Abstract
Aim
The aim was to determine if the University of Minnesota (MN, USA) healthcare students’ perceived value of pharmacogenomics matches their self-observed comfort and education in pharmacogenomics.
Materials & methods
A 24-question, anonymous, online survey was distributed to all pharmacy, nursing and medical students enrolled at the University of Minnesota.
Results
Among healthcare students, 70.6% agreed or strongly agreed that pharmacogenomics should be an important part of their curriculum; however, only 11.1% agreed or strongly agreed that it actually is. Only 29.7% of students reported taking a genetics course that specifically addressed the applications of genetics in pharmacy, and those students were more likely to feel comfortable interpreting information from a pharmacogenetics test, answering questions on pharmacogenomics, educating patients on risks and benefits of testing, and were comfortable that they knew which medications required pharmacogenomics testing.
Conclusion
Healthcare students consider pharmacogenomics to be an important area of clinical practice; yet generally express it has not been an important part of their curriculum. Education emphasizing medical applications of pharmacogenomics can increase student comfort level in pharmacogenomics practice.
Keywords: curriculum, education, healthcare, pharmacogenetics, pharmacogenomics, pharmacy, student, survey
Pharmacogenomics is an exploding field of science that explores genetic contributions to patient variability in drug response [1]. It combines our knowledge of drug pharmacokinetics and pharmacodynamics with knowledge from modern genetic testing to provide a comprehensive view of how a specific patient will react to a medication [2]. Pharmacogenomics can enable healthcare practitioners to predict who will respond to a medication, who will not, what dose to select and who may have an adverse drug reaction to the medication [101,102]. Advancements in this field are key to practicing personalized medicine and the ultimate goal is to optimize drug efficacy, prevent toxicity and reduce overall medical costs [3]. With the knowledge of how genetic variation affects drug response, treatments can begin to be reliably tailored to the individual [103].
Over a century ago, it was recognized that genetic factors play a role in drug response, and the concept and its practice have been evolving ever since [4,5]. In 2003, the Human Genome Project was completed, which threw open the doors to pharmacogenomics exploration. Shortly after, in 2007, the US FDA added pharmacogenomics information to the warfarin label [1,4,102]. More recently, clopidogrel received a black box warning pertaining to patients genetic information [1,4,102]. Today, nearly 100 medications contain pharmacogenetic information on their drug labels, and the FDA has mandated pharmacogenomics testing for medications such as trastuzumab, cetuximab, maraviroc and more [1,102]. DNA-sequencing technology is perpetually evolving, and may soon enable genetic screening in a doctor’s office to be commonplace [104]. The addition of pharmacogenomics information into drug labels, coupled with increased availability of genetic research and testing, has contributed to the evolution of pharmacogenomics from research to clinical practice [2].
With the ever-increasing amount of pharmacogenomic applications and requirements, healthcare practitioners and educators face the challenge of keeping up. The National Coalition for Health Professional Education in Genetics (NCHPEG) has established core competencies expected of all healthcare professionals; associations representing individual specialties have also followed suit [105]. In 2002, the Academic Affairs Committee of the American Association of Colleges of Pharmacy (AACP) recommended that pharmacy schools incorporate pharmacogenomics into their curricula to educate future practitioners in core competencies necessary for pharmacogenomics practice [6]. In 2005 the American College of Physicians (ACP) acknowledged that it was increasingly important for physicians to be knowledgeable about genetic testing and counseling, and in 2006 the American Nurses Association (ANA) established genetic competencies for nurses recommended for use in nursing education [7,106].
Despite the outstanding amount of evidence promoting pharmacogenomics practice and education, many healthcare practitioners continue to feel inadequate in the field. Studies show that practitioners continue to lack confidence and education in pharmacogenomics [1,8]. In order to continue optimizing patient care, the USA needs to provide the practitioners of tomorrow with the basic education necessary to practice relevant medical fields. While practicing health-care professionals have raised concerns about the clinical importance but limited knowledge of pharmacogenomics, there is little knowledge of student opinions on pharmacogenomics and their perceived education and knowledge of its practice.
This survey was designed to assess whether the University of Minnesota (UMN; MN, USA) healthcare student’ professional worth of pharmacogenomics matched the self-understood knowledge, comfort and education in pharmacogenomics. The secondary goal in this survey was to illustrate which specialty of healthcare students assumed more responsibility for pharmacogenomics within their profession.
