Abstract
The purpose of this study is to determine if patellar maltracking is more prevalent among patellofemoral (PF) pain subjects with patella alta compared to subjects with normal patella height. We imaged 37 PF pain and 15 pain free subjects in an open-configuration magnetic resonance imaging scanner while they stood in a weightbearing posture. We measured patella height using the Caton-Deschamps, Blackburne-Peel, Insall-Salvati, Modified Insall-Salvati, and Patellotrochlear indices, and classified the subjects into patella alta and normal patella height groups. We measured patella tilt and bisect offset from oblique-axial plane images, and classified the subjects into maltracking and normal tracking groups. Patellar maltracking was more prevalent among PF pain subjects with patella alta compared to PF pain subjects with normal patella height (two-tailed Fisher’s exact test, p < 0.050). Using the Caton-Deschamps index, 67% (8/12) of PF pain subjects with patella alta were maltrackers, whereas only 16% (4/25) of PF pain subjects with normal patella height were maltrackers. Patellofemoral pain subjects classified as maltrackers displayed a greater patella height compared to the pain free and PF pain subjects classified as normal trackers (two-tailed unpaired t-tests with Bonferroni correction, p < 0.017). This study adds to our understanding of PF pain in two ways - 1) we demonstrate that patellar maltracking is more prevalent in PF pain subjects with patella alta compared to subjects with normal patella height; and 2) we show greater patella height in PF pain subjects compared to pain free subjects using four indices commonly used in clinics.
Keywords: patellofemoral pain, patella alta, patellar maltracking, patella height, patella tilt, bisect offset
INTRODUCTION
Patellofemoral (PF) pain is common, accounting for approximately one in four knee conditions diagnosed in sports medicine clinics.1 Although there are several causes of PF pain, patella alta, or high-riding patella, is thought to predispose individuals to PF pain.2,3 A high-riding patella is theorized to engage the femoral trochlear groove at a greater knee flexion angle,4 resulting in less medial-lateral constraint of the patella and lateral patellar maltracking at low knee flexion angles. Lateral patellar maltracking is theorized to decrease PF contact area and increase joint stress, resulting in pain.5-10 However, a recent review of the literature concluded that the definition of patella alta and its causal relationship to the conditions associated with PF pain remain controversial.11
Evidence in support of a relationship between patella alta and maltracking in PF pain subjects is limited. Davies et al.12 and Moller et al.13 found that patella height (superior-inferior location of the patella with respect to the tibia or femur) was correlated with PF incongruence in subjects with PF pain or instability. Insall et al.14 found that average patella height was 25% greater in subjects with recurrent patella dislocations compared to non-dislocating controls. Ward et al.10 reported a greater lateral patellar displacement and tilt in subjects with patella alta compared to subjects with normal patella height. However, Ward et al.10 did not include or exclude subjects on the basis of pain. As a result, the relationship between patella height and patella tracking in PF pain subjects remains unclear.
A barrier to simultaneous measurement of patella height and tracking under weightbearing conditions is that patellar maltracking is primarily observed in low degrees of knee flexion (< 30°), and it is difficult to acquire axial scans in low degrees of knee flexion under weightbearing conditions using radiographic techniques.15,16 To overcome this limitation with radiographic techniques, we developed a method for imaging the knee joint in low degrees of flexion using an open-configuration magnetic resonance imaging (MRI) scanner.17 Using the open-configuration MRI scanner we evaluated the PF joint in an upright position with ~45% body weight supported by the measured limb; this is in contrast to the Ward et al.10 and McWalter et al.18 studies that evaluated the PF joint in a supine position with ~15% body weight supported by the measured limb. We previously demonstrated the importance of measuring PF kinematics under weightbearing conditions19 and classified PF pain subjects into maltracking and normal tracking groups.20,21 The purpose of this study was to investigate the relationship between patella height and patella tracking in PF pain subjects. We hypothesized that patellar maltracking was more prevalent among PF pain subjects with patella alta compared to PF pain subjects with normal patella height.
METHODS
Subject recruitment
Fifty-two subjects were recruited for this study: 37 subjects with chronic PF pain and 15 pain free subjects (Table 1). The PF pain group included 17 males (31.9 ± 7.2 years, 1.80 ± 0.08 m, 74.4 ± 10.5 kg) and 20 females (30.1 ± 4.7 years, 1.68 ± 0.06 m, 63.1 ± 9.6 kg). The pain free group included 7 males (28.0 ± 2.9 years, 1.80 ± 0.07 m, 73.2 ± 4.2 kg) and 8 females (28.8 ± 4.7 years, 1.66 ± 0.05 m, 58.3 ± 4.6 kg). There were no statistically significant differences in age, height or weight between the male PF pain and pain free subjects, or between the female PF pain and pain free subjects (two-tailed, unpaired t-tests, p < 0.050). The PF pain subjects were recruited from the university’s orthopaedic clinics and sports medicine centers, and were diagnosed by a sports medicine physician with over 20 years of clinical experience. The pain free subjects were recruited from the local community and screened for previous injuries or knee disorders. A subject was included in the PF pain group if he/she reported consistent anterior knee pain for longer than 3 months (ranging from 3 months to 11 years), and if he/she experienced reproducible pain during at least two of the following activities: stair ascent/descent, kneeling, squatting, prolonged sitting, or isometric quadriceps contraction.22 For subjects with bilateral pain, the more painful knee at the time of examination was included in this study. A PF pain subject was excluded if he/she had demonstrated knee ligament instability, pain in the patellar tendon during clinical exam or signs of degeneration of the patellar tendon observed from MRI, joint line tenderness or knee effusion, previous knee trauma or surgery, patellar dislocation, or if signs of osteoarthritis were detected from MRI of the knee. We used the Anterior Knee Pain Score23 to evaluate subjective symptoms and functional limitations in the PF pain subjects. The Anterior Knee Pain Score consists of 13 multiple-choice questions. A score of 100 indicated no pain or disability. The subjects were instructed to complete the questionnaire independently to exclude investigator bias.23 The score for the PF pain subjects averaged 73 (range 42-97). Subjects were informed on all aspects of the study and provided consent according to the policies of our Institutional Review Board.
