Abstract
Asthma is one of the most common chronic conditions affecting the Australian population. Amongst primary healthcare professionals, pharmacists are the most accessible and this places pharmacists in an excellent position to play a role in the management of asthma. Globally, trials of many community pharmacy-based asthma care models have provided evidence that pharmacist delivered interventions can improve clinical, humanistic and economic outcomes for asthma patients. In Australia, a decade of coordinated research efforts, in various aspects of asthma care, has culminated in the implementation trial of the Pharmacy Asthma Management Service (PAMS), a comprehensive disease management model.
There has been research investigating asthma medication adherence through data mining, ways in which usual asthma care can be improved. Our research has focused on self-management education, inhaler technique interventions, spirometry trials, interprofessional models of care, and regional trials addressing the particular needs of rural communities. We have determined that inhaler technique education is a necessity and should be repeated if correct technique is to be maintained. We have identified this effectiveness of health promotion and health education, conducted within and outside the confines of the pharmacy, in public for a and settings such as schools, and established that this outreach role is particularly well received and increases the opportunity for people with asthma to engage in their asthma management.
Our research has identified that asthma patients have needs which pharmacists delivering specialized models of care, can address. There is a lot of evidence for the effectiveness of asthma care by pharmacists, the future must involve integration of this role into primary care.
Keywords: Asthma, community pharmacy, pharmacists’disease state management, self-management, health promotion, inhaler technique
Introduction
A high population prevalence of asthma (10.2%) in Australia underpins its listing as a national health priority area1.Despite significant national efforts to improve asthma management, several areas remain of concern. These include inappropriate medication use, lack of self-management skills and lack of access to timely and comprehensive care.
There are high costs associated with the use of asthma services (GP visits, hospitalisation, and medications). In 2004–05, it was estimated that of the $606 million asthma related expenditure, half was attributable to medications1. Moreover, inappropriate medication use persists, with common overuse of relievers and underuse/overuse of preventers. In the National Health Survey of 2004–05, among people with current asthma aged five years and over, 18.5% reported having used inhaled corticosteroids in the previous two weeks1.In the subgroup who reported using short-acting beta-agonists in the previous two weeks, indicating that they were likely to have experienced symptoms of asthma during that time, only 28% had also used inhaled corticosteroids during this period. Hence, there is evidence that use of inhaled corticosteroids for control of symptomatic asthma is sub-optimal in the community1. Since its introduction, use of combination therapy of inhaled corticosteroids and long acting β agonists has been increasing, however, the percentage of users does not match the prevalence of people with moderate-severe persistent asthma, indicating possible overuse and lack of ‘step-down’ or titration of corticosteroid dose1. Another issue associated with medication use is thatintermittent use of inhaled corticosteroids is the most common mode of use in adults and children, despite treatment guidelines recommending regular use in people with persistent asthma.
As well as medication issues, the low rates of provision of self-management plans or action plans suggest that self-management skills are infrequently being taught to patients, notwithstanding the emphasis placed on self-management as a critical component of asthma management in national guidelines. Rural and regional areas in Australia have an undersupply of healthcare professionals with long waiting times for a GP or specialist consultation and limited lung function testing laboratories. Lastly, continued exposure to known triggers such as smoking is a problem; in 2004–05 the prevalence of smoking at least once a week in people aged 18 years and over was 24.5% among those with current asthma and 22.3% among those without current asthma1.
Most, if not all such issues can be addressed at the primary healthcare level through patient education and specific interventions. There are approximately 5000 pharmacies in Australia; they serve as accessible and convenient venues for patients to receive primary healthcare advice. Patients with asthma possibly visit community pharmacies more regularly than their GPs to seek medicines, for example to obtain reliever medicines such as salbutamol or terbutaline inhalers which do not require a prescription, or to obtain repeat prescription medications. Often preventer medications are prescribed with five repeats (one original supply and five repeats), which means that ordinarily it may be at least six months between doctor consultations for a patient, unless there is an exacerbation requiring a doctor or hospital visit. Optimal asthma management centres around appropriate use of medications and therefore the pharmacist with their therapeutic expertise can play a pivotal role in assisting patients with their asthma.
Pharmacist led asthma care models in Australia
In recognition of this, researchers and pharmacy practitioners have actively trialled several different models of the delivery of asthma-related healthcare using pharmacist interventions. Models of care trialled have ranged from focused interventions around a key area of asthma management to comprehensive disease state management interventions where high cost poorly controlled patients are targeted and a suite of interventions are delivered by trained pharmacists. In addition to intervention models, pharmacists have been involved in outreach programs with a health education/health promotion focus. Some asthma health promotion models have also been trialled with a specific population focus for example, a rural/regional focus. A majority of this work has been carried out by a research team based at the Faculty of Pharmacy, University of Sydney.
Focussed Interventions
1. Inhaler technique
Despite its importance, inhaler technique review by primary healthcare professionals is not common2,3. To address this, a team of researchers at the Faculty of Pharmacy, University of Sydney, Australia has been working on developing intervention models to assist pharmacists in fulfilling this important role. In an initial trial of optimising dry powder inhaler (Turbuhaler) technique in patients, a small group of 26 asthma patients, recruited through community pharmacies in Sydney, NSW were allocated to one of three groups: standard verbal counselling, verbal counselling with an emphasis on Turbuhaler priming position, and verbal counselling augmented with physical demonstration of technique4. Patient technique was scored prior to and two weeks after counselling on a score of nine using a standard checklist for correct technique. The mean scores at baseline showed that most patients could not achieve even a single correct step. After the intervention, the proportion with technique improvement was significantly different between groups i.e. 0% (n=7, standard verbal), 25%(n=8, verbal counselling with emphasis on priming position) and 77% (n=9, verbal counselling augmented by a physical demonstration by the pharmacist). This study highlighted that physical demonstration appears to be an important component of effective Turbuhaler training for patient education and achieving optimal Turbuhaler technique4. This was an important finding as most inhaler technique review usually involves verbal counselling alone by the healthcare professional, which did not achieve any improvement in technique.
Using these findings the researchers then conducted a randomised controlled trial with 53 intervention and 44 control asthma patients recruited through community pharmacies in metropolitan Sydney (NSW, Australia)5. The intervention pharmacists used the technique of verbal counselling augmented with a physical demonstration of correct technique using a placebo inhaler whereas control pharmacists provided usual care. Patient data were collected at baseline and one, two three plus six months post baseline. Both the Accuhaler (Diskus) and Turbuhaler devices were the focus in this study5. Compared with the control group, a significantly higher proportion of Turbuhaler (50% vs. 14%) and Accuhaler (79% vs. 14%) users in the intervention group were able to demonstrate correct technique after six months5. Whilst these findings validated the initial study, interestingly the upward trend in technique scores was maintained until three months with monthly reinforcement and although still improved compared to baseline, there were was a downward trend in scores between three and six months when there was no monthly reinforcement7. Importantly this study also indicated that besides improvements in inhaler technique in the intervention patients, there were synchronous improvements in asthma related quality of life, perception of control over asthma and decreased variability in peak expiratory flow6. Another strategy tested within the above trial was the use of correct inhaler use checklists on a personalised label for a patient. Pharmacists in the active group used these innovative labels to deliver personalised education to patients. The results suggested that inhaler technique education needs to be repeated at regular intervals for patients and that personalised reminders such as sticky labels on an inhaler device may be useful counselling aids6. The utility of the physical demonstration of inhaler technique along with verbal counselling and the need for reinforcing technique was also shown in a later study by the same group7.
It is known that many healthcare professionals themselves may not have optimal inhaler technique. In the study described above6, pharmacists who had delivered the intervention, had their own technique tested prior to receiving any education from the research team, after the education and two years later. At the initial assessment, few pharmacists demonstrated correct technique (Turbuhaler: 13%, Accuhaler: 6%). All pharmacists in the active group demonstrated correct technique following training. Two years later, pharmacists in the active group demonstrated significantly better inhaler technique than pharmacists in the control group for both the Turbuhaler and Accuhaler devices (83% vs.11%; 75% vs.11%, respectively) suggesting that once correct technique is achieved it can be maintained by health professionals for a long period8.
Whilst inhaler technique education and review are only one area of focus for improving the management of asthma in primary healthcare, it is nonetheless a key area. As shown by the data from pharmacist models highlighted above, improved inhaler technique may be associated with better asthma outcomes4-6, 9. Another cross-sectional retrospective study of 176 Japanese adult asthma patients suggested that better adherence to medications in asthma may be associated with repeated instruction on inhaler techniques. The consequences of poor inhaler technique were highlighted by a retrospective study of 1677 adults with moderate-severe asthma in Singapore which found that poor inhaler technique is a predictor of emergency department visits10.Given these associations of improved outcomes with better inhaler technique, it is imperative that primary healthcare professionals devote some time to this. The average time taken by the most comprehensive intervention in the University of Sydney studies (verbal counselling augmented by a physical demonstration of the correct technique using a show and tell method) was 2.5 minutes5. Since community pharmacists are possibly the most frequently visited primary healthcare professional, and have a thorough understanding of formulation and usage principles for inhalation devices, intervention models developed by the University of Sydney team and cited above should be trialled at a national level. Denmark is an exemplar of this approach where community pharmacies are expected to and remunerated for applying their therapeutic expertise and training in patient consultations through education and regular re-inforcement of appropriate inhaler technique11. Inhaler instruction using checklists has also been shown to be effective in hospital settings when delivered by a hospital pharmacist12. Collectively, these studies highlight the important role of pharmacists in improving inhaler technique in patients – and different methods by which education can be effectively delivered.
2. Self-management
The Australian National Asthma Management Handbook suggests that all adults with asthma should be offered self-management education that involves a written action plan, self-monitoring and regular medical review. This approach can improve asthma control13. In people with asthma, the variable nature and sudden onset of symptoms of the condition necessitate self-management. Self-management is a complex concept to understand, perceptions of illness, personality type, confidence in healthcare and many other factors can affect it14-16. The skills required to self-manage can be provided through a variety of means such as education, motivation and through tools such as written self-management or action plans16. It has been suggested that whilst patient education merely provides technical skills and information, self-management training helps patients problem solve and troubleshoot17.
In asthma few published pharmacy models or interventions have focused on self-management. Led by a health psychologist, researchers at the University of Sydney developed one of the few self-management focused pharmacy intervention studies18.The asthma self-management model, based on a theoretical framework, was implemented in a community pharmacy setting in metropolitan Sydney, using a controlled, parallel-groups repeated-measures design. Twenty-one trained pharmacists recruited 91 (35 Intervention, 56 Control) patients with asthma and delivered a structured, step-wise, patient-focused self-management program over a nine-month period focusing on identification of asthma problems, goal setting and strategy development. Data on process, clinical and psychosocial outcome measures were gathered. Results showed that participants set an average of four new goals and six repeated goals over the course of the intervention. Most common goal-related themes included asthma triggers, asthma control and medications. An average of nine strategies per participant was developed to achieve the set goals. Common strategies involved visiting a medical practitioner for review of medications, improving adherence to medications and using medications before exercise. Clinical and psychosocial outcomes indicated significant improvements over time in asthma symptom control, asthma-related self-efficacy and quality of life, and negative affect.
These results suggest that an asthma self-management model of illness behaviour has the potential to provide patients with a range of process skills for self-management, and deliver improvements in clinical and psychosocial indicators of asthma control. The results also indicate the capacity for the effective delivery of such an intervention by pharmacists in Australian community pharmacy settings18. This is the only pharmacist led, theory based model focusing entirely on self-management in asthma that has been trialled. Other reported models such as the one reported by Barbanel and colleagues, in the UK have shown successful outcomes when self-management is delivered by the pharmacist, however the intervention mostly dealt with patient education about asthma, asthma triggers and avoidance, and basic self-management skills such as education about action to be taken in an emergency or self-monitoring using peak flows19. As discussed above, these approaches can improve technical skills but do not help patients troubleshoot and strategise their management. The novel model developed by Smith and colleagues (2007)18 was focused mainly on self-management, but elements of this model were later incorporated into more comprehensive disease state management programs.
3. Adherence /appropriate medication use profiles
In a proof of concept study Elliott and colleagues 200820 showed that by utilising a self-regulatory model, trained pharmacists can use a patient centered telephone advice line to help reduce medication related problems and non-adherence, at least short term, in patients initiating medication use for a chronic illness including asthma20,21. This study differs from interventions that focus on self-management, as the focus here was on improving adherence. Pharmacist (face-to-face or telephone-based) led interventions that focus exclusively on medication adherence have not yet been trialled in Australia. However a recent approach trailed in Tasmania, used data mining and prescription refill information to identify patients who were overusing short acting beta agonists or under-using inhaled corticosteroids. These patients were subsequently sent a letter encouraging them to see their GP. After these letters were sent to patients, there was an increase in the preventer to reliever ratio, suggesting that referral to and GP consultation by patients resulted in improved medication use in the intervention group as opposed to the control group22,23. Patients receiving letters from the pharmacy also had improved asthma control and quality of life at the end of six months22,23. In this case, bar the identification of medication using data mining software and the sending of an intervention pack to the patient prompting them to see their GP, no direct pharmacist interventions were delivered. Such trials should be undertaken nationally using robust research designs with adequate power to establish causality and uncover the sustainability of effects.
Since most pharmacists would find it relatively straightforward to implement such an approach, once the evidence for effects on asthma outcomes is widespread, can be sustained and cost savings calculated, this may be an excellent baseline approach. However, it does not take into account the therapeutic and health service expertise of the pharmacist, and their willingness to enact proactive roles in asthma management24. In a study in Quebec, Canada, inappropriate medication use identified through prescription records for patients with asthma was fed back to the patient’s physician as well as the pharmacist25. The study results indicated that feedback provided to physicians did not improve the appropriate use of asthma medication. However, feedback to pharmacists was promising, especially when including patients’ names so that pharmacists could intervene more specifically 25. There are noticeable lacunae in the research literature around the area of focused interventions for improving adherence in asthma patients. Models based purely on medication use profiles, such as the Mirixa program26, whilst valuable, are based on a simplistic view for improving a complex problem such as adherence. As highlighted above mere education and information can only improve technical skills, not long term self-management skills. Whereas evidence for focused interventions on adherence are lacking, improvements in adherence have been repeatedly demonstrated with more comprehensive pharmacist led models.
Comprehensive Models
Disease State Management Models
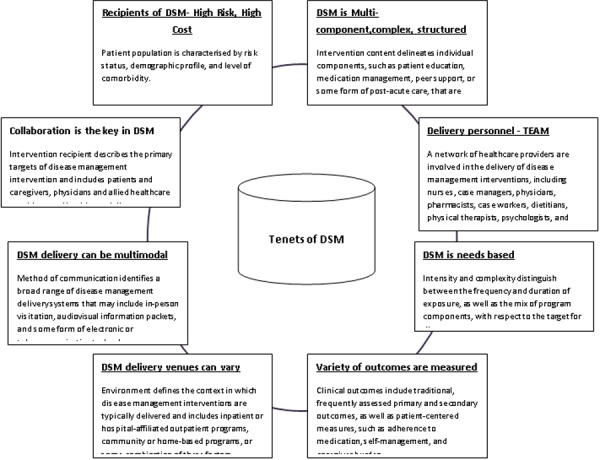
A relatively new approach to providing care to patients with chronic disease is disease state management (DSM). Previous patient care models were “compartmentalised” in the sense that practitioners focused solely on those aspects of patient care within their areas of expertise27. Unlike these previous models, DSM focuses on integrated patient care. Given the comprehensive nature of DSM, definitions abound. Ouwens and colleagues, for example defined it as “a systematic approach for co-coordinating healthcare interventions and communications at individual, organizational, regional or national level. Evidence suggests that planned proactive care can lead to a better quality of life and improved health outcomes for people with long-term conditions.”28. The American Heart Association Disease Management Taxonomy Writing Group recently proposed a taxonomy for defining DSM29. The key features of DSM based on this taxonomy are outlined in Figure 2.
Figure 1. Pharmacist/pharmacy based asthma service models trialled in Australia.
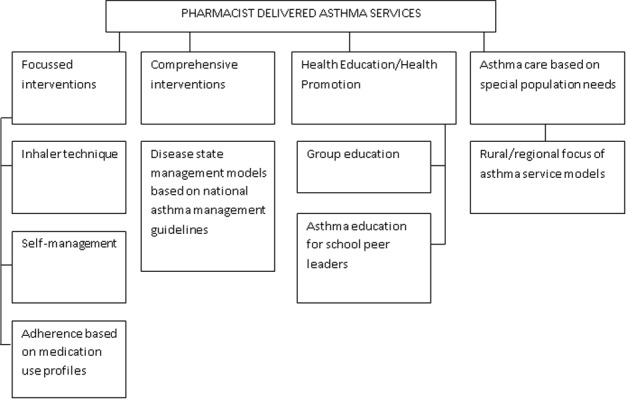
Figure 2. Basic tenets of DSM Source Modified from Krumholz and colleagues29.
The Pharmaceutical Society of Australia recently revised its standards of practice for pharmacists in which the concept (Standard 17) is defined thus: “DSM is a consumer-centred process that focuses on enabling consumers suffering from chronic conditions to participate in the management of their disease with the objective of reducing their disease-related risk factors.”30. The standard states that DSM can be achieved through monitoring, counselling, education, enhancement of self-management, and promotion of the quality use of medicines. The pharmacist must recognise the need for involvement in an ongoing cycle of care, assessment, intervention, monitoring/feedback, and assessment of consumer behaviour changes when providing DSM services. Similarly the role of pharmacists in DSM is encouraged through supportive legislation in several US states31.
In the late 1990s and the early part of the new century several pharmacy based comprehensive asthma programs were trialled globally32-37, however there were no pharmacist led disease state management based programs in Australia. A group of researchers at the Faculty of Pharmacy, University of Sydney along with a number of motivated pharmacists in the Illawarra and Blue mountain region of NSW pioneered the first pharmacy asthma DSM model. The model was developed based on the results of a preliminary needs assessment of practitioners38. The testing of the model comprised a parallel group controlled design39. Twelve pharmacists (nine pharmacies) recruited 52 patients with asthma in the intervention area. Thirteen pharmacists (11 pharmacies) recruited 50 control patients. Pharmacists were extensively trained about asthma, and the DSM protocols for the delivery of the service40. In the intervention area, pharmacists delivered a service protocol with three follow up visits over six months and data was collected at each visit. In the control sites, patients received standard pharmacy services and the data was collected at baseline only. Comparison of final intervention patient outcomes with baseline values showed significant improvements in mean asthma severity score, peak flow indices, and defined daily dose of salbutamol used by patients, asthma related quality of life, perceived control of asthma and patient plus provider satisfaction41. The Illawarra Pharmacists Asthma Group that participated in the intervention were awarded the Aventis Medal of Clinical Excellence for their dedicated efforts in trialling the asthma care model.
Following the success of this pilot study, a large scale multisite randomised controlled trial tested an updated version of the model developed above42. Fifty Australian pharmacies were randomised into two groups: intervention pharmacies implemented the Pharmacy Asthma Care Program (PACP-an ongoing cycle of assessment, goal setting, monitoring and review) to 191 patients over six months, while control pharmacies gave their usual care to 205 control patients. Pharmacists in both groups administered questionnaires and conducted spirometric testing at baseline and six months later. Ninety-one per cent of the intervention and 86% of the control patients completed the study. The intervention resulted in improved asthma control: patients receiving the intervention were 2.7 times more likely to improve from “severe” to “not severe” than control patients42. The intervention also resulted in improved adherence to preventer medication, decreased mean daily dose of reliever medication and improved scores on risk of non-adherence, quality of life (difference -asthma knowledge and perceived control of asthma questionnaires42. An economic evaluation of the PACP indicated that the cost per QALY gained by the PACP was estimated to be $A 2,946 over a five year period assuming annual reviews to maintain the PACP benefit43.
The unprecedented success of the PACP led to a national implementation trial of the service as part of the Fourth community pharmacy Agreement. Under this implementation trial, nearly 100 pharmacists in several Australian states were trained to deliver the DSM model. The trial is completed and results awaiting publication. Despite the positive outcomes of the trial and the enthusiasm of the specialized and trained pharmacists, the Pharmacy Asthma Management Service has not been established as a remunerated service under the Fifth Community Pharmacy Agreement. There is now much supportive evidence for the role of pharmacists in DSM generally and asthma specifically44-46. Given the substantial improvements in clinical, humanistic and economic outcomes demonstrated by the specialised pharmacy asthma DSM models developed through years of research by the University of Sydney team, it is imperative that the pharmacy profession explore wider avenues for implementation of such models.
Health Education/Health Promotion Models
Other models of pharmacist led asthma programs that have been trialled by the proactive University of Sydney team include group based asthma education delivered by pharmacists, and asthma health promotion in pharmacy outreach models47.
Community pharmacy represents a valuable health promotion setting and there is growing research to recommend health promotion in pharmacy practice48. This is certainly true for asthma where preventive behaviours are so important. With this focus, the Sydney University Pharmacy research group trialled an innovative asthma management technique49. Between September 2002 and May 2003, seven community pharmacists from Orange, a rural town in NSW, were trained to provide two asthma outreach programs: one targeting adolescents in high schools (Year 11 students); and a public forum on asthma for the wider community. Results indicated that there was a significant increase in the mean asthma knowledge scores of Year 11 students in each high school after adolescent training. There was also a significant increase in the proportion of asthma-related pharmacy visits involving requests for information on asthma and on asthma devices after the intervention. The study provided a unique opportunity for community pharmacists to increase asthma awareness in a rural setting. It also demonstrated that it is feasible for rural community pharmacists to become involved in proactive health promotion and effectively provide asthma outreach programs.
Applying a similar health education approach, the same team also trialled a pharmacist led group asthma education approach50. This study aimed to compare the effects of two small-group asthma education interventions (one delivered by specially trained pharmacists (group A) and one delivered by a pharmacist researcher trained as an asthma educator (group B)) with usual care provided by community pharmacists (group C) on clinical and humanistic outcomes for people with asthma. Forty-eight people with asthma were recruited into groups A (n = 16), B (n = 16), and C (n = 16). At 12 weeks after the interventions there was a significant decrease in the proportion of patients with severe asthma/poor control in groups A and B compared with group C (56%, 44% and 50% to 25%, 13% and 50% respectively). In Groups A and B, the proportion of patients with optimal metered dose inhaler (MDI) technique improved from 9% and 14% respectively, at baseline, to 82% and 93% respectively, at 12 weeks. The proportion of patients with optimal dry powder inhaler (DPI) technique improved in Groups A and B from 0% and 8% respectively, at baseline to 86% and 92% respectively, at 12 weeks. No change in inhaler technique was observed for Group C. There were significant improvements in asthma knowledge scores in Groups A and B compared to Group C over time. This study clearly demonstrated that small-group asthma education delivered by pharmacists appears to be more effective than usual care in improving clinical and humanistic asthma outcomes50.
Population Needs
The health needs of rural and remote populations have come into focus globally. This is especially true in Australia where there is an undersupply of healthcare resources in rural areas. The role of community pharmacists becomes highly prominent in light of their accessibility in these areas. There are fewer facilities delivering asthma care in rural areas compared to urban settings, such as lung function testing laboratories. Further, in rural areas, there are chronic shortages of healthcare professionals such as GPs, asthma educators and respiratory specialists. To address these issues the Rural Asthma Management Service model was developed based on earlier work by the Sydney University Pharmacy Asthma Research Group. The Rural Asthma Management Service (RAMS) was unique as it clearly focused on the needs of the rural regional centres in Central West NSW. These needs were identified based on previous work which involved community health promotion49. The RAMS consisted of standardised protocols and resources based on national asthma management guidelines, delivered by specially trained community pharmacists. Patients visited the pharmacy at baseline and one, three and six months after baseline in the intervention group and at baseline plus six months after baseline in the control group. The intervention pharmacists (n = 12) were trained to deliver the RAMS model, while control pharmacists (n = 8) provided standard asthma care to their recruited patients. Fifty-one and 39 patients were recruited by intervention and control pharmacists. Data compared at the final visit between groups indicated that the RAMS patient group demonstrated a significant reduction in the asthma severity scores (7.9 +/− 2.6 versus 10.4 +/− 2.6,; a significant reduction in the risk of non-adherence to medication scores (1.6 +/− 0.7 versus 2.3 +/− 1.1,); and a significant increase in the proportion of patients owning a written action plan (50% versus 23%). These results indicated that the community pharmacy-based asthma DSM model can improve asthma outcomes for patients in rural settings.
Similar models for asthma and other chronic diseases should be tested rigorously and adopted in rural primary care practice. It is known that rural/regional pharmacists do consider that their role encompasses a broader spectrum of asthma management compared to metropolitan pharmacists24. The shortage of pharmacists in rural areas has, however, resulted in a plateau of the growth of enhanced pharmacy services provided by pharmacists, as shown in Western Australia51.
Conclusion
A decade of coordinated research into community pharmacist delivered asthma care in Australia has indicated the value of this role. Many diverse models have now been trialled using robust research designs. Most of these studies showed significant benefits for patients with improvement in clinical, humanistic and economic asthma outcomes. Patients express a high degree of satisfaction and can make informed choices about preferred service elements52. It is notable that similar structured services for asthma offered in other Australian primary healthcare venues have shown less objective evidence of improvement in patient management and outcomes as compared to those delivered through the community pharmacy53. Regardless of the service type – e.g. focused on a single aspect, multi-faceted, based on disease state management or on the concepts of health promotion, the often overwhelmingly positive results speak for a clear need for such services. It is time for healthcare policy makers, health insurance funds, and other healthcare professionals to consider utilising the largely untapped potential of the community pharmacist in asthma care. It may be the case that no one model or type is ‘best’. The community need, resources available and unique asthma issues may need to dictate the type of model chosen for implementation in a particular area. Some key aspects that need to be considered and still built upon are how asthma care services delivered by community pharmacists can be integrated into the current framework of practice of other primary care healthcare professionals. This may need to change the way professionals are trained – asthma for example is a topic for interprofessional learning programs that have been successfully implemented at the University of Sydney54. This approach needs further investigation and evaluation. Whilst the evidence for benefit of pharmacist led asthma care models is available, practical implementation in healthcare lags behind this evidence. Further research on patient uptake in the absence of research fuelled participation, and therefore long-term sustainability as well as the economic value of services needs to be conducted by pharmacy practice researchers in order to convince policy makers to take up our successful models. Non-conventional avenues for sustaining such models in primary care should be explored and tested.
ACKNOWLEDGEMENTS
All pharmacists and participants with asthma who have been so generous with their time and expertise.
Footnotes
PEER REVIEW
Not commissioned, externally peer reviewed
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
Please cite this paper as: Saini B, Krass I, Smith L, Bosnic Anticevich S, Armour C. Role of Community Pharmacists in asthma – Australian Research Highlighting Pathways for Future Primary Care Models. AMJ 2011, 4, 4, 190-200 http//dx.doi.org/10.4066/AMJ.2011.790
References
- 1.Australian Centre for Asthma Monitoring. Asthma in Australia 2008. 2008. AIHW Asthma Series no. 3.
- 2.Schneider C, Everett A, Geelhoed E, Padgett C, Ripley S, Murray K. et al. Intern pharmacists as change agents to improve the practice of nonprescription medication supply: provision of salbutamol to patients with asthma. Ann Pharmacother. 2010;44(7-8):1319–26. doi: 10.1345/aph.1P142. [DOI] [PubMed] [Google Scholar]
- 3.Barton C, Proudfoot J, Amoroso C, Ramsay E, Holton C, Bubner T. et al. Management of asthma in Australian general practice: Care is still not in line with clinical practice guidelines. Prim Care Respir J. 2009;18(2):100–5. doi: 10.3132/pcrj.2008.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basheti I, Reddel H, Armour C, Bosnic-Anticevich S.. Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respiratory Care. 2005;50(5):617–23. [PubMed] [Google Scholar]
- 5.Basheti I, Reddel H, Armour C, Bosnic-Anticevich S.. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol. 2007;119(6):1537–8. doi: 10.1016/j.jaci.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 6.Basheti I, Armour C, Bosnic-Anticevich S, Reddel H.. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Education & Counseling. 2008;72(1):26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Bosnic-Anticevich S, Sