Abstract
Background
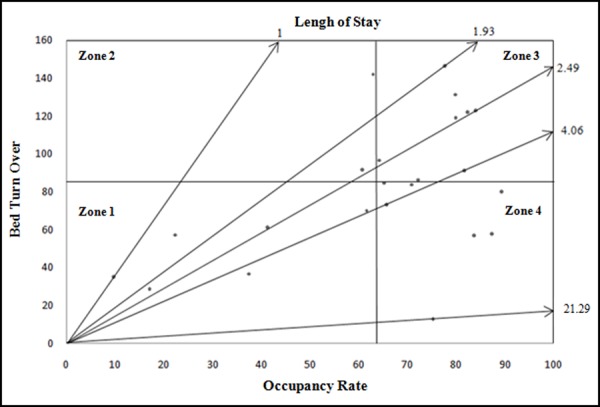
One of the most important and useful models for assessing hospital performance is the Pabon Lasso Model, a graphical model that determines the relative performance of hospitals using three indicators: 1. Bed Occupancy Rate (BOR); 2. Bed Turnover (BTO); 3) Average Length of Stay (ALS). The aim of this research is to investigate the performance of the hospitals affiliated with Urmia University of Medical Sciences in Iran during the year 2009 based on the Pabon Lasso Model.
Method
This cross-sectional descriptive study was undertaken in 2009. All the 23 hospitals affiliated with Urmia University of Medical Sciences were included. To ensure accuracy and reliability of data, the required data on BOR, BTO, and the ALS were accumulated by referring to the Statistical Year Book of the Urmia University of Medical Sciences. Data analysis was performed using the Pabon Lasso Model and SPSS 16 statistical software.
Results
Across all hospitals, the following average results for each performance indicator were obtained: ALS = 2.84 days, BOR = 63.55% and BTO = 85.44 times per year. Six hospitals were located in the Pabon Lasso Model zone 1, two hospitals in zone 2, eight hospitals in zone 3, and seven hospitals in zone 4 of the model.
Conclusion
The study showed that 60.87% of the studied hospitals had low performance in terms of either BOR or BTO, or both. Thus, the analysis on why that low performance may have occurred, and suggestions to enhance future performance, is provided.
Keywords: Performance assessment, key performance indicators, hospital, Pabon Lasso Model, Iran
Background
Despite conspicuous and undeniable scientific and technological progress, healthcare systems worldwide still face numerous challenges1. Factors such as inefficiencies and failure to meet patients' expectations continually threaten healthcare systems2. Hospitals play a key role in providing healthcare services and can positively impact the efficiency of these systems3-4. Hospitals in developed and developing countries account for 40% and 80% of the healthcare sector costs respectively. Thus, the impact of evaluating performance of hospitals and changing systems as a result could be particularly significant5.
Performance evaluation is an effective technique used by hospital management to assess and supervise hospital activities; nevertheless, it has been relatively neglected in previous research of healthcare productivity6.
Numerous methods have been presented for use in evaluating the performance of hospitals and how to analyse the results obtained from such evaluations7. An important and useful model for the evaluation of hospital performance is the Pabon Lasso Model. This graphical model was introduced in 1986 by Pabon Lasso for use in determining the relative performance of the hospitals. It uses three indicators to evaluate the overall performance of a hospital, namely: BOR, BTO and ALS8. Interpretation of performance using this model is based on a chart which is divided into four parts by two crossing lines: the longitudinal axis (x) shows the mean for BOR and the transverse axis (y) shows the BTO. Each hospital assigns itself special features by being positioned in one of the four parts (zones) of the chart (see Table 1). By identifying and analysing to which zone a hospital belongs, the management team can make a more logical and relevant assessment of how to best improve the performance9.
Table 1: Description and interpretation of each of the zones of the Pabon Lasso Model10-12.
| Zone | Definition | Interpretation |
| 1 | Low BTOs and low BORs | The number of beds is high relative to the current demand, the hospital demonstrates poor performance |
| 2 | Low BOR but high BTO rate (common among obstetric and gynaecology hospitals) | Indicates multiple patients requiring short-term hospitalisation. There is potential for unnecessary hospitalisation and surplus bed capacity among these hospitals |
| 3 | High BOR and high BTOs | These hospitals have reached an appropriate efficiency with the minimum number of beds used |
| 4 | High BORs and low BTOs (common among psychiatric and elderly medicine) | Indicates long-term hospitalisation of the patients, perhaps under-using other outpatient facilities and incurring high costs |
Although not all the features associated with each zone of the Pabon Lasso Model may be applicable to every hospital, this kind of analysis is useful for quick identification of the hospitals with weak performance and highlighting areas to direct rectification of their inefficiencies. However, a limitation of the Pabon Lasso Model is that performance indicators may be affected by a number of factors that cannot be measured using this simplistic instrument, such as access to communication facilities, lack of availability of home- or community-care, geographic location, teaching hospital status, the number of employees and hospitalpolicies11-12.