Materials & methods
All pharmacy, nursing and medical students at the UMN were selected to receive an invitation to an anonymous, self-administered, online survey consisting of 24 questions (supplementary material; see www.futuremedicine.com/doi/suppl/10.2217/pgs.12.139). Prior to initiation, the study received institutional review board exemption from the UMN and was assigned study number 1108E03461. Survey questions were developed with consideration of the NCHPEG core competencies required for healthcare professionals, consideration of outcomes of the Assessment of the Pharmacogenomics Educational Needs of Pharmacists study published in the American Journal of Pharmaceutical Education in 2011, and educational recommendations from the AACP, ANA and ACP [1,6,7,106].
Survey questions were consistent across medical, nursing and pharmacy students apart from individualizing survey questions to address medical students/physicians, nursing students/ nurses and pharmacy students/pharmacists. The survey consisted of demographic questions and three clusters of focus. Demographic questions were multiple choice and short answer, while clusters of focus responses were based on a five-point Likert scale: strongly disagree, disagree, neutral, agree or strongly agree. The first cluster evaluated students perceived relevance of pharmacogenomics. The second cluster evaluated what pharmacogenomics skills students understood to be necessary once in clinical practice and the third cluster identified students’ comfort level in pharmacogenomics.
The target population included medical, nursing and pharmacy students enrolled at the UMN. Members were identified and contacted through student LISTSERVs. Access to LISTSERVs was obtained through contact and approval from each school of study’s individual LISTSERV administrator. A survey invitation including the study title, the title of the investigator and a website link to the online survey was sent in electronic mail format to each student. Students were informed in the invitation that the study was crucial to the investigator’s fourth year pharmacy student thesis and responses would be anonymous and would not affect their academic standing.
Response rate bias was expected, as students with strong opinions on pharmacogenomics may have more personal incentive to participate in the survey. To limit this bias, students were informed they could enter their e-mails into a random drawing for a US$20 Target gift card upon survey completion. To maintain anonymity, e-mail entries were not attached to the survey the student had completed. In addition, to further limit bias, the survey and invitation did not contain a definition of pharmacogenomics.
Medical student LISTSERVs consisted of a total of 887 contacts, pharmacy LISTSERVs contained 722 contacts and nursing contained 806. The total number of subjects invited to participate was 2415. A reminder e-mail was sent to pharmacy and nursing students several days before survey close. Medical student LISTSERV administrators refused reminder e-mails. Surveys were closed 13 days after release.
Incomplete surveys were thrown out of study results. The percentage of students who responded ‘yes’ to having taken post-high school genetics coursework and genetics coursework with applications in pharmacy was compared across student comfort level in pharmacogenomics using χ2 analysis to a 95% CI of 3.66.
Results
A total of 2415 survey invitations were distributed. In total, 217 (27%) nursing subjects completed the electronic surveys and 578 (71.7%) did not respond. Two nursing respondents reported that they were not students and so their answers were not considered in study results. In total, 328 (45.4%) pharmacy students completed the survey and 379 (52.5%) did not respond. A total of 170 (19.2%) medical students completed the survey and 712 (80.3%) did not respond. Overall, 715 (29.6%) students completed the survey and 1669 (69.1%) did not respond. Incomplete surveys were excluded from study results.
The majority (35%) of nursing students were in the DNP program and the largest portion (71%) had worked in hospital healthcare settings. The majority (59%) of nursing students had not taken a genetics course in their post-high school career and, of those that had, only 43% stated the course had included information on the applications of genetics in pharmacy.
The majority (31.2%) of medical students were in the second year of the medical program, and the largest amount (81.8%) had work experience in a hospital setting. Impressively, almost all (95.3%) had taken a genetics course in their post-high school career, and 67.3% of those respondents reported the course included information about the applications of genetics in pharmacy.
The majority of pharmacy students were in the first (27%) and second years (27%) of the pharmacy program and the largest amount (80%) of students had work experience in a community/retail setting. Most (66%) had taken a genetics course in their post-high school career; however, only 30% of those respondents reported the course included information about the applications of genetics in pharmacy. Overall, only 29.7% of all healthcare student respondents reported taking a genetics course that specifically addressed the applications of genetics in pharmacy. Participant demographics are listed in Table 1.
