Abstract
Objective
To determine whether obstructive sleep apnea mediates the relationship between posttraumatic stress disorder (PTSD) and psychosomatic and somatic disorders and its implications for self-rated health (SRH) among Iraqi immigrants in the United States.
Methods
A random sample of immigrants who had left Iraq before the 1991 Gulf War (n = 145) or after (n = 205) and are residing in metropolitan Detroit responded to a structured interview covering questions on sociodemographics, premigration trauma, SRH, physician-diagnosed and -treated obstructive sleep apnea, somatic disorders, and psychosomatic disorders. Structural equation modeling was used to evaluate the relationship between premigration trauma scores and health, as well as to explore mediating pathways between PTSD, obstructive sleep apnea, and health.
Results
The prevalence of obstructive sleep apnea among post-Gulf War immigrants (30.2%) was significantly higher than among pre-Gulf War immigrants (0.7%; p < .001). Premigration trauma scores were positively associated with depression and PTSD. Structural equation modeling supported a model in which obstructive sleep apnea mediated the relationship between PTSD and psychosomatic and somatic disorders. Premigration trauma also related directly to SRH.
Conclusions
Part of the PTSD-associated adverse health effects observed in Iraqi immigrants is mediated by obstructive sleep apnea. Because sleep apnea in the current study is based on medical history and current treatment, there is a need for future confirmatory polysomnographic studies.
Keywords: stress, Gulf War, PTSD, obstructive sleep apnea, health, psychosomatic disorder
INTRODUCTION
Immigrants, in general, and refugees, in particular, are at increased risk for trauma-related disorders, including depression, posttraumatic stress disorder (PTSD), anxiety disorders, musculoskeletal disorders, and cardiovascular diseases (1–10). As such, they are an important group to study for disease prevalence, mechanism, and prevention strategies. Moreover, lower self-rated health (SRH), metabolic syndrome, diabetes, and hypercholesterolemia have been reported to be more prevalent in refugees than in reference populations (7,11). A few studies have also reported that certain sleep disorders are more common among immigrants, especially refugees (12). However, despite the fact that many of the aforementioned health disorders have been reported to be associated with obstructive sleep apnea in the general population, there is a lack of studies on the possible mediating role of obstructive sleep apnea in linking PTSD symptoms and health outcomes in immigrants, including refugees (13). Although it is well known that obstructive sleep apnea occurs when the muscles supporting the soft palate at the back of the throat relax, less is known about the reasons behind this neuromuscular malfunctioning. It is being hypothesized that key components of the brain’s stress response system, including the amygdala and the prefrontal cortex, are involved (14). The health implications for trauma-induced disorders, such as depression and PTSD, might thus be aggravated by obstructive sleep disorders, with relevance to recovery from trauma, nightmare, and related sensitization to prior trauma (15).
Iraqis were exposed to harsh conditions during the entirety of Saddam Hussein al-Tikriti’s more than 20 years’ reign, including the Iraq-Iran war (16). However, trauma and environmental exposures increased measurably and dramatically after the initiation of the 1991 Gulf War (GW). The implications of GW-associated trauma, psychosocial conditions, and physical conditions for health are becoming increasingly documented, as discussed above (17).
The purpose of the present study was to estimate the prevalence of physician-diagnosed and -treated obstructive sleep apnea in a random sample of Iraqis who had left Iraq before and after the initiation of the 1991 GW, respectively. We also wanted to determine the degree of premigration trauma in relation to stress-related disorders and whether obstructive sleep apnea was a mediator between PTSD symptoms and somatic and psychosomatic symptoms and its relationship to SRH. We tested three main hypotheses:
Persons who left Iraq after the 1991 GW will exhibit an increased prevalence of PTSD symptoms, somatic and psychosomatic disorders, and obstructive sleep apnea.
Obstructive sleep apnea will be a mediator of the relationship between PTSD symptoms and somatic and psychosomatic health.
There is an inverse relationship between premigration trauma exposure and SRH.
METHODS
Participants
The study took place in the metropolitan Detroit area. The sample consisted of 350 Iraqi immigrants who had left Iraq either before the 1991 GW (pre-GW; n = 145) or after the initiation of the GW (post-GW; n = 205). Participants are described in detail in Table 1.
TABLE 1.
Study Demographics Comparing Immigrants Who Left Iraq Before and After the 1991 Gulf War
| Post-1991 (n = 205) | Pre-1991 (n = 145) | Total (N = 350) | |
|---|---|---|---|
| Age, M (SD), y* | 44.8 (7.7) | 46.6 (7) | 45.6 (7.46) |
| Years in the United States, M (SD)** | 9.4 (3.16) | 26.7 (6.97) | 18.6 (9.96) |
| Sex, n (%)* | |||
| Women | 99 (48.3) | 55 (37.9) | 154 (44) |
| Men | 106 (51.7) | 90 (62.1) | 196 (56) |
| Marital status, n (%)** | |||
| Single | 15 (7.3) | 27 (18.6) | 42 (12) |
| Married | 190 (92.7) | 118 (81.4) | 308 (88) |
| Education, n (%)* | |||
| High school or more | 114 (55.6) | 97 (66.9) | 211 (60.3) |
| Less than high school | 91 (44.4) | 48 (33.1) | 139 (39.7) |
| Occupation, n (%)** | |||
| Unemployed | 121 (59) | 36 (25) | 157 (45) |
| Employed | 84 (41) | 108 (75) | 192 (55) |
| Health insurance, n (%)** | |||
| No | 49 (23.9) | 64 (44.1) | 113 (32.3) |
| Yes | 156 (76.1) | 81 (55.9) | 237 (67.7) |
| Annual income, n (%)*** | |||
| Higher than US $10,000 | 41 (59.4) | 48 (87.3) | 89 (71.8) |
| US $10,000 or less | 28 (40.6) | 7 (12.7) | 35 (28.2) |
| Smoking status, n (%) | |||
| Never smoker | 143 (69.8) | 90 (62.1) | 233 (66.6) |
| Smoker | 62 (30.2) | 55 (37.9) | 117 (33.4) |
Independent-sample t test and χ2 test were used for continuous and discrete variables, respectively.
