Abstract
Laparoscopic liver resections are being performed with increasing frequency, with several groups having reported minimally invasive approaches for major anatomic hepatic resections. Some surgeons favor a pure laparoscopic approach, while others prefer a hand-assisted approach for major laparoscopic liver resections. There are clear advantages and disadvantages to a hand-assisted technique. The purpose of this study is to summarize the literature comparing pure laparoscopic and hand-assisted approaches for minimally invasive hepatic resection, and to describe our approach in 432 laparoscopic liver resections.
Keywords: Laparoscopic, Liver, Hepatectomy
Introduction
Laparoscopic liver resection (LLR) is now an important technique in the field of hepatic surgery with >3,000 cases performed worldwide [1–6]. Minimally invasive liver resection is carried out for benign and malignant tumors with low operative mortality (0.3 %) and morbidity (11 %) [1]. Overall benefits of LLR compared to open liver resection (OLR) have been reported in a large review of 31 case-controlled matched studies [7] as well as six recent meta-analyses [8–13] and include reduced operative blood loss, less post-operative pain, and shorter length of stay.
Variations of the laparoscopic approach to liver resection surgery include pure laparoscopic, hand-assisted, hybrid technique, and robotic liver resection [1, 14, 15]. Selection of approach depends on tumor size and location, extent of resection, and surgeon preference. Some advocate starting with a pure laparoscopic approach with conversion to hand-assistance only if bleeding or technical difficulties are encountered [16], while others prefer to start with the hand-port incision if a laparoscopic hepatic lobectomy is planned [1, 3, 17]. For major anatomic LLRs, some recommend the hybrid approach where the liver is mobilized laparoscopically with the resection being completed through a small open (~14 cm) incision [18, 19].
Many high-volume centers use a pure laparoscopic approach for peripherally located easily accessible lesions, and reserve a hand-assisted or hybrid technique for formal hepatic lobectomies. In a 2009 review of the literature, Nguyen et al. [1] reported an exponential growth in the numbers of LLRs performed in the past decade, with >2,800 cases being performed worldwide. A pure laparoscopic approach was utilized in 75 % of cases, hand-assisted in 17 %, and hybrid approach in 2 %, with the remaining cases being carried out with gasless, thoracoscopic, or full conversion to open approaches. 45 % of laparoscopic cases were non-anatomic segmentectomy/ wedge resection, while anatomic left lateral sectionectomy was performed in 20 % of cases, right hepatectomy in 9 %, and left hepatectomy in 7 % [1]. Laparoscopic extended hepatic lobectomies or trisectionectomies have been reported only in small numbers [20, 21].
Several groups have described small series of laparoscopic major liver resections [22–25]. Dagher et al. [26] recently reported the results of a large multi-center international study of laparoscopic major hepatectomy. In this study, prospective databases collected between 1997 and 2008 from 3 European, 2 USA, and 1 Australian center were combined. Of 210 major liver resections, 136 right (65 %) and 74 left (35 %) hepatic lobectomies were performed. A pure laparoscopic approach was used in 91 (43 %) patients and hand-assisted in 119 (57 %). Open conversion was required in 26 (12.4 %) cases. The reason for conversion to open was unsatisfactory progress in 10 patients, bleeding in 6 patients, difficulty in obtaining tumor margin in 4 patients, posterior tumor location in 2 patients, portal vein or inferior vena cava injury in 3 patients, and anesthetic concern in 1 patient. Median tumor size was 5.4 cm and median surgical margin was 10.5 mm. There were no operative deaths, and 2 patients (1.0 %) died post-operatively from pulmonary embolus and urosepsis, respectively [26].
LLR has also been performed selectively for living donor liver transplantation. Cherqui et al. [27] were the first to report laparoscopic living donor left lateral sectionectomy for adult to child liver transplantation, and subsequently, a larger series of 16 cases was reported by the same group [28]. For the left lateral sectionectomy, a pure laparoscopic approach was used and the specimen was retrieved via a suprapubic Pfannenstiel incision. Two other groups have described laparoscopic-assisted live donor right or left hepatectomy for adult-to-adult liver transplantation [29, 30]. These groups start the operation laparoscopically for liver mobilization and initial vascular dissection, and then complete the transection through a small open incision. However, due to the stressful nature and overall low numbers of living donor hepatectomies, LLR for this indication has not been widely adopted.