Table 1.
Demographic information for participating nursing, medical and pharmacy students at the University of Minnesota.
| Demographic | Pharmacy student, n (%) | Nursing student, n (%) | Medical student, n (%) | Total healthcare student, n (%) |
|---|---|---|---|---|
| Academic year | ||||
| Undergraduate | 0 (0) | 7 (3) | 0 (0.0) | 7 (1.0) |
| PhD | 0 (0) | 11(5) | 2 (1.2) | 13 (1.8) |
| Residency | 0 (0) | 0 (0) | 1 (0.6) | 1 (0.0) |
| PharmD year 1 | 88 (27) | – | – | 88 (12.3) |
| PharmD year 2 | 88 (27) | – | – | 88 (12.3) |
| PharmD year 3 | 73 (22) | – | – | 73 (10.2) |
| PharmD year 4 | 79 (24) | – | – | 79 (11.0) |
| Nursing year 1 | – | 1 (0) | – | 1 (0.0) |
| Nursing year 2 | – | 42 (19) | – | 42 (5.9) |
| Nursing year 3 | – | 30 (14) | – | 30 (4.2) |
| MN nursing | – | 43 (20) | – | 43 (6.0) |
| MSN nursing | – | 6 (3) | – | 6 (0.8) |
| DNP | – | 77 (35) | – | 77 (10.8) |
| Medicine year 1 | – | – | 31 (18.2) | 31 (4.3) |
| Medicine year 2 | – | – | 53 (31.2) | 53 (7.4) |
| Medicine year 3 | – | – | 42 (24.7) | 42 (5.9) |
| Medicine year 4 | – | – | 41 (24.1) | 41 (5.7) |
| Work experience | ||||
| Community/retail | 251 (80) | 66 (31) | 46 (27.0) | 363 (50.8) |
| Hospital | 140 (45) | 150 (71) | 139 (82.0) | 429 (60.0) |
| Ambulatory/outpatient | 41 (13) | 69 (33) | 114 (67.0) | 224 (31.3) |
| Research/industry | 52 (17) | 22 (10) | 76 (45.0) | 150 (21.0) |
| Other | 26 (8) | 54 (26) | 11 (2.0) | 91 (12.7) |
| Genetics academia | ||||
| Took a genetics course in post-high school career | 218 (66) | 88 (41) | 162 (95.0) | 468 (65.5) |
| Genetics course included information about the applications of genetics in pharmacy | 65 (20) | 38 (18) | 109 (64.0) | 212 (29.7) |
Total respondents = 715.
–: Not included in survey; specific to this student population.
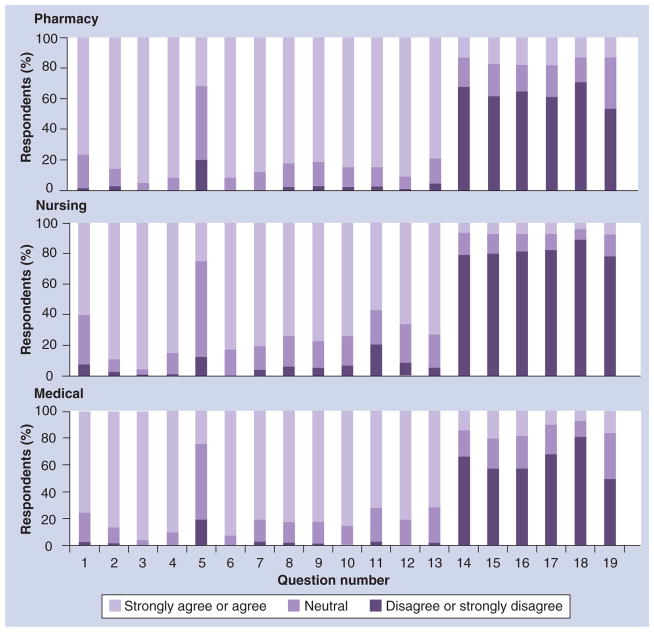
The first cluster of the survey evaluated students’ perceived relevance of pharmacogenomics. A total of 75.31% of pharmacy students agreed or strongly agreed that pharmacogenomics should be an important part of their curriculum; however, only 13.1% agreed or strongly agreed that pharmacogenomics had been and important part of the curriculum. In fact, over half of the pharmacy student respondents disagreed or strongly disagreed that pharmacogenomics had been an important part of their curriculum (Figure 1). In addition, over 90% of pharmacy students agreed or strongly agreed that pharmacogenomics could improve patient care. Results for the first cluster were similar for nursing students, with 59.9% agreeing or strongly agreeing and only 7.8% disagreeing or strongly disagreeing that pharmacogenomics should be an important part of their school curriculum. Only 7.4% of nursing students felt pharmacogenomics had been important in their nursing school curriculum, while 84.8% agreed or strongly agreed that it could improve patient care. Similarly, the vast majority (75.3%) of medical students agreed or strongly agreed that pharmacogenomics should be an important part of the curriculum, while only 2.9% disagreed or strongly disagreed with this statement. Only 15.9% of medical students agreed or strongly agreed the subject had been an important part of their school curriculum; however, 90% agreed or strongly agreed pharmacogenomics can improve patient care and no medical students disagreed with this statement. Curriculum opinions are represented in Figure 1.