GW = Gulf War; M = mean; SD = standard deviation.
p < .05.
p < .001.
Sampling Process
Most studies of immigrants are based on convenience samples because there is a lack of ethnicity-specific public databases (18,19). The current study faced the same challenge because there is no single all-encompassing database to identify Iraqis residing in the United States, in general, or in metropolitan Detroit, in particular. Thus, to reach out to as many Iraqis as possible regarding the research study, we established an elaborate network with numerous community resources, including immigration and resettlement agencies, Arab and Chaldean community centers, churches, and mosques. In addition, the project was announced in the metropolitan Detroit region using Arab media. Furthermore, we distributed flyers in stores and service centers frequented by Iraqis. This was performed to ensure that the ultimate sample was representative of the target population. The process resulted in a list of 5490 addresses, representing people with a high likelihood of being of Arabic inheritance based on their names or their participation in various Arabic entities and social organizations. The address list was coded and entered into an SPSS program to randomly select a sample of 7.5%. Of 411 randomly generated addresses, 44 residents did not fit the study criteria (e.g., not Iraqi-born). The inclusion criterion for the current study was that participants were aged 18 years or older at the time that they emigrated from Iraq. Out of 367 eligible candidates, 17 persons (4.6%) declined to participate. The reasons were lack of time (n = 9) and lack of interest in the study (n = 7), whereas one provided no reason. The final number of participants was 350 people, representing a response rate of 95%. The study took place in 2004 and 2005.
Measures
The structured survey questionnaire was adapted from a validated instrument that has been used in a series of large-scale surveys including US and Iraqi GW veterans, as well as Iraqi immigrants and refugees in the United States. In addition to sociodemographics, including education, the survey contained questions on the existence, frequency, and intensity of 33 specific medical conditions, including sleep apnea (20). To be classified in the current study as patients with obstructive sleep apnea, the persons had to state that they had been diagnosed by a physician as having obstructive sleep apnea and that they had been receiving treatment. The survey also asked about the current existence of other disorders, including heart disease, hypertension, diabetes, chronic headache, migraine, chronic fatigue, musculoskeletal disorders, PTSD, and depression. PTSD scores were determined using the PTSD Checklist-Military version. PRIME-MD was used to assess depression (20,21). Psychosomatic disorders were operationally defined as affirmative answers to one or more of the following disorders: migraine, musculoskeletal symptoms, chronic fatigue, and chronic headaches. Somatic disorders included affirmative answers to one or more of the following conditions: hypertension, heart disease, and diabetes mellitus. For each of these disorders, participants were asked whether they received the original diagnosis from a physician before or after 1991 (the year of the GW) and whether they received any physician-prescribed treatment of the respective disorder. There was also a global question asking the participants to rate their SRH at the time of the interview. Responses were provided using a Likert-type scale ranging from 1 (poor health) to 5 (excellent health). The SRH scale is well validated and shown to predict future health and mortality in currently healthy participants (22,23).
Premigration trauma exposures were assessed by a standardized set of questions (16). Respondents were asked whether they had been exposed to one or more of the following nine potential traumas: exposure to dead animals; hearing chemical alarms sounding; Scud missiles exploding in the air or on the ground within 1 mile; having artillery, rocket, or mortar (anything other than Scud missiles) explosions within 1 mile; coming under small-arms fire; seeing dead bodies or people maimed or seriously injured; witnessing someone dying; and any other exposure that the participant deemed to be harmful or stressful. These exposures were considered to be of sufficient severity to fulfill the exposure criterion A in DSM-IV-R for PTSD. For each specific exposure, exposure status was multiplied by exposure duration (none, <5 days, 5–30 days, and >30 days, respectively, coded as 0, 1, 2, and 3) to calculate the cumulative exposure trauma exposure dose used in the analysis. We used the premigration trauma exposure score as an indicator of aggregate premigration trauma. It is less likely that a person would systematically bias one’s responses to the series of trauma questions as compared with using pre-GW versus post-GW as an alternative exposure variable.
Informed Consent
All survey questions were administered in Arabic by two Iraqi-born, Arab-speaking physicians who had been specifically trained by the research team in interview methodology. The structured interview allowed for the physicians to dwell deeper into medical history when so warranted. The study was approved by the Institutional Review Board of Wayne State University.
After detailed written and oral information, participants were asked to complete and sign an informed consent form. They were informed that participation was voluntary, they could rest during the interview process if they so desired, and they had the right to stop any further participation in the interview without any further explanation or consequences. The interviews took between 2 and 3 hours each. Participants received a gift certificate for US $25.00 at the completion of the interview.
Statistical Analysis
We used independent-sample t test for bivariate analyses of continuous outcomes and χ2 test for discrete variables to compare immigrants who arrived before and after the 1991 GW.
Structural equation modeling (SEM) was used in the multivariate analysis to test the proposed mediated pathways (24,25). Several steps were involved to empirically identify potentially important confounders. The SEM analytical strategy was as follows: First, an a priori conceptual model was specified and statistically evaluated (Table 4, Model 1; Fig. 1). Second, theoretically plausible pathways for improving the fit of this initial model were added. The objective of this second step was to determine if a good-fitting model could be achieved with the addition of theoretically plausible pathways (Table 4, Model 2; Fig. 2). Third, eight potentially confounding variables (Table 3, Variables 8–15) were added to the model and evaluated using both empirical and theoretical criteria (Table 4, Model 3). The final model excluded covariate pathways that were not significant (Table 4, Model 4; Fig. 3).