Table 1.
Population characteristics of the patellofemoral pain and pain free subjects.
| Patellofemoral pain (n = 37) | Pain free (n = 15) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | |
| Age (years) | 30.9 | 6.0 | 19.0 - 50.0 | 28.4 | 3.8 | 22.0 - 35.0 |
| Height (meters) | 1.73 | 0.09 | 1.57 - 1.93 | 1.72 | 0.09 | 1.58 - 1.91 |
| Weight (kilograms) | 68.3 | 11.4 | 46.5 - 90.7 | 65.3 | 8.8 | 52.1 - 77.3 |
Weightbearing MRI
We imaged the PF joint of all subjects in an upright, weightbearing posture using an open-configuration MRI scanner (0.5T SP/i MR, GE Healthcare, Milwaukee, WI).20 The subjects maintained an upright pose at approximately 5° knee flexion with the quadriceps engaged and without locking their knees. We used a goniometer to locate the greater trochanter, lateral femoral epicondyle, and lateral malleolus as a standardized metric for knee flexion. Subjects were assisted by a custom-built low-friction backrest that required a subject to support about 90% of his/her bodyweight. The subjects were requested to load both legs evenly during scanning. The scan parameters for the sagittal plane images were: repetition time, 33 milliseconds; echo time, 9 milliseconds; flip angle, 45°; matrix, 256 × 160 interpolated to 256 × 256; field of view, 20 × 20 cm; slice thickness, 2 mm; scan time, ~2 minutes. All subjects were able to maintain the upright position for the duration of the scan.
Measurement of patella height
We measured patella height from sagittal plane images acquired during the upright, weightbearing MRI at ~5° knee flexion (Figure 1). Studies have reported measuring patella height with the knee flexed more than 30° to eliminate kinks in the unloaded patellar tendon.11 Our patella height measurements near full knee extension are justified because we imaged all subjects under weightbearing conditions with the quadriceps muscles engaged, ensuring a kink-free patellar tendon, similar to the method used by Ward et al.10 We selected a sagittal scan plane corresponding to the apex of the patella to acquire the largest diagonal length of the patella. We used four established indices11 used in clinics for measuring patella height: 1) the Caton-Deschamps index,24,25 the ratio of the distance from the distal point of the patellar articular cartilage to the anterior-superior border of the tibia and patellar cartilage length; 2) the Blackburne-Peel index,26 the ratio of the perpendicular distance from a line drawn along the tibial plateau to the distal point of the patellar articular cartilage and patellar cartilage length; 3) the Insall-Salvati index,27 the ratio of the patellar tendon length and the patella bone diagonal length; and 4) the Modified Insall-Salvati index,28 the ratio of the distance from the tibial tubercle to the distal point of the patellar articular cartilage and patellar cartilage length (Figure 1). These four indices provide a measure of the height of the patella relative to the proximal tibia, but provide little insight into the position of the patella relative to the femoral trochlea. To acquire a direct measure of patella height relative to the femoral trochlea, we used the Patellotrochlear index,29,30 which is the ratio of the length of the femoral trochlear articular cartilage overlapping the patellar cartilage and patellar cartilage length. Direct comparison of patella height measurements from these five indices provide insight into method-dependency in categorization of patella alta.31 All patella height measurements were blinded; the subjects were randomized, and the investigator was unaware if an image set under analysis was from a PF pain or pain free subject, or from a maltracker or a normal tracker. The measurements were performed twice, on separate days, by the same investigator. Intra-rater reliability was measured using the Concordance Correlation Coefficient,32 and ranged from “fairly good” to “excellent” in all cases.33 The Concordance Correlation Coefficients (95% confidence interval) were 0.90 (0.82 -0.94), 0.87 (0.79 - 0.92), 0.96 (0.93 - 0.98), 0.94 (0.90 - 0.96), and 0.89 (0.82 - 0.93) for the Caton-Deschamps, Blackburne-Peel, Insall-Salvati, Modified Insall-Salvati, and Patellotrochlear indices, respectively. Average patella heights from the two measurements were reported.
Figure 1.
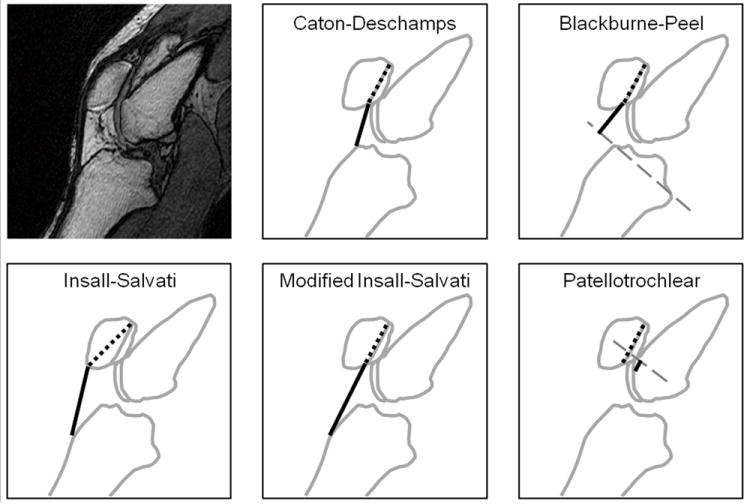
Measurement of patella height using common indices. Patella height was represented as the ratio of the length of a solid line to the length of a dotted line.