Trocar placement and advantages/disadvantages of a hand-port
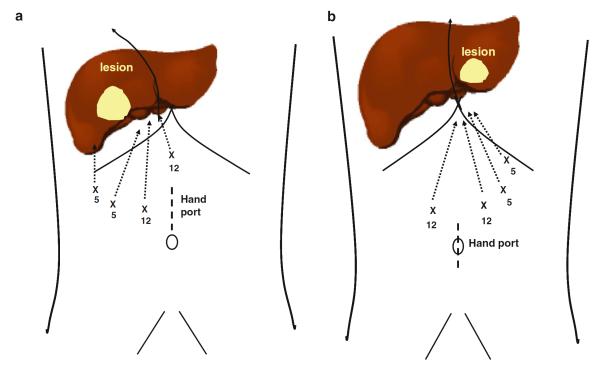
Hand-port and trocar positioning are shown for hand-assisted right (Fig. 1a) and left hepatic lobecotmy (Fig. 1b). Advantages of the hand-port are (1) tactile feedback, (2) facilitation of liver mobilization, (3) ability to manually compress the liver, and (4) eliminating the need for making a separate extraction site incision. Conversely, disadvantages of the hand port are (1) lack of domain, (2) interference with the laparoscopic trocars and instruments, (3) risk of hand-port incisional herniation, and (4) increased post-operative pain. Furthermore, a learning curve to using a hand-port clearly exists. For much of the operation, the hand is not in the hand-port, allowing for the placement of 1–2 additional trocars through the hand-port, as needed. An additional trocar can also be placed next to the hand while in the port if required.
Fig. 1.
Port placement for laparoscopic hand-assisted right (a) and left lobectomy (b). For right lobectomy, an 8 cm hand access site is placed in the supraumbilical position. Two 12 and two 5 mm ports are placed in the subxiphoid, R paramedian and R subcostal positions, respectively for hand-assisted liver mobilization and transaction. For left lobectomy, the hand access site is placed more inferiorly and the trocar positioning is essentially inverted from that of a right lobectomy with the exception of the 12 mm subxiphoid port being placed in the right paramedian position instead for appropriate angling for laparoscopic staple firing
For right hepatic lobectomy, a hybrid technique is anticipated/planned, then hand access (~8 cm) is placed in the upper midline or right subcostal position, allowing for extension to a small open incision (~14 cm). With the hybrid technique, the liver is mobilized laparoscopically and then delivered into the extended hand-port incision. Visualization and retractor placement is limited with this technique, making the amount of work that is accomplished laparoscopically paramount.
The UPMC experience
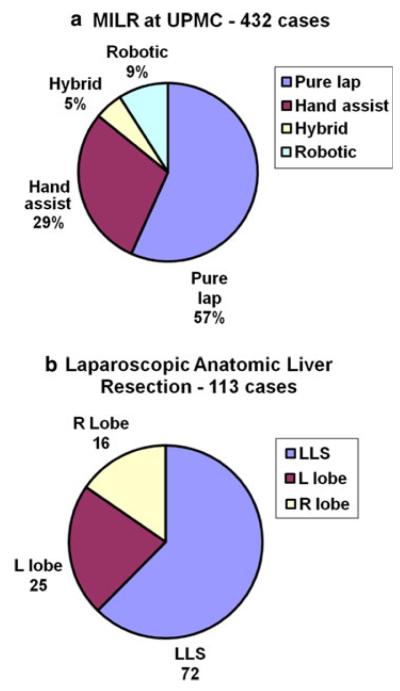
The minimally invasive liver resection (MILR) program at the University of Pittsburgh Medical Center (UPMC) began in 2001 and initially consisted entirely of a totally laparoscopic approach to lesions in the left lateral segments or right anterior segments. With more experience, anatomic lobectomies were performed and hand-assisted or hybrid approaches were used selectively. Beginning in 2007, robotic minimally invasive liver resection was started, and these operations are carried out totally minimally invasively. From 2001 to 2011, there have been a total of 432 minimally invasive liver resections performed. A pure laparoscopic approach was utilized in 245 cases (57 %), hand-assisted in 126 (29 %), hybrid in 22 (5 %), and robotic in 39 (9 %) cases (Fig. 2a).
