Abstract
Background
Disturbances of smell and taste are common. About 5% of the general population have anosmia (absence of the sense of smell). Olfactory dysfunction can markedly impair the quality of life.
Methods
Review of pertinent literature retrieved by a selective search.
Results
In recent years, simple and reliable tests of the sense of smell have been introduced in otorhinolaryngology. Olfactory testing has become a new focus of attention in neurology as well, mainly because many patients with neurodegenerative diseases—including the majority of those with Parkinson’s or Alzheimer’s disease—have olfactory loss early on in the course of their disorder. Olfactory dysfunction is thus regarded as an early sign of neurodegenerative disease that may allow a tentative diagnosis to be made years before the motor or cognitive disturbances become evident. As for the treatment of olfactory loss, anti-inflammatory drugs and surgery can help in some cases, and olfactory training can lead to significant improvement of post-viral olfactory deficits.
Conclusion
Olfactory dysfunction is common and becomes more common with advancing age. It is increasingly receiving attention as an important sign for the early diagnosis and the differential diagnosis of neurodegenerative disorders.
The sense of smell is particularly important in recognition of danger, in interpersonal communication, and in eating and drinking (1). Most of the complaints of patients who have become anosmic or were born without a sense of smell fall into these three categories:
The absence of an olfactory warning function often leads to food poisoning.
The inability to perceive body odors may lead to insecurity in partnerships or in contact with children, for example.
The pleasure gained from eating and drinking is greatly reduced.
Owing to these limitations many patients with olfactory dysfunction show signs of depression (2).
Interestingly, around 5% of people are anosmic. The loss of olfactory function clearly increases with age: Above 50, a quarter of the population has an impaired sense of smell (presbyosmia) (3– 5). Although this is well known, research into olfaction is at least 40 years behind work on the senses of hearing and sight. It was not until 2004, for instance, that a Nobel Prize was awarded for research into the sense of smell. This also goes to show how smell plays a much less important part in human life than hearing and vision.
This article is based essentially on the findings of a selective literature review.
Physiological aspects
As a rule, olfaction forms one component of a multisensory event. Eating and drinking involves the interaction of at least three sensory pathways: the gustatory, trigeminal, and olfactory systems (6). The gustatory system (glossopharyngeal, facial, and vagus nerves) conveys sweet, sour, salty, bitter, and umami flavors (umami is the flavor of glutamate, best described as the taste of meat broth). The trigeminal nerve transmits sensations such as the pungency of mustard and the sparkling of carbonated drinks. The olfactory system picks up thousands of different odors from the environment via the nostrils, but when food and drink are being consumed the smells reach the olfactory mucosa by way of the throat, imparting the final subtleties of taste. Many patients who have lost their sense of smell initially complain that their sense of taste is blunted.
The olfactory mucosa is situated in the upper third of the nasal cavity; only about 10% of inhaled air reaches the olfactory epithelium (e1).
Odoriferous substances penetrate the mucous membrane and activate the olfactory receptor proteins on the cell wall of the apical cilia of the olfactory cells (7). The special characteristic of the ca. 6 to 30 million olfactory receptor neurons (ORNs) is that they continuously renew themselves from the basal cells. This regeneration capacity diminishes with increasing age (interestingly, there is a statistical association between olfactory acuity and mortality [8]).
Around 380 functional receptors are coded in the human genome (9, 10). Every ORN expresses a certain receptor type. ORNs that express the same receptor type send axons to specific glomeruli in the olfactory bulb (OB). Odors regularly bind to more than one type of receptor. This leads to various patterns of stimulation in the OB that serve to code the quality of odors. The subsequent cerebral processing of odors involves, among other structures, the limbic system (e.g., amygdala, hippocampus), cerebellum, and insula (11). The orbitofrontal cortex is important for the conscious perception of odors (5).
Diagnosis
The most important thing when investigating olfactory dysfunction is to take a detailed medical history. Patients must be asked about the onset, course, and nature of the impairment, their previous illnesses, and the medications they have taken (12). The ENT examination should include nasal endoscopy. Referral to a neurologist is advisable particularly in the case of idiopathic olfactory dysfunction. Magnetic resonance imaging (MRI) of the brain may be necessary, for instance if the dysfunction is suspected to be congenital.