Categorization of subjects into patella alta and normal patella height groups
We categorized all subjects into patella alta and normal patella height groups based on thresholds calculated from our patella height measurements (Figure 3). A Gaussian distribution model best fit our empirical data, with the coefficients of determination (R2) being 0.98 (Caton-Deschamps) (Figure 3), 0.97 (Blackburne-Peel), 0.98 (Insall-Salvati), 0.99 (Modified Insall-Salvati), & 0.94 (Patellotrochlear). Fitting empirical data with distribution models, such as the Gaussian, is a standard statistical technique for representing population variability. The R2 is an indicator of how well a distribution model fits the empirical data; the closer R2 is to 1.00, the better a model fits the empirical data. In the case of our patella height measurements, R2 ≥ 0.94 demonstrates that the Gaussian distribution provided excellent fits to the measured patella height data. We defined patella height values corresponding to the 75th percentile of the distribution models as the thresholds for patella alta (Table 2). A subject was categorized with patella alta if his/her patella height index was in the highest quartile of the measured population data. The Patellotrochlear index is complement to the four established methods; a subject was categorized with patella alta if his/her Patellotrochlear index was in the lowest quartile of measured population data. Twelve (4 males, 8 females) out of 37 PF pain subjects and 1 (male) out of 15 pain free subjects were categorized with patella alta using the Caton-Deschamps index; similar percentages of populations were categorized with patella alta using the Blackburne-Peel, Insall-Salvati, and Modified Insall-Salvati indices (S-Table 3).
Figure 3.
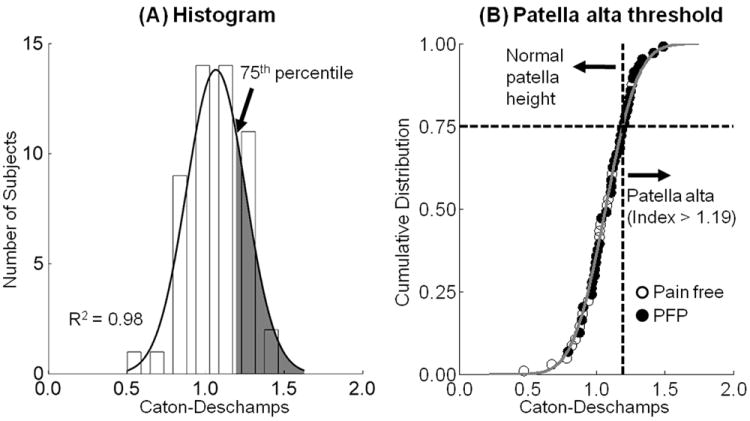
Categorization of patella alta using the Caton-Deschamps index in pain free and patellofemoral pain (PFP) subjects (total n = 52). The histogram distribution of Caton-Deschamps index (A) was fit with a Gaussian model (A, B: solid lines). A subject was categorized with patella alta if his/her patella height was greater than the 75th percentile threshold value (A: shaded region, B: vertical dashed line).
Table 2.
Patella alta thresholds based on the 75th percentile of the Gaussian distribution fit to the empirical data from this study compared to the range of previously published data.
Measurement of patellar tilt and bisect offset
We measured patellar tilt and bisect offset, patellar tracking measures, from an oblique-axial plane identified from the weightbearing 3D MRI volume (Figure 2).20,21 The oblique-axial plane was created to intersect the center of the patella and the most posterior points of the femoral condyles. Anatomical landmarks were identified on the oblique-axial plane image, including the most lateral and most medial points on the patella, the most posterior points on the femoral condyles, and the deepest point on the trochlea. Two patellar tracking measures, patellar tilt and bisect offset, were used to quantify the position of the patella with respect to the femur. Patellar tilt, a measure of patella internal-external rotation, was defined by the angle between the patella and the posterior femoral condyles.20 Bisect offset, a measure of patella medial-lateral translation, was defined as the percentage of the patella lateral to the midline of the femur.20 All patellar tilt and bisect offset measurements were performed by the same investigator; the average intraobserver variance between measurements was 2° for patellar tilt and 4% for bisect offset.20
Figure 2.
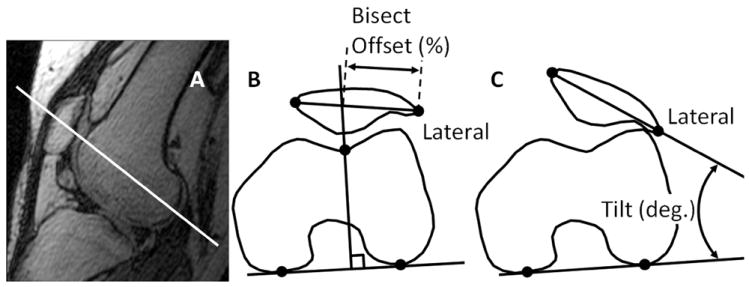
An oblique-axial plane (solid white line) intersecting the center of the patella and the most posterior points of the femoral condyles was created from 3D MRI volume (A). Anatomical landmarks (black dots) on the oblique-axial plane were used to determine bisect offset (B) and patellar tilt (C).
