Abstract
Background
Racial/ethnic disparities in birth weight persist within the United States.
Purpose
Examine the association between maternal everyday discrimination and infant birth weight among young, urban women of color; as well as mediators (depressive symptoms, pregnancy distress, pregnancy symptoms) and moderators (age, race/ethnicity, attributions of discrimination) of this association.
Methods
420 women participated (14–21 years old; 62% Latina, 38% Black), completing measures of everyday discrimination and moderators during their second trimester of pregnancy and mediators during their third trimester. Birth weight was primarily recorded from medical record review.
Results
Path analysis demonstrated that everyday discrimination was associated with lower birth weight. Depressive symptoms mediated this relationship, and no tested factors moderated this relationship.
Conclusions
Given the association between birth weight and health across the lifespan, it is critical to reduce discrimination directed at young, urban women of color so that all children can begin life with greater promise for health.
Keywords: everyday discrimination, birth weight, depressive symptoms, pregnancy distress, adolescents, pregnancy
Racial/ethnic disparities in birth weight within the United States are pronounced. In 2009, the rate of low birth weight infants (i.e., less than 2500 grams or 5 pounds, 8 ounces) was 5.23% for White women, 5.72% for Latina women, and 11.44% for Black women (1). Although rates of low birth weight are generally similar between White and Latina women (e.g., Mexican), certain Latina women (e.g., Puerto Rican) are more likely to give birth to low birth weight infants (2). Birth weight, in turn, is associated with health across the lifespan. Low birth weight is among the three leading causes of infant death (3), and is further associated with intubation at birth, sepsis, and seizures during the first day of life (4). Low birth weight infants are more likely to suffer chronic lung disease (5), and be hospitalized during the first year of life (6). By childhood, low birth weight is associated with greater illness and neurodevelopmental problems (7). Among adults, low birth weight is associated with diminished lung functioning and death from chronic obstructive airways disease (8), increased risk of cardiovascular disease (9), and increased risk of diabetes (10). Therefore, disparities in birth weight give way to a wide range of health disparities among infants, children, and adults.
Given the relationship between infant birth weight and health across the lifespan, it is critical to understand why racial/ethnic disparities in birth weight persist. Recent reviews theorize that experiences of perceived discrimination contribute to the formation and maintenance of racial/ethnic disparities in birth outcomes (11–14). Further, empirical evidence demonstrates an association between discrimination during pregnancy and across the lifespan with adverse birth outcomes even after controlling for medical, socio-demographic, and behavioral risk factors (15–19). However, most of this research has focused on racism or race-based discrimination among adult Black American women specifically. We build on this past work by examining the process whereby perceived discrimination impacts birth weight among a sample of urban Latina and Black pregnant teens and young women aged 14–21 years. To better understand the mechanisms through which discrimination is associated with birth weight, we consider depressive symptoms, pregnancy distress, and pregnancy symptoms as potential mediators. These psychosocial and physiological mechanisms have been highlighted as contributors to birth outcomes in recent theoretical work (11). We further test whether age, race/ethnicity, and attributions of discrimination moderate this process. Before describing the current study, we consider sources of discrimination experienced by young, urban women of color and review literature identifying potential pathways linking discrimination to birth weight.
Multiple Sources of Maternal Discrimination
Young, urban women of color possess several stigmas – personal attributes, marks, or characteristics that are socially devalued and discredited (20). They may perceive discrimination associated with any of these stigmas. Racism persists in the United States (21), and therefore young, urban women of color may experience discrimination associated with their race or ethnicity. For example, childbearing African American women describe social distancing from Whites, overhearing racist comments in the workplace, and being treated with disrespect and distrust in stores (22). Sexism also persists in the United States (23,24), and therefore pregnant teens and young women may also experience discrimination associated with their gender. Young women report experiencing traditional gender role stereotyping, demeaning comments, and sexual objectification in their everyday lives (25).
Young, urban women of color may also experience discrimination associated with other characteristics. For example, they may experience discrimination associated with their age (26). Adults have greater power than young people, and young people report being treated with less respect and being taken less seriously than adults (27). Pregnant teens and young women may also experience discrimination associated with pregnancy. Although pregnant women are sometimes viewed positively (28), they are also negatively stereotyped and treated in certain domains (29). Pregnancy may be particularly stigmatizing for very young women, as social norms of the dominant culture discourage pregnancy among unwed teens. Very young pregnant women report experiences of social ostracism, exclusion, marginalization and being treated as an outcast (30) as well as experiences of verbal abuse from other teenagers and criticism from family members (31). Differences may exist by race/ethnicity: In one study, 45% of White adolescents, 41% of Black adolescents, and 33% of Latina adolescents reported feeling stigmatized by their pregnancy (31). Pregnant teens and young women may also possess other stigmas, such as low socio-economic status. Taken together, it is important to study experiences based on race and ethnicity as well as other possible stigmas to best understand the role of discrimination in adverse birth outcomes among young, urban women of color.
Experiences of discrimination are perceived across a continuum. At one end of this continuum are major acute experiences of discrimination (32). These include significant life events, such as being fired or denied housing. At the other end of this continuum are more minor chronic experiences of discrimination that often occur with greater frequency than major acute experiences. These include day-to-day irritations, such as being treated rudely or receiving poor service. Research and theory suggest that chronic experiences of more minor instances of discrimination have a significant impact on health outcomes, possibly greater than acute experiences of discrimination (32). Sustained exposure to discrimination may increase allostatic load, activation of stress processes that result in adverse health outcomes (33). Therefore, it may be important to focus on how experiences of everyday discrimination – chronic yet subtle mistreatment that may appear ‘trivial’ or ‘normal’ (34) – relate to birth weight among pregnant teens and young women.
Potential Pathways Linking Discrimination to Birth Weight
Although most prior work has not specifically tested mediators of the relationship between discrimination and birth outcomes, recent theory suggests that there are several pathways through which experiences of discrimination may result in greater risk of adverse birth outcomes (11). We focus on depressive symptoms, pregnancy distress, and pregnancy symptoms. Increasing evidence demonstrates that experiences of discrimination associated with a variety of stigmas are linked to depression and depressive symptoms. For example, experiences of racial discrimination are associated with higher risk of major depression (35), and experiences of gender discrimination are associated with greater depressive symptoms (25) in non-pregnant samples. Depressive symptoms, in turn, are associated with greater risk of low birth weight among pregnant women (for reviews, see 11,36). Depressive symptoms may impact birth weight via physiological processes that lead to dysfunctional placentation and intrauterine growth restriction (37). Dunkel Schetter (11) notes that although this process has not yet been studied, “depression may be an important mechanism whereby the effects of exposure to chronic stress and racism influence fetal growth and birth weight” (p. 536).