This study will evaluate the performance of the hospitals affiliated with the Urmia University of Medical Sciences using the Pabon Lasso Model. The subsequent aim was to inform policy makers during the compilation of plans for increasing the productivity of the hospitals by determining strategies for effective utilisation of the existing resources.
Method
This cross-sectional descriptive study was undertaken in 2009 in the West Azerbayjan province. This province is located in North-West Iran and has 17 townships, with Urmia Township at its centre. All 23 hospitals affiliated with the Urmia University of Medical Sciences were included in this research.
To ensure accurate and reliable data collection, the general data (including the number of active beds, number of active bed-days, number of occupied bed-days and number of discharges) and performance data (including BOR, BTO, and ALS) were accumulated from the statistical almanac of the Urmia University of Medical Sciences, issued quarterly by the statistics and information centre. Using descriptive statistics, the annual status of the mentioned indicators was determined. The data was then analysed using the Pabon Lasso Model and SPSS 16 Statistical Software.
Results
All the hospitals were public except for one, which was a specialist psychiatry hospital and belonged to a governmental sector. Four hospitals were teaching hospitals. The overall number of the active beds, active bed-days, occupied bed-days and the number of discharges were 2,659, 970,535, 722,901 and 220,690 respectively. Based on the results, in all of the studied hospitals (except for the psychiatric hospital), the following average values were recorded: ALS: 2.84 days, BOR: 63.55%, BTO: 85.44 times/year. The reason for excluding data from the above mentioned psychiatric hospital was because of the particularly lengthy admissions in that hospital which could significantly skew the results. Six hospitals (no. 8, 11, 12, 14, 20, 23) were located in zone one of the model, indicating inefficiency in the use of the resources available to them, as they tended to have low BTOs and BORs. There were eight hospitals in zone three, which represents high levels of efficiency. Finally two hospitals (no. 17, 22) and seven hospitals (no. 1, 2, 3, 4, 7, 9, 21) belonged to zones 2 and 4 respectively (see Table 2 & Chart 1).
Table 2. Frequency distribution of different indicators for the studied hospitals.
| Hospital No. | Active beds | Active bed-days | Occupied bed-days | Discharges | ALS | BOR | BTO |
| 1 | 448 | 163520 | 142916 | 25938 | 5.51 | 87.40 | 57.91 |
| 2 | 232 | 84680 | 60038 | 19493 | 3.08 | 70.90 | 83.93 |
| 3 | 200 | 73000 | 61138 | 11428 | 5.35 | 83.75 | 57.17 |
| 4 | 93 | 33945 | 25567 | 1201 | 21.29 | 75.32 | 12.91 |
| 5 | 164 | 59860 | 38472 | 15898 | 2.42 | 64.27 | 96.86 |
| 6 | 209 | 76285 | 61020 | 25008 | 2.44 | 79.99 | 119.42 |
| 7 | 75 | 27375 | 24471 | 6027 | 4.06 | 89.39 | 80.34 |
| 8 | 30 | 10950 | 4105 | 1107 | 3.71 | 37.49 | 36.83 |
| 9 | 70 | 25550 | 16799 | 5137 | 3.27 | 65.75 | 73.47 |
| 10 | 50 | 18250 | 14184 | 7349 | 1.93 | 77.72 | 146.87 |
| 11 | 10 | 3650 | 354 | 354 | 1.00 | 9.70 | 35.40 |
| 12 | 23 | 8395 | 1439 | 660 | 2.18 | 17.14 | 28.71 |
| 13 | 237 | 86505 | 62465 | 20480 | 3.05 | 72.21 | 86.48 |
| 14 | 107 | 39055 | 24085 | 7503 | 3.21 | 61.67 | 70.21 |
| 15 | 131 | 47815 | 39079 | 11951 | 3.27 | 81.73 | 91.32 |
| 16 | 125 | 45625 | 37609 | 15288 | 2.46 | 82.43 | 122.21 |
| 17 | 71 | 25915 | 15751 | 6536 | 2.41 | 60.78 | 91.91 |
| 18 | 56 | 20440 | 16325 | 7387 | 2.21 | 79.87 | 131.63 |
| 19 | 125 | 45625 | 38343 | 15399 | 2.49 | 84.04 | 123.12 |
| 20 | 68 | 24820 | 10253 | 4168 | 2.46 | 41.31 | 61.37 |
| 21 | 86 | 31390 | 20479 | 7288 | 2.81 | 65.24 | 84.81 |
| 22 | 27 | 9855 | 6208 | 3832 | 1.62 | 62.99 | 142.34 |
| 23 | 22 | 8030 | 1800 | 1258 | 1.43 | 22.41 | 57.31 |
Chart 1. The status of the studied hospitals based on the Pabon Lasso Model.
