Abstract
This study examined the latent structure of psychiatric disorders in a sample with a high prevalence of PTSD. A series of confirmatory factor analyses tested competing models for the covariation between SCID diagnoses among 1,325 Vietnam veterans. The best fitting solution was a three-factor model that included two correlated internalizing factors: anxious-misery, defined by PTSD and major depression, and fear, defined by panic disorder/agoraphobia and obsessive-compulsive disorder. The third factor, externalizing, was defined by antisocial personality disorder, alcohol abuse/dependence, and drug abuse/dependence. Both substance-related disorders also showed significant, albeit smaller, cross-loadings on the anxious-misery factor. These findings shed new light on the structure of psychiatric comorbidity in a treatment-seeking sample characterized by high rates of PTSD.
Traumatic stress is a risk factor for a wide array of psychiatric disorders. Posttraumatic stress disorder (PTSD) may be the most common syndrome to develop following trauma, but other conditions frequently co-occur with, or develop independently of it, including other anxiety disorders, unipolar depressive disorders and substance-related disorders (Breslau, Davis, Andreski, & Peterson, 1991; Breslau, Davis, Peterson & Schultz, 2000; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Kulka et al., 1990). Behavior genetic studies suggest that common genetic factors may account for the co-occurrence of PTSD with other disorders including alcohol and drug dependence (Xian et al., 2000), nicotine dependence (Koenen et al., 2005), major depression and dysthymia (Koenen et al., 2003), generalized anxiety disorder and panic disorder (Chantarujikapong et al., 2001). However, research has yet to achieve a consensus about the number and/or definition of the factors that underlie these patterns of comorbidity. The primary aim of this study was to elucidate this latent structure in a large and carefully assessed sample of combat veterans with a high prevalence of PTSD.
One well-established model of co-occurring mental disorders that may be relevant to the understanding of the structure of posttraumatic psychopathology proposes that patterns of behavioral disturbance and psychiatric symptoms cohere along latent dimensions termed externalizing (EXT) and internalizing (INT). This model, rooted in a tradition of research on childhood behavior disorders (Achenbach & Edelbrock, 1978, 1984), has recently come to the fore in the adult psychopathology literature as the result of a series of influential factor-analytic studies on the latent structure of adult mental illness (Kendler, Prescott, Myers, & Neale, 2003; Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Krueger, 1999; Krueger, Caspi, Moffitt & Silva, 1998; Krueger, Chentsova-Dutton, Markon, Goldberg, & Ormel, 2003; Krueger, McGue, & Iacono, 2001; Vollebergh et al., 2001). Findings of these studies suggest that the alcohol- and drug-related disorders and antisocial personality disorder load on an EXT dimension characterized primarily by problems in the domain of impulsivity, whereas the unipolar mood and anxiety disorders fall on an INT dimension defined largely by heightened negative emotionality. In several studies, the latter has been subdivided into correlated factors termed “anxious-misery” (defined by major depression, dysthymia, generalized anxiety disorder) and “fear” (comprised of panic and phobic disorders; Cox, Clara, & Enns, 2002; Krueger, 1999; Vollebergh et al., 2001; Slade & Watson, 2006). This basic structure has demonstrated invariance across sex, time, and multiple samples drawn at random from a larger one (Kendler et al., 2003; Krueger, 1999; Vollebergh et al., 2001) and may offer a useful framework for incorporating a dimensional component into future editions of the Diagnostic and Statistical Manual (DSM; APA).
Emerging evidence suggests that the INT/EXT model may also be relevant to our understanding of the heterogeneity of posttraumatic psychopathology (Miller, Greif, & Smith, 2003; Miller, Kaloupek, Dillon, & Keane, 2004; Miller & Resick, 2007). Through a series of cluster analytic studies of personality inventories completed by individuals with PTSD and other disorders, Miller and colleagues (2003, 2004, 2007) have found and replicated evidence of INT and EXT subtypes in both male veteran and female civilian samples. Summarizing across these studies, one subtype, termed “externalizing”, was characterized by elevated levels of anger and aggression, substance-related disorders, antisocial and borderline personality disorder features, and personality inventory profiles defined by high disconstraint coupled with high negative emotionality. In contrast, the “internalizing” subtype was characterized by high rates of comorbid major depression and panic disorder, schizoid and avoidant personality disorder features, and personality profiles defined by high negative emotionality combined with low positive emotionality. Similar patterns that might now be interepreted as reflecting individual differences in internalizing and externalizing processes were described in earlier cluster analytic studies of U.S. and Australian veterans with PTSD (Hyer, Davis, Albrecht, Boudewyns, Woods, 1994; Forbes et al., 2003; Piekowski, Sherwood, & Funari, 1993). Together, these findings suggest that the INT/EXT model be may be a useful heurisitic for studying the structure of posttraumatic psychopathology. However, while cluster analysis is a reasonable starting point for classifying qualitatively different subgoups of individuals, it is not well suited for examining facets of psychopathology that are conceptualized as fundamentally dimensional in nature. Thus, a primary objective of this study was to test competing models for the latent structure of posttraumatic psychopathology using confirmatory factor analysis.