Figure 1. Student opinions on pharmacogenomics inclusion in their healthcare curriculum.
†‘Pharmacy’, ‘nursing’ or ‘medical’ was inserted at __________ specific to the appropriate school to which each survey was distributed.
The second cluster assessed pharmacogenomics skills students understood to be necessary. A large majority of pharmacy (88.1%), medical (80.6%) and nursing students (80.1%) agreed or strongly agreed that their profession should be required to have some knowledge of pharmacogenomics. A greater amount of pharmacy (91.2%), medical (80.6%) and nursing students (65.7%) agreed or strongly agreed that once in practice, they should be able to identify medications requiring genetic testing.
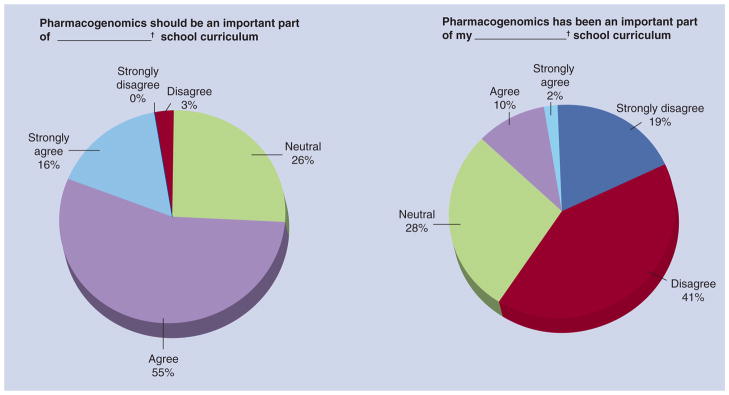
The final cluster identified students’ comfort level in pharmacogenomics. In total, 57.6% of medical, 61.9% of pharmacy and 80.2% of nursing students disagreed or strongly disagreed with a statement that they were comfortable answering questions on pharmacogenomics. In response to the statement that the student knew which medications require pharmacogenomics testing, 70.7% of pharmacy, 80.6% of medical and 89.4% of nursing students disagreed or strongly disagreed. In fact, only 3.7% nursing, 7% medical and 12.8% of pharmacy students agreed or strongly agreed they knew which medications required pharmacogenomics testing. Comprehensive cluster survey responses for collective and individual areas of study are listed in Table 2, Figure 2 & supplementary Tables 1, 2 & 3.
Table 2.
Healthcare student participants’ comprehensive responses to survey.