After initial, at least cursory assessment of the sense of taste with flavor sprays, the patient’s sense of smell is investigated. There are simple screening tests that distinguish between “healthy” and “sick,” deliver useful and readily understandable results in a matter of minutes, and are easy to apply. The Olfactology/Gustology Working Group of the German Society of Otorhinolaryngology, Head and Neck Surgery recommends “Sniffin’ Sticks” for this purpose (Figure 1). The “Sniffin’ Sticks” system comprises a screening test, more extensive tests of the detection and distinction of odors, and determination of the olfactory threshold. The pen-like devices containing the odoriferous substances are reusable (13). In the case of more complex problems, additional information can be provided by retronasal tests of olfaction, recording of olfactory evoked potentials, and volume measurement of the OB (13).
Figure 1.
Simple odor identification test (Sniffin’ Sticks). Pen-like odor dispensers are held under the proband’s nose and each odor has to be identified from a list of four choices. The test can be completed in a matter of minutes.
Etiology
Olfactory dysfunction is divided into quantitative and qualitative impairments (Table 1). The principal causes of olfactory dysfunction include:
Table 1. Classification of olfactory dysfunction (from [39]).
| Olfactory dysfunction (dysosmia) | ||
| Quantitative | Hyperosmia | Oversensitivity |
| Normosmia | Normal sensitivity | |
| Hyposmia | Reduced sensitivity | |
| Anosmia (functional anosmia, specific anosmia) | Complete anosmia: absolute loss of olfactory function; no sense of smell detectable | |
| Functional anosmia: severe limitation of olfactory function; includes complete loss as well as residual odor perception | ||
| Partial anosmia: greatly reduced sensitivity to a particular odoriferous substance/group of substances compared with the general population, usually not viewed as pathological | ||
| Qualitative | Parosmia | Altered perception of odors in the presence of a stimulus |
| Phantosmia | Perception of odors in the absence of a stimulus |
Trauma
Viral infections
Rhinosinusitis or nasal polyposis
Neurodegenerative illnesses such as Parkinson disease or Alzheimer dementia (14, 15).
Posttraumatic olfactory dysfunction may be due to rupture of the olfactory filaments or cerebral contusion. In the case of viral infections, the causal factor is assumed to be damage to the ORNs. The causes of sinonasal olfactory dysfunction include inflammatory or mechanical factors such as diversion of access to the olfactory epithelium (13). Smell tests can contribute to the localization of the underlying pathology. If only the ability to discriminate between odors is affected, central nervous impairment can be suspected, while isolated shifting of the olfactory threshold tends to indicate peripheral damage (16).
Early symptom of neurodegenerative disease
In recent years, extensive investigations have confirmed the association between neurodegenerative disease and olfactory impairment and demonstrated the high diagnostic significance of this link (17– 19). Olfactory dysfunction thus serves as an early warning of the most frequent neurodegenerative diseases —idiopathic Parkinson disease (IPD) and Alzheimer dementia (AD)—and aids differential diagnosis.
Idiopathic Parkinson disease
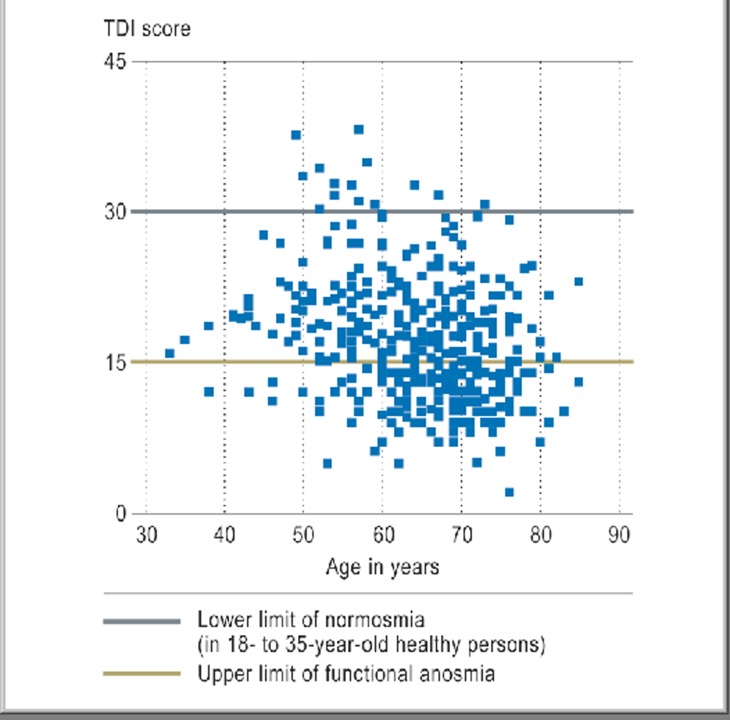
Together with tremor, rigidity, and akinesia, olfactory dysfunction is a prominent symptom of IPD (17). Taking the olfactory function of healthy young people as the normal value, over 95% of patients with IPD exhibit olfactory impairment (20) (Figure 2). Even using age-related normal values (21), almost 75% of IPD patients have hyposmia or functional anosmia. The test (21) shows severe hyposmia or anosmia in most patients, occasionally accompanied by parosmia. The olfactory deficit can be detected by simple means, but comprehensive olfactory testing offers the greatest sensitivity. In patients found to have normal olfactory function the diagnosis of IPD should be reconfirmed or other diagnoses considered.