TABLE 4.
Statistics Used to Evaluate Model Fit
| Statistics | Criteria for “Good” Fit | Model 1 | Model 2a | Model 3b | Model 4c |
|---|---|---|---|---|---|
| χ2 | 69.13 | 19.76 | 306.11 | 49.47 | |
| df | 12 | 8 | 56 | 33 | |
| p | <.001 | .01 | <.001 | .03 | |
| CFI | >0.95 | 0.93 | 0.99 | 0.82 | 0.99 |
| RMSEA | <0.08 | 0.12 | 0.07 | 0.11 | 0.04 |
df = degrees of freedom; p = significance value; CFI = comparative fit index; RMSEA = root mean square error of approximation.
Three paths and one covariance were added to the model, resulting in the loss of 4 df.
Eight covariates were added to the model, and modification indices were evaluated to identify potential confounders.
Three potential covariates (years in the United States, married, and health insurance) and six paths were added between covariates and endogenous variables.
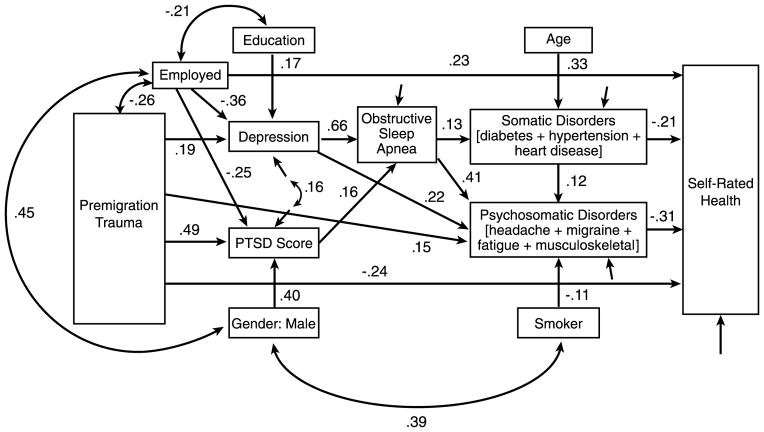
Figure 1.

Initial model showing proposed relations and standardized path coefficients. All coefficients were significant, p < .05. Fit statistics indicate that fit could be improved by adding additional paths (model fit statistics: χ2 = 69.13, df = 12, p < .001, comparative fit index = 0.93, root mean square error of approximation = 0.12). PTSD = posttraumatic stress disorder.
Figure 2.
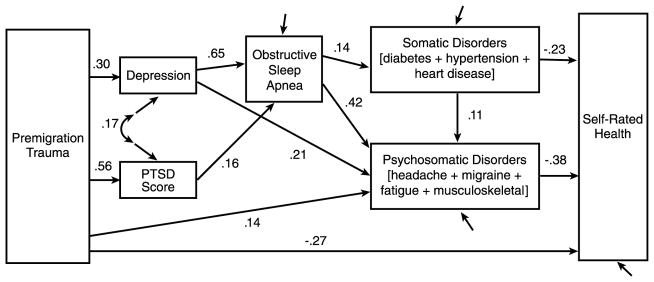
Result of fitting the initial model with three additional paths and one covariance (model fit statistics: χ2 = 19.76, df = 8, p = .011, comparative fit index = 0.99, root mean square error of approximation = 0.065). PTSD = posttraumatic stress disorder.
Figure 3.
Final model showing standardized path coefficients. All path coefficients are significant, p < .01. Covariance terms among exogenous variables with correlation less than 0.2 are not shown to improve readability (model fit statistics: χ2 = 49.47, df = 33, p = .033, comparative fit index = 0.986, root mean square error of approximation = 0.038). PTSD = posttraumatic stress disorder.
Primary analysis was carried out on the variance-covariance matrix and using maximum likelihood (ML) estimation (AMOS version 18). Modification indices (Lagrange multipliers) were used to empirically identify potentially important paths that were not specified in the a priori model. Because ML assumes multivariate normality among endogenous variables, bootstrapping was used to estimate the statistical significance of path coefficients, in addition to the standard ML asymptotic statistics. Overall model fit was evaluated using the comparative fit index (CFI), root mean square error of approximation, and analysis of standardized residuals. The CFI is a measure of relative fit ranging from 0 (worst-fitting possible model) to 1 (model with perfect fit) (26). Models with a CFI of 0.95 or larger are considered to have a good fit to the data; however, a value of 0.90 or larger is often used. We used the stricter cutoff score of 0.95. The root mean square error of approximation fits statistical ranges from 0 to ∞, with a value of 0 indicating exact fit (27). Small values of 0.08 or less indicate acceptable fit, and values of 0.05 or less indicate good fit (25). (See Table 4 for cutoff scores for fit indices used in this study.) The model χ2 statistic, including degrees of freedom and probability values, is reported, but we do not use this to evaluate model fit because it is strongly affected by sample size and assumes a perfect-fitting model, which is unrealistic. For simulation work, when the true model is known, the χ2 probability should be greater than 0.05. Other details of analytical strategies are described in the “Results” section. Statistical significance was set to a two-sided p value of <.05.
RESULTS
A total of 350 Iraqi immigrants responded to the survey. Of these, 145 persons had left Iraq before the 1991 GW, and 205 had left after the initiation of the GW. The pre-GW group was slightly but significantly older than the post-GW group (Table 1). The former group had also spent a longer time in the United States as compared with post-GW immigrants. As further depicted in Table 1, the pre-GW versus post-GW groups differed in a number of socioeconomic variables, except smoking. Thus, those in the post-GW group were more likely to be women, to have less educational attainment, to be unemployed, to have health insurance, and to have an annual income of US $10,000 or less.