| Survey question | Strongly disagree, n (%) | Disagree, n (%) | Neutral, n (%) | Agree, n (%) | Strongly agree, n (%) |
|---|---|---|---|---|---|
| 1 Pharmacogenomics should be an important part of _____† school curriculum | 4 (0.56) | 23 (3.21) | 183 (25.56) | 391 (54.61) | 115 (16.06) |
| 2 Pharmacogenomics is relevant to current medical practice | 2 (0.28) | 15 (2.09) | 76 (10.61) | 450 (62.85) | 173 (24.16) |
| 3 Pharmacogenomics will be relevant in future medical practice | 1 (0.14) | 3 (0.42) | 29 (4.05) | 341 (47.63) | 342 (47.77) |
| 4 Pharmacogenomics can improve patient care | 1 (0.14) | 2 (0.28) | 74 (10.34) | 416 (58.10) | 223 (31.15) |
| 5 Pharmacogenomics is cost effective | 9 (1.26) | 117 (16.34) | 391 (54.61) | 153 (21.37) | 46 (6.42) |
| 6 Pharmacogenomics can aid in optimizing medication therapy | 0 (0.00) | 3 (0.42) | 74 (10.34) | 400 (55.87) | 239 (33.38) |
| 7 _____‡ should be required to have some comprehension of pharmacogenomics | 2 (0.28) | 14 (1.96) | 99 (13.83) | 456 (63.69) | 145 (20.25) |
| 8 Once in practice, I should be able to answer patient questions on pharmacogenomics | 1 (0.14) | 24 (3.35) | 120 (16.76) | 462 (64.53) | 109 (15.22) |
| 9 Once in practice, I should be able to educate patients on the risks and benefits of pharmacogenomics testing | 1 (0.14) | 23 (3.21) | 118 (16.48) | 461 (64.39) | 113 (15.78) |
| 10 Once in practice, I should be able to identify patients that could benefit from pharmacogenomics testing | 1 (0.14) | 21 (2.93) | 110 (15.36) | 465 (64.94) | 119 (16.62) |
| 11 Once in practice, I should be able to provide drug therapy recommendations based on previously obtained patient genetic information | 5 (0.70) | 53 (7.40) | 134 (18.72) | 403 (56.28) | 121 (16.90) |
| 12 Once in practice, I should be able to identify medications that require pharmacogenomics testing | 2 (0.28) | 20 (2.79) | 114 (15.92) | 428 (59.78) | 152 (21.23) |
| 13 I should have access to my patients pharmacogenetic information in clinical practice | 2 (0.28) | 29 (4.05) | 146 (20.39) | 421 (58.80) | 118 (16.48) |
| 14 I am comfortable interpreting information from a pharmacogenomics test | 193 (26.96) | 314 (43.85) | 130 (18.16) | 68 (9.50) | 11 (1.54) |
| 15 I am comfortable answering questions on pharmacogenomics | 162 (22.63) | 313 (43.72) | 135 (18.85) | 97 (13.55) | 9 (1.26) |
| 16 I am comfortable educating patients on the risks and benefits of pharmacogenomics testing | 173 (24.16) | 314 (43.85) | 124 (17.32) | 97 (13.55) | 8 (1.12) |
| 17 I can apply information from a pharmacogenomics test to medication selection, dosing or monitoring for a patient | 208 (29.05) | 288 (40.22) | 129 (18.02) | 84 (11.73) | 7 (0.98) |
| 18 I know which medications require pharmacogenomics testing | 230 (32.12) | 334 (46.65) | 90 (12.57) | 60 (8.38) | 2 (0.28) |
| 19 Pharmacogenomics has been an important part of my _____† school curriculum | 139 (19.41) | 291 (40.64) | 199 (27.79) | 75 (10.47) | 12 (1.68) |
Insert ‘pharmacy’, ‘nursing’ or ‘medical’; particular to specific student population.
Insert ‘pharmacists’, ‘nurses’ or ‘physicians’; particular to specific student population.
Figure 2. Comprehensive responses to survey questions represented as percentage for pharmacy, nursing and medical students from the University of Minnesota.
Questions 1–19 represented on X-axis are in same order as questions indicated in Table 2.
In addition, healthcare students who had a class outlining the applications of genetics in pharmacy agreed or strongly agreed to comfort-level cluster questions more often than those that did not have a class in the genetics of pharmacy and were more likely to feel comfortable interpreting and answering questions on pharmacogenomics (Figure 3a) as well as trended towards knowing which medications required pharmacogenomics testing (Figure 3b).
Figure 3. Pharmacogenomics comfort level in healthcare students with and without a genetics course in their post-high school career.