Figure 2.
Olfactory function in 400 patients with idiopathic Parkinson disease. The results are expressed as TDI scores (sum of threshold discrimination and identification tests). (From [e7]: Hähner A, Welge-Lüssen A: Riechstörungen bei neurodegenerativen Erkrankungen [Olfactory dysfunction in neurodegenerative diseases]. HNO 2012; 7: 644–9 by kind permission of Springer-Verlag Heidelberg)
At the individual level it is very difficult to establish a correlation between the extent of olfactory impairment and the duration of the Parkinson disease symptoms. However, measurement of evoked potentials (EPs) after passive olfactory stimulation demonstrated a correlation between EP latency times and the severity of IPD (22). Furthermore, a recently published study indicates a marker function for hyposmia for disease progression, at least in the early stages (23).
Olfactory dysfunction is an early symptom of IPD. Because the sense of smell deteriorates only slowly, however, the loss of olfactory acuity often goes unnoticed by those affected and is hardly ever reported. The olfactory impairment is thought to precede the motor symptoms by ca. 4 to 6 years. For this reason IPD should be considered in at least some cases of idiopathic olfactory dysfunction, particularly in patients who display REM sleep behavior disorder or depression. In a study of 361 relatives of IPD patients who themselves showed no motor symptoms, 4 (10 %) of the 40 subjects found to have hyposmia were diagnosed as having IPD 2 years later (24) (see [25]). These findings receive support from the model described by Braak et al. (26), according to which the earliest pathological changes in stage I occur in the OB and the anterior olfactory nucleus, while the substantia nigra is not involved until stage III. These early changes in olfactory function currently form part of several longitudinal cohort studies (e.g., www.trend-studie.de).
Other parkinsonian syndromes
Severe olfactory dysfunction is also found in Lewy body dementia. The olfactory impairment is less far-reaching in multisystemic atrophy, and patients with progressive supranuclear ophthalmoplegia (PSP) or corticobasal degeneration (CBD) generally have practically unaffected olfactory function (18). The American Academy of Neurology now recommends including tests of olfaction in the diagnosis of IPD, although so far only the distinction of IPD from PSP or CBD is viewed as reliable.
Very few studies have provided data on olfactory function in familial Parkinson disease. While mild hyposmia was observed in individuals with mutations in the alpha-synuclein gene (PARK-1), persons with mutations in the parkin gene (PARK-2) showed practically normal olfactory function. Individuals with mutations in the LRRK2 gene (PARK-8) displayed olfactory dysfunction identical to that in IPD; however, the small number of asymptomatic carriers of the gene examined to date were normosmic (e2).
Differentiation of vascular Parkinson disease from IPD may be difficult because of the possibly similar findings (27).
Patients with neuroleptic drug–induced parkinsonian syndromes exhibit moderate olfactory dysfunction (28). There is a close correlation between the degree of hyposmia and the severity of the motor symptoms. This raises the question of whether the patients who develop parkinsonism under the influence of neuroleptics possess a predisposition for IPD, or whether the administration of neuroleptics unmasks IPD and the accompanying olfactory dysfunction.
In symptomatic parkinsonian syndromes, e.g. on the basis of Wilson disease, there is a clear correlation between olfactory dysfunction and extrapyramidal motor symptoms. This illustrates the close connection between the function of the basal ganglia and olfactory processing (29).