Another pathway whereby discrimination impacts birth weight may be distress, a negative emotional response to a stressor. Everyday discrimination has been conceptualized as a chronic psychological stressor that elicits distress (18; 34). Pregnant women of color may experience pregnancy distress specifically, or concern and worry about pregnancy- and motherhood-specific issues (38), as a response to discrimination. Rosenthal and Lobel (14) argue that Black American women experience pregnancy distress as a consequence of being the target of contradictory social pressures regarding motherhood and race. As American women they are encouraged to be mothers, but as Black American women they are discouraged from being mothers. In the past, this discouragement has even taken on the form of forced sterilization. Those who have children are often stereotyped as “welfare queens,” or incompetent mothers who are drains on society. Experiences of discrimination may trigger stereotype threat: Worry about confirming stereotypes or being treated according to stereotypes (14). Stereotype threat results in psychological and physiological stress responses among a variety of samples (39), and as hypothesized in the present work, may result in distress associated with pregnancy and motherhood among young, urban women of color. Rosenthal and Lobel theorize that Latina women may experience similar pressures with similar resulting consequences. Further, young women of color who are additionally stereotyped as immature or irresponsible due to their youth may be at heightened risk of experiencing pregnancy distress. Pregnancy distress, in turn, is a critical predictor of adverse birth outcomes (11,40). Pregnancy distress sets in motion a chain of physiological processes (e.g., involving maternal cortisol levels, placental corticotropin-releasing hormone) that impact birth weight (11).
Physical health may also be a pathway through which discrimination impacts birth weight. Recent meta-analytic evidence suggests that discrimination is directly associated with poor physical health outcomes among people living with a variety of stigmas (33). Among pregnant women specifically, stressors such as everyday discrimination are associated with low birth weight through their impact on the vascular system (e.g., vasoconstriction, reduced uteroplacental perfusion, hypoxia), hypothalamic-pituitary-adrenal axis (e.g., increased maternal cortisol), and immune-inflammatory pathway (36). Such stressors are further related to physical symptoms during pregnancy (e.g., low belly or pelvic pain, nausea or vomiting) (41), which may be indicative of underlying pregnancy complications. Although not always the case, greater pregnancy symptoms such as vomiting and nausea in turn can be associated with lower infant birth weight for example, via reduced caloric retention or intake (42).
Current Study Hypotheses
We hypothesized that everyday discrimination experienced by young, urban women of color would be associated with lower infant birth weight after controlling for important factors including gestational age. We also hypothesized that increased depressive symptoms, pregnancy distress, and pregnancy symptoms mediate the relationship between discrimination and birth weight. Further, we tested whether this process is moderated by age, race/ethnicity, and/or attributions of discrimination. Accumulating evidence suggests that experiences of everyday discrimination are related to poor health among people regardless of race/ethnicity (43–45), and that experiences of discrimination broadly – not just those associated with race – are associated with poor health (33,46). We therefore hypothesized that the relationship between everyday discrimination and birth weight would be similar for younger versus older women, Black versus Latina women, and women attributing their experiences to race/ethnicity versus other stigmas.
Methods
Procedure
Data for this study were drawn from a new randomized controlled trial (RCT) of a group prenatal care model aimed at promoting improved general health and reproductive health behaviors (47,48). Study sites were community hospitals and health centers located in New York City (i.e., Manhattan, Queens, Brooklyn, the Bronx). Clinical sites were randomized to deliver the group prenatal care intervention or standard prenatal care. For this study, we utilize data from the seven control sites delivering standard of care to avoid any potential confounding from participation in the intervention.
Between 2008 and 2011, young women aged 14–21 attending an initial prenatal care visit at a participating study site were referred by a health care provider or approached directly by research staff. Inclusion criteria included pregnancy less than 24 weeks gestation, no medical problems requiring individual care as a high-risk pregnancy (e.g., HIV positive), ability to speak English or Spanish, and willingness to participate in study procedures. After obtaining informed consent, baseline interviews were conducted during the second trimester between 14 and 24 weeks gestation (M =19.35, SD = 3.20). Second interviews were completed during the third trimester between 32 and 42 weeks gestation (M = 34.74, SD = 2.70). Additional interviews were completed 6 and 12 months postpartum.
Structured interviews were completed using Audio-Handheld Assisted Personal Interview (A-HAPI) technology. A-HAPI allows respondents to listen over headphones to spoken questions that have been digitally recorded and stored on a computer, as well as displayed on the computer’s screen. Participants who reported being most comfortable speaking Spanish (18.3% of the analytic sample) completed interviews in Spanish, and others completed interviews in English. Interviews were translated from English into Spanish, then back-translated by an independent translator and compared to the original to ensure accuracy. Spanish measures were reviewed by native Spanish-speakers from various regions to ensure that language would be appropriate for use with women from a variety of countries. Participants were paid $20 for each interview. All procedures were approved by Institutional Review Boards at Yale University, the Clinical Directors Network, and each study site.
Participants
Of 1,549 young women eligible for the larger study, 1,236 enrolled (80%). Those who agreed to participate were slightly younger (participants: M = 18.63, SD = 1.73; non-participants: M = 19.00, SD = 1.67; t(1,548) = −3.46, p = .001); and were more likely to be Black (participants: 38%; non-participants: 27%; χ2 (1) = 23.36, p < .001) and less likely to be White (participants: 3%; non-participants: 6%; χ2 (1) = 4.38, p = .03). Of those enrolled, 624 women were assigned to the control condition. Participants in the control versus intervention conditions did not differ in terms of age or race/ethnicity. Analyses for this paper included 420 women who identified as Black or Latina (24 women excluded), completed a second interview (150 women excluded because they could not be reached), had a singleton birth (6 women with twins excluded), and had birth weight data available (24 women excluded). Women who missed the second interview did not differ on any baseline constructs (i.e., age, race/ethnicity, born outside the US, grade level, relationship status, nutrition, exercise, pregnancy history, everyday discrimination) or on birth outcomes (i.e., birth weight, gestational age).