Fig. 2.
Summary of minimally invasive liver resection (a) and laparoscopic anatomic resection (b) experiences at University of Pittsburgh Medical Center (UPMC) (2001–2011). 432 total minimally invasive liver resections including pure laparoscopic, hand-assisted, hybrid and robotic techniques were performed at UPMC over the last decade. The majority of anatomic resections carried out at UPMC were left lateral sectionectomies (LLS) followed in order of decreasing frequency, left and right hepatic lobectomy
Our experience with laparoscopic anatomic liver resections consists of left lateral sectionectomy, left hepatic lobectomy, and right hepatic lobectomy. Of the 432 MILR, 113 (26 %) laparoscopic anatomic resections have been performed. 72 laparoscopic left lateral sectionectomies, 25 laparoscopic left hepatic lobectomies, and 16 laparoscopic right hepatic lobectomies were performed, comprising 63.7, 22.1 and 14.2 % of the laparoscopic anatomic liver resections, respectively (Fig. 2b). A 3.5 % conversion rate (4/113 cases) exists in our series due to bleeding (maximum transfusion 2 units packed red blood cells [pRBC]) or additional tumors.
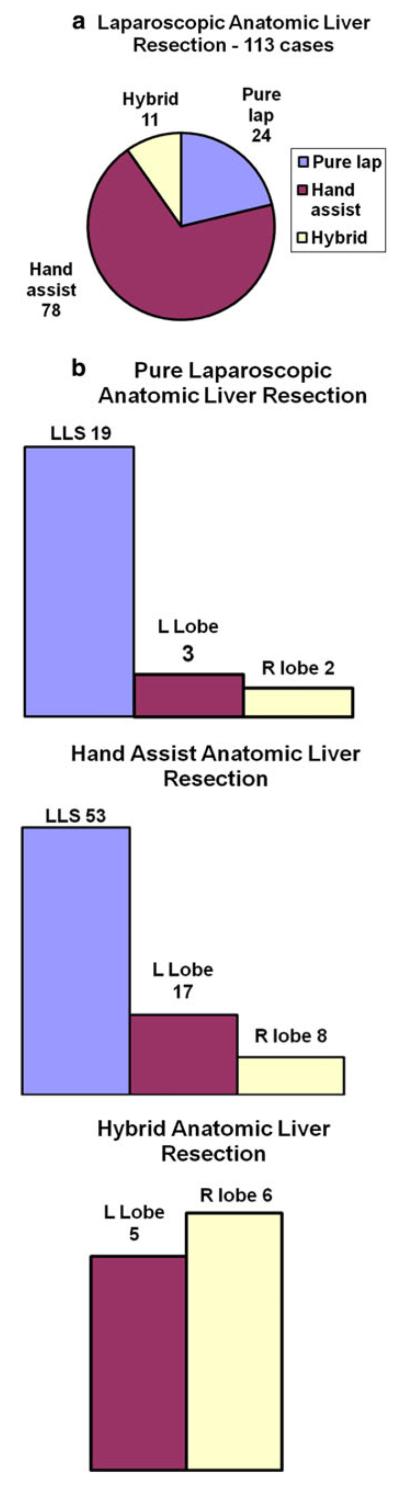
The hand-assisted technique was used in 78 cases (69 %), while pure laparoscopic and hybrid approaches accounted for 24 (21.3 %) and 11 (9.7 %) of the 113 anatomic liver resections, respectively (Fig. 3a). Of the 78 hand-assisted cases, 53 (67.9 %) were left lateral sectionectomies, 17 (21.8 %) were left lobectomies and 8 (10.3 %) were right lobectomies (Fig. 3b). Of the 24 pure laparoscopic cases, 19 (79.2 %) were left lateral sectionectomies, 3 (12.5 %) were left lobectomies and 2 (8.3 %) were right lobectomies. Finally, 5 (45.4 %) of the 11 cases in which the hybrid technique was utilized were left lobectomies while 6 (54.6 %) were right lobectomies.
Fig. 3.