Classification of subjects into maltracking and normal tracking groups
Gender-specific maltracking thresholds based on the patellar tilt and bisect offset measurements were used to classify the PF pain and pain free subjects into maltracking and normal tracking groups (Figure 4). Gender-specific maltracking thresholds were required because of statistically significant differences in patellar tracking measures between males and females.20 A non-Gaussian two-parameter Weibull distribution model best fit the measured patellar tilt and bisect offset data, with R2 ≥ 0.86 in all cases. We defined gender-specific patellar tilt and bisect offset values corresponding to the 75th percentile of the Weibull model as thresholds for maltracking. The gender-specific maltracking thresholds were 11.9° (males) and 14.9° (females) for patellar tilt, and 68.9% (males) and 72.0% (females) for bisect offset. A subject was classified as a maltracker if either patellar tilt or bisect offset was greater than the corresponding gender-specific thresholds. Twelve (5 males, 7 females) out of 37 PF pain subjects and 4 (2 males, 2 females) out of 15 pain free subjects were classified as maltrackers. Out of the 12 PF pain subjects classified as maltrackers, seven had both abnormal patellar tilt and abnormal bisect offset, three had only abnormal patellar tilt, and two had only abnormal bisect offset. Out of the 12 PF pain subjects categorized with patella alta using the Caton-Deschamps index, six subjects were maltrackers with both abnormal patellar tilt and abnormal bisect offset, two subjects were maltrackers with only abnormal patellar tilt, and four subjects were normal trackers.
Figure 4.
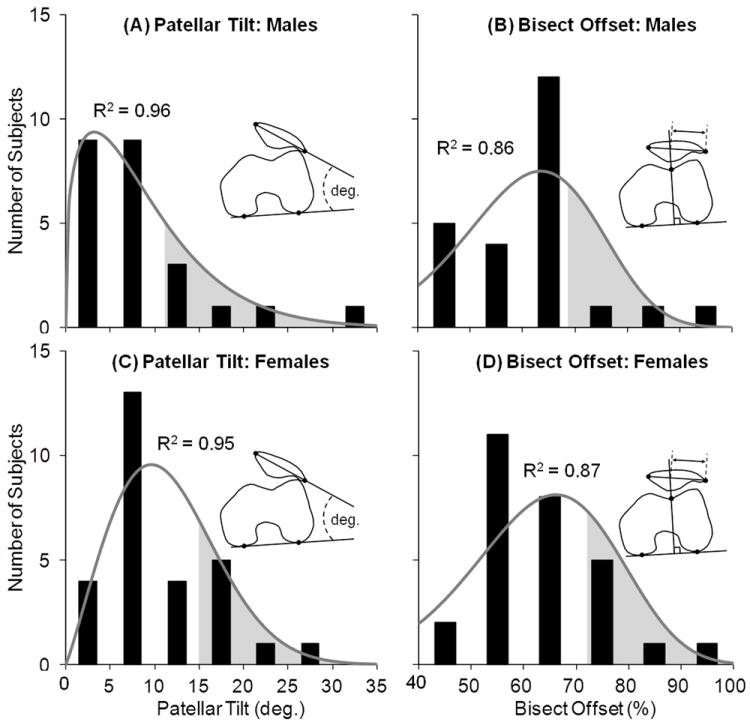
Classification of pain free and patellofemoral pain subjects into maltracking and normal tracking groups. The histogram distributions were best fit with a two-parameter Weibull model (solid lines). A subject was classified as a maltracker if his/her tilt or bisect offset was greater than the gender-specific 75th percentile maltracking thresholds (shaded regions).
Data analysis and statistical methods
We evaluated the difference in percentage of maltracking PF pain subjects between the patella alta and normal patella height groups using the two-tailed Fisher’s exact test (p < 0.050). We compared average patella height between the pain free and PF pain subjects classified into maltracking and normal tracking groups, and between all PF pain and all pain free groups using two-tailed, unpaired t-tests (post Bonferroni correction, p < 0.017 for the pain free and PF pain subjects classified into maltracking and normal tracking groups; p < 0.050 for all PF pain and all pain free groups). We compared average patellar tilt and bisect offset measures between PF pain subjects with patella alta and PF pain subjects with normal patella height using two-tailed, unpaired t-tests (p < 0.050). We compared average Anterior Knee Pain Score between PF pain subjects with patella alta and normal patella height, and between PF pain subjects classified into maltracking and normal tracking groups using two-tailed, unpaired t-tests (p < 0.050). We performed the above comparisons for all five patella height indices evaluated in this study. Our comparisons between the 37 PF pain and 15 pain free subjects were valid because we used two-tailed, unpaired t-tests to test the difference between the means of two groups. A two-tailed, unpaired t-test accounts for unequal sample size between groups (Glantz 2002, p. 79).34 Our study required a greater number of PF pain subjects than pain free subjects because our hypothesis tested sub-groups of PF pain subjects. We calculated the sample size of PF pain sub-groups using power calculations based on estimated prevalence of patella alta and patellar maltracking.
RESULTS
Lateral patellar maltracking was more prevalent among PF pain subjects with patella alta compared to PF pain subjects with normal patella height (Figure 5). Eight out of 12 (67%) PF pain subjects categorized with patella alta using the Caton-Deschamps index were classified as maltrackers; in comparison, only 4 out of 25 (16%) PF pain subjects categorized with normal patella height were classified as maltrackers. The percentage of maltracking PF pain subjects was greater in the patella alta group compared to the normal patella height group (p = 0.006). We obtained similar results using the Blackburne-Peel index (p = 0.010), while there was a trend towards significance using the Insall-Salvati (p = 0.067) and Modified Insall-Salvati (p = 0.067) indices.
Figure 5.