Measures
Everyday discrimination
Experiences of everyday discrimination were measured using a modified, 10-item version (46,49) of the Everyday Discrimination scale (50) at baseline. Participants indicated how often they experience 10 forms of discriminatory treatment from others (e.g., “treated with less respect than other people”) in their day-to-day lives on a scale from never (1) to often (4). A mean score was created based on responses (English α = .84, Spanish α = .85). Participants were then asked “What do you think the main reason is for these experiences?” They could attribute their experiences to race/ethnicity, gender, age, income level, language, physical appearance, sexual orientation, other, or refuse to answer. Participants could only choose one attribution for discrimination.
Depressive symptoms
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale [CES-D (51)] at the second interview. As done with prior studies of pregnant women (47), somatic items were dropped because pregnancy may cause physical symptoms similar to those caused by depression (e.g., changes in appetite or sleep). The remaining 15 items asked participants how often they experienced affective components of depressed mood (e.g., “feel depressed”, “feel lonely”) in the past week, and were rated on the following scale: less than 1 day (0), 1–2 days (1), 3–4 days (2), 5–7 days (3). Responses were summed to create a composite score (English α = .87, Spanish α = .79).
Pregnancy distress
Pregnancy distress was measured using the Revised Prenatal Distress Questionnaire [PDQ (38,40)] at the second interview. Participants were asked “how much are you bothered, worried, or upset” about 17 issues associated specifically with pregnancy on a scale from not at all (0) to very much (2). Items included issues about medical care, physical symptoms, parenting, bodily changes, and the infant’s health (e.g., “whether you might have an unhealthy baby”, “pain during labor and delivery”). Responses were summed to create a composite score (English α = .86, Spanish α = .82).
Pregnancy symptoms
Pregnancy symptoms were measured using the Pregnancy Symptom Distress Scale at the second interview. This scale was modeled after a previously developed symptom distress scale (52), and has been used in our prior work (53). Participants indicated how often they were bothered by 14 pregnancy symptoms in the past month on a scale from never (0) to always (4). Symptoms included: “low belly (pelvic) pain, nausea or vomiting, heart burn, frequent peeing, vaginal discharge, headaches, leg cramps, varicose veins, sore breasts, fatigue or feeling tired, low back pain, swelling of hands or feet, cramping, and bleeding gums.” Responses were summed to create a composite score.
Outcome variable: Birth weight
Trained study staff abstracted birth weight data from labor and delivery logs at hospitals and health centers. Labor and delivery logs were available for 391 participants (93.1%). These data were supplemented with self-report data from interviews at 6 (n = 22, 5.2%) and 12 (n = 3, 0.7%) months postpartum, as well as postpartum phone calls made to participants (n = 4, 1.0%). Self-report birth weight was highly correlated with birth weight recorded from labor and delivery logs (n = 276; r = 0.94, p < .001).
Participant characteristics
Participants reported age, race/ethnicity, whether they were born outside the U.S., whether they were enrolled in school, the highest grade that they had completed, their relationship status, and their pregnancy history at baseline. Participants also reported on health behaviors. Nutrition was measured with the Rapid Eating Assessment for Patients [REAP (54]. Exercise was measured with the Weight, Activity, Variety, Excess Assessment [WAVE (54)]. Gestational age, a particularly strong predictor of birth weight (18,36), was abstracted from labor and delivery logs at hospitals and health centers, using the same methodology as birth weight data (described above); gestational age was estimated using ultrasound results when available or last menstrual period. All of these variables were included as control variables.
Analysis Strategy
We first explored demographic and related characteristics of the sample. Second, we conducted a preliminary logistic analysis to examine the relationship between everyday discrimination and low birth weight, measured dichotomously. Third, we used path analysis to examine mediators of the relationship between everyday discrimination and birth weight, measured continuously. Finally, we used multigroup analyses to examine moderators of this relationship. Together, these analyses examine the impact of everyday discrimination and birth weight both dichotomously and continuously. This strategy has been recommended by Dunkel Schetter and Lobel, who note that the effects of psychosocial factors on birth weight are often linear (36). Analyses were conducted using SPSS 17.0 and AMOS 17.0.
Results
Participant Characteristics
Table 1 includes participant characteristics. Sixty-two percent of participants identified as Latina and 38% identified as Black. Notably, nearly one-third (28%) of participants had been born outside of the United States. Of participants born outside of the U.S., the majority were born in the Dominican Republic (42%), Mexico (18%), or Jamaica (11%). Several others were born in other Central or Southern American countries, other Caribbean countries, or Southern or Western Africa. On average, participants reported experiencing everyday discrimination between “never” and “rarely.” Of participants who made an attribution for their discrimination, 18% attributed their experiences to their race/ethnicity and 14% attributed their experiences to their age. Interestingly, 26% of participants attributed discrimination to “other,” or a reason not provided by the scale, and 25% refused to make an attribution for discrimination. On average, participants reported experiencing depressive symptoms between 0 and 1–2 days per week, pregnancy distress “not at all” to “somewhat, ” and pregnancy symptoms “rarely” to “sometimes.” Birth weight ranged from 1275 grams (2 lb, 12.97 oz) to 4580 grams (10 lb, 1.55 oz), with an average birth weight of 3152.51 grams (6 lb, 15.20 oz; SD = 519.79). This is within the range of normal birth weight.
Table 1.