Three prior published studies have employed factor analysis to examine the relationship of PTSD to hypothesized INT and EXT dimensions of psychopathology. In the first, Cox et al. (2002) performed a principal components analysis on lifetime prevalence data from the National Comorbidity Survey (Kessler et al., 1994) and found that PTSD loaded rather weakly on Anxious-Misery (r = .39) but not on Fear or EXT in a three-factor (Fear, Anxious-Misery, and EXT) solution. This pattern was replicated in 12-month prevalence data and indicated that PTSD may share more common variance with disorders defined by anhedonic mood and anxious rumination than with those characterized primarily by pathological fear (e.g., panic disorder and phobias) or externalizing. In the second study, Kessler et al. (2005) performed an exploratory factor analysis on 12-month prevalence data from the National Comorbidity Survey Replication and found evidence for a two-factor (INT/EXT) solution with PTSD loading again on INT but not EXT. In the third one, Slade & Watson (2006) performed confirmatory factor analyses on 12-month prevalence data from the Australian National Survey of Mental Health and Wellbeing (N = 10,641) and found that PTSD loaded strongly on Anxious-misery (r = .83) but not on Fear or EXT in a three-factor solution.
Conclusions from these studies were limited by two concerns. First, although representative of the general population, the base rates of PTSD were rather low in these studies (7.8% for lifetime in the first, 3.7% for 12-month in the second, 1.3% for 12-month in the third). In the present study, we wondered whether the INT/EXT factor structure would replicate in a sample with higher rates of diagnosed psychopathology and how the pattern of factor loadings for PTSD might change. Only one prior study has examined this question in a treatment-seeking sample. In that one, which did not include PTSD in the analysis, Krueger (1999) examined data from a subsample (n = 251) of the National Comorbidity Survey but reported equivocal findings regarding the relative fit of 2, 3, or 4 factor solutions. A second limitation of prior studies that have examined the relationship of PTSD to INT/EXT was that two out of three of them employed analyses that do not permit a priori specification of the patterns of relationships between observed measures and latent variables so they were unable to test competing models/hypotheses for the associations between disorders. Furthermore, no prior study has focused on testing alternative representations of the relationship of PTSD to these dimensions.
This study was designed to address these limitations in two ways. First, we examined data drawn from a large sample of Vietnam veterans receiving services in the U.S. Department of Veterans Affairs Healthcare System (VA) who had a high rate of combat-related PTSD and other disorders. Second, we performed a sequence of hypothesis-driven model testing using confirmatory factor analysis that permitted comparison of alternative models for the relationship of PTSD to latent dimensions of psychopathology. We began by examining a one-factor general disturbance model in which all disorders were specified as indicators of a single latent psychopathology dimension. Next, we evaluated variations of the two-factor (INT/EXT) and three-factor (FEAR, anxious-misery [ANX-MIS], and EXT) models suggested by prior research. In each of these models, major depressive disorder, panic disorder/agoraphobia, and obsessive-compulsive disorder were conceptualized as indicators of INT, whereas alcohol abuse/dependence, substance abuse/dependence, and antisocial personality disorder were defined as indicators of EXT. In one variation, PTSD loaded exclusively on INT (two-factor model; cf. Kessler et al., 2005) or ANX-MIS (three-factor model; cf. Cox et al., 2002). In a second variation, suggested by prior evidence for high rates of comorbidity between PTSD and disorders of both the INT and EXT domain, PTSD cross-loaded on ANX-MIS and EXT (Breslau et al., 1991, 2000; Kessler et al., 1995; Kulka et al., 1990; Miller et al., 2003, 2004, 2007; Xian et al., 2000).