Table 2 illustrates health conditions by immigration group. The post-GW group was significantly more likely to have physician-diagnosed and -treated obstructive sleep apnea than those who had arrived in the United States before the outbreak of the GW. However, groups did not differ as to when obstructive sleep apnea had been diagnosed, with 90% having been diagnosed after 1991. The post-GW group also reported a significantly higher prevalence of somatic and psychosomatic disorders.
TABLE 2.
Health Conditions by Immigration Group (Pre-1991 Versus Post-1991 Gulf War)
| Health Condition | Post-1991 (n = 205) | Pre-1991 (n = 145) | Total (N = 350) |
|---|---|---|---|
| SRH** | |||
| Excellent | 9 (4.4) | 21 (14.5) | 30 (8.6) |
| Very good | 19 (9.3) | 46 (31.7) | 65 (18.6) |
| Good | 55 (26.8) | 50 (34.5) | 105 (30.0) |
| Fair | 83 (40.5) | 26 (17.9) | 109 (31.1) |
| Poor | 39 (19) | 2 (1.4) | 41 (11.7) |
| Physician-diagnosed obstructive sleep apnea** | |||
| With sleep apnea | 62 (30.2) | 1 (0.7) | 63 (18.0) |
| Without sleep apnea | 143 (69.8) | 144 (99.3) | 287 (82.0) |
| Physician-diagnosed somatic disorders | |||
| Hypertension* | 43 (21.0) | 19 (13.1) | 62 (17.7) |
| Heart disease* | 11 (5.4) | 2 (1.4) | 13 (3.7) |
| Diabetes | 32 (15.6) | 16 (11.0) | 48 (13.7) |
| Physician-diagnosed psychosomatic disorders | |||
| Migraine** | 40 (19.5) | 4 (2.8) | 44 (12.6) |
| Chronic headache** | 71 (34.6) | 9 (6.2) | 80 (22.9) |
| Chronic fatigue** | 62 (30.2) | 18 (12.4) | 80 (22.9) |
| Musculoskeletal symptoms** | 132 (64.4) | 70 (48.3) | 202 (57.7) |
| Depression** | 78 (38.0) | 17 (11.7) | 95 (27.1) |
| PTSD** | |||
| Without PTSD | 181 (88.3) | 142 (97.9) | 323 (92.3) |
| With PTSD | 24 (11.7) | 3 (2.1) | 27 (7.7) |
Values are expressed as n (%).
χ2 was used for discrete variables.
SRH = self-rated health; PTSD = posttraumatic stress disorder.
p < .05.
p < .001.
Correlations among the variables used in SEM are shown in Table 3. The first seven variables in the table are the primary variables of interest. The proposed theoretical structural model for these variables is shown in Figure 1. The additional eight variables, starting with age, were added as covariates or control variables in SEM Models 3 and 4 (Table 4; Models 3 and 4).
TABLE 3.
Correlations, Means, and Standard Deviations for Variables Used in the Analysis
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Premigration trauma | 1.00 | 0.56 | 0.30 | 0.32 | 0.35 | −0.41 | −0.50 | 0.11 | −0.26 | 0.16 | |||||
| 2. PTSD | 0.56 | 1.00 | 0.31 | 0.36 | 0.33 | −0.35 | 0.30 | −0.36 | 0.12 | −0.20 | 0.16 | 0.16 | |||
| 3. Depression | 0.30 | 0.31 | 1.00 | 0.70 | 0.19 | 0.57 | −0.43 | −0.14 | −0.27 | 0.12 | −0.26 | −0.44 | 0.16 | ||
| 4. Sleep apnea | 0.32 | 0.36 | 0.70 | 1.00 | 0.14 | 0.63 | −0.35 | −0.15 | −0.13 | −0.19 | 0.14 | ||||
| 5. Somatic disorders | 0.05 | 0.06 | 0.19 | 0.11 | 1.00 | 0.22 | −0.33 | 0.33 | 0.15 | −0.11 | −0.17 | ||||
| 6. Psychosomatic disorders | 0.43 | 0.42 | 0.56 | 0.46 | 0.22 | 1.00 | −0.52 | −0.16 | −0.31 | 0.13 | −0.15 | −0.41 | 0.19 | −0.15 | |
| 7. SRH | −0.41 | −0.35 | −0.43 | −0.35 | −0.33 | −0.52 | 1.00 | −0.12 | 0.14 | 0.44 | −0.14 | 0.44 | −0.12 | ||
| 8. Age | −0.05 | 0.02 | 0.04 | 0.05 | 0.33 | 0.03 | −0.12 | 1.00 | 0.19 | 0.17 | |||||
| 9. Male | 0.02 | 0.30 | −0.14 | −0.15 | −0.06 | −0.16 | 0.14 | 0.03 | 1.00 | 0.45 | 0.38 | ||||
| 10. Years in the United States | −0.50 | −0.36 | −0.27 | −0.13 | −0.08 | −0.31 | 0.44 | 0.19 | 0.10 | 1.00 | 0.35 | −0.12 | |||
| 11. Married | 0.11 | 0.12 | 0.12 | 0.07 | 0.15 | 0.13 | −0.14 | 0.17 | −0.03 | −0.09 | 1.00 | −0.12 | 0.14 | ||
| 12. High school | −0.09 | −0.07 | −0.26 | −0.05 | −0.11 | −0.15 | 0.08 | −0.07 | 0.10 | 0.04 | 0.06 | 1.00 | 0.20 | ||
| 13. Employed | −0.26 | −0.20 | −0.44 | −0.19 | −0.17 | −0.41 | 0.44 | −0.02 | 0.45 | 0.35 | −0.12 | 0.20 | 1.00 | −0.18 | 0.19 |
| 14. Health insurance | 0.16 | 0.16 | 0.16 | 0.14 | 0.10 | 0.19 | −0.12 | 0.03 | −0.03 | −0.12 | 0.14 | −0.01 | −0.18 | 1.00 | −0.17 |
| 15. Smoker | 0.00 | 0.16 | −0.04 | −0.09 | 0.03 | −0.15 | 0.02 | 0.07 | 0.38 | 0.04 | 0.02 | −0.06 | 0.19 | −0.17 | 1.00 |
| Mean or proportion | 7.71 | 12.30 | 0.17 | 0.18 | 0.35 | 0.60 | 2.81 | 45.55 | 0.56 | 16.57 | 0.88 | 0.60 | 0.55 | 0.68 | 0.33 |
| Standard deviation | 10.23 | 19.18 | 0.38 | 0.39 | 0.61 | 0.97 | 1.13 | 7.46 | 0.50 | 9.96 | 0.33 | 0.49 | 0.50 | 0.47 | 0.47 |
Nonsignificant (p < .05) correlations are omitted in the upper triangular part of the table (N = 350).