Summary of University of Pittsburgh Medical Center (UPMC) laparoscopic anatomic liver resection experience (2001–2011) as broken down by technique (pure laparoscopic vs. hand-assisted vs. hybrid) (a) and type of resection performed (left lateral sectionectomy, left lobectomy, right lobectomy) utilizing each technique (b). The majority of laparoscopic anatomic lobectomies performed at UPMC were carried out utilizing a hand-assisted technique. Furthermore, the vast majority of left and right lobetcomies (88 %) performed in our experience were carried out with either hand assistance or via the hybrid technique
Operative parameters in our laparoscopic anatomic liver resection series are summarized in Table 1. Estimated blood loss and need for pRBC transfusion was similar amongst the three MILR techniques; however, the pure laparoscopic group had shorter operative times (188 min) compared to the hand-assisted (264 min) and hybrid groups (298 min). The numbers of complications as a percentage of total cases in each group were similar with 3/24 in the pure laparoscopic group, 7/78 in the hand-assisted, and 2/11 in the hybrid group (Table 1). There were more major complications, defined as those requiring invasive intervention to manage, in the hand-assisted group [4] than the pure laparoscopic [1] or hybrid [1] groups. The one major complication in the pure laparoscopic group was hypotension requiring pRBC transfusion, re-intubation and management in the intensive care unit (ICU) while that in the hybrid group was an intra-abdominal abscess that required placement of a percutaneous drainage catheter. In the hand-assisted group, there was one bile leak whose closure was facilitated by endoscopic retrograde cholangiopancreatography and stenting. In the hand-port and hybrid groups, 3/89 (3.3 %) incisional hernias developed post-operatively that required surgical repair.
Table 1.
Operative (A) and post-operative (B) characteristics of 113 laparoscopic anatomic liver resections performed at University of Pittsburgh Medical Center (UPMC) (2001–2011) as broken down by technique utilized
| Pure laparoscopic (24 cases) |
Hand- assisted (78 cases) |
Hybrid (11 cases) |
|
|---|---|---|---|
| A Operative characteristics of 113 laparoscopic anatomic liver resections | |||
| Left lateral sectionectomy |
19 | 53 | 0 |
| Left | 3 | 17 | 5 |
| Right | 2 | 8 | 6 |
| Benign/malignant | 16/8 | 57/21 | 3/8 |
| EBL (mL) | 91 ± 104 | 96 ± 97 | 93 ± 49 |
| Transfusions (# of pRBC units) |
1 | 4 | 0 |
| OR time (min) | 188.2 ± 92/7* | 264.5 ± 71.2 | 298.4 ± 82.2 |
| B Post-operative characteristics of 113 laparoscopic anatomic liver resections | |||
| Complication rate | 3 | 7 | 2 |
| Major complication rate |
1 | 4 | 1 |
| Post-operative ICU stay |
1 | 3 | 0 |
| Length of stay (days) |
2.5 ± 1.5* | 3.5 ± 1.5 | 3.8 ± 1.5 |
| 30-day mortality | 0 | 0 | 0 |
The pure laparoscopic series of patients exhibited decreased overall recovery times and lengths of stay compared to patients in the hand-assisted and hybrid groups. This reflects the increased complexity of cases done in both the hand-assisted and hybrid groups compared to the pure laparoscopic group
EBL estimated blood loss, LLR laparoscopic liver resection, OLR open liver resection, MILR minimally invasive liver resection, OR overall recovery, pRBC packed red blood cells, UPMC University of Pittsburgh Medical Center
Asterisk indicates p < 0.05 vs hand-assisted or hybrid groups
Discussion
Minimally invasive approaches to liver resection have been increasingly utilized in the past decade [1, 7] Worldwide experience with LLR has matured sufficiently to allow the theoretical advantages over an open approach to be evaluated in numerous case-controlled studies. Advantages of LLR include decreased blood loss, less post-operative pain, more rapid return to diet, and shorter length of stay, all of which have been well-documented when LLR has been compared to OLR in case-controlled studies [7]. Importantly, when matched for extent of resection and tumor size, comparable oncologic outcomes have been shown between LLR and OLR for surgical margins, R0 resection rate, and 3-year or 5 year-overall survival rates for both for hepatocellular carcinoma and metastatic colorectal cancer [1, 7, 10, 14, 31–42]. Furthermore, cost-effectiveness has also been demonstrated where the added expense of disposables used in the operating room is more than offset by ~50 % reduction in length of stay for LLR, resulting in actual decreased overall hospital costs [7, 16, 43–45].