Participant Characteristics (n = 420)
| n | % | M | SD | |
|---|---|---|---|---|
| Baseline/Trimester 2 | ||||
| Age (range = 14–21) | 18.56 | 1.68 | ||
| Race/Ethnicitya | ||||
| Latina | 262 | 62.4 | ||
| Black | 158 | 37.6 | ||
| Born Outside U.S. | 119 | 28.3 | ||
| Enrolled in School | 207 | 49.3 | ||
| Grade Completed | 10.92 | 2.06 | ||
| Relationship Status | ||||
| Single, Never Married | 243 | 57.9 | ||
| Not Married, Living with Partner | 114 | 27.1 | ||
| Married | 41 | 9.8 | ||
| Other | 11 | 3.0 | ||
| Pregnancy History: Nulliparous | 352 | 83.8 | ||
| Nutrition | 13.92 | 5.38 | ||
| Exercise | 5.77 | 2.79 | ||
| Everyday Discrimination | 1.45 | 0.46 | ||
| Reason for Discrimination | ||||
| Race/Ethnicity | 74 | 17.6 | ||
| Age | 58 | 13.8 | ||
| Physical Appearance | 24 | 5.7 | ||
| Language | 19 | 4.5 | ||
| Income Level | 14 | 3.3 | ||
| Gender | 11 | 2.6 | ||
| Sexual Orientation | 7 | 1.7 | ||
| Other | 108 | 25.7 | ||
| Refuse to Answer | 105 | 25.0 | ||
| Time 2/Trimester 3 | ||||
| Depressive Symptoms | 10.78 | 8.10 | ||
| Pregnancy Distress | 12.35 | 6.63 | ||
| Pregnancy Symptoms | 20.75 | 9.07 | ||
| Birth Outcomes | ||||
| Birth Weight (grams) | 3152.51 | 519.79 | ||
| Low Birth Weight (BW <2500 grams) | 38 | 9.0 | ||
| Gestational Age (days) | 274.08 | 12.50 | ||
| Preterm Birth (GA < 259 days) | 38 | 9.0 | ||
Note: Percentages may not add to 100 due to rounding. Nutrition was measured on a 31 point scale, exercise was measured on a 15 point scale.
24 women who did not identify as Latina or Black were excluded from analyses.
Preliminary Analysis: Discrimination and Low Birth Weight
We examined the association between everyday discrimination and low birth weight using logistic regression controlling for maternal age, born outside the US, grade level, relationship status, nutrition, exercise, pregnancy history, and gestational age. The resulting model was statistically significant, χ2 (9) = 118.13, p < .001, and everyday discrimination was associated with greater odds of low birth weight, OR = 2.78, p = .05. Among the control variables, only gestational age was associated with low birth weight, OR = .85, p < .001.
Path Analysis: Test of Mediators
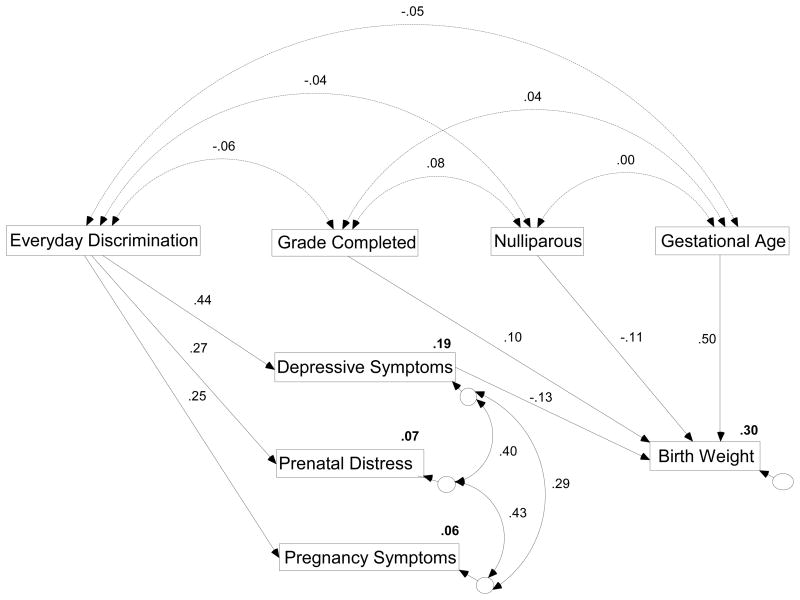
We next evaluated the hypothesized path model, which included paths between everyday discrimination and the three mediators, a path between everyday discrimination and continuous birth weight, and paths between the three mediators and birth weight. Correlations between these primary variables are included in Table 2. The path analysis further included maternal age, born outside the US, grade level, relationship status, nutrition, exercise, pregnancy history, and gestational age as exogenous variables predicting birth weight, thereby controlling for their effects. Four data points were missing (missing data = < .01% of total data), and were imputed using regression imputation with AMOS 17.0. Because depression, pregnancy distress, and pregnancy symptoms were correlated, we correlated their errors in the path analysis. We first examined the saturated model, and then trimmed non-statistically significant paths (55). Several of the control variables had no association with birth weight and were therefore trimmed from the model. The direct paths from everyday discrimination (β = −.02, p = .62), pregnancy distress (β = −.04, p = .36), and pregnancy symptoms (β = .04, p = .35) to birth weight were also non-statistically significant and were trimmed from the model. Figure 1 includes the final path model, which accounted for 30% of the variance in birth weight. Because several variables included in the model were skewed (e.g., gestational age skew = −1.83, SE = .12), a Bollen-Steine bootstrap was performed to acquire an adjusted p-value (56). Model fit indices indicated that the model was a good fit for the data, χ2 (12) = 21.34, p = .49; Standardized Root Mean Square Residual (SRMR) = 0.03; Comparative Fit Index (CFI) = 0.98; Root Mean Square Error of Approximation (RMSEA) = 0.04 (CI = 0.01 = 0.07).
Table 2.
Correlations between main variables included in path analysis
| Everyday Discrimination | Depressive Symptoms | Pregnancy Distress | Pregnancy Symptoms | Birth Weight | |
|---|---|---|---|---|---|
| Everyday Discrimination | 1.00 | ||||
| Depressive Symptoms | .44** | 1.00 | |||
| Pregnancy Distress | .27** | .46** | 1.00 | ||
| Pregnancy Symptoms | .25** | .37** | .47** | 1.00 | |
| Birth Weight | −.11* | −.15** | −.07 | −.01 | 1.00 |
Note:
p < .05,
p < .01
Figure 1.
Final path model of relationship between everyday discrimination and birth weight. Figure includes standardized regression weights for all non-trimmed paths, correlations, and squared multiple correlations in bold. All solid lines are statistically significant at p < .01, all dashed lines are non-statistically significant at p > .10.