Correlations in absolute values of 0.11 or larger are significant at p < .05. Correlations between dichotomous variables are Φ coefficients, and correlations between dichotomous variables and continuous variables are r point biserial correlations.
PTSD = posttraumatic stress disorder; SRH = self-rated health.
All together, four SEM models were fitted. The standardized path coefficients resulting from the fitting of the initial structural model are shown in Figure 1. Each of the pathways was significant, but the overall fit of this initial model was poor (Table 4, Model 1). Note that the path coefficients leading to depression, PTSD, somatic disorders, and psychosomatic disorders are simple correlation coefficients because, with a single predictor, path coefficients are standardized bivariate regression coefficients.
Examination of modification indices identified three additional structural paths and one covariance that were theoretically plausible and would improve model fit. The addition of these paths resulted in a good-fitting model (Table 4, Model 2). This model did not include potential confounders. To identify confounders, we added eight sociodemographic variables (age, sex, years in the United States, married, high school, employed, health insurance, and smoking status) to the model. Three of these—years in the United States, married, and health insurance—were omitted because they contributed no explanatory variance.
The resulting model is shown in Figure 3. All paths were significant, and the model fit well (Table 4, Model 4). Thus, the proposed structural model shown in Figure 1 held up after the addition of potential confounders and covariates. The strongest path in the model was the direct effect of depression on obstructive sleep apnea (standard path coefficient β = .66, p < .001). The direct effect of PTSD on obstructive sleep apnea was smaller but also significant (β = .16, p = .003). Several indirect effects are also of interest. The specific indirect effect of premigration trauma on obstructive sleep apnea through depression was small but significant (0.19 × 0.66 = 0.13, 95% confidence interval [CI] = 0.05 to 0.17, p = .039). The specific indirect effect of premigration trauma on obstructive sleep apnea through PTSD score was also significant and similar in magnitude (0.49 × 0.16 = 0.08, 95% CI = 0.042 to 0.13, p = .006). The total effect of obstructive sleep apnea on SRH through somatic and psychosomatic disorders was −0.15 (95% CI = −0.21 to −0.10, p = .012). The total effect of premigration trauma on obstructive sleep apnea was 0.21 (95% CI = 0.13 to 0.29, p = .012). Several covariate pathways emerged from the fitting of the model; obstructive sleep apnea, depression, premigration trauma, and smoking were predictive of psychosomatic disorders. Health conditions (somatic and psychosomatic), premigration trauma, and unemployment were predictive of poor SRH. Men were more likely to be employed, to have higher PTSD scores, and to be smokers than women. Employment emerged as a central covariate in this model. It was associated with premigration trauma, sex, education, depression, PTSD score, and SRH. The total effect of employment on obstructive sleep apnea was 0.11 (95% CI = 0.05 to 0.17), whereas the total effect of premigration trauma on obstructive sleep apnea was 0.21 (95% CI = 0.13 to 0.29).
DISCUSSION
This study of a random selection of 350 Iraqi Americans (205 had left Iraq after the initiation of the 1991 GW and the rest had left Iraq before the war) confirms prior studies on the adverse health effects of the war (28,29). Thus, persons who had emigrated from Iraq to the United States after the initiation of the war reported systematically worse physician-diagnosed outcomes for somatic, psychosomatic, and psychiatric disorders. Moreover, there was a direct path between premigration trauma exposure and depression and PTSD scores, which are recognized trauma-related disorders. There was a direct path between PTSD scores (significantly elevated among post-GW emigrants) and obstructive sleep apnea. This held true even after controlling for the effects of other risk factors, including sex and health insurance status. We included health insurance status in the model because it could be hypothesized that persons with health insurance might be more likely to visit a physician and be diagnosed as having obstructive sleep apnea should they experience it (30). Moreover, as reported in studies of non–war-exposed people, obstructive sleep apnea related to psychosomatic disorders and mental disorders, including headache, migraine, fatigue, and depression (31–33). To our knowledge, this is the first time that this possible mechanism has been demonstrated in a random sample of ethnically and culturally comparable immigrants to the same host country. The only difference in the current study is that one group was living in Iraq during and after the 1991 GW, whereas the other group left the country before the outbreak of the GW. As discussed above, participants who left Iraq after the outbreak of the 1991 GW reported significantly higher aggregate trauma exposure scores. This is in line with other studies reporting higher stressor exposures among those who left Iraq after the GW as opposed to those who left Iraq before the GW (16,17,34). In the current study, those who left Iraq after the eruption of the GW also scored significantly higher on the PTSD symptoms scale. Because the post-GW group was more likely to report physician-diagnosed and -treated obstructive sleep apnea, which had predominantly been diagnosed after the GW at which time the pre-GW group had already left Iraq, it is likely that environmental and trauma exposures in Iraq contributed to the increased rates of PTSD and sleep apnea in the post-GW group. Acculturation processes might have played a role because the post-GW group had spent substantially less number of years in the United States as compared with the pre-GW immigrants. However, as indicated in Table 3, the association between years spent in the United States and obstructive sleep apnea is rather low. Years in the United States did not add further to the explained variance and did not act as a significant covariate in the final model. Thus, PTSD might be an important causal mediator between trauma exposures and obstructive sleep apnea. Because the prevalence of PTSD in the current and prior studies of trauma- and war-exposed persons is typically higher as compared with non–war-related trauma studies, our study points to the importance of considering not just sleep disturbance, in general, among forcibly displaced persons but also the likelihood of obstructive sleep apnea in such persons when evaluating factors contributing to adverse somatic and mental health (12). Obstructive sleep apnea might potentiate the effects of trauma, sensitize the person against prior trauma owing to more frequent nightly awakenings, and attenuate recovery from PTSD and depression due to less restorative sleep as a consequence of obstructive sleep apnea (14).