In summary, laparoscopic major hepatectomy remains a technically demanding procedure and should only be performed by experienced hepatobiliary surgeons after adequate training and volume of minimally invasive non-anatomic resections [46]. Placement of a hand-port for hand-assisted or hybrid technique has both advantages and disadvantages, and is largely dependent on preference of the surgeon. In our experience, a pure laparoscopic approach resulted in reduced operating room time and length of stay compared to the other two groups; however, there is certainly a selection bias in choosing easier cases for a pure laparoscopic approach. Furthermore, in our experience, the majority of anatomic left or right formal hepatic lobectomies are performed with the hand-assisted approach. Further data is needed to determine what benefits a pure laparoscopic approach confers over the hand-assisted or hybrid approaches for major hepatectomy.
Footnotes
Conflict of interest None.
References
- 1.Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection—2,804 patients. Ann Surg. 2009;250(5):831–41. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen KT, Geller DA. Laparoscopic liver resection—current update. Surg Clin North Am. 2010;90(4):749–60. doi: 10.1016/j.suc.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009;250(5):825–30. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]
- 4.Tsuchiya M, Otsuka Y, Tamura A, Nitta H, Sasaki A, Wakabayashi G, Kaneko H. Status of endoscopic liver surgery in Japan: a questionnaire survey conducted by the Japanese Endoscopic Liver Surgery Study Group. J Hepatobiliary Pancreat Surg. 2009;16(4):405–9. doi: 10.1007/s00534-009-0119-1. [DOI] [PubMed] [Google Scholar]
- 5.Vigano L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009;16(4):410–21. doi: 10.1007/s00534-009-0120-8. [DOI] [PubMed] [Google Scholar]
- 6.Reddy SK, Tsung A, Geller DA. Laparoscopic liver resection. World J Surg. 2011;35(7):1478–86. doi: 10.1007/s00268-010-0906-5. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011;146(3):348–56. doi: 10.1001/archsurg.2010.248. [DOI] [PubMed] [Google Scholar]
- 8.Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, Antoniou A. Laparoscopic versus open hepatic resections for benign and malignant neoplasms—a meta-analysis. Surgery. 2007;141(2):203–11. doi: 10.1016/j.surg.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 9.Croome KP, Yamashita MH. Laparoscopic vs open hepatic resection for benign and malignant tumors: an updated meta-analysis. Arch Surg. 2010;145(11):1109–18. doi: 10.1001/archsurg.2010.227. [DOI] [PubMed] [Google Scholar]
- 10.Zhou YM, Shao WY, Zhao YF, Xu DH, Li B. Meta-analysis of laparoscopic versus open resection for hepatocellular carcinoma. Dig Dis Sci. 2011;56(7):1937–43. doi: 10.1007/s10620-011-1572-7. [DOI] [PubMed] [Google Scholar]
- 11.Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu HM, Pearce NW, Primrose JN, Sutcliffe RP. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 2011;13(5):295–308. doi: 10.1111/j.1477-2574.2011.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mizuguchi T, Kawamoto M, Meguro M, Shibata T, Nakamura Y, Kimura Y, Furuhata T, Sonoda T, Hirata K. Laparoscopic hepatectomy: a systematic review, meta-analysis, and power analysis. Surg Today. 2011;41(1):39–47. doi: 10.1007/s00595-010-4337-6. [DOI] [PubMed] [Google Scholar]
- 13.Li N, Wu YR, Wu B, Lu MQ. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: a meta-analysis. Hepatol Res. 2012;42(1):51–9. doi: 10.1111/j.1872-034X.2011.00890.x. [DOI] [PubMed] [Google Scholar]
- 14.Sasaki A, Nitta H, Otsuka K, Takahara T, Nishizuka S, Wakabayashi G. Ten-year experience of totally laparoscopic liver resection in a single institution. Br J Surg. 2009;96(3):274–9. doi: 10.1002/bjs.6472. [DOI] [PubMed] [Google Scholar]