The final path model demonstrates that everyday discrimination is associated with increased depressive symptoms, pregnancy distress, and pregnancy symptoms. Depressive symptoms, in turn, are associated with decreased birth weight. These associations occur controlling for grade completion, nulliparous status, and gestational age. The path analysis was performed with bootstrapping to examine the direct and indirect effects of everyday discrimination on birth weight (56). Everyday discrimination had a statistically significant indirect effect on birth weight through depressive symptoms of −0.04, p = .01. The unstandardized coefficient was −49.27 indicating that for every one point increase in everyday discrimination, birth weight decreased by approximately 49 grams.
We also compared a model representing the alternative hypothesis that there is no mediation between everyday discrimination and birth weight by treating all predictor variables as exogenous. The Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) associated with this alternative model were both higher than the final model (final model: AIC = 69.34, BIC = 166.31; alternative model: AIC = 72.00, BIC = 217.45), indicating that the final model is a better fit for the data than the alternative model.
Multigroup Analyses: Test of Moderators
We were interested in whether age of participants (based on median split: 18 years and younger versus 19 years and older), race of participants (Black vs. Latina), or participants’ attributions of discrimination (to race/ethnicity versus another stigma) moderated the effects represented in the model. We tested for structural weight variance (i.e., differences in the strength of regression weights represented in the model) as well as structural mean variance (i.e., differences in the mean scores on variables represented in the model) within three multigroup analyses. We considered a CFI less than 0.95 and/or a RMSEA greater than 0.05 as an indication of variance between models to be further examined (55).
Results indicated structural weight invariance for age [CFI = 0.98; RMSEA = 0.03 (CI = 0.00 –0.05)], race [CFI = 0.99; RMSEA = 0.02 (CI = 0.00 – 0.05)], and attributions of discrimination [CFI = 0.97; RMSEA = 0.04 (CI = 0.00 – 0 .06)], meaning that differences between the regression weights in the model were not detected between groups. Therefore, the process whereby discrimination impacts birth weight was similar for women 18 years and under versus 19 years and older, Black versus Latina women, and women who attributed their experiences of discrimination to race versus to other stigmas. Additional multigroup analyses testing the saturated model further demonstrated structural weight invariance, suggesting that the paths from pregnancy distress and pregnancy symptoms to birth weight did not differ based on these groups either.
In contrast, results indicated structural mean variance for age [CFI = 0.84; RMSEA = 0.08 (CI = 0.06 – 0.09)] and race [CFI = 0.92; RMSEA = 0.05 (CI = 0.04 – 0.07)], but not attributions [CFI = 0.97; RMSEA = 0.03 (0.00 – 0.05)]. We followed up on this finding with a series of t-tests testing for mean differences in the main variables represented in the path model between women 18 years and younger versus 19 years and older, and Black versus Latina women. Results are included in Table 3. Women aged 18 years and younger reported lower pregnancy distress than women aged 19 years and older. There were no other mean differences by age. Black women reported higher pregnancy distress and pregnancy symptoms than Latina women, however they did not differ in everyday discrimination or depressive symptoms. Black women also gave birth to lower birth weight infants. An additional analysis replicated this disparity for low birth weight: A higher percentage of Black women had infants classified as low birth weight (13.9%) than Latina women [6.1%; χ2 (1) = 7.32, p = .01].
Table 3.
Results of Multigroup Analyses: Structural Mean Comparison
| Age | Race | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| 18 and younger | 19 and older | t-test | Black | Latina | t-test | |
| Everyday Discrimination | 1.44 (.47) | 1.47 (.45) | −0.72 | 1.50 (.44) | 1.43 (.47) | 1.42 |
| Depressive Symptoms | 10.85 (7.81) | 10.72 (8.36) | 0.16 | 11.42 (8.52) | 10.40 (7.83) | 1.25 |
| Pregnancy Distress | 11.57 (6.32) | 13.01 (6.83) | −2.22* | 13.52 (6.49) | 11.64 (6.63) | 2.84* |
| Pregnancy Symptoms | 20.37 (9.02) | 21.09 (9.13) | −0.81 | 21.79 (8.34) | 20.13 (9.45) | 1.82† |
| Birth Weight | 3179.18 (502.95) | 3121.45 (538.38) | −1.14 | 3046.37 (529.79) | 3216.52 (504.25) | −3.29** |
Note: M(SD) included.
p < .10,
p < .05,
p < .01
These analyses demonstrate that the process through which discrimination is associated with birth weight was similar regardless of age, race/ethnicity, and attribution of discrimination. However, there were some differences in the mean scores on variables represented in the model. Notably, Black women gave birth to lower birth weight infants.
Discussion
We explored the relationship between maternal experiences of everyday discrimination and infant birth weight among young, urban women of color to add to knowledge of the process whereby discrimination contributes to racial/ethnic disparities in birth outcomes. Study participants were recruited from community hospitals and health centers in New York City and received standard prenatal care. The resulting sample identified as Latina and Black, and reported low levels of everyday discrimination. Despite these low levels, everyday discrimination reported during the second trimester was associated with lower infant birth weight. Given that we controlled for gestational age, this suggests that everyday discrimination is associated with fetal growth process. Findings are consistent with past research in which low levels of everyday discrimination (i.e., averaging in never to rarely range) reported by African American adults are associated with poor health outcomes including higher amounts of visceral fat (45), poor ambulatory blood pressure responses (43), and poor sleep (57). Therefore, this finding contributes to a growing body of research suggesting that experiences with small, subtle instances of discrimination in everyday life have a significant impact on health outcomes (35).
Results further provide insight into the magnitude of the relationship between everyday discrimination and birth weight. The preliminary logistic regression demonstrated that for every one point increase in everyday discrimination, the likelihood of giving birth to a low birth weight baby increased by 178%. The path analysis demonstrated that for every one point increase in everyday discrimination, birth weight decreased by approximately 49 grams. This is a modest change in continuous birth weight: It is smaller than changes associated with major determinants of birth weight such as smoking (149 grams) and drinking alcohol (155 grams), but comparable to other determinants such as parity (43 grams) and caloric intake (35 grams; 58). Evidence suggests that such modest changes in birth weight, even within normal range, have a significant impact on health outcomes. For example, studies examining the full range of birth weight find associations with five-minute APGAR scores (indicating infant health) and mortality within the first year of life (59), decreased cognitive functioning and IQ in childhood and adulthood (60,61), and number of physician visits during adolescence (62).