Discussion
Many indicators exist in the literature for measuring hospital performance. It is important to apply those measures to monitor the performance of a hospital, as it will result in a number of benefits, such as indicating important organisational goals for the policy makers, directing planning of future services, and management of available resources.
Using a single performance indicator may result in incorrect and/or misleading conclusions about the overall performance of a hospital. For instance, high BOR can result from either high ALS due to the efficient use of hospital resources for needy patients, or the existence of unnecessary hospitalisations resulting in inefficient use of resources. Nonetheless, only few studies have investigated the use of multiple indicators to evaluate the hospital sector. This study has applied the Pabon Lasso Model which provided us with a quick evaluation about the overall performance of the hospital by charting three indicators (BOR, BTO, ALS). Besides, by using graphical charts, the relationship between multiple performance indicators were identified better and could facilitated the analysis process.
Obviously many differences exist in the performance of the multiple studied hospitals; however a better understanding about such differences must be based on objective evidences. Overall, the average values for each of the three performance indicators of the studied hospitals were BOR 63.55%, ALS 2.84 days, and BTO 85.44/year.
As highlighted earlier, in our study we found that six hospitals (26.10%) lay in zone 1, two hospitals (4.34%) in zone 2, eight hospitals (39.13%) in zone 3 and seven hospitals (30.43%) in zone 4 of the Pabon Lasso Model. These results are in line with previous studies that showed a relatively low performance of hospitals in Iran. For instance, in 2000, Shahrestani undertook a study to evaluate the performance of the country hospitals and found out that 14 provinces lay in zone 1, 10 provinces in zone 2, and only one province lay in zone 3 of the Pabon Lasso Model. In the same study, the average of the BOR, BTO and ALS indicators for the West Azerbayjan province were recorded as 43.05%, 28 times/year, 6.87 days respectively. These statistics place the province generally in zone 1 of the Pabon Lasso Model, indicating a low overall performance for the province11. A close comparison between the present study's results with Shahrestani's study indicates that improvement of the performance indicators under study has occurred over the nine-year time span between the two studies. This improvement may due to a change in age distribution and prevalent diseases and, perhaps due to different data collection and analysis methods.
In Goshtasbi's study of performance evaluation of the hospitals existing in the Kohgilouyeh-Bouyer-Ahmad province based on the Pabon Lasso Model, from a total of six hospitals under investigation, two hospitals lay in zone 3, three lay in zone 1 and one hospital lay in zone 410 In another study, Sajjadi evaluated the performance of the hospitals affiliated with the Isfahan University of Medical Sciences based on the Pabon Lasso Model and showed that from a total of 31 hospitals under study, two cases lay in zone 1, 14 cases lay in zone 2, 13 hospitals lay in zone three, and 2 cases located in zone 4 of the Pabon Lasso Model chart13.
Considering the results, the suitable strategy for the hospitals located in zone 1 of the Pabon Lasso Model is to focus on their weak points so that they can improve upon these. Therefore, they need to identify and rectify the factors that caused low BTOs and low BORs, and eventually pushed the hospital to fall under zone 1. Regarding the hospitals located in the zone 4, the suitable strategy will be directing the tendency towards providing the bedridden patients with diagnostic-therapeutic services partly as outpatients, thereby overcoming the shortcomings and improving the BTO.