We also tested alternative representations of the relationship of alcohol and drug abuse/dependence to the hypothesized INT and EXT latent factors. Recent research linking substance-related disorders to an EXT factor defined also by adult and childhood antisocial behavior and the personality dimension disconstraint (e.g., Krueger et al., 2001) contrasts with another body of research demonstrating strong associations between these disorders and psychopathology in the domain of INT. For example, research has shown high rates of alcohol and drug dependence in individuals with major depression (e.g., Hasin, Goodwin, Stinson, & Grant, 2005; Kendler, Heath, Neale, Kessler, & Eaves, 1993) and twin and family studies suggest that the association between these disorders may be due to a common genetic factor (Kendler et al., 1993; Lin et al., 1996; Merikangas, Risch, & Weissman, 1994). In individuals with PTSD, substance-related disorders are among the most common comorbidities (Breslau et al., 1991; Kessler et al., 1995; Kulka et al., 1990) and evidence suggests that when these disorders co-occur, PTSD tends to predate the substance abuse (Kessler, 2000; Kessler et al., 1995). The dominant explanation for this association, known as the self-medication hypothesis, posits that individuals abuse substances in an effort to reduce or control distress-related symptoms and this behavior is maintained by negative reinforcement resulting from symptom relief (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Stewart, 1996). This conceptually distinct model provided the rationale for testing alternative representations of the associations between alcohol abuse/dependence, drug abuse/dependence, and the latent factors INT and EXT. To do so, our model testing sequence evaluated the relative fit of models in which alcohol and drug abuse/dependence loaded exclusively on EXT, and two alternatives suggested by the self-medication hypothesis: In the first, alcohol abuse/dependence cross-loaded on INT (2 factor solution) or ANX-MIS (3 factor solution), in the second, alcohol abuse/dependence and drug abuse/dependence both cross-loaded on these factors.
Method
Participants
Participants were 1,325 male military veterans who served in the Vietnam theater of operations between August 1964 and May 1975 and were using health services of the VA at the time of study enrollment. Recruitment took place over a 42-month interval between 1989 and 1992 from inpatient and outpatient programs at 15 VA medical centers across the United States. As the focus of the original study was on the psychophysiological assessment of PTSD (Keane et al., 1998), individuals were excluded from participation if they (a) were taking medications that might have significantly altered their autonomic responding, (b) had any medical condition that would influence psychophysiological responses or entail undue risk for the participant, or (c) refused to refrain from the use of alcoholic beverages and illicit drugs for 24 hours prior to the evaluation as verified by urine toxicology.
Participants were predominantly Caucasian (67.4%) with honorable discharges from the military (92.0%). The majority served in the Army (62.1%), followed by the Marines (23.3%), Navy (8.5%), and Air Force (6.0%). Over half of the sample met criteria for a current (58.5%) or lifetime (71.9%) diagnosis of military-related PTSD. The mean age at first arrival in Vietnam was 20 years (SD = 3.3; range = 17-46 years). Mean education at the time of the study was 14 years (SD = 2.5 years) and mean income was $17,194 (SD = $17,502). The sample was approximately evenly split among those who were (51.7%) and were not (48.3%) currently married. Written informed consent was obtained from all participants following a complete description of the study.
Measures
Participants were assessed for current and lifetime psychiatric diagnoses with the Structured Clinical Interview for DSM-III-R (SCID; Spitzer, Williams, Gibbon, & First, 1989). Table 1 presents the base rates and inter-rater reliabilities (Kappas) for lifetime SCID-assessed diagnoses (i.e., defined as having ever met criteria for a given disorder up to the age at interview; cf. Kessler et al., 2005). All diagnostic interviews were audiotaped, and inter-rater reliability was assessed via review of 128 tapes by a second clinician and re-assessment of 36 participants by another clinician. Kappas were computed using the combined results of the two approaches (see Keane et al., 1998) and were in the moderate to excellent range. To ensure reliable estimates of covariation between disorders, we excluded one that was not reliably assessed (social phobia; kappa = .23) and several that showed very low base rates in the sample (bipolar, schizophrenia, somatoform, and dissociative disorders). Generalized anxiety disorder and simple phobia were not assessed. Following prior work, panic disorder with and without agoraphobia were combined into one variable (Brown, Chorpita, & Barlow, 1998) as were abuse and dependence for the drug and alcohol diagnoses (Kendler et al., 2003). The prevalence of use for specific drugs among individuals with a lifetime diagnosis of drug abuse/dependence was as follows: Cannabis (73%), Stimulants (42%), Opioids (42%), and Sedatives/Hypnotics/Anxiolytics (29%).
Table 1.
Prevalence Rates and Interrater Reliabilities (Kappas) for Lifetime SCID-Assessed Psychiatric Disorders
| Diagnosis | Lifetime Prevalence |
Kappa |
|---|---|---|
| Panic/Agoraphobia | 11.4% | .60 |
| Major Depression | 52.1% | .49 |
| Obsessive-Compulsive | 10.8% | .54 |
| PTSD | 71.9% | .73 |
| Alcohol Abuse/Dependence | 76.2% | .88 |
| Substance Abuse/Dependence | 58.2% | .81 |
| Antisocial Personality | 11.1% | .64 |
Statistical Analyses
Confirmatory factor analyses were performed using the Mplus software, Version 3.11 (Muthén & Muthén, 1998 - 2006). Robust Weighted Least Squares (WLSMV) estimation was used because the diagnostic variables were dichotomous and non-normally distributed. Several statistics were used as indicators of model fit (cf., Brown, 2006). First, the χ2 value provided an index of the degree to which the model reproduced the sample variances and covariances with smaller values indicative of better fit. Second, we used the Tucker-Lewis Index (TLI), or non-normed fit index, which includes a penalty function for adding freely estimated parameters that do not markedly improve fit; fit improves as TLI values approach 1.0. Third, we used the root mean square error of approximation (RMSEA) which relies on the noncentral χ2 distribution and compensates for the effect of model complexity; values less than .06 are indicative of good fit. Fourth, we used the comparative fit index (CFI) which evaluates the fit of a user-specified solution relative to a more restricted, nested baseline model; values closer to 1.0 imply good model fit. We also used the weighted root mean square residual (WRMR), an index of absolute fit similar to the standardized root mean square residual (SRMR) but adapted for use with non-normally distributed data; values below .80 are indicative of good fit. Finally, because most of the factor models were nested, when possible, more restrictive models were tested directly against less restrictive ones to identify the superior model using χ2 difference testing procedures (see Factor Model Comparisons in Table 3).
Table 3.
Fit statistics and Factor Model Comparisons for all Models Tested
| Fit Indices |
Factor Model Comparisons |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model | df | χ2 fit | RMSEA | TLI | CFI | WRMR | Models | χ2 Diff |
| 1-Factor: General Disturbance | 12 | 108.41*** | .08 | .83 | .88 | 1.89 | -- | -- |
| 2-Factor: INT & EXT | ||||||||
| (a) PTSD on INT | 11 | 33.46*** | .04 | .96 | .97 | 1.05 | 2a vs 1 | 66.26*** |
| (b) PTSD x-loads on INT and EXT |
10 | 32.68*** | .04 | .95 | .97 | 1.04 | 2b vs 2a | .41 |
| (c) PTSD on INT; ALC x- loads on INT and EXT |
10 | 29.39*** | .04 | .96 | .98 | .99 | 2c vs 2a | 4.10* |
| (d) PTSD on INT; ALC & DRUG x-load on INT and EXT |
10 | 25.75** | .04 | .97 | .98 | .88 | 2d vs 2a 2d vs 2c |
10.34** 6.04** |
| 3-Factor: Fear, ANX-MIS, & EXT | ||||||||
| (a) PTSD on ANX-MIS | 10 | 29.52*** | .04 | .96 | .98 | .93 | 3a vs 2a | 6.75* |
| (b) PTSD x-loads on ANX- MIS & EXT |
9 | 28.22*** | .04 | .95 | .98 | .91 | 3b vs 3a | 1.30 |
| (c) PTSD on ANX-MIS; ALC x-loads on ANX-MIS and EXT |
9 | 25.91** | .04 | .96 | .98 | .87 | 3c vs 3a | 3.62 |
| (d) PTSD on ANX-MIS; ALC & DRUG x-loads on ANX-MIS and EXT |
8 | 17.90* | .03 | .97 | .99 | .71 | 3d vs 3a 3d vs 3c 3d vs 2d |
11.23** 7.34** 7.02* |
Note. Best fitting model in testing sequence is model 3d. χ2 fit = chi-square goodness of fit test; RMSEA = root mean square error of approximation; TLI = Tucker-Lewis index; CFI = comparative fit index; WRMR = weighted root mean square residual; INT = internalizing; EXT = externalizing; ANX-MIS = anxious-misery; PTSD = posttraumatic stress disorder; x-loads = cross loads; ALC = alcohol abuse/dependence; DRUG = drug abuse/dependence.
p < .05.
p < .01.
p < .001.
Results
Table One lists the lifetime prevalence rates and inter-rater reliability statistics for the seven disorders examined. Tetrachoric correlations (i.e., used with binary variables) among diagnoses are listed in Table Two. Table Three lists fit statistics for each model and the results of model comparisons using χ2 difference testing. Fit indices showed that all of the two and three factor models fit the data better than the one factor, general disturbance model. Overall, the three factor models fit better than their two factor counterparts. For example, the χ2 difference test comparing model 3a with 2a showed that the three factor model with PTSD loading on ANX-MIS fit the data better than the two factor model with PTSD loading on INT. Results for models 2b and 3b suggested that allowing PTSD to cross-load on EXT did not significantly improve model fit relative to the simpler variation in which PTSD loaded exclusively on INT (2a) or ANX-MIS (3a).1 Alternative representations of the loadings of alcohol and drug disorders indicated that having alcohol cross-load on INT (2c) or ANX-MIS (3c) provided marginal improvement relative to the basic model in which it loaded exclusively on EXT (2a and 2c, respectively). However, models in which both alcohol and drug diagnoses cross-loaded showed significant improvement in fit relative to both of the non-cross-loading models (2a and 3a) and the ones in which only alcohol cross-loaded (2c and 3c).
Table 2.
Correlations between SCID-Assessed Disorders
| Diagnosis | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. PTSD | 1.0 | ||||||
| 2. MDD | .55 | 1.0 | |||||
| 3. PDA | .48 | .28 | 1.0 | ||||
| 4. OCD | .34 | .15 | .41 | 1.0 | |||
| 5. ALC | .42 | .32 | .22 | .45 | 1.0 | ||
| 6. DRG | .36 | .21 | .16 | .09 | .53 | 1.0 | |
| 7. ASPD | .07 | .08 | .05 | .18 | .39 | .31 | 1.0 |
Note. PTSD = posttraumatic stress disorder; MDD = major depressive disorder; PDA = panic disorder with or without agoraphobia; OCD = obsessive-compulsive disorder; ALC = alcohol abuse/dependence; DRG = drug abuse/dependence; ASPD = antisocial personality disorder.
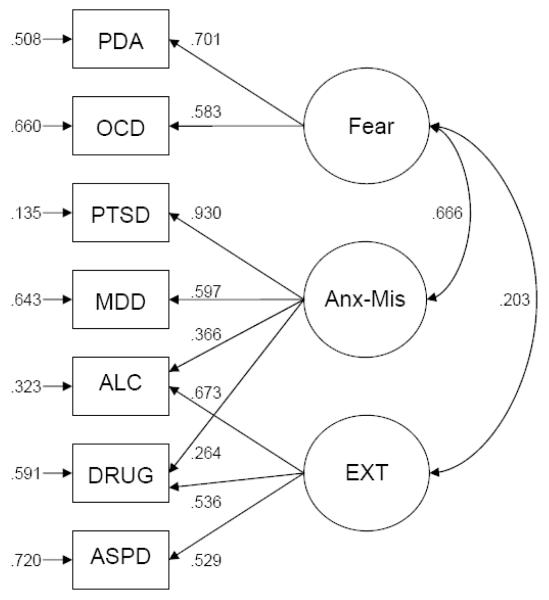
The best fitting model, shown in Figure 1, was the three factor variation in which PTSD loaded on ANX-MIS and alcohol and drug abuse/dependence both cross-loaded on ANX-MIS and EXT. The diagram illustrates several important findings. First, examination of the associations among the latent factors showed a high correlation (.67) between the anxious-misery and fear factors. Second, there was a significant but substantially smaller correlation between the Fear and EXT factors (.20), but no such association between ANX-MIS and EXT. Third, factor loadings were generally large, with two exceptions: the loadings of alcohol and drug abuse/dependence on ANX-MIS (.37 and .26, respectively), while statistically significant, were considerably smaller than their loadings on EXT (.67 and .54, respectively).
Figure 1.
Best-fitting model showing all statistically significant completely standardized parameter estimates. EXT = externalizing; SP = social phobia; OCD = obsessive-compulsive disorder; MDD = major depressive disorder; PDA = panic disorder with/without agoraphobia; PTSD = posttraumatic stress disorder; ALC = alcohol abuse/dependence; DRG = drug abuse/dependence; ASPD = antisocial personality disorder; ANX-MIS = anxious-misery.