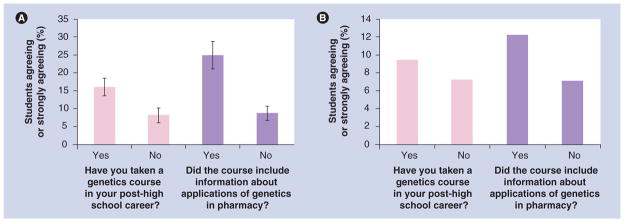
(A) Percentage of students with or without a genetics course in their post-high school career (light gray) and whether or not the course included information about applications of genetics in pharmacy (dark gray) agreeing or strongly agreeing to four questions related to their comfort level in: interpreting information of pharmacogenomics test; answering questions on pharmacogenomics; educating patients on risks and benefits of pharmacogenomics testing; and ability to apply information from pharmacogenomics test to medication selection, dosing or monitoring. (See Table 2 questions 14–17). Bars represent average of percentage response in each category for the four questions. (B) Percentage of students with or without a genetics course in their post-high school career (light gray) and whether or not the course included information about applications of genetics in pharmacy (dark gray) agreeing or strongly agreeing to a question on knowing medications that require pharmacogenomics testing (See Table 2 question 18).
Discussion
Over the past decade, the field of pharmacogenomics has expanded significantly and could be considered one of the most immediate clinical benefits from the Human Genome Project [9]. It is quickly becoming an important part of health-care and students and practitioners are beginning to recognize it. Previous studies have demonstrated current healthcare practitioners consider pharmacogenomics to be a relevant field of clinical practice, and this study has demonstrated healthcare students agree that pharmacogenomics is important to patient care [1,8].
Although multiple healthcare associations specifically recommend specific genetic education for professionals, pharmacogenomics education remains highly variable from program to program. For example; a study published in the American Journal of Pharmaceutical Education in 2010 demonstrated that 69 out of 75 responding pharmacy schools were currently providing pharmacogenomics education to their students; however, the study also identified that the pharmacogenomics instruction was currently inconsistent in devoted didactic hours between schools and less than half of the colleges were planning to increase hours dedicated to pharmacogenomics instruction [10]. Such findings are representative of healthcare curriculums at the UMN. The UMN is home to the third-ranked pharmacy program according to the US News and World Report [107], and also have well-respected medical and nursing programs [108]; however, the pharmacy program offers pharmacogenomics only as an elective course with very little subject education built into other coursework [109].
A 2010 Mayo Clinic (MN, USA) survey of practicing pharmacists explored similar clusters of perception, but among practicing pharmacists [1]. The study also found that practitioners believe knowledge of pharmacogenomics is important for pharmacy practice; however, they lack knowledge and self confidence in the subject [1]. This suggests that absent pharmacogenomics education in healthcare schools is carrying on into clinical practice, even though students and practitioners alike have acknowledged the clinical relevance of pharmacogenomics.
This study demonstrated pharmacy, nursing and medical students at the UMN consider pharmacogenomics to be an important and relevant area of clinical practice; yet students generally express it has not been an important part of their curriculum. The survey also demonstrated that, across the board, healthcare students believe that they should have the knowledge to use genetic information to make drug therapy decisions and educate patients. However, students have a lack of confidence in their pharmacogenomics skills and abilities. The disparity between the pharmacogenomics skills current and future practitioners need and the skills they have is concerning as this next frontier of medical practice is explored. Students who have had didactic education in pharmacogenomics are significantly more comfortable in identifying and using pharmacogenomics than their peers.
In addition, this study identified that pharmacy students may assume more professional responsibility for pharmacogenomics. The survey response rate was higher among pharmacy students than other healthcare students, indicating that they may have a stronger opinion on this subject. Pharmacy students were also more likely than any other students to agree or strongly agree that their profession should be required to have some knowledge of pharmacogenomics and once in practice, they should be able to identify medications that require pharmacogenomics testing.
This study has brought to light how educational inconsistencies in pharmacogenomics may be affecting the practitioners of the future. Pharmacogenomics will continue to evolve over time and become increasingly important in patient care [4]. Healthcare students recognize the clinical benefits of pharmacogenomics; however, the skills they are learning and the skills they believe they should have for this practice are not matching up. The results of this study indicate that education emphasizing medical applications of pharmacogenomics can significantly increase student comfort level in pharmacogenomics practice.