- 15.Kitisin K, Packiam V, Bartlett DL, Tsung A. A current update on the evolution of robotic liver surgery. Minerva Chir. 2011;66(4):281–93. [PubMed] [Google Scholar]
- 16.Koffron AJ, Auffenberg G, Kung R, Abecassis M. Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg. 2007;246(3):385–92. doi: 10.1097/SLA.0b013e318146996c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fong Y, Jarnagin W, Conlon KC, DeMatteo R, Dougherty E, Blumgart LH. Hand-assisted laparoscopic liver resection: lessons from an initial experience. Arch Surg. 2000;135(7):854–9. doi: 10.1001/archsurg.135.7.854. [DOI] [PubMed] [Google Scholar]
- 18.Koffron AJ, Kung RD, Auffenberg GB, Abecassis MM. Laparoscopic liver surgery for everyone: the hybrid method. Surgery. 2007;142(4):463–8. doi: 10.1016/j.surg.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Nitta H, Sasaki A, Fujita T, Itabashi H, Hoshikawa K, Takahara T, Takahashi M, Nishizuka S, Wakabayashi G. Laparoscopy-assisted major liver resections employing a hanging technique: the original procedure. Ann Surg. 2010;251(3):450–3. doi: 10.1097/SLA.0b013e3181cf87da. [DOI] [PubMed] [Google Scholar]
- 20.Gumbs AA, Bar-Zakai B, Gayet B. Totally laparoscopic extended left hepatectomy. J Gastrointest Surg. 2008;12(7):1152. doi: 10.1007/s11605-007-0461-z. [DOI] [PubMed] [Google Scholar]
- 21.Gumbs AA, Gayet B. Multimedia article. Totally laparoscopic extended right hepatectomy. Surg Endosc. 2008;22(9):2076–7. doi: 10.1007/s00464-008-9979-8. [DOI] [PubMed] [Google Scholar]
- 22.O’Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg. 2004;8(2):213–6. doi: 10.1016/j.gassur.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 23.Topal B, Aerts R, Penninckx F. Laparoscopic intrahepatic Glissonian approach for right hepatectomy is safe, simple, and reproducible. Surg Endosc. 2007;21(11):2111. doi: 10.1007/s00464-007-9303-z. [DOI] [PubMed] [Google Scholar]
- 24.Gayet B, Cavaliere D, Vibert E, Perniceni T, Levard H, Denet C, Christidis C, Blain A, Mal F. Totally laparoscopic right hepatectomy. Am J Surg. 2007;194(5):685–9. doi: 10.1016/j.amjsurg.2006.11.044. [DOI] [PubMed] [Google Scholar]
- 25.Dagher I, Di GG, Dubrez J, Lainas P, Smadja C, Franco D. Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg. 2009;198(2):173–7. doi: 10.1016/j.amjsurg.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 26.Dagher I, O’Rourke N, Geller DA, Cherqui D, Belli G, Gamblin TC, Lainas P, Laurent A, Nguyen KT, Marvin MR, Thomas M, Ravindra K, Fielding G, Franco D, Buell JF. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg. 2009;250(5):856–60. doi: 10.1097/SLA.0b013e3181bcaf46. [DOI] [PubMed] [Google Scholar]
- 27.Cherqui D, Soubrane O, Husson E, Barshasz E, Vignaux O, Ghimouz M, Branchereau S, Chardot C, Gauthier F, Fagniez PL, Houssin D. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet. 2002;359(9304):392–6. doi: 10.1016/S0140-6736(02)07598-0. [DOI] [PubMed] [Google Scholar]
- 28.Soubrane O, Cherqui D, Scatton O, Stenard F, Bernard D, Branchereau S, Martelli H, Gauthier F. Laparoscopic left lateral sectionectomy in living donors: safety and reproducibility of the technique in a single center. Ann Surg. 2006;244(5):815–20. doi: 10.1097/01.sla.0000218059.31231.b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koffron AJ, Kung R, Baker T, Fryer J, Clark L, Abecassis M. Laparoscopic-assisted right lobe donor hepatectomy. Am J Transplant. 2006;6(10):2522–5. doi: 10.1111/j.1600-6143.2006.01498.x. [DOI] [PubMed] [Google Scholar]
- 30.Kurosaki I, Yamamoto S, Kitami C, Yokoyama N, Nakatsuka H, Kobayashi T, Watanabe T, Oya H, Sato Y, Hatakeyama K. Video-assisted living donor hemihepatectomy through a 12-cm incision for adult-to-adult liver transplantation. Surgery. 2006;139(5):695–703. doi: 10.1016/j.surg.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 31.Shimada M, Hashizume M, Maehara S, Tsujita E, Rikimaru T, Yamashita Y, Tanaka S, Adachi E, Sugimachi K. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc. 2001;15(6):541–4. doi: 10.1007/s004640080099. [DOI] [PubMed] [Google Scholar]
- 32.Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003;138(7):763–9. doi: 10.1001/archsurg.138.7.763. [DOI] [PubMed] [Google Scholar]
- 33.Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Maeda T, Shiba T. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg. 2005;189(2):190–4. doi: 10.1016/j.amjsurg.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 34.Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, Karoui M, Duvoux C, Dhumeaux D, Fagniez PL. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006;243(4):499–506. doi: 10.1097/01.sla.0000206017.29651.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cai XJ, Yang J, Yu H, Liang X, Wang YF, Zhu ZY, Peng SY. Clinical study of laparoscopic versus open hepatectomy for malignant liver tumors. Surg Endosc. 2008;22(11):2350–6. doi: 10.1007/s00464-008-9789-z. [DOI] [PubMed] [Google Scholar]
- 36.Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM. Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol. 2009;16(6):1572–7. doi: 10.1245/s10434-009-0414-8. [DOI] [PubMed] [Google Scholar]
- 37.Belli G, Limongelli P, Fantini C, D’Agostino A, Cioffi L, Belli A, Russo G. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg. 2009;96(9):1041–8. doi: 10.1002/bjs.6680. [DOI] [PubMed] [Google Scholar]
- 38.Tranchart H, Di GG, Lainas P, Roudie J, Agostini H, Franco D, Dagher I. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24(5):1170–6. doi: 10.1007/s00464-009-0745-3. [DOI] [PubMed] [Google Scholar]
- 39.Dagher I, Belli G, Fantini C, Laurent A, Tayar C, Lainas P, Tranchart H, Franco D, Cherqui D. Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg. 2010;211(1):16–23. doi: 10.1016/j.jamcollsurg.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 40.Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, et al. Minimally invasive liver resection for metastatic colorectal cancer: a multi-institutional, international report of safety, feasibility, and early outcomes. Ann Surg. 2009;250(5):842–8. doi: 10.1097/SLA.0b013e3181bc789c. [DOI] [PubMed] [Google Scholar]
- 41.Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B. Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg. 2009;250(5):849–55. doi: 10.1097/SLA.0b013e3181bcaf63. [DOI] [PubMed] [Google Scholar]
- 42.Kazaryan AM, Marangos IP, Røsok BI, Rosseland AR, Villanger O, Fosse E, et al. Laparoscopic resection of colorectal liver metastases: surgical and long-term oncologic outcome. Ann Surg. 2010;252(6):1005–12. doi: 10.1097/SLA.0b013e3181f66954. [DOI] [PubMed] [Google Scholar]
- 43.Vanounou T, Steel JL, Nguyen KT, Tsung A, Marsh JW, Geller DA, Gamblin TC. Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol. 2010;17(4):998–1009. doi: 10.1245/s10434-009-0839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tsinberg M, Tellioglu G, Simpfendorfer CH, Walsh RM, Vogt D, Fung J, Berber E. Comparison of laparoscopic versus open liver tumor resection: a case-controlled study. Surg Endosc. 2009;23(4):847–53. doi: 10.1007/s00464-008-0262-9. [DOI] [PubMed] [Google Scholar]
- 45.Polignano FM, Quyn AJ, de Figueiredo RS, Henderson NA, Kulli C, Tait IS. Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc. 2008;22(12):2564–70. doi: 10.1007/s00464-008-0110-y. [DOI] [PubMed] [Google Scholar]
- 46.Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009;250(5):772–82. doi: 10.1097/SLA.0b013e3181bd93b2. [DOI] [PubMed] [Google Scholar]