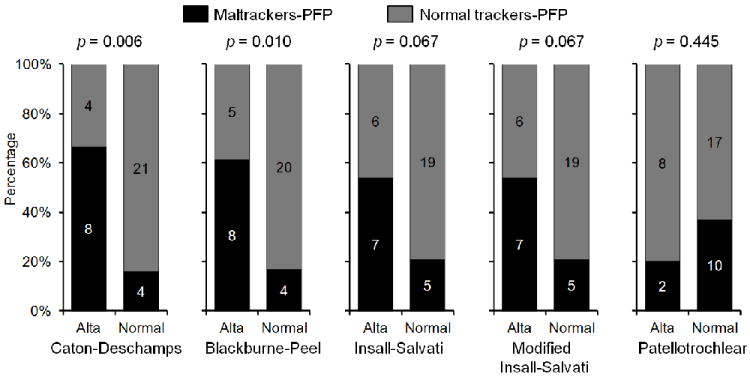
Percentage of patellofemoral pain (PFP) subjects with patella alta (Alta) and normal patella height (Normal) classified as maltrackers and normal trackers using the five indices. The bars are labeled with number of subjects in each group.
Patellofemoral pain subjects classified as maltrackers displayed a greater patella height compared to the pain free and PF pain subjects classified as normal trackers (Figure 6). Average Caton-Deschamps index for the PF pain subjects classified as maltrackers was 32% greater than the normal tracking pain free subjects (p < 0.001), and 16% greater than the normal tracking PF pain subjects (p < 0.001, Figure 6A). Similar differences in average patella height were observed using the Blackburne-Peel, Insall-Salvati, and Modified Insall-Salvati indices (Figures 6B-D). There were no differences in average Patellotrochlear index between the maltracking PF pain and normal tracking pain free subjects (p = 0.558), or between the maltracking PF pain and normal tracking PF pain subjects (p = 0.282, Figure 6E).
Figure 6.
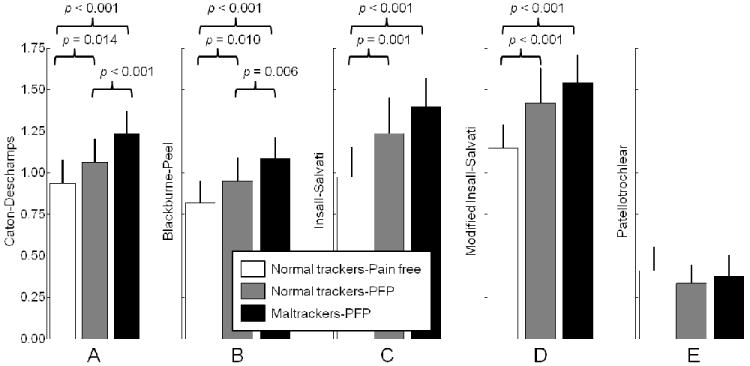
Average (+1 SD) patella height for pain free and patellofemoral pain (PFP) subjects classified into normal tracking and maltracking groups. Patella height was measured using the (A) Caton-Deschamps, (B) Blackburne-Peel, (C) Insall-Salvati, (D) Modified Insall-Salvati, and (E) Patellotrochlear indices.
Average patella height was greater in all PF pain subjects grouped together compared to all pain free subjects (Figure 7). Average patella height for all PF pain subjects was 20%, 29%, 30%, and 27% greater than the pain free subjects using the Caton-Deschamps, Blackburne-Peel, Insall-Salvati, and Modified Insall-Salvati indices, respectively (p < 0.001 for all four indices, Figures 7A-D). Average Patellotrochlear index was similar for the PF pain and pain free groups (p = 0.319, Figure 7E).
Figure 7.
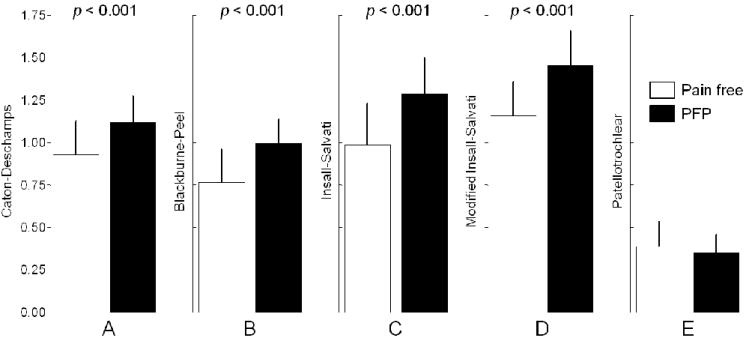
Average (+1 SD) patella height for pain free and patellofemoral pain (PFP) subjects using the (A) Caton-Deschamps, (B) Blackburne-Peel, (C) Insall-Salvati, (D) Modified Insall-Salvati, and (E) Patellotrochlear indices.
Average patellar tilt was greater in PF pain subjects with patella alta compared to PF pain subjects with normal patella height categorized using the Caton-Deschamps (p = 0.002) and the Insall-Salvati (p = 0.048) indices. Average ± SD patellar tilt values for PF pain subjects with patella alta and normal patella height categorized using the Caton-Deschamps index were 15.7° ± 9.2° and 8.3° ± 4.2°, respectively. Average ± SD patellar tilt values for PF pain subjects with patella alta and normal patella height categorized using the Insall-Salvati index were 13.8° ± 8.9° and 9.0° ± 5.3°, respectively. We found no differences in patellar tilt between PF pain subjects with patella alta and PF pain subjects with normal patella height categorized using the Blackburne-Peel (p = 0.061), the Modified Insall-Salvati (p = 0.069), or the Patellotrochlear (p = 0.108) indices. Furthermore, average ± SD bisect offset values for PF pain subjects with patella alta and normal patella height categorized using the Caton-Deschamps index were 68.5% ± 12.8% and 60.8% ± 10.4%, respectively, with a trend towards significance (p = 0.058). We found no differences in bisect offset values between PF pain subjects with patella alta and PF pain subjects with normal patella height categorized using the Blackburne-Peel (p = 0.559), Insall-Salvati (p = 0.619), Modified Insall-Salvati (p = 0.483), or the Patellotrochlear (p = 0.876) indices.