There are limitations to this study that should be considered. Individuals with strong opinions may have been more inclined to complete the survey than individuals without knowledge of, or opinions on pharmacogenomics. Pharmacy students had a much higher response rate (45.4%) than other students. This may have been attributable to the primary investigator sharing her status as a pharmacy student; potentially eliciting empathy from pharmacy student invitees. Pharmacy students may have more exposure to pharmacogenomics and stronger opinions. All of these factors could have potentially produced bias; however, the financial incentive offered to survey participants was designed to limit bias.
The medical student survey did not contain an option for students to select ‘Medical Student Year 4’ upon original release and had to be updated within a few days of survey release. This may have resulted in fourth year medical students selecting other years and skewing demographics. The Likert method used in this survey may have allowed participants without strong opinions or participants who had not heard of pharmacogenomics to select neutral. Survey fatigue may have contributed to nonresponses, although the survey was designed to take less than 5 min to complete in order to limit nonresponse due to fatigue. In addition, the sample size is limited to the UMN and may not be representative of all healthcare students in the USA. We expect that expansion of the study to include a variety of healthcare schools across the nation would further strengthen study results. We also like to compare results of similar results from other universities in future studies.
Conclusion & future perspective
To our knowledge, no one has explored students’ own expectations for pharmacogenomics’ relevance and education, and how that compares with the education they have received. This survey has demonstrated that healthcare students, like practicing professionals, regard pharmacogenomics as a clinically important area of practice. However, few students feel they have developed the skills necessary to employ basic concepts of pharmacogenomics. The students that did express a higher comfort level in application of pharmacogenomics likely developed those skills from coursework specifically addressing this subject. Knowledge of healthcare students clinical comfort level can help institutions better develop coursework vital to current and future clinical practice, specifically in the area of pharmacogenomics.
The survey did not explore healthcare students’ interest in learning about pharmacogenomics or tools students favor for learning. These may be important areas for future study in order to determine the most effective way to educate students.
Supplementary Material
Executive summary.
Background
Pharmacogenomics is a relevant and expanding field of clinical practice and the National Coalition for Health Professional Education in Genetics has established core competencies expected of all healthcare professionals.
Previous survey evidence suggests practitioners may feel inadequate in this field and these inadequacies may stem from their professional education.
Materials & methods
A 24-question, anonymous, online survey was distributed to pharmacy, nursing and medical students enrolled at the the University of Minnesota (MN, USA).
Survey questions designed to identify what skills students believed to be necessary to practice pharmacogenomics as well as what skills they believed they possessed.
Results
A total of 715 students across three fields completed the survey; the majority of participants across the three fields expressed that pharmacogenomics should be an important part of their curriculum and generally agreed that pharmacogenomics could improve patient care. Participants also generally expressed that once in clinical practice they should have the skills necessary to employ pharmacogenomics.
Only 11.1% of student respondents felt that pharmacogenomics had been an important part of their curriculum and less than half of the student respondents were comfortable answering questions on pharmacogenomics.
Students who had taken a genetics course specifically addressing applications of genetics in pharmacy were more likely to know which medications required genetic testing, feel comfortable answering questions on pharmacogenomics and feel comfortable interpreting a pharmacogenetic test.
Conclusion & future perspective
Although healthcare students consider pharmacogenomics to be important to patient care they lack self-confidence in the ability to practice it. Students that were more confident in their pharmacogenomics skills likely achieved those skills through coursework addressing genetics in pharmacy.
Further exploration could identify tools for teaching pharmacogenomics or models for coursework that would develop the National Coalition for Health Professional Education in Genetics core competencies.
Acknowledgments
The authors would like to thank K Janke for contributions to Qualtrics access.