Alzheimer dementia
The olfactory deficits observed in patients with Alzheimer dementia (AD) are similar in severity to those in IPD. Olfactory testing cannot distinguish between early AD and early IPD (30). In AD as in IPD, olfactory dysfunction is an early symptom. According to Braak et al. (31), there is very early involvement of the entorhinal cortex, which plays a role in both mnestic and olfactory processing. In contrast to IPD, therefore, a clear correlation has been demonstrated between the severity of symptoms and olfactory performance. Patients with AD also display MRI signs of OB volume reduction at a very early stage. Patients with only mild cognitive impairments were found to have impaired olfactory function compared with healthy controls (32), and the deterioration in olfactory performance may precede the cognitive deficits.
Similarly severe olfactory abnormalities have been described in other dementias of neurodegenerative origin, such as the above-mentioned Lewy body dementia and frontotemporal dementia.
Huntington disease
Huntington disease is associated with moderate hyposmia. Family members with a 50% risk of disease show no olfactory abnormalities (see, for example, [e3]), so it can be assumed that the olfactory changes begin at the same time as the motor and cognitive symptoms. In contrast, Larsson et al. (33) reported odor discrimination impairments in asymptomatic carriers of the Huntington disease gene.
Other neurodegenerative diseases
Many other neurodegenerative diseases are accompanied by olfactory dysfunction, but usually not as an early symptom. Among the heredoataxias, olfactory function has so far been investigated, and impairments found, in patients with Friedreich ataxia and spinocerebellar ataxia types 2 and 3. Mild olfactory dysfunction is also found in motor neuron diseases. Hyposmia has been described as occurring early in the course of Creutzfeldt–Jakob disease; for other prion diseases the data are insufficient. Worthy of mention is a study in knockout mice demonstrating that the physiological prion protein has a role in olfactory processing (34).
Prognosis and treatment
The prognosis of olfactory dysfunction depends on the cause. There is very little that can be done to affect age-related and congenital olfactory dysfunction; the patients can best be helped by counseling (www.hno.org/olfaktologie/index.html [in German]). Ten to thirty percent of patients with posttraumatic anosmia and around 60% of those with postinfectious olfactory dysfunction experience partial recovery over the course of time. Factors that favor recovery from posttraumatic and postinfective impairment of the sense of smell include:
High residual olfactory capacity
Young age
Nonsmoker
Initial parosmia
Absence of lateral differences in olfactory function
Large amplitudes of the chemosensory evoked potentials to trigeminal stimuli
Large OB volume.
The time since the onset of olfactory dysfunction is also prognostically relevant (35).
Treatment of the cause of olfactory dysfunction is possible only when nasal diseases are responsible (see review in [13]). Operative treatment, e.g., polypectomy or surgery for pansinusitis, and administration of corticosteroids are the primary options.
The best results in surgical treatment of olfactory dysfunction are generally thought to be obtained in patients with polyposis. The patient’s age and the number of previous operations do not predict postoperative olfactory performance (36).
Corticoids for conservative treatment of sinonasal olfactory dysfunction can be administered topically or systemically (e4). Systemic corticoids are often given in the form of so-called cortisone pulse therapy (e.g., 40 mg initially with reduction by 5 mg every 2 days). This procedure also seems sensible in idiopathic olfactory dysfunction, for instance in the case of endoscopically undetectable mucosal swelling in the olfactory fissure. Because of the nasal filtering function, local corticoids (37) should be given using an extra-long applicator (e5) or with the patient’s head tilted backwards.
With regard to the treatment of other, nonsinonasal forms of olfactory dysfunction, accounts of some interesting approaches have been published but no blinded studies have been conducted. The procedures described include the use of caroverine, alpha-lipoic acid, theophylline, or acupuncture; most of these approaches are based on the hope that the olfactory system will be possessed of plasticity. One newly described approach, olfactory training, takes advantage of the unique regenerative capacity of the ORNs (38). A multicenter double-blind study under the aegis of the Olfactology/Gustology Working Group of the German Society of Otorhinolaryngology, Head and Neck Surgery demonstrated that this inexpensive, complication-free stimulation of the sense of smell in patients with postviral olfactory disorders achieved improvement of olfactory function that was significantly better than spontaneous recovery (manuscript in preparation).
Treatment options in dysfunction of neurodegenerative origin
Medicinal treatment of IPD seems to have no effect on the olfactory dysfunction. In contrast to dopaminergic therapy, deep brain stimulation in the subthalamic nucleus showed a positive effect on some aspects of olfactory processing (e6). One promising approach is the recently described olfactory training (38), in which the patient regularly sniffs at samples of various odors.