We found no difference in Anterior Knee Pain Score between PF pain subjects with patella alta and normal patella height categorized using the Caton-Deschamps (p = 0.782), Blackburne-Peel (p = 0.389), Insall-Salvati (p = 0.935), Modified Insall-Salvati (p = 0.724), or the Patellotrochlear (p = 0.841) indices. Average ± SD Anterior Knee Pain Scores for PF pain subjects with patella alta and normal patella height categorized using the Caton-Deschamps index were 72 ± 12 and 74 ± 15, respectively. We found similar average ± SD Anterior Knee Pain Scores for PF pain subjects with patella alta and normal patella height categorized using the Blackburne-Peel, Insall-Salvati, Modified Insall-Salvati, and Patellotrochlear indices. Furthermore, we found no differences in Anterior Knee Pain Score between PF pain subjects classified into maltracking and normal tracking groups (p = 0.406). Average ± SD Anterior Knee Pain Scores for PF pain subjects classified into maltracking and normal tracking groups were 70 ± 11 and 75 ± 15, respectively.
DISCUSSION
The aim of this study was to investigate the relationship between patella height and patella tracking in PF pain subjects. We hypothesized that patellar maltracking was more prevalent among PF pain subjects with patella alta compared to those with normal patella height. Our results support this hypothesis and demonstrate a greater percentage of patellar maltracking among the PF pain subjects with patella alta compared to PF pain subjects with normal patella height (Figure 5). We observed greater patella height in PF pain subjects classified as maltrackers compared to the normal tracking groups (Figure 6). These findings were consistent for patella height measurements using the Caton-Deschamps, Blackburne-Peel, Insall-Salvati, and Modified Insall-Salvati indices. Our hypothesis was not supported by results obtained using the Patellotrochlear index. It is difficult to deduce from our data why we found no relationships between patella height and patella tracking using the Patellotrochlear index. We speculate that patellar maltracking may be more sensitive to the height of the patella relative to the proximal tibia than the height of the patella relative to the distal femur articular surface. Furthermore, we found no differences in Anterior Knee Pain Scores between PF pain subjects with patella alta and normal patella height, and between PF pain subjects classified into maltracking and normal tracking groups. It is unclear why Anterior Knee Pain Score is not related to patella height or patella tracking measures. The Anterior Knee Pain Score consists of only 1 (out of 13) question pertaining to patella position;23 this questionnaire may not have the adequate sensitivity to capture the range of patella height and patellar tracking measured from MRI. Also, there are other sources of PF pain besides patellar maltracking, including fat pad and bone edema.
This study provides new evidence relating patellar maltracking to patella alta in PF pain subjects. Previous studies have reported relationships between patella height and PF joint congruence,12,13 and joint dislocation.14 Ward et al.10 reported a positive correlation between patella height and patella maltracking in a cohort of subjects with patella alta and normal patella height; however, it is unclear how many, if any, of these subjects were symptomatic with PF pain. Our study builds on the findings of the Ward et al.10 study to provide new insight into the prevalence of patellar maltracking in PF pain subjects with patella alta. Consistent with Ward et al.,10 we observed positive correlations between the Insall-Salvati index and patellar tilt (R2 = 0.11, p = 0.019), and Insall-Salvati index and bisect offset (R2 = 0.09, p = 0.035), when all PF pain and pain free subjects were grouped together. Within the PF pain subjects, we observed a positive correlation between the Insall-Salvati index and patellar tilt (R2 = 0.12, p = 0.034), but no correlation between the Insall-Salvati index and bisect offset (R2 = 0.04, p = 0.220).
This study addresses the controversial question of the presence of patella alta among PF pain subjects. It is unclear based on past studies if PF pain subjects have greater patella height compared to pain free subjects, and it is difficult to compare directly the findings of the previous studies, in part, because the studies used different indices to measure patella height. For example, Aglietti et al.35 reported greater patella height in chondromalacia patella subjects compared to pain free subjects using the Insall-Salvati index. Using the same index, Kannus2 reported greater patella height in the affected knee of subjects diagnosed with unilateral PF pain compared to their asymptomatic knee. In contrast, Laprade and Culham36 reported that there were no differences in patella height between the PF pain and pain free groups using the Caton-Deschamps index; their conclusion was consistent with the findings of Marks and Bentley37 and Haim et al.38 Our study demonstrates greater patella height in PF pain subjects compared to pain free subjects using the four most established indices (Figure 7). A possible explanation for this consistency between the four indices in our study is that we measured patella height under upright, weightbearing conditions. It is plausible that differences in patella height between the PF pain and pain free groups are accentuated under upright, weightbearing conditions. Laprade and Culham36 evaluated patella height under supine, non-weightbearing conditions, and this may explain the minimal differences in patella height between the PF pain and pain free groups in their study. It is unclear if Marks and Bentley37 and Haim et al.38 evaluated patella height under weightbearing or non-weightbearing conditions.
Results from this study suggest that patella alta affects both patellar tilt and bisect offset. Six out of 12 PF pain subjects categorized with patella alta using the Caton-Deschamps index had both abnormal patellar tilt and abnormal bisect offset, while two subjects had only abnormal patellar tilt. Average patellar tilt was greater in PF pain subjects with patella alta compared to PF pain subjects with normal patella height categorized using the Caton-Deschamps (p = 0.002) and the Insall-Salvati (p = 0.048) indices. Difference in average bisect offset between PF pain subjects with patella alta and PF pain subjects with normal patella height categorized using the Caton-Deschamps index trended towards significance (p = 0.058).