A major strength of this study is the fact that it is based on a random sample of immigrants from Iraq to the United States. Most prior studies of war-exposed and non–war-exposed controls are based on convenience samples (18,19,35). Furthermore, our sample represents the same ethnic group, thus eliminating the possible effects of culture and country of origin on health measures. Structural interviews were carried out in Arabic by especially trained dual language–speaking Iraqi physicians residing in the United States. This allowed the physicians to complement medical history taking when warranted.
A shortcoming of the study is that we used physician-diagnosed and currently treated obstructive sleep apnea as the criterion for assigning a person with a diagnosis of obstructive sleep apnea. The optimal means to verify the diagnosis would be to carry out confirmatory polysomnographic studies. However, the interviewing physicians were able to follow up the structured medical interviews with additional questions in case there were reasons to suspect that a patient had other diseases (e.g., narcolepsy or central sleep apnea) rather than obstructive sleep apnea. Furthermore, we required that a person both had received the diagnosis of obstructive sleep apnea and was currently receiving treatment of this condition to be classified as having sleep apnea. This should further increase the validity of the diagnosis. Nevertheless, considering the possibility that many of the somatic and mental health symptoms common in war-exposed persons are partially related to obstructive sleep apnea, we suggest that future studies include confirmatory polysomnographic studies. Even though the frequency of obstructive sleep apnea seems high in the post-GW group, there is little reason to believe that there has been differential misclassification of sleep apnea between the groups that left Iraq before and after the GW. It is also important not to view obstructive sleep apnea as a simple peripheral disease due to a weakening of the muscular tonus of the pharynx. It is plausible that stress-associated centrally mediated factors contribute to peripheral neuromuscular changes (14).
Because obesity has been associated with obstructive sleep apnea, it is possible that the post-1991 immigrants were more obese than the pre-1991 immigrants. In the current study, we did not have access to anthropometric data. However, in an ongoing study of a random sample of approximately 600 Iraqi refugees and Arab immigrant controls residing in Michigan, we found no statistically significant differences in body mass index between the groups (mean [standard deviation] body mass index = 26.3 [5.0] in refugees versus 25.5 [9.5] in immigrant controls; p between groups = not significant). However, using a body mass index cutoff higher than 30 kg/m2 to classify a person as obese, we classified 19.5% of refugees versus 11.8% of immigrants as obese (Pearson χ2 = 6.4, df = 1, p = .011). We do not believe that this relatively minor difference in the prevalence of obesity between groups could explain the substantial differences in sleep apnea between pre-GW and post-GW immigrants in the current study.
Another argument might be that persons arriving after the eruption of the GW have been more thoroughly evaluated and diagnosed. However, we controlled for health insurance status, years in the United States, and period of immigration. Furthermore, our exposure variable was “exposed versus not exposed to the GW,” something that might have introduced a systematic misclassification or recall bias. Rather, we used a composite premigration trauma exposure score that was not specifically tied to the outbreak of the GW and thus less likely to be systematically biased.
It is well known that sleep disorders lead to psychosomatic problems in immigrants and nonimmigrants (36–38). However, the mechanisms behind this relationship remain unknown. We developed a structural equation model to further explore these relationships. We found that obstructive sleep apnea had a strong direct effect on psychosomatic disorders, in line with other studies (39).
As reported by others as well, obstructive sleep apnea was predictive of somatic disorders in our model (40–42).
Health conditions (somatic and psychosomatic), immigration before or after the GW, premigration trauma scores, and unemployment were predictive of poor SRH, in line with other studies (43,44).
CONCLUSIONS
This structured interview study of Iraqis who left their country before and after the outbreak of the 1991 GW revealed that physician-diagnosed and -treated obstructive sleep apnea is a contributing factor to psychosomatic disorders and lower SRH in the latter group. Somatic and psychosomatic disorders are highly prevalent among immigrants, in general, and refugees, in particular. Immigration, war-related environmental and psychological trauma, and stressor exposures contribute to such findings. Our results also have implications for efforts to improve the overall health of immigrants and war-exposed persons through early health screening for obstructive sleep apnea, which can be treated. This would in turn likely lower the risk for psychosomatic disorders and poor general health and lead to better performance and integration of refugees and immigrants with trauma-related disorders.
Acknowledgments
B. B. Arnetz and H. Jamil were supported, in part, by Award R01MH085793 from the National Institute of Mental Health, National Institutes of Health (NIH). B. B. Arnetz was further supported, in part, by Award 1R34MH086943-01 from the National Institute of Mental Health, NIH. Pfizer Corporation provided financial support for collection of original survey data.
Glossary
- SRH
self-rated health
- SEM
structural equation modeling
- PTSD
posttraumatic stress disorder
- ML
maximum likelihood
- CFI
comparative fit index
- RMSEA
root mean square error of approximation
- ANOVA
Analysis of variance
Footnotes
The authors declare no conflict of interests.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the NIH.
References
- 1.Jamil H, Hakim-Larson J, Farrag M, Kafaji T, Jamil LH, Hammad A. Medical complaints among Iraqi American refugees with mental disorders. J Immigr Health. 2005;7:145–52. doi: 10.1007/s10903-005-3671-z. [DOI] [PubMed] [Google Scholar]
- 2.Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, Hassan G, Rousseau C, Pottie K. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183:E959–67. doi: 10.1503/cmaj.090292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farley T, Galves A, Dickinson LM, de Perez MJ. Stress, coping, and health: a comparison of Mexican immigrants, Mexican-Americans, and non-Hispanic whites. J Immigr Health. 2005;7:213–20. doi: 10.1007/s10903-005-3678-5. [DOI] [PubMed] [Google Scholar]
- 4.Gong F, Xu J, Fujishiro K, Takeuchi DT. A life course perspective on migration and mental health among Asian immigrants: the role of human agency. Soc Sci Med. 2011;73:1618–26. doi: 10.1016/j.socscimed.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Aviram A, Silverberg DS, Carel RS. Hypertension in European immigrants to Israel—the possible effect of the holocaust. Isr J Med Sci. 1987;23:257–63. [PubMed] [Google Scholar]
- 6.Kaplan MS, Chang C, Newsom JT, McFarland BH. Acculturation status and hypertension among Asian immigrants in Canada. J Epidemiol Community Health. 2002;56:455–6. doi: 10.1136/jech.56.6.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kinzie JD, Riley C, McFarland B, Hayes M, Boehnlein J, Leung P, Adams G. High prevalence rates of diabetes and hypertension among refugee psychiatric patients. J Nerv Ment Dis. 2008;196:108–12. doi: 10.1097/NMD.0b013e318162aa51. [DOI] [PubMed] [Google Scholar]
- 8.Porsch-Oezcueruemez M, Bilgin Y, Wollny M, Gediz A, Arat A, Karatay E, Akinci A, Sinterhauf K, Koch H, Siegfried I, von Georgi R, Brenner G, Kloer HU. Prevalence of risk factors of coronary heart disease in Turks living in Germany: The Giessen Study. Atherosclerosis. 1999;144:185–98. doi: 10.1016/s0021-9150(99)00054-4. [DOI] [PubMed] [Google Scholar]
- 9.Uppaluri CR, Schumm LP, Lauderdale DS. Self-reports of stress in Asian immigrants: effects of ethnicity and acculturation. Ethn Dis. 2001;11:107–14. [PubMed] [Google Scholar]
- 10.Kinzie JD. Immigrants and refugees: the psychiatric perspective. Transcult Psychiatry. 2006;43:577–91. doi: 10.1177/1363461506070782. [DOI] [PubMed] [Google Scholar]
- 11.Sorkin D, Tan A, Hays R, Mangione C, Ngo-Metzger Q. Self-reported health status of Vietnamese and non-Hispanic white older adults in California. J Am Geriatr Soc. 2008;8:1543–8. doi: 10.1111/j.1532-5415.2008.01805.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colman MF. Sudden nocturnal death in Southeast Asian refugees. JAMA. 1987;257:1473. [PubMed] [Google Scholar]
- 13.Veber OA, Dunai A, Novak M, Mucsi I. Links between diabetes mellitus and sleep disorders: focusing on obstructive sleep apnea. Orv Hetil. 2010;151:8–16. doi: 10.1556/OH.2010.28676. [DOI] [PubMed] [Google Scholar]
- 14.Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev. 2008;12:185–95. doi: 10.1016/j.smrv.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jamil H, Hamdan TA, Grzybowski M, Arnetz BB. Health effects associated with geographical area of residence during the 1991 Gulf War: a comparative health study of Iraqi soldiers and civilians. US Army Med Dep J. 2011:87–96. [PMC free article] [PubMed] [Google Scholar]
- 17.Jamil H, Nassar-McMillanb S, Lambert R, Wangd Y, Ager J, Arnetz B. Pre- and post-displacement stressors and time of migration as related to self-rated health among Iraqi immigrants and refugees in Southeast Michigan. Med Confl Surviv. 2010;26:207–22. doi: 10.1080/13623699.2010.513655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keller A, Lhewa D, Rosenfeld B, Sachs E, Aladjem A, Cohen I, Smith H, Porterfield K. Traumatic experiences and psychological distress in an urban refugee population seeking treatment services. J Nerv Ment Dis. 2006;194:188–94. doi: 10.1097/01.nmd.0000202494.75723.83. [DOI] [PubMed] [Google Scholar]
- 19.Porter M. Global evidence for a biopsychosocial understanding of refugee adaptation. Transcult Psychiatry. 2007;44:418–39. doi: 10.1177/1363461507081639. [DOI] [PubMed] [Google Scholar]
- 20.Barrett DH, Doebbeling CC, Schwartz DA, Voelker MD, Falter KH, Woolson RF, Doebbeling BN. Posttraumatic stress disorder and self-reported physical health status among U.S. Military personnel serving during the Gulf War period: a population-based study. Psychosomatics. 2002;43:195–205. doi: 10.1176/appi.psy.43.3.195. [DOI] [PubMed] [Google Scholar]
- 21.Self-reported illness and health status among Gulf War veterans. A population-based study. The Iowa Persian Gulf Study Group. JAMA. 1997;277:238–45. [PubMed] [Google Scholar]
- 22.Hasson D, Arnetz BB, Theorell T, Anderberg UM. Predictors of self-rated health: a 12-month prospective study of IT and media workers. Popul Health Metrics. 2006;4:8. doi: 10.1186/1478-7954-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halford C, Anderzen I, Arnetz B. Endocrine measures of stress and self-rated health: a longitudinal study. J Psychosom Res. 2003;55:317–20. doi: 10.1016/s0022-3999(02)00634-7. [DOI] [PubMed] [Google Scholar]