Footnotes
Financial & competing interests disclosure
J Lamba is funded through R01CA132946 and R21CA155524 from the NIH. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- 1▪▪.McCullough KB, Formea CM, Berg KD, et al. Assessment of the pharmacogenomics educational needs of pharmacists. Am J Pharm Educ. 2011;75(3):51. doi: 10.5688/ajpe75351. Illustrated key weaknesses in pharmacogenomics education in practicing pharmacists and helped the present study’s authors shape survey questions to identify areas of weakness in current healthcare professional students. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crews KR, Cross SJ, McCormick JN, et al. Development and implementation of a pharmacist-managed clinical pharmacogenetics service. Am J Health Syst Pharm. 2011;68:143–150. doi: 10.2146/ajhp100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zembles T. An inservice program on pharmacogenetics to individualize drug therapy. Am J Pharm Educ. 2010;74(1):10. doi: 10.5688/aj740110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Streetman, Daniel S. Emergence and evolution of pharmacogenetics and pharmacogenomics in clinical pharmacy over the past 40 years. Ann Pharmacother. 2007;41:2038–2041. doi: 10.1345/aph.1K273. [DOI] [PubMed] [Google Scholar]
- 5.Roden DM, Tyndale RF. Pharmacogenomics at the tipping point: challenges and opportunities. Clin Pharmacol Ther. 2011;89(3):323–327. doi: 10.1038/clpt.2010.340. [DOI] [PubMed] [Google Scholar]
- 6.Knoell DL, Johnston JS, Bao S, Kelley KA. A genotyping exercise for pharmacogenetics in pharmacy practice. Am J Pharm Educ. 2009;73(3):43. doi: 10.5688/aj730343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howington L, Riddlesperger K, Cheek DJ. Essential nursing competencies for genetics and genomics: implications for critical care. Crit Care Nurse. 2001;31:e1–e7. doi: 10.4037/ccn2011867. [DOI] [PubMed] [Google Scholar]
- 8.Gurwitz D, Lunshof JE, Dedoussis G, et al. Pharmacogenomics education: International Society of Pharmacogenomics recommendations for medical, pharmaceutical, and health schools deans of education. Pharmacogenomics J. 2005;5:221–225. doi: 10.1038/sj.tpj.6500312. [DOI] [PubMed] [Google Scholar]
- 9.Moridani MY. The significance of pharmacogenomics in pharmacy education and practice. Am J Pharm Educ. 2005;69(2):37. [Google Scholar]
- 10▪.Murphy JE, Green JS, Adams LA, Squire RB, Kuo GM, McKay A. Pharmacogenomics in the curricula of colleges and schools of pharmacy in the United States. Am J Pharm Educ. 2010;74(1):7. doi: 10.5688/aj740107. Illustrated graduate schools’ self-identified quality in pharmacogenomics curriculum. [DOI] [PMC free article] [PubMed] [Google Scholar]
Websites
- 101.What is pharmacogenomics? US National Library of Medicine; [Accessed 17 October 2011]. http://ghr.nlm.nih.gov/handbook/genomicresearch/pharmacogenomics. [Google Scholar]
- 102.Table of Pharmacogenomic Biomarkers in Drug Labels. US FDA; [Accessed 10 October 2011]. www.fda.gov/drugs/scienceresearch/researchareas/pharmacogenetics/ucm083378.htm. [Google Scholar]
- 103.Pharmacogenomics: When Medicine Gets Personal. Mayo Clinic 1998–2011. [Accessed 5 September 2012];Consumer Health. www.mayoclinic.com/health/personalized-medicine/CA00078.
- 104.A Science Primer. National Center for Biotechnology Information; [Accessed 5 September 2012]. Just the Facts: A Basic Introduction to the Science Underlying NCBI Resources. www.ncbi.nlm.nih.gov/About/primer/pharm.html. [Google Scholar]
- 105▪▪.Core Competencies for All Health Care Professionals. [Accessed 5 September 2012];National Coalition for Health Professional Education in Genetics. http://www.nchpeg.org/index.php?option=com_content&view=article&id=237&Itemid=84. Explains the basic pharmacogenomics skills expected of all healthcare professionals and was vital in developing questions to identify healthcare students’ pharmacogenomics skills.
- 106.Sha M. [Accessed 5 September 2012];Council of young physicians meeting: strategic planning. www.acponline.org/about_acp/committees/young_physicians/agendas/9-12-05ag.pdf.
- 107.Education Grad Schools: Pharmacy. US News and World Report LP; [Accessed 6 September 2012]. http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-health-schools/pharmacy-rankings. [Google Scholar]
- 108.Education Colleges: University of Minnesota – Twin Cities. US News and World Report LP; [Accessed 6 September 2012]. http://colleges.usnews.rankingsandreviews.com/best-colleges/university-of-minnesota-twin-cities-174066/overall-rankings. [Google Scholar]
- 109.Curriculum: PharmD Professional Program. Regents of the University of Minnesota; [Accessed 10 November 2011]. www.pharmacy.umn.edu/pharmd/curriculum/home.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.