A limitation of this study is that our patella alta and patellar maltracking thresholds are based on data from PF pain and pain free subjects combined. One could argue that these thresholds should be based on pain free subjects, or based on a large, randomly selected population. Access to pain free subjects or a random population, however, is difficult in clinical settings where only symptomatic patients are evaluated; this difficulty is highlighted by the recruitment of predominantly symptomatic patients to determine patella alta thresholds.27-29,39 In the absence of a large data set on pain free subjects or a random population, there remains a gap in understanding the normal range of patella height and patella tracking. A second potential limitation is our definition of the 75th percentile of a distribution model as the patella alta threshold. Previous studies have defined patella alta thresholds based on 95th to 99th percentiles of population distribution.27-30 In our study, using the 95th to 99th percentile thresholds resulted in only 3%-5% (1-2 out of 37) of PF pain subjects categorized with patella alta. The reported prevalence of patella alta, however, ranges from 24%-39%40-42 in the symptomatic PF joint. The 75th percentile threshold yielded 27%-35% (10-13 out of 37) of PF pain subjects with patella alta (S-Table 3). Small changes in our 75th percentile thresholds (e.g., ± 5 percentile) did not change the conclusions reported in this study. Furthermore, our results are based on 52 subjects (37 PF pain, 15 pain free), with 10-13 PF pain subjects categorized with patella alta (S-Table 3), and 12 PF pain subjects classified as maltrackers. A study with a larger number of PF pain and pain free subjects may help test the generality of our findings. Addition of more subjects will likely strengthen the results presented in this study.
This study adds to our understanding of PF pain in two ways - 1) it is currently unknown if PF pain subjects with patella alta are predisposed to patellar maltracking. Our study shows that patellar maltracking is more prevalent in PF pain subjects with patella alta compared to subjects with normal patella height; and 2) it is unclear based on previous studies if PF pain subjects have greater patella height compared to pain free subjects, and it is difficult to compare directly the findings of the previous studies, in part, because the studies used different indices to measure patella height. Our study demonstrates greater patella height in PF pain subjects compared to pain free subjects using four indices commonly used in clinics.
Clinical evaluation of PF pain subjects should include measurement of patellar tracking and patella height under weightbearing conditions prior to selection of a treatment pathway. A subject accurately diagnosed as a maltracker will more likely benefit from a treatment targeting patellar maltracking, such as vastus medialis retraining43 or EMG biofeedback,44 compared to a subject accurately diagnosed as a normal tracker.
Supplementary Material
Acknowledgments
We thank Christine Draper for help with data collection. We thank Jarrett Rosenberg for help with statistical methods. Financial support provided by NIH (EB005790-05) and the Office of Research and Development (Rehabilitation R&D Service grant #A2592R), Veterans Affairs.
References
- 1.Devereaux MD, Lachmann SM. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br J Sports Med. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kannus PA. Long patellar tendon: radiographic sign of patellofemoral pain syndrome-a prospective study. Radiology. 1992;185:859–863. doi: 10.1148/radiology.185.3.1438776. [DOI] [PubMed] [Google Scholar]
- 3.Kujala UM, Osterman K, Kvist M, et al. Factors predisposing to patellar chondropathy and patellar apicitis in athletes. Int Orthop. 1986;10:195–200. doi: 10.1007/BF00266208. [DOI] [PubMed] [Google Scholar]
- 4.Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90:2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 5.Elias JJ, Cech JA, Weinstein DM, Cosgrea AJ. Reducing the lateral force acting on the patella does not consistently decrease patellofemoral pressures. Am J Sports Med. 2004;32:1202–1208. doi: 10.1177/0363546503262167. [DOI] [PubMed] [Google Scholar]
- 6.Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715–724. [PubMed] [Google Scholar]
- 7.Kramer PG. Patella malalignment syndrome: rationale to reduce excessive lateral pressure. J Orthop Sports Phys Ther. 1986;8:301–309. doi: 10.2519/jospt.1986.8.6.301. [DOI] [PubMed] [Google Scholar]
- 8.Grabiner MD, Koh TJ, Draganich LF. Neuromechanics of the patellofemoral joint. Med Sci Sports Exerc. 1994;26:10–21. [PubMed] [Google Scholar]
- 9.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 10.Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weightbearing. J Bone Joint Surg. 2007;89:1749–1755. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- 11.Phillips CL, Silver DA, Schranz PJ, Mandalia V. The measurement of patellar height: a review of the methods of imaging. J Bone Joint Surg Br. 2010;92:1045–1053. doi: 10.1302/0301-620X.92B8.23794. [DOI] [PubMed] [Google Scholar]
- 12.Davies AP, Costa ML, Donnell ST, et al. The sulcus angle and malalignment of the extensor mechanism of the knee. J Bone Joint Surg Br. 2000;82B:1162–1166. doi: 10.1302/0301-620x.82b8.10833. [DOI] [PubMed] [Google Scholar]
- 13.Moller BN, Krebs B, Jurik AG. Patellar height and patellofemoral congruence. Arch Orthop Trauma Surg. 1986;104:380–381. doi: 10.1007/BF00454436. [DOI] [PubMed] [Google Scholar]
- 14.Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res. 1972;88:67–69. doi: 10.1097/00003086-197210000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Baldini A, Anderson JA, Cerulli-Mariani P, et al. Patellofemoral evaluation after total knee arthroplasty. Validation of a new weight-bearing axial radiographic view. J Bone Joint Surg Am. 2007;89:1810–1817. doi: 10.2106/JBJS.E.00432. [DOI] [PubMed] [Google Scholar]
- 16.Boegard T, Jonsson K. Radiography in osteoarthritis of the knee. Skeletal Radiol. 1999;28:605–615. doi: 10.1007/s002560050561. [DOI] [PubMed] [Google Scholar]
- 17.Gold GE, Besier TF, Draper CE, et al. Weight-bearing MRI of patellofemoral joint cartilage contact area. J Magn Reson Imaging. 2004;20:526–530. doi: 10.1002/jmri.20146. [DOI] [PubMed] [Google Scholar]
- 18.McWalter EJ, Hunter DJ, Harvey WF, et al. The effect of a patellar brace on three-dimensional patellar kinematics in patients with lateral patellofemoral osteoarthritis. Osteoarthritis Cartilage. 2011;19:801–808. doi: 10.1016/j.joca.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Draper CE, Besier TF, Fredericson M, et al. Differences in patellofemoral kinematics between weight-bearing and non-weight-bearing conditions in patients with patellofemoral pain. J Orthop Res. 2011;29:312–317. doi: 10.1002/jor.21253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pal S, Draper CE, Fredericson M, et al. Patellar maltracking correlates with vastus medialis activation delay in patellofemoral pain patients. Am J Sports Med. 2011;39:590–598. doi: 10.1177/0363546510384233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pal S, Besier TF, Draper CE, et al. Patellar tilt correlates with vastus lateralis: Vastus medialis activation ratio in maltracking patellofemoral pain patients. J Orthop Res. 2012;30:927–933. doi: 10.1002/jor.22008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brechter JH, Powers CM. Patellofemoral joint stress during stair ascent and descent in persons with and without patellofemoral pain. Gait Posture. 2002;16:115–123. doi: 10.1016/s0966-6362(02)00090-5. [DOI] [PubMed] [Google Scholar]
- 23.Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 24.Caton J, Deschamps G, Chambat P, et al. Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68:317–325. [PubMed] [Google Scholar]
- 25.Caton J. Method of measuring the height of the patella. Acta Orthop Bel. 1989;55:385–386. [PubMed] [Google Scholar]
- 26.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 27.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 28.Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992:170–176. [PubMed] [Google Scholar]
- 29.Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707–712. doi: 10.1007/s00167-005-0015-4. [DOI] [PubMed] [Google Scholar]
- 30.Ali SA, Helmer R, Terk MR. Patella alta: lack of correlation between patellotrochlear cartilage congruence and commonly used patellar height ratios. AJR Am J Roentgenol. 2009;193:1361–1366. doi: 10.2214/AJR.09.2729. [DOI] [PubMed] [Google Scholar]
- 31.Anagnostakos K, Lorbach O, Reiter S, Kohn D. Comparison of five patellar height measurement methods in 90 degrees knee flexion. Int Orthop. 2011;35:1791–1797. doi: 10.1007/s00264-011-1236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin LI. A Concordance Correlation-Coefficient to Evaluate Reproducibility. Biometrics. 1989;45:255–268. [PubMed] [Google Scholar]
- 33.Partik BL, Stadler A, Schamp S, et al. 3D versus 2D ultrasound: accuracy of volume measurement in human cadaver kidneys. Invest Radiol. 2002;37:489–495. doi: 10.1097/01.RLI.0000023573.59066.43. [DOI] [PubMed] [Google Scholar]
- 34.Glantz SA. Primer of Biostatistics. Fifth Edition. McGraw-Hill; 2002. [Google Scholar]
- 35.Aglietti P, Insall JN, Cerulli G. Patellar pain and incongruence. I: Measurements of incongruence. Clin Orthop Relat Res. 1983:217–224. [PubMed] [Google Scholar]
- 36.Laprade J, Culham E. Radiographic measures in subjects who are asymptomatic and subjects with patellofemoral pain syndrome. Clin Orthop Relat Res. 2003:172–182. doi: 10.1097/01.blo.0000079269.91782.f5. [DOI] [PubMed] [Google Scholar]
- 37.Marks KE, Bentley G. Patella alta and chondromalacia. J Bone Joint Surg Br. 1978;60:71–73. doi: 10.1302/0301-620X.60B1.627582. [DOI] [PubMed] [Google Scholar]
- 38.Haim A, Yaniv M, Dekel S, Amir H. Patellofemoral pain syndrome: validity of clinical and radiological features. Clin Orthop Relat Res. 2006;451:223–228. doi: 10.1097/01.blo.0000229284.45485.6c. [DOI] [PubMed] [Google Scholar]
- 39.Shabshin N, Schweitzer ME, Morrison WB, Parker L. MRI criteria for patella alta and baja. Skeletal Radiol. 2004;33:445–450. doi: 10.1007/s00256-004-0794-6. [DOI] [PubMed] [Google Scholar]
- 40.Stefanik JJ, Zhu Y, Zumwalt AC, et al. Association between patella alta and the prevalence and worsening of structural features of patellofemoral joint osteoarthritis: the multicenter osteoarthritis study. Arthritis Care Res (Hoboken) 2010;62:1258–1265. doi: 10.1002/acr.20214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 42.Jibri Z, Martin D, Mansour R, Kamath S. The association of infrapatellar fat pad oedema with patellar maltracking: a case-control study. Skeletal Radiol. 2012 doi: 10.1007/s00256-011-1299-8. [DOI] [PubMed] [Google Scholar]
- 43.Bennell K, Duncan M, Cowan S, et al. Effects of vastus medialis oblique retraining versus general quadriceps strengthening on vasti onset. Med Sci Sports Exerc. 2010;42:856–864. doi: 10.1249/MSS.0b013e3181c12771. [DOI] [PubMed] [Google Scholar]
- 44.Ng GY, Zhang AQ, Li CK. Biofeedback exercise improved the EMG activity ratio of the medial and lateral vasti muscles in subjects with patellofemoral pain syndrome. J Electromyogr Kinesiol. 2008;18:128–133. doi: 10.1016/j.jelekin.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 45.Miller TT, Staron RB, Feldman F. Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol. 1996;167:339–341. doi: 10.2214/ajr.167.2.8686598. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