- 24.Joreskog KG. Modeling development: using covariance structure models in longitudinal research. Eur Child Adolesc Psychiatry. 1996;5:8–10. doi: 10.1007/BF00538536. [DOI] [PubMed] [Google Scholar]
- 25.Babyak MA, Green SB. Confirmatory factor analysis: an introduction for psychosomatic medicine researchers. Psychosom Med. 2010;72:587–97. doi: 10.1097/PSY.0b013e3181de3f8a. [DOI] [PubMed] [Google Scholar]
- 26.Bentler PM, Stein JA. Structural equation models in medical research. Stat Methods Med Res. 1992;1:159–81. doi: 10.1177/096228029200100203. [DOI] [PubMed] [Google Scholar]
- 27.Marsh H, Hau K, Wen Z. In search of golden rules: comments on hypothesis-testing approaches and setting cutoff values for fit indexes and dangers of overgeneralizing Hu and Bentler’s (1999) findings. Struct Equation Model. 2004;11:320–41. [Google Scholar]
- 28.Jamil H, Hakim-Larson J, Farrag M, Kafaji T, Duqum I, Jamil LH. A retrospective study of Arab American mental health clients: trauma and the Iraqi refugees. Am J Orthopsychiatry. 2002;72:355–61. doi: 10.1037/0002-9432.72.3.355. [DOI] [PubMed] [Google Scholar]
- 29.Black DW, Carney CP, Peloso PM, Woolson RF, Schwartz DA, Voelker MD, Barrett DH, Doebbeling BN. Gulf War veterans with anxiety: prevalence, comorbidity, and risk factors. Epidemiology. 2004;15:135–42. doi: 10.1097/01.ede.0000103188.18059.21. [DOI] [PubMed] [Google Scholar]
- 30.Sole-Auro A, Guillen M, Crimmins EM. Health care usage among immigrants and native-born elderly populations in eleven European countries: results from SHARE. Eur J Health Econ. 2011 doi: 10.1007/s10198-011-0327-x. Epub 2011/06/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beating the blues by treating sleep apnea. Obstructive sleep apnea and depression: treating the sleep problem may boost mood. Harv Ment Health Lett. 2007;24:4–5. [PubMed] [Google Scholar]
- 32.Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, Majima T, Horie T. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122:861–5. doi: 10.1378/chest.122.3.861. [DOI] [PubMed] [Google Scholar]
- 33.Assoumou HG, Gaspoz JM, Sforza E, Pichot V, Celle S, Maudoux D, Kossovsky M, Chouchou F, Barthelemy JC, Roche F. Obstructive sleep apnea and the metabolic syndrome in an elderly healthy population: the SYNAPSE cohort. Sleep Breath. 2012;16:895–902. doi: 10.1007/s11325-011-0593-y. [DOI] [PubMed] [Google Scholar]
- 34.Jamil H, Nassar-McMillan SC, Lambert RG. Immigration and attendant psychological sequelae: a comparison of three waves of Iraqi immigrants. Am J Orthopsychiatry. 2007;77:199–205. doi: 10.1037/0002-9432.77.2.199. [DOI] [PubMed] [Google Scholar]
- 35.Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294:602–12. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- 36.Andrews JG, Oei TP. The roles of depression and anxiety in the understanding and treatment of obstructive sleep apnea syndrome. Clin Psychol Rev. 2004;24:1031–49. doi: 10.1016/j.cpr.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 37.Briones B, Adams N, Strauss M, Rosenberg C, Whalen C, Carskadon M, Roebuck T, Winters M, Redline S. Relationship between sleepiness and general health status. Sleep. 1996;19:583–8. doi: 10.1093/sleep/19.7.583. [DOI] [PubMed] [Google Scholar]
- 38.Buysse DJ, Grunstein R, Horne J, Lavie P. Can an improvement in sleep positively impact on health? Sleep Med Rev. 2010;14:405–10. doi: 10.1016/j.smrv.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 39.Kjelsberg FN, Ruud EA, Stavem K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005;6:341–6. doi: 10.1016/j.sleep.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Jean-Louis G, Brown CD, Zizi F, Ogedegbe G, Boutin-Foster C, Gorga J, McFarlane SI. Cardiovascular disease risk reduction with sleep apnea treatment. Expert Rev Cardiovasc Ther. 2010;8:995–1005. doi: 10.1586/erc.10.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Juuti AK, Hiltunen L, Rajala U, Laakso M, Harkonen P, Hedberg P, Ruikonen A, Keinänen-Kiukaanniemi S, Läärä E. Association of abnormal glucose tolerance with self-reported sleep apnea among a 57-year-old urban population in Northern Finland. Diabetes Res Clin Pract. 2008;80:477–82. doi: 10.1016/j.diabres.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Keckeis M, Lattova Z, Maurovich-Horvat E, Beitinger PA, Birkmann S, Lauer CJ, Wetter TC, Wilde-Frenz J, Pollmächer T. Impaired glucose tolerance in sleep disorders. PLoS One. 2010;5:e9444. doi: 10.1371/journal.pone.0009444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arnetz BB, Wasserman J, Petrini B, Brenner SO, Levi L, Eneroth P, Salovaara H, Hjelm R, Salovaara L, Theorell T, Petterson I-L. Immune function in unemployed women. Psychosom Med. 1987;49:3–12. doi: 10.1097/00006842-198701000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Brenner SO, Arnetz B, Levi L, Petterson IL. Health and well-being of unemployed women. Nord Med. 1988;103:47. [PubMed] [Google Scholar]