Finally, to examine the reliability of this solution we randomly split the sample into two halves using the SPSS select random cases function and repeated the sequence of model testing on each half separately. Findings closely paralleled the results listed in Table 3. For both halves of the sample the best fitting model was the three factor variation with PTSD loading on ANX-MIS and alcohol and drug abuse/dependence cross-loading on ANX-MIS and EXT. Finally, when the grouping variable was included in an equal form analysis of the final model, change in the fit indices was minimal, χ2 = 25.84, df = 17 (p = .08), RMSEA = .03, TLI = .98, CFI = .98, WRMR = .96.
Discussion
This study tested competing models for the latent structure of posttraumatic psychopathology using data drawn from a VA treatment-seeking sample of male Vietnam veterans. Confirmatory factor analyses compared the relative fit of models that differed with respect to the number of latent factors and loadings of PTSD and substance-related disorders on them. Results showed that the best fitting solution was a three factor (Fear, ANX-MIS, EXT) variation in which PTSD loaded on ANX-MIS and the substance-related diagnoses cross-loaded on both ANX-MIS and EXT. In this model, the INT disorders bifurcated into two correlated factors, one defined by major depression and PTSD (ANX-MIS), the other by panic-agoraphobia and obsessive-compulsive disorder (Fear). These results replicate and extend findings from prior structural analyses of psychiatric comorbidity in epidemiologic samples (Cox et al., 2002; Kendler et al., 2003; Krueger, 1999; Slade & Watson, 2006; Vollebergh et al., 2001) to a VA treatment-seeking sample characterized by high rates of PTSD and comorbid disorders.
These findings suggest that PTSD may share more in common with the melancholy, apathy, and rumination of major depression than with the disabling anxiety and avoidance that is characteristic of panic disorder/agoraphobia and obsessive-compulsive disorder—a finding that is inconsistent with the current placement of PTSD in the anxiety disorders category in DSM-IV. This finding is in line with evidence from a previous study of twin brothers of Vietnam veterans which showed that (a) combat veterans with PTSD had higher rates of major depression and dysthymia than combat controls and (b) the unexposed twins of veterans with combat-related PTSD had higher rates of both disorders than the unexposed twins of combat veterans without PTSD (Koenen et al., 2003). Taken collectively, these findings suggest that the affinity between major depression and PTSD observed in this and prior structural analyses (Cox et al., 2002; Kessler et al., 2005; Slade & Watson, 2006) may reflect an endophenotypic trait or common genetic factor that confers vulnerability for the development of posttraumatic psychopathology, i.e., negative emotionality (for a review, see Miller, 2003).
The second internalizing factor, termed Fear, was defined by OCD and panic disorder. OCD has been excluded from most previous studies of this type because of its low prevalence in the general population so knowledge about its structural relationships to other disorders is limited. Three prior studies that have addressed the issue produced inconsistent results. Brown et al. (1998) reported that OCD was more highly correlated with major depression and generalized anxiety disorder than with panic disorder/agoraphobia or social phobia. In contrast, Watson (2005) and Slade and Watson (2006) found that OCD loaded primarily on a Fear factor defined also by panic disorder, agoraphobia, social phobia. The relationship between panic disorder and PTSD has been the source of similar disagreement. Some investigations have suggested that a close affinity exists between these two disorders, possibly reflecting the involvement of pathological autonomic arousal in both (Brown, Campbell, Lehman, Grisham, & Mancill, 2001), while others suggest a dissociation between them. For example, Cox et al. (2002) and Slade and Watson (2006) both reported that panic disorder loaded primarily on a Fear factor, whereas PTSD loaded on an Anxious-Misery factor as it did in the present study.
Another noteworthy finding from this study was that the best fitting model included cross-loadings of alcohol and drug abuse/dependence diagnoses on both ANX-MIS and EXT. The relative strengths of these loadings indicated that these disorders cohered primarily with the EXT factor defined also by antisocial personality disorder (as they have in prior studies using epidemiologic samples), but they also showed a significant affinity for the ANX-MIS factor defined by major depression and PTSD. In addition, alcohol abuse/dependence loaded more highly on ANX-MIS than drug abuse/dependence did. These novel findings align empirically with prior evidence of high rates of comorbid alcohol and drug abuse in individuals with major depression and PTSD and they are conceptually consistent with the aforementioned self-medication hypothesis which posits a reciprocal relationship between negative emotional distress and addictive behaviors (Baker et al., 2004; Stewart, 1996). Theses associations are also consistent with prior evidence for a stronger relationship between alcohol-related problems and symptoms in the domain of negative emotionality than between illicit drug-related problems and this dimension (Miller, Vogt, Mozley, Kaloupek, & Keane, 2006). Most importantly, these findings appear to reconcile contrasting models of comorbid substance-related disorders and seem to capture the complex relationships between these disorders and broad but distinct (INT and EXT) classes of psychopathology. The fact that similar cross-loadings have not been reported in prior analyses of data from community studies implies that there may be differences in the structure of comorbidity between epidemiologic and clinical samples (Keane & Wolfe, 1990). Stronger links between substance-related disorders and psychopathology of the INT spectrum may be evident in pathological groups in which these disorders develop secondary to a primary INT syndrome. Unfortunately, the cross-sectional data from this study precluded a direct test of this temporal hypothesis.
