is tested by running the pattern in reverse.
Statistical Analyses
The VHP and MAT tests were performed within the two testing days, evaluating the left and right sides separately. Additionally, the VHP was compared between sessions. Since fatigue would likely affect the results of multiple trials of the VHP test, intrasession results were calculated between three of the jumps performed in one trial. For both the power and jump height of the VHP test, the first three consecutive hops that reached at least 70% of the jump height of the initial jump were evaluated for reliability. For intersession results, the first three consecutive hops that reached at least 70% of the initial jump of the first day were compared to the first three jumps that met the same criteria on the second day. Means and standard deviations were calculated from the data collected for each test and intraclass correlation coefficients (within ICC [3,k], between: ICC [3,1]) were calculated with statistical software. ICC values below 0.4 were reported as poor, from 0.4 to 0.75 were fair to good, and greater than 0.75 were considered excellent.(38)
RESULTS
The mean age of the subjects was 20.8 ± 3.8 years. The subjects weighed 68.9± 43.3 kilograms and measured 172.21 ± 9.12 centimeters in height. The mean power measured during the VHP test was 28.05 ± 3.58 Watts in this population. The mean jump height measured during the VHP test was 13.06 ± 3.04 cm (Table 1). Separately, the left mean power was 28.47 ± 3.75 Watts and the right was 27.62 ± 3.40 Watts. The left mean jump height was 13.08 ± 2.88 cm and the right was 13.04 ± 3.23 cm.
Table 1.
Subject mean values were recorded for both the VHP and MAT test for both the left and right side. The jump height and power upon landing were recorded for the VHP test. The MAT test was measured in the time necessary to complete the course.
| Left | Right | |
|---|---|---|
| Power (Watt) | 28.47 ± 3.75 | 27.62 ± 3.40 |
| Height (cm) | 13.08 ± 2.88 | 13.04 ± 3.23 |
| MAT (seconds) | 9.63 ± 0.59 | 9.55 ± 0.57 |
The VHP test had excellent within-session reliability for peak power of both the right (ICC = 0.942) and left (ICC = 0.895) sides. Jump height showed excellent within session reliability for both the right (ICC = 0.963) and left (ICC = 0.940) sides.
The between session reliability for peak power between jumps was good for the right (ICC = 0.748) and left (ICC = 0.834) sides. Jump height showed excellent between session reliability on the right (ICC = 0.794) and left (ICC = 0.909) sides.
The mean time to complete the MAT test in this population was 9.59 ± 0.57 seconds. The subjects performed the right MAT test in a mean time of 9.55 ± 0.57 seconds and the left MAT test in a mean of 9.63 ± 0.59 seconds. The MAT test also showed excellent reliability between days (ICC = 0.825).
DISCUSSION
The purpose of this report is to provide objective field testing methodology for tests designed to isolate lower extremity asymmetry and to demonstrate the potential for these tests to provide reliable measures. Quantitative measurements, such as functional assessment tests, can be used to document the progression of a patient’s strength, tolerance, and performance abilities during rehabilitation. (5, 29, 32, 36) Highly reliable functional assessment tests are required to compare results from multiple testing sessions during the progression of rehabilitation protocols. The current findings indicate that the VHP and MAT tests provide good to excellent reliability as lower extremity functional assessment tests. One of major hypotheses was accepted, as the VHP and the MAT tests provide high within, but not between session test-retest reliability (ICC > 0.75) in athletes tested. These tests may be useful measures of determining an athlete’s readiness to return to sport following lower extremity injury.
Athletes who have experienced a significant lower extremity injury such as an ACL rupture are likely at an increased risk of injury for both the injured and contralateral limbs. (2, 34, 39, 40) Paterno et al. demonstrated that female athletes who have completed rehabilitation and returned to sports following ACL reconstruction continued to have significant asymmetries in landing, cutting, and jumping over two years after surgery. (36) Mattacola et al. and Kobayashi et al. found that significant asymmetry in strength measures were present 18 months after ACL reconstruction. (22, 25) Since side-to-side asymmetries may increase risk for injury in healthy subjects, (15) residual side-to-side deficits may be important risk factors to consider before allowing an athlete to return to sports activities and should be targeted during the rehabilitation process.(22, 25, 29, 36) Functional assessment tests may help identify deficits in strength, coordination, landing kinetics and power that may increase an athlete’s risk of injury when returning to sports activities. (5, 19, 22, 25, 29, 32, 36)
Current functional assessment tests, such as performance during shuttle run tests and force measurements during landing from a jump or side step tasks may not effectively evaluate movement performance or contributions of a single limb.(6, 16, 18, 19, 29, 35) Functional hop tests such as the single leg hop, cross-over hop, triple hop, and timed hop have been used to evaluate ACL injury rehabilitation progress. (32) However, many of these functional hop tests have a low sensitivity and specificity for determining lower extremity asymmetries (16) and these movements do not take into account other high risk multi-planar movements, such as perpendicular cutting and challenging lateral motions.(7, 29) Thus, additional tests may be required to further evaluate the functional readiness of an athlete to return to sport following ACL reconstruction or other lower extremity injury.
The VHP and MAT tests used in this study may provide alternative methods to evaluate lower extremity symmetry during functionally demanding tasks. In the past, power hops on a force plate and functional hop tests for subjective analysis of lower extremity function have been used to evaluate single limb symmetry.(29, 32) However, in sporting activities, athletes must make multiple single footed ground contacts safely, while controlling the landing forces and take-off power. Therefore, a VHP test was developed in order to integrate these parameters into a functional assessment test. At the same time, the MAT test was developed to evaluate perpendicular cutting tasks. Pauole et al. reported that the T-test (Figure 4), typically used in football conditioning, is a useful tool for determining sports related measures of speed, power, and agility.(37) The T-test incorporates perpendicular cuts in both right and left directions during the timed test. In order to identify limb function asymmetries, the T-test was modified to isolate right and left directional cuts into two different test measures (Figure 3).
Both the VHP and MAT tests are challenging tasks that require sufficient strength and neuromuscular control. While these tests may be excellent tools for evaluating patient progress following injury and readiness to return to sport, using a single test in isolation may not adequately simulate all of the challenging movements an athlete may encounter on the playing field. Thus, incorporation of several different types of functional assessment tests are important when evaluating an athlete’s readiness to return to sport.(29)
Clinicians should be especially aware of the possible gap between an athlete’s perceived versus actual functional readiness to return to sport.(29) Objective, quantitative functional assessment tests, such as the VHP and MAT, may help clinicians justify why sports restriction may be important, despite an athlete’s perceived readiness to return to sport. At the same time, fear of re-injury is a major concern of many athletes and their fear may hinder performance and return to sports activity. (23) Kvist and colleagues reported that 24% of athletes who sustained ACL injury did not return to their pre-injury level of activity due to fear of re-injury.(23) Functional assessment tests may help athletes gain confidence in their rehabilitated limbs, as quantitative measures allow the athlete to see progressive improvement during the rehabilitation process and show the athlete that they are within sufficient ranges of function compared to their non-injured limb before returning to sport.
Functional assessment tests may also be useful as pre-screening tools to identify risks for lower extremity injury, particularly tools that identify lower extremity asymmetry. Hewett and colleagues prospectively measured biomechanical factors predictive of ACL injury in healthy female athletes. (15) Uninjured athletes who later sustained an ACL injury after biomechanical testing demonstrated significant side-to-side differences in knee load compared to control athletes. Side-to-side knee abduction moment was 6.4 times greater in athletes who sustained ACL injury compared to control athletes. In addition, knee abduction moments predicted ACL injury with high sensitivity and specificity.(15) If effective screening tools can be developed to identify athletes at risk for potential lower extremity injury, these at risk athletes can be placed in injury prevention programs.(12, 13, 24, 30)
PRACTICAL APPLICATIONS
Functional assessment tests that measure functional ability provide clinicians with useful tools to monitor the rehabilitation progress of athletes. The VHP test and the MAT tests are objective, quantitative, and reliable functional field assessment tests that may help clinicians evaluate patient rehabilitation progress and readiness to return to sport after lower extremity injury. The VHP and MAT tests may also be useful on-site screening tools to help identify athletes who may be at increased risk for lower extremity injury. Future studies should evaluate the validity, sensitivity, and specificity of the MAP and VHP test for identifying lower extremity asymmetries in patients recovering from lower extremity injury and in healthy populations. If the VHP and MAT tests are found to be valid, sensitive, and specific measures for identifying lower extremity asymmetries, these tests may be useful tools to determine the readiness of an athlete to safely return to sport following injury, to predict risk for lower extremity injury and guide prevention programs.
ACKNOWLEDGEMENTS
The authors would like to acknowledge funding support from NFL Charities.(14) The authors would like to thank St. Xavier High School, especially John Brehm and Michael Gordon, Boone County School District, Kentucky, especially School Superintendent Dr. Brian Blavatt, for use of the school facilities in this study.
REFERENCES
- 1.Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33:75–81. doi: 10.2165/00007256-200333010-00006. [DOI] [PubMed] [Google Scholar]
- 2.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 3.Baumhauer J, Alosa D, Renstrom A, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sport Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 4.Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 5.Brosky JA, Jr, Nitz AJ, Malone TR, Caborn DN, Rayens MK. Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:39–48. doi: 10.2519/jospt.1999.29.1.39. [DOI] [PubMed] [Google Scholar]
- 6.Cascio BM, Culp L, Cosgarea AJ. Return to play after anterior cruciate ligament reconstruction. Clin Sports Med. 2004;23:395–408. doi: 10.1016/j.csm.2004.03.004. ix. [DOI] [PubMed] [Google Scholar]
- 7.Ernst G, Moore J, VanLunen B, Ball D. Pondering plyometrics. J Orthop Sports Phys Ther. 1997;25:350–352. [PubMed] [Google Scholar]
- 8.Ferretti A, Papandrea P, Conteduca F, Mariani PP. Knee ligament injuries in volleyball players. American Journal of Sports Medicine. 1992;20:203–207. doi: 10.1177/036354659202000219. [DOI] [PubMed] [Google Scholar]
- 9.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clinical Biomechanics. 2006;21:33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Giza E, Fuller C, Junge A, Dvorak J. Mechanisms of foot and ankle injuries in soccer. Am J Sports Med. 2003;31:550–554. doi: 10.1177/03635465030310041201. [DOI] [PubMed] [Google Scholar]
- 11.Hawkins RD, Fuller CW. A prospective epidemiological study of injuries in four English professional football clubs. Br J Sports Med. 1999;33:196–203. doi: 10.1136/bjsm.33.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heidt RS, Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28:659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE, Myer GD, Ford KR, Heidt RS, Jr, Colosimo AJ, Divine JG. Pre-season Football combine testing to isolate neuromuscular deficits predictive of ACL injury and reinjury risk. Cincinnati Children's Hospital Medical Center, NFL Charities. 2007 [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR, Heidt RS, Jr, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop. 2002;402:76–94. doi: 10.1097/00003086-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311–319. [PMC free article] [PubMed] [Google Scholar]
- 18.Jamshidi AA, Olyaei GR, Heydarian K, Talebian S. Isokinetic and functional parameters in patients following reconstruction of the anterior cruciate ligament. Isokinetics and Exercise Science. 2005;13:267–272. [Google Scholar]
- 19.Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231–237. doi: 10.1016/S0736-0266(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 20.Klein KK. Asymmetries in the pelvis and legs and their implications in knee injury. Am Correct Ther J. 1970;24:93–95. [PubMed] [Google Scholar]
- 21.Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76–81. doi: 10.1177/036354659101900113. [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi A, Higuchi H, Terauchi M, Kobayashi F, Kimura M, Takagishi K. Muscle performance after anterior cruciate ligament reconstruction. Int Orthop. 2004;28:48–51. doi: 10.1007/s00264-003-0502-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:393–397. doi: 10.1007/s00167-004-0591-8. [DOI] [PubMed] [Google Scholar]
- 24.Mandelbaum BR, Silvers HJ, Watanabe D, Knarr J, Thomas S, Griffin L, Kirkendall DT, Garrett WJ. Effectiveness of a neuromuscular and proprioceptive training program in preventing the incidence of ACL injuries in female athletes: two-year follow up. Am J Sport Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 25.Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC., 3rd Strength, Functional Outcome, and Postural Stability After Anterior Cruciate Ligament Reconstruction. J Athl Train. 2002;37:262–268. [PMC free article] [PubMed] [Google Scholar]
- 26.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKay GD, Goldie PA, Payne WR, Oakes BW, Watson LF. A prospective study of injuries in basketball: a total profile and comparison by gender and standard of competition. J Sci Med Sport. 2001;4:196–211. doi: 10.1016/s1440-2440(01)80030-x. [DOI] [PubMed] [Google Scholar]
- 28.Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337–342. doi: 10.1007/s001670000143. [DOI] [PubMed] [Google Scholar]
- 29.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after Anterior Cruciate Ligament Reconstruction: Criteria Based Progression Through the Return to Sport Phase. J Orthop Sports Phys Ther. 2006;36:385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 30.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13:71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 31.NFHS. High School Participation Survey. Indianapolis: National Federation of State High School Associations; 2007. [Google Scholar]
- 32.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 33.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 34.Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196–200. doi: 10.1177/03635465010290021301. [DOI] [PubMed] [Google Scholar]
- 35.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Biomechanical Limb Asymmetries in Female Athletes 2 Years Following ACL Reconstruction. Clin J Sport Med. 2007;17:258–262. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 36.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17:258–262. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 37.Pauole K, Madole K, Garhammer J, Lacourse M, Rozene R. Reliability and Validity of the T-Test as a Measure of Agility, Leg Power, and Leg Speed in College-Aged Men and Women. Journal of Strength and Conditioning Research. 2000;14:443–450. [Google Scholar]
- 38.Portney LG, Watkins MP. Foundations of Clinical Research. Norwalk, CT: Appleton & Lange; 2000. [Google Scholar]
- 39.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 40.Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]