Olfactory dysfunction can considerably impair the patient’s quality of life but is not always seen as meriting treatment, partly because attention is focused on the symptoms of the underlying disease and partly owing to the gradual development of the dysfunction in most neurodegenerative diseases, so that patients become accustomed to it. Nevertheless, in view of the potential consequences of olfactory dysfunction, e.g., failing to notice that foodstuffs are spoiled, patients with such diseases should be informed about the accompanying olfactory symptoms.
Although the options for treatment of olfactory dysfunction in neurodegenerative diseases are limited, it is important to record the presence of any olfactory disorder. It has to be assumed that early diagnosis will enable earlier initiation of disease-modifying—or, in the future, perhaps neuroprotective—treatment strategies. In this way, recording of hyposmia has an important part to play.
Conclusion
Olfactory dysfunction accompanies many neurodegenerative diseases. Its early occurrence in IPD and AD gives it a special role in the early detection and differential diagnosis of these diseases, which may be decisive in timely initiation of treatment. Patients with olfactory dysfunction of unknown cause seem to have a two- to threefold risk of developing IPD or AD at a later point in time.
The guidelines of the German Society of Otorhinolaryngology, Head and Neck Surgery (39) thus recommend that patients with olfactory dysfunction of uncertain origin be referred to a neurologist after conclusion of the ENT work-up.
Table 2. Characteristics of posttraumatic, postviral/infectious und sinonasal-related olfactory dysfunction (from [40]).
| Head injury | Infection of the upper respiratory tract | Rhinitis/sinusitis | |
| Probable cause | Lesion of the olfactory fibers in the region of the lamina cribrosa; contusion of brain areas relevant to olfaction | Viral damage of olfactory epithelium | Mechanical displacement, edema/functional impairment as a consequence of inflammatory processes of the mucosa/the olfactory bulb (?) |
| Isolated odor impressions | Rare | Frequent | Frequent |
| Epithelium | Degeneration | Metaplasia, faulty development of ORNs | Signs of inflammation; often normal |
| Rate of occurrence of olfactory dysfunction | Around 5% | Less than 1% | Ca. 60% of all patients with chronic sinusitis |
| Typical age | 20–50 years | 45–65 years | 30–60 years |
| Onset of olfactory dysfunction | Rapid | Rapid | Slow |
| Olfactory loss | Severe | Moderate | Variable |
| Occurrence of parosmia | Frequent | Very frequent | Rather rare |
| Likelihood of regression of olfactory dysfunction | Infrequent, encountered mostly in hyposmic patients | Frequent, usually over a period of years | Very frequent, improvement due to surgery or conservative treatment, but often only for a short time |
ORNs, olfactory receptor neurons
Table 3. Relative severity of olfactory dysfunction in neurodegenerative diseases.
| Disease | Relative restriction of olfactory function |
| Idiopathic Parkinson disease, Alzheimer dementia, Lewy body dementia, PARK 8 | + + + |
| Multisystemic atrophy, Huntington disease | + + |
| Motor neuron diseases, Friedreich ataxia, spinocerebellar ataxia type 2, progressive supranuclear ophthalmoplegia, PARK 1 | + |
| Corticobasal degeneration, spinocerebellar ataxia type 3, PARK 2 | + / 0 |
+++… severe loss of olfactory function; 0/(+)… no or only discrete loss of olfactory function. Most of the data are based on studies of small numbers of patients. PARK 1 and 2 = gene loc
Key Messages.
Olfactory disorders are common and their frequency increases with age.
The principal causes of olfactory dysfunction are sinonasal diseases, viral infections, head injuries, and neurodegenerative diseases.
Olfactory dysfunction is an early symptom of the most common neurodegenerative diseases, idiopathic Parkinson disease and Alzheimer dementia, and may be helpful in differential diagnosis.
Causal treatment is currently available only for olfactory dysfunction owing to nasal diseases; the primary options are surgery or administration of corticosteroids.
A new approach to the treatment of nonsinonasal olfactory dysfunction is a course of olfactory training.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Hüttenbrink heads the Olfactology/Gustology Working Group of the German Society of Otorhinolaryngology, Head and Neck Surgery. The manufacturer of Sniffin’ Sticks, Burghart Messtechnik, is represented at the meetings of the working group. Research using Sniffin’ Sticks takes place in cooperation with Burghart.
Prof. Hummel has received reimbursement of congress participation fees (e.g., MDPD) and travel costs from Teva. He has received third-party funding from Teva, Takasago, Unilever, Fragrance Resources, Primavera, Bionorica, Givaudan, and Burghart (manufacturer of Sniffin’ Sticks).
Prof. Berg has received third-party funding from Teva and CIN Pharma.
Prof. Gasser has received payments from Cephalon Pharma and Merck Serono for acting as a consultant.
Dr. Hähner has received third-party funding from Teva.
References
- 1.Stevenson RJ. An initial evaluation of the functions of human olfaction. Chem Senses. 2010;35:3–20. doi: 10.1093/chemse/bjp083. [DOI] [PubMed] [Google Scholar]
- 2.Hummel T, Nordin S. Olfactory disorders and their consequences for quality of life—a review. Acta Oto-Laryngol. 2005;125:116–121. doi: 10.1080/00016480410022787. [DOI] [PubMed] [Google Scholar]
- 3.Murphy C, Schubert CR, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM. Prevalence of olfactory impairment in older adults. JAMA. 2002;288:2307–2312. doi: 10.1001/jama.288.18.2307. [DOI] [PubMed] [Google Scholar]
- 4.Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population. J Neurol. 2008;255:1121–1126. doi: 10.1007/s00415-008-0807-9. [DOI] [PubMed] [Google Scholar]
- 5.Brämerson A, Johansson L, Ek L, Nordin S, Bende M. Prevalence of olfactory dysfunction: The Skövde population-based study. Laryngoscope. 2004;114:733–737. doi: 10.1097/00005537-200404000-00026. [DOI] [PubMed] [Google Scholar]
- 6.Shepherd GM. Perspectives on olfactory processing, conscious perception, and orbitofrontal cortex. Ann N Y Acad Sci. 2007;1121:87–101. doi: 10.1196/annals.1401.032. [DOI] [PubMed] [Google Scholar]
- 7.DeMaria S, Ngai J. The cell biology of smell. J Cell Biol. 2010;191:443–452. doi: 10.1083/jcb.201008163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson RS, Yu L, Bennett DA. Odor identification and mortality in old age. Chem Senses. 2010;36:63–67. doi: 10.1093/chemse/bjq098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buck L, Axel R. A novel multigene family may encode odorant receptors: a molecular basis for odor recognition. Cell. 1991;65:175–187. doi: 10.1016/0092-8674(91)90418-x. [DOI] [PubMed] [Google Scholar]
- 10.Firestein S. How the olfactory system makes sense of scents. Nature. 2001;413:211–218. doi: 10.1038/35093026. [DOI] [PubMed] [Google Scholar]
- 11.Gottfried JA. Smell: central nervous processing. Adv Otorhinolaryngol. 2006;63:44–69. doi: 10.1159/000093750. [DOI] [PubMed] [Google Scholar]
- 12.Welge-Lüssen A, Hummel T. Praktisches Vorgehen bei Patienten mit Riechstörungen. In: Hummel T, Welge-Luessen A, editors. Riech- und Schmeckstörungen. Stuttgart: Georg Thieme Verlag; 2009. pp. 3–10. [Google Scholar]
- 13.Hummel T, Landis BN, Hüttenbrink KB. Störungen des Riechens und Schmeckens. Laryngo-Rhino-Otol. 2011;90:44–55. doi: 10.1055/s-0030-1270445. [DOI] [PubMed] [Google Scholar]
- 14.Deems DA, Doty RL, Settle RG, Moore-Gillon V, Shaman P, Mester AF, et al. Smell and taste disorders: a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otorhinolaryngol Head Neck Surg. 1991;117:519–528. doi: 10.1001/archotol.1991.01870170065015. [DOI] [PubMed] [Google Scholar]
- 15.Damm M, Temmel A, Welge-Lüssen A, Eckel HE, Kreft MP, Klussmann JP, et al. Epidemiologie und Therapie von Riechstörungen in Deutschland, Österreich und der Schweiz. HNO. 2004;52:112–120. doi: 10.1007/s00106-003-0877-z. [DOI] [PubMed] [Google Scholar]
- 16.Hedner M, Larsson M, Arnold N, Zucco GM, Hummel T. Cognitive factors in odor detection, odor discrimination, and odor identification tasks. J Clin Exp Neuropsychol. 2010;30:1–6. doi: 10.1080/13803391003683070. [DOI] [PubMed] [Google Scholar]
- 17.Doty RL, Deems D, Steller S. Olfactory dysfunction in Parkinson’s disease: A general deficit unrelated to neurologic signs, disease stage, or disease duration. Neurology. 1988;38:1237–1244. doi: 10.1212/wnl.38.8.1237. [DOI] [PubMed] [Google Scholar]
- 18.Müller A, Mungersdorf M, Reichmann H, et al. Olfactory function in Parkinsonian syndromes. J Clin Neurosci. 2002;9:521–524. doi: 10.1054/jocn.2001.1071. [DOI] [PubMed] [Google Scholar]
- 19.Hawkes C. Olfaction in neurodegenerative disorder. Adv Otorhinolaryngol. 2006;63:133–151. doi: 10.1159/000093759. [DOI] [PubMed] [Google Scholar]
- 20.Haehner A, Boesveldt S, Berendse HW, et al. Prevalence of smell loss in Parkinson's disease—a multicenter study. Parkinsonism Relat Disord. 2009;15:490–494. doi: 10.1016/j.parkreldis.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Hummel T, Kobal G, Gudziol H, Mackay-Sim A. Normative data for the „Sniffin’ Sticks“ including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3,000 subjects. Eur Arch Otorhinolaryngol. 2007;264:237–243. doi: 10.1007/s00405-006-0173-0. [DOI] [PubMed] [Google Scholar]
- 22.Barz S, Hummel T, Pauli E, Majer M, Lang CJ, Kobal G. Chemosensory event-related potentials in response to trigeminal and olfactory stimulation in idiopathic Parkinson’s disease. Neurology. 1997;49:1424–1431. doi: 10.1212/wnl.49.5.1424. [DOI] [PubMed] [Google Scholar]
- 23.Berendse HW, Roos DS, Raijmakers P, Doty R. Motor and non-motor correlates of olfactory dysfunction in Parkinson’s disease. J Neurol Sci. 2011;310:21–24. doi: 10.1016/j.jns.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 24.Ponsen MM, Stoffers D, Booij J, et al. Idiopathic hyposmia as a preclinical sign of Parkinson’s disease. Ann Neurol. 2004;56:173–181. doi: 10.1002/ana.20160. [DOI] [PubMed] [Google Scholar]
- 25.Ross GW, Petrovitch H, Abbott RD, Tanner CM, Popper J, Masaki K, Launer L, White LR. Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann Neurol. 2008;63:67–73. doi: 10.1002/ana.21291. [DOI] [PubMed] [Google Scholar]
- 26.Braak H, Del Tredici K, Rub U, et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24:97–211. doi: 10.1016/s0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 27.Katzenschlager R, Zijlmans J, Evans A, Watt H, et al. Olfactory function distinguishes vascular parkinsonism from Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2004;75:1749–1752. doi: 10.1136/jnnp.2003.035287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krüger S, Haehner A, Thiem C, Hummel T. Neuroleptic-induced parkinsonism is associated with olfactory dysfunction. J Neurol. 2008;255:1574–1579. doi: 10.1007/s00415-008-0993-5. [DOI] [PubMed] [Google Scholar]
- 29.Müller A, Reuner U, Landis B, Kitzler H, Reichmann H, Hummel T. Extrapyramidal symptoms in Wilson`s disease are associated with olfactory dysfunction. Mov Disord. 2006;21:1311–1316. doi: 10.1002/mds.20989. [DOI] [PubMed] [Google Scholar]
- 30.Mesholam RI, Moberg PJ, Mahr RN, Doty RL. Olfaction in neurodegenerative disease: a meta-analysis of olfactory functioning in Alzheimer’s and Parkinson’s diseases. Arch Neurol. 1998;55:84–90. doi: 10.1001/archneur.55.1.84. [DOI] [PubMed] [Google Scholar]
- 31.Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82:239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- 32.Wilson RS, Arnold SE, Schneider JA, Boyle PA, et al. Olfactory impairment in presymptomatic Alzheimer's disease. Ann N Y Acad Sci. 2009;1170:730–735. doi: 10.1111/j.1749-6632.2009.04013.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larsson M, Lundin A, Robins Wahlin TB. Olfactory functions in asymptomatic carriers of the Huntington disease mutation. J Clin Exp Neuropsychol. 2006;28:1373–1380. doi: 10.1080/13803390500473746. [DOI] [PubMed] [Google Scholar]
- 34.Le Pichon CE, Valley MT, Polymenidou M, et al. Olfactory behavior and physiology are disrupted in prion protein knockout mice. Nat Neurosci. 2009;12:60–69. doi: 10.1038/nn.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reden J, Müller A, Mueller C, Konstantinidis I, Landis BN, Hummel T. Recovery of olfactory function following closed head injury or infections of upper respiratory tract. Arch Otolaryngol Head Neck Surg. 2006;132:265–269. doi: 10.1001/archotol.132.3.265. [DOI] [PubMed] [Google Scholar]
- 36.Pade J, Hummel T. Olfactory function following nasal surgery. Laryngoscope. 2008;118:1260–1264. doi: 10.1097/MLG.0b013e318170b5cb. [DOI] [PubMed] [Google Scholar]
- 37.Blomqvist EH, Lundblad L, Bergstedt H, Stjarne P. Placebo-controlled, randomized, double-blind study evaluating the efficacy of fluticasone propionate nasal spray for the treatment of patients with hyposmia/anosmia. Acta Otolaryngol. 2003;123:862–868. doi: 10.1080/00016480310002140. [DOI] [PubMed] [Google Scholar]
- 38.Hummel T, Rissom K, Hähner A, Reden J, Weidenbecher M, Hüttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009;119:496–499. doi: 10.1002/lary.20101. [DOI] [PubMed] [Google Scholar]
- 39.Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- und Hals-Chirurgie Riechstörungen. Leitlinie zur Epidemiologie, Pathophysiologie, Klassifikation, Diagnose und Therapie. www.awmf.org/uploads/tx_szleitlinien/017-050_S2_Riechstoerungen__mit_Algorithmus__05-2007_05-2011_01.pdf (last accessed 7 December 2012)
- 40.Knecht M, Hüttenbrink KB, Hummel T. Störungen des Riechens und Schmeckens. Schweiz Med Wochenschr. 1999;129:1039–1046. [PubMed] [Google Scholar]
- e1.Delank KW. Aerodynamik im Bereich des Riechorgans. In: Wolfgang Stoll., editor. Klinik der menschlichen Sinne. Wien: Springer Verlag; 2008. pp. 51–58. [Google Scholar]
- e2.Brockmann K, Gröger A, Di Santo A, Liepelt I, Schulte C, Klose U, Maetzler W, Hauser AK, Hilker R, Gomez-Mancilla B, Berg D, Gasser T. Clinical and brain imaging characteristics in leucine-rich repeat kinase 2-associated PD and asymptomatic mutation carriers. Mov Disord. 2011;26:2335–2342. doi: 10.1002/mds.23991. [DOI] [PubMed] [Google Scholar]
- e3.Moberg PJ, Doty RL. Olfactory function in Huntington's disease patients and at-risk offspring. Int J Neurosci. 1997;89:133–139. doi: 10.3109/00207459708988468. [DOI] [PubMed] [Google Scholar]
- e4.Jafek BW, Moran DT, Eller PM, Rowley JC, 3rd, Jafek TB. Steroid-dependent anosmia. Arch Otolaryngol Head Neck Surg. 1987;113:547–549. doi: 10.1001/archotol.1987.01860050093023. [DOI] [PubMed] [Google Scholar]
- e5.Shu CH, Lee PL, Chen KT, Lan MY. Topical corticosteroid applied with a squirt system being more effective than with nasal spray for steroid-dependent olfactory impairment. Rhinology. 2012 doi: 10.1002/lary.23212. in press. [DOI] [PubMed] [Google Scholar]
- e6.Hummel T, Jahnke U, Sommer U, Reichmann H, Müller A. Olfactory function in patients with idiopathic Parkinson’s disease: Effects of deep brain stimulation in the subthalamic nucleus. J Neural Transm. 2005;112:669–676. doi: 10.1007/s00702-004-0207-y. [DOI] [PubMed] [Google Scholar]
- e7.Hähner A, Welge-Lüssen A. Riechstörungen bei neurodegenerativen Erkrankungen. HNO. 2012;7:644–649. doi: 10.1007/s00106-010-2122-x. [DOI] [PubMed] [Google Scholar]