In addition to establishing a relationship between everyday discrimination and low birth weight among pregnant teens and young women, we explored the process whereby this relationship occurs. We considered depressive symptoms, pregnancy distress, and pregnancy symptoms as mediators or potential pathways through which everyday discrimination is associated with birth weight. Results revealed that experiences of everyday discrimination were associated with increased depressive symptoms, pregnancy distress, and pregnancy symptoms measured at the second interview. Therefore, young, urban women of color who experienced greater everyday discrimination during their second trimester experienced decreased mental and physical health during their third trimester. However, only increases in depressive symptoms mediated the relationship between everyday discrimination and infant birth weight. That is, women who experienced greater everyday discrimination experienced more depressive symptoms and these depressive symptoms predicted lower infant birth weight.
Finally, we examined moderators of this relationship using multigroup analyses. We found that the process whereby everyday discrimination is associated with birth weight was similar for young women aged 14–18 and 19–21, Black and Latina women, and women who attributed their experiences of discrimination to their race/ethnicity versus other stigmas. This suggests that the association between discrimination and infant birth weight among pregnant teens and young women of color may be indiscriminate – taking its toll on women of different ages, races/ethnicities, and those who make different attributions for discrimination.
Strengths, Limitations, and Future Directions of Work
The current investigation has several strengths, allowing it to make contributions to understandings of the relationship between discrimination and birth weight as well as causes of persistent disparities in birth weight. First, we extended research on discrimination and birth outcomes to young, urban women of color. To date, most research has focused on adults. We documented that this association also exists among a vulnerable, underserved, and understudied population that experiences discrimination associated with multiple stigmas. Second, we tested the process whereby discrimination impacts birth weight among this population. In doing so, we found support for theoretical claims that depression mediates the relationship between experiences of discrimination and birth weight (11). Third, we examined several moderators of this process. Past work has focused on Black American women who attribute discrimination to race. We studied both Black and Latina women who attribute discrimination to different stigmas, and demonstrated that the process whereby discrimination is related to birth weight is similar for young women aged 14–18 and 19–21, Black and Latina women, and women who attribute discrimination to race and to other stigmas. This research further answers a call for work to examine the relationship between discrimination and health outcomes using prospective data (32). The longitudinal design paired with the statistical modeling technique of path analysis enables firmer conclusions regarding the association between everyday discrimination and birth weight.
Much theorizing has suggested that discrimination constitutes a stressor (32) and therefore stress may be an important mechanism through which discrimination affects birth outcomes (13,18). Additionally, research has suggested that pregnancy distress specifically may be the most important predictor of adverse birth outcomes (11). We found that discrimination was associated with increased pregnancy distress but that pregnancy distress was not associated with birth weight. It is possible that other forms of stress such as race and gender-specific stress (63,64) contribute to birth weight among this population. Future research might test whether such specific or contextualized forms of stress experienced during pregnancy contribute to birth weight, and possibly mediate the relationship between discrimination and birth weight. Future research might also test whether other stress-related processes, including health behavior and substance use, mediate this relationship. However, it may also be the case that the process whereby discrimination impacts birth outcomes is different for teens and younger women versus adults. We found that depressive symptoms were a mediator of the relationship between discrimination and birth weight. This is consistent with recent theorizing as well as past work linking depression with low birth weight (11). Future research should examine depression as a possible mediator of the relationship between discrimination and birth weight across different samples.
Other methodological limitations should be addressed within future research. For example, our measure of pregnancy symptoms was based on self-report and may not capture the full range of health complications associated with pregnancy. Future research should include more specific biological measurements and health complications to test physiological mechanisms that link experiences of discrimination during pregnancy with lower birth weight (11,36). Future research might also test whether everyday discrimination, depressive symptoms, pregnancy distress, and pregnancy symptoms measured at different points during pregnancy differentially contribute to birth weight. Relatedly, some research indicates that lifetime discrimination rather than discrimination experienced during pregnancy specifically is an important predictor of low birth weight (15,18). Future work should continue to compare discrimination experienced at different times in life, both before and during pregnancy, to identify when experiences of discrimination are most detrimental to birth outcomes.
Although we tested several potential moderators of the effects reported, we did not find evidence of moderation. There may not have been enough diversity within our sample to detect moderation. For example, the age range was narrow and the number of women who attributed discrimination to race/ethnicity was low in comparison to the number who attributed discrimination to other stigmas. Future research should include a larger more diverse sample of pregnant women, and examine other moderators such as nativity status particularly among Latina women. This comparative research may provide greater insight into the extent to which these processes contribute to disparities in birth weight, and contribute to understandings of variation in birth weight among Latina women.
Finally, future research should continue to explore the nature of discrimination experienced by young, urban women of color. More women in this study attributed discrimination to “other” than to any specified reason, including race/ethnicity or age. For what other reasons are young, urban women of color experiencing discrimination? Past work suggests that they may be experiencing discrimination associated with pregnancy specifically (30,31), but they may also be experiencing discrimination associated with other understudied stigmas. Future research should continue to explore other reasons for discrimination, as well as how attributions of discrimination are made by young, urban women of color. Additionally, it is possible that this population attributes discrimination to multiple stigmas. Because participants were only able to attribute discrimination to one stigma, we were unable to test whether experiencing discrimination associated with multiple stigmas moderated the association between discrimination and birth weight. Further, because relatively small numbers of participants attributed discrimination to stigmas other than race/ethnicity, we were unable to test whether attributions to other stigmas (e.g., age, physical appearance) moderated the association. Future research should measure discrimination associated with multiple stigmas to explore the impact of the intersectionality of stigmas (65), or how experiencing discrimination associated with multiple stigmas impacts birth weight.
Implications
This work has implications for practice and policy. Healthcare providers who work with pregnant teens and young women during the prenatal period have an opportunity to alleviate the impact of discrimination on birth weight, thus reducing disparities in birth outcomes and improving maternal mental and physical health. This work highlights depressive symptoms as a mediator of the relationship between discrimination and birth weight. Therefore, treating depressive symptoms experienced by young, urban women of color may mitigate the impact of discrimination on birth weight. Further, discrimination is a social determinant of health whose effect must ultimately be intervened upon at the sociocultural level though policy and other methods. Given the association between birth weight and health across the lifespan, it is critical to reduce discrimination directed at urban youth of color so that all children are able to begin life with greater promise for health. In doing so, we have an opportunity to eliminate disparities not only in birth weight, but in health outcomes across the lifespan.
Acknowledgments
The project described was supported by grants from the National Institute of Mental Health, including R01MH074399, a research grant that funded the study, and T32MH020031, a training grant that funded Dr. Earnshaw’s effort. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. The authors thank three anonymous reviewers and Dr. Laura Bogart for their helpful comments on earlier versions of this manuscript.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References
- 1.Martin JA, Hamilton BE, Ventura SJ, et al. Births: Final data for 2009. National Vital Statistics Report. 2011:60. [PubMed] [Google Scholar]
- 2.Fuentes-Afflick E, Hessol NA, Perez-Stable EJ. Testing the epidemiologic paradox of low birth weight in Latinos. Arch Pediatr Adolesc Med. 1999;153:147–153. doi: 10.1001/archpedi.153.2.147. [DOI] [PubMed] [Google Scholar]
- 3.Matthews TJ, Menacker F, MacDorman MF. Infant mortality statistics from the 2002 period linked birth/infant death data set. National Vital Statistics Report. 2005;53:1–30. [PubMed] [Google Scholar]
- 4.McIntire DD, Bloom SL, Casey BM, Leveno KJ. Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med. 1999;340:1234–1238. doi: 10.1056/NEJM199904223401603. [DOI] [PubMed] [Google Scholar]
- 5.Lemons JA, Bauer CR, Oh W, et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. Pediatrics. 2001;107:e1. doi: 10.1542/peds.107.1.e1. [DOI] [PubMed] [Google Scholar]
- 6.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 7.Hack M, Klein NK, Taylor HG. Long-term developmental outcomes of low birth weight infants. Future Child. 1995;5:176–196. [PubMed] [Google Scholar]
- 8.Barker DJ, Godfrey KM, Fall C, et al. Relation of birth weight and childhood respiratory infection to adult lung function and death from chronic obstructive airways disease. BMJ. 1991;303:671–675. doi: 10.1136/bmj.303.6804.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rich-Edwards JW, Stampfer MJ, Manson JE, et al. Birth weight and risk of cardiovascular disease in a cohort of women followed up since 1976. BMJ. 1997;315:396–400. doi: 10.1136/bmj.315.7105.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hattersley AT, Tooke JE. The fetal insulin hypothesis: an alternative explanation of the association of low birth weight with diabetes and vascular disease. Lancet. 1999;353:1789–1792. doi: 10.1016/S0140-6736(98)07546-1. [DOI] [PubMed] [Google Scholar]
- 11.Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 12.Giscombé CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: the impact of stress, racism, and related factors in pregnancy. Psychol Bull. 2005;131:662–683. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dominguez TP. Race, racism, and racial disparities in adverse birth outcomes. Clin Obstet Gynecol. 2008;51:360–370. doi: 10.1097/GRF.0b013e31816f28de. [DOI] [PubMed] [Google Scholar]
- 14.Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med. 2011;72:977–983. doi: 10.1016/j.socscimed.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 15.Collins JW, David RJ, Symons R, et al. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11:337–339. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Dole N, Savitz DA, Hertz-Picciotto I, et al. Maternal stress and preterm birth. Am J Epidemiol. 2003;157:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 17.Lespinasse AA, David RJ, Collins JW, Handler AS, Wall SN. Maternal support in the delivery room and birthweight among African-American women. J Natl Med Assoc. 2004;96:187–195. [PMC free article] [PubMed] [Google Scholar]
- 18.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychol. 2008;27:194–203. doi: 10.1037/0278-6133.27.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Corwin MJ. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13:646–652. doi: 10.1097/00001648-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Goffman E. Stigma : Notes on the Management of Spoiled Identity. 1. New York: Simon & Schuster; 1963. [Google Scholar]
- 21.Dovidio J, Gaertner S. Aversive racism. In: Zanna MP, editor. Advances in Experimental Social Psychology. 36. San Diego, CA: Elsevier; 2004. pp. 1–52. [Google Scholar]
- 22.Nuru-Jeter A, Dominguez TP, Hammond WP, et al. “It’s the skin you’re in”: African-American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J. 2008;13:29–39. doi: 10.1007/s10995-008-0357-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swim JK, Aikin KJ, Hall WS, Hunter BA. Sexism and racism: old-fashioned and modern prejudices. J Pers Soc Psychol. 1995;68:199–214. [Google Scholar]
- 24.Glick P, Fiske ST. The ambivalent sexism inventory: differentiating hostile and benevolent sexism. J Pers Soc Psychol. 1996;70:491–512. [Google Scholar]
- 25.Swim JK, Hyers LL, Cohen LL, Ferguson MJ. Everyday sexism: evidence for its incidence, nature, and psychological impact from three daily diary studies. J Soc Issues. 2001;57:31–53. [Google Scholar]
- 26.Kimmel DC. Ageism, psychology, and public policy. Am Psychol. 1988;43:175–178. doi: 10.1037//0003-066x.43.3.175. [DOI] [PubMed] [Google Scholar]
- 27.Gordon HR. Allies within and without: how adolescent activists conceptualize ageism and navigate adult power in youth social movements. J Contemp Ethnogr. 2007;36:631–668. [Google Scholar]
- 28.Marván ML, Islas M, Vela L, Chrisler JC, Warren EA. Stereotypes of women in different stages of their reproductive life: data from Mexico and the United States. Health Care Women Int. 2008;29:673–687. doi: 10.1080/07399330802188982. [DOI] [PubMed] [Google Scholar]
- 29.Halpert JA, Wilson ML, Hickman JL. Pregnancy as a source of bias in performance appraisals. J Organ Behav. 1993;14:649–663. [Google Scholar]
- 30.Whitehead E. Teenage pregnancy: on the road to social death. Int J Nurs Stud. 2001;38:437–446. doi: 10.1016/s0020-7489(00)00086-9. [DOI] [PubMed] [Google Scholar]
- 31.Wiemann CM, Rickert VI, Berenson AB, Volk RJ. Are pregnant adolescents stigmatized by pregnancy? J Adolesc Health. 2005;36:352–352. doi: 10.1016/j.jadohealth.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pascoe EA, Richman LS. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Essed P. Understanding Everyday Racism: An Interdisciplinary Theory. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- 35.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2008;98:S29–S37. doi: 10.2105/ajph.98.supplement_1.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dunkel Schetter C, Lobel M. Handbook of Health Psychology. 2. Pregnancy and birth outcomes: a multi-level analysis of prenatal maternal stress and birth weight. in press. [Google Scholar]
- 37.McElrath TF, Hecht O, Dammann K, et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol. 2008;168:980–989. doi: 10.1093/aje/kwn202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yali AM, Lobel M. Coping and distress in pregnancy: an investigation of medically high risk women. J Psychosom Obstet Gynecol. 1999;20:39–52. doi: 10.3109/01674829909075575. [DOI] [PubMed] [Google Scholar]
- 39.Schmader T, Johns M, Forbes C. An integrated process model of stereotype threat effects on performance. Psych Rev. 2008;115:336–356. doi: 10.1037/0033-295X.115.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lobel M, Cannella DL, Graham JE, et al. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008;27:604–615. doi: 10.1037/a0013242. [DOI] [PubMed] [Google Scholar]
- 41.Paarlberg KM, Vingerhoets A, Passchier J, et al. Psychosocial factors as predictors of maternal well-being and pregnancy-related complaints. J Psychosom Obstet Gynecol. 1996;17:93–102. doi: 10.3109/01674829609025669. [DOI] [PubMed] [Google Scholar]
- 42.Zhou Q, O’Brien B, Relyea J. Severity of nausea and vomiting during pregnancy: what does it predict? Birth. 1999;26:108–114. doi: 10.1046/j.1523-536x.1999.00108.x. [DOI] [PubMed] [Google Scholar]
- 43.Smart Richman L, Pek J, Pascoe E, Bauer DJ. The effects of perceived discrimination on ambulatory blood pressure and affective responses to interpersonal stress modeled over 24 hours. Health Psychol. 2010;29:403–411. doi: 10.1037/a0019045. [DOI] [PubMed] [Google Scholar]
- 44.Tomfohr L, Cooper DC, Mills PJ, Nelesen RA, Dimsdale JE. Everyday discrimination and nocturnal blood pressure dipping in Black and White Americans. Psychosom Med. 2010;72:266–272. doi: 10.1097/PSY.0b013e3181d0d8b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lewis TT, Kravitz HM, Janssen I, Powell LH. Self-reported experiences of discrimination and visceral fat in middle-aged African-American and Caucasian women. Am J Epidemiol. 2011;173:1223–1231. doi: 10.1093/aje/kwq466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lewis TT. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN heart study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- 47.Ickovics JR, Kershaw TS, Westdahl C, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol. 2007;110:330–339. doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kershaw TS, Magriples U, Westdahl C, Rising SS, Ickovics JR. Pregnancy as a window of opportunity for HIV prevention: effects of an HIV intervention delivered within prenatal care. Am J Public Health. 2009;99:2079–2086. doi: 10.2105/AJPH.2008.154476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lewis TT, Yang FM, Jacobs EA, Fitchett G. Racial/ethnic differences in response to the everyday discrimination scale: a differential item functioning analysis. Am J Epidemiol. doi: 10.1093/aje/kwr287. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams DR, Yan Yu, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 51.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 52.McCorkle R, Young K. Development of a symptom distress scale. Cancer Nurs. 1978;1:373–378. [PubMed] [Google Scholar]
- 53.Magriples U, Kershaw TS, Rising SS, Massey Z, Ickovics JR. Prenatal health care beyond the obstetrics service: utilization and predictors of unscheduled care. Am J Obstet Gynecol. 2008;198:75.e1–75.e7. doi: 10.1016/j.ajog.2007.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gans GM, Ross E, Barner CW, Wylie-Rosett J, McMurray J, Eaton C. REAP and WAVE: new tools to rapidly assess/discuss nutrition with patients. J Nutr. 2003;133:556S–562S. doi: 10.1093/jn/133.2.556S. [DOI] [PubMed] [Google Scholar]
- 55.Kline RB. Principles and Practice of Structural Equation Modeling. 2. New York: The Guilford Press; 2005. [Google Scholar]
- 56.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- 57.Beatty DL, Hall MH, Kamarck TA, et al. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychol. 2011;30:351–359. doi: 10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kramer MS. Determinants of low birth weight: Methodological assessment and meta-analysis. Bull World Health Organ. 1987;65:663–737. [PMC free article] [PubMed] [Google Scholar]
- 59.Black SE, Devereux PJ, Salvanes KG. From the cradle to the labor market? The effect of birth weight on adult outcomes. Q J Econ. 2007;122:409–439. [Google Scholar]
- 60.Matte TD, Bresnahan M, Begg MD, Susser E. Influence of variation in birth weight within normal range and within sibships on IQ at age 7 years: cohort study. BMJ. 2001;323:310–314. doi: 10.1136/bmj.323.7308.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Richards M, Hardy R, Kuh D, Wadsworth ME. Birth weight and cognitive function in the British 1946 birth cohort: longitudinal population based study. BMJ. 2001;322:199–203. doi: 10.1136/bmj.322.7280.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oreopoulos P, Stabile M, Walld R, Roos LL. Short-, medium-, and long-term consequences of poor infant health: an analysis using siblings and twins. J Hum Resour. 2008;43:88–138. [Google Scholar]
- 63.Jackson FM, Hogue CR, Phillips MT. The development of a race and gender-specific stress measure for African-American women: Jackson, Hogue, Phillips contextualized stress measure. Ethn Dis. 2005;15:594–600. [PubMed] [Google Scholar]
- 64.Woods-Giscombé CL, Lobel M. Race and gender matter: a multidimensional approach to conceptualizing and measuring stress in African American women. Cultur Divers Ethnic Minor Psychol. 2008;14:173–182. doi: 10.1037/1099-9809.14.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berger MT. Workable Sisterhood: The Political Journey of Stigmatized Women with HIV/AIDS. Princeton, NJ: Princeton University Press; 2004. [Google Scholar]