As for the hospitals located in zone 2, with a low BOR, there seems to be unnecessary hospitalisation and surplus bed capacity. Hence, it is suggested that suitable measures are taken for rationalising the hospitalisation in a more efficient manner. Finally, for the hospitals under zone 3 of the model, they should follow their strategy to ensure having a consistently efficient service provision with an optimised number of beds used.
Conclusion
The current study has looked into 23 hospitals in Iran and evaluated their performance through the Pabon Lasso Model. The results showed that while some of the studied hospitals (39.13%) had significantly good performance indicators (both high BOR and high BTO), the rest of the hospitals had a poor performance in one or more of the performance indicators. The authors have discussed the results and proposed some suggestions on how to improve the performance of these hospitals.
Based on the indicators from the Pabon Lasso Model, the areas of improvement for each hospital could be identified. These weak areas would then need to be enhanced, by modifying the current policies and strategies, as well as applying necessary changes, in order to lead the hospital towards performing at its maximum performance capacity. Future research should try to explore the factors that have caused the low efficiency of these hospitals and propose more practical way to overcome them.
Footnotes
PEER REVIEW
Not commissioned, externally peer reviewed
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
Please cite this paper as: Bahadori M, Sadeghifar J, Hamoudzadeh P, Hakimzadeh M, Nejati M. Combining Multiple Indicators to Assess Hospital Performance in Iran using the Pabon Lasso Model. AMJ 2011, 4, 4, 175-179 http//dx.doi.org/10.4066/AMJ.2011.620
References
- 1.Groene O, Garcia-Barbero M.. Health promotion in hospitals: evidence and quality management. Citeseer. 2005:1–120. [Google Scholar]
- 2.Jakab M, Harding A, Preker A, Hawkins L. Organizational reform and management of public providers: focus on hospitals: common performance problems in public hospitals and their causes. Washington D.C.: World Bank; 2000. [Google Scholar]
- 3.Barnum H, Kutzin J. Public Hospitals in Developing Countries: Resource Use, Cost, Financing. Baltimore, Maryland: John Hopkins University Press; 1993. pp. 1–335. [Google Scholar]
- 4.Ersoy K, Kavuncubasi S, Ozcan YA, Harris JM.. Technical efficiencies of Turkish hospitals: DEA approach. J Med Sys. 1997;21(2):67–74. doi: 10.1023/a:1022801222540. [DOI] [PubMed] [Google Scholar]
- 5.Aversion A. Tehran: Islamic Azad University, Science and Research Branch; 2002. Comparative study of evaluation and supervision mechanism of services delivery in public and private hospitals of Tehran. [Google Scholar]
- 6.Farzianpour M, Rangraz Jeddi F, Mousavi G.. How often do the managers use the statistics for hospital management? Feyz Journal. 2003;27:92–98. [Google Scholar]
- 7.Mehrotra A, Lee S, Dudley R. Washington D.C: National Business Coalitions on Health; 2006. Hospital performance evaluation: what date do we want, how do we get it, and how should we use it? [Google Scholar]
- 8.Lasso P.. Evaluating hospital performance through simultaneous application of several indicators. Bulletin of the Pan American Health Organization. 1986;20(4):341–57. [PubMed] [Google Scholar]
- 9.Asefzadeh S. Ghazvin: Qazvin University of Medical Sciences; 2007. Hospital Management & Research. [Google Scholar]
- 10.Goshtasebi A, Vahdaninia M, Gorgipour R, Samanpour A, Maftoon F, Farzadi F. et al. Assessing Hospital Performance by the Pabon Lasso Model. Iranian Journal of Public Health. 2009;38(2):119–124. [Google Scholar]
- 11.Shahrestani T. Tehran: Iran University of Medical Sciences; 2000. Using three major indicators (bed occupancy rate, Bed Turnover, and average length of stay) to assess the performance of Iranian hospitals in a Pabon Lasso model. [MSc Dissertation] [Google Scholar]
- 12.Thomas S, Normand C, Smith S.. Social health insurance: further options for Ireland. Report prepared by TCD and published by the Adelaide Hospital Society. 2008:1–48. [Google Scholar]
- 13.Sajadi H, Hariri M, Sajadi Z. Tehran: Health Economics Research Centre; 2007. Assessment performance of hospitals affiliated to the Isfahan University of Medical Sciences according to Pabon Lasso model in 2007. [Google Scholar]