Conclusions from this study must be weighed against its limitations. First, the sample was composed entirely of male Vietnam veterans, which raises the question of whether similar relationships would be observed in mixed gender or female clinical samples, individuals with more recent trauma exposure, or samples defined by disorders other than PTSD. Second, the diagnostic variables that were available for analysis provided only a partial representation of the full range of common INT disorders and did not include generalized anxiety disorder, simple phobia, or social phobia. Third, to replicate methods employed in several key prior studies (e.g., Kendler et al., 2003; Kessler et al., 2005; Krueger, 1999) we focused our analyses on lifetime diagnoses. In doing so, we did not distinguish subjects with current disorders from those with temporally separate disorders over the lifespan. Additionally, patterns of comorbidity and our resulting factor structure may have been influenced by DSM diagnostic decision/hierarchy rules. These study limitations were arguably offset, however, by its strengths which included a very large and racially diverse clinical sample drawn from across the United States, a high prevalence of PTSD and comorbid psychopathology, and clinician-based diagnoses with good inter-rater reliability. Finally, this study illustrates the use of latent variable modeling to identify core psychopathological processes or endophenotypic traits that may underlie broad classes of psychopathology. It also clarifies the location of PTSD in the INT/EXT framework and demonstrates the relevance of this model to the structure of comorbidity in a help seeking clinical sample.
Acknowledgments
This research was supported by the VA Cooperative Studies Program of the Veterans Health Administration under designation CS-334 and by a VA Merit Review grant to Mark W. Miller. We are grateful to Timothy A. Brown for his comments on an early draft on the manuscript.
Footnotes
We also tested a model in which PTSD loaded on both Fear and ANX-MIS, but not EXT, and found fit indices equivalent to model 3b.
Portions were presented at the 21st Annual Meeting of the International Society for Traumatic Stress Studies, Toronto, Canada, November 3-6, 2005.
Contributor Information
Mark W. Miller, VA Boston Healthcare System, National Center for PTSD & Boston University, Departments of Psychiatry and Psychology
Jason M. Fogler, National Center for PTSD, VA Boston Healthcare System & Boston University, Department of Psychiatry
Erika J. Wolf, VA Boston Healthcare System, National Center for PTSD & Boston University, Department of Psychology
Danny G. Kaloupek, VA Boston Healthcare System, National Center for PTSD & Boston University, Department of Psychiatry
Terence M. Keane, VA Boston Healthcare System, National Center for PTSD & Boston University, Departments of Psychiatry and Psychology
References
- Achenbach TM, Edelbrock CS. The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin. 1978;85:1275–1301. [PubMed] [Google Scholar]
- Achenbach TM, Edelbrock CS. Psychopathology of childhood. Annual Review of Psychology. 1984;35:227–256. doi: 10.1146/annurev.ps.35.020184.001303. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed Author; Washington, DC: 1994. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: the posttraumatic stress disorder-major depression connection. Biological Psychiatry. 2000;48:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. Guilford; New York: 2006. [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Chantarujikapong SI, Scherrer JF, Xian H, Eisen SA, Lyons MJ, Goldberg J, et al. A twin study of generalized anxiety disorder symptoms, panic disorder symptoms and post-traumatic stress disorder in men. Psychiatry Research. 2001;103:133–145. doi: 10.1016/s0165-1781(01)00285-2. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Clara IP, Enns MW. Posttraumatic stress disorder and the structure of common mental disorders. Depression and Anxiety. 2002;15:168–171. doi: 10.1002/da.10052. [DOI] [PubMed] [Google Scholar]
- Forbes D, Creamer M, Allen N, Elliott P, McHugh T, Debenham P, Hopwood M. MMPI-2 based subgroups of veterans with combat-related PTSD. Journal of Nervous and Mental Disease. 2003;191:531–537. doi: 10.1097/01.nmd.0000082181.79051.83. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hyer L, Davis H, Albrecht W, Boudewyns P, Woods G. Cluster analysis of MCMI and MCMI-II on chronic PTSD victims. Journal of Clinical Psychology. 1994;50:502–515. doi: 10.1002/1097-4679(199407)50:4<502::aid-jclp2270500404>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Keane TM, Kolb LC, Kaloupek DG, Orr SP, Blanchard EB, Thomas RG, et al. Utility of psychophysiological measurement in the diagnosis of posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Journal of Consulting and Clinical Psychology. 1998;66:914–923. doi: 10.1037//0022-006x.66.6.914. [DOI] [PubMed] [Google Scholar]
- Keane TM, Wolfe J. Comorbidity in post-traumatic stress disorder: An analysis of community and clinical studies. Journal of Applied Social Psychology. 1990;20:1776–1788. [Google Scholar]
- Kendler KS, Heath AC, Neale MC, Kessler RC, Eaves LJ. Alcoholism and major depression in women. A twin study of the causes of comorbidity. Archives of General Psychiatry. 1993;50:690–698. doi: 10.1001/archpsyc.1993.01820210024003. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61:4–12. [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Study. Archives of General Psychiatry. 1995;5:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Hitsman B, Lyons MJ, Niaura R, McCaffery J, Goldberg J, et al. A twin registry study of the relationship between posttraumatic stress disorder and nicotine dependence in men. Archives of General Psychiatry. 2005;62:1258–1265. doi: 10.1001/archpsyc.62.11.1258. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Lyons MJ, Goldberg J, Simpson J, Williams WM, Toomey R, et al. A high risk twin study of combat-related PTSD comorbidity. Twin Research. 2003;6:218–226. doi: 10.1375/136905203765693870. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology. 2003;112:437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personality & Individual Differences. 2001;30:1245–1259. [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam War generation: Report on the findings from the National Vietnam Veterans Readjustment Study. Brunner/Mazel; New York: 1990. [Google Scholar]
- Lin N, Eisen SA, Scherrer JF, Goldberg J, True WR, Lyons MJ, et al. The influence of familial and non-familial factors on the association between major depression and substance abuse/dependence in 1874 monozygotic male twin pairs. Drug and Alcohol Dependence. 1996;43:49–55. doi: 10.1016/s0376-8716(96)01287-2. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Risch NJ, Weissman MM. Co-morbidity and co-transmission of alcoholism, anxiety and depression. Psychological Medicine. 1994;24:69–80. doi: 10.1017/s0033291700026842. [DOI] [PubMed] [Google Scholar]
- Miller MW. Personality and the etiology and expression of PTSD: A three-factor model perspective. Clinical Psychology: Science and Practice. 2003;10:373–393. [Google Scholar]
- Miller MW, Greif JL, Smith AA. Multidimensional Personality Questionnaire profiles of veterans with traumatic combat exposure: Internalizing and externalizing subtypes. Psychological Assessment. 2003;15:205–215. doi: 10.1037/1040-3590.15.2.205. [DOI] [PubMed] [Google Scholar]
- Miller MW, Kaloupek DG, Dillon AL, Keane TM. Externalizing and internalizing subtypes of combat-related PTSD: A replication and extension using the PSY-5 Scales. Journal of Abnormal Psychology. 2004;113:636–645. doi: 10.1037/0021-843X.113.4.636. [DOI] [PubMed] [Google Scholar]
- Miller MW, Resick PA. Internalizing and externalizing subtypes of female sexual assault survivors: Implications for the understanding of complex PTSD. Behavior Therapy. 2007;38:58–71. doi: 10.1016/j.beth.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MW, Vogt DS, Mozley SL, Kaloupek DG, Keane TM. PTSD and substance-related problems: The mediating roles of disconstraint and negative emotionality. Journal of Abnormal Psychology. 2006;115:369–379. doi: 10.1037/0021-843X.115.2.369. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 4thd ed Authors; Los Angeles: 1998-2006. [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MD. Structured Clinical Interview for DSM-III-R, Patient Version (SCID-P) New York State Psychiatric Institute; New York: 1989. [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Idema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: The NEMESIS Study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Xian H, Chantarujikapong SI, Scherrer JF, Eisen SA, Lyons MJ, Goldberg J, et al. Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence in twin pairs. Drug and Alcohol Dependence. 2000;61:95–102. doi: 10.1016/s0376-8716(00)00127-7. [DOI] [PubMed] [Google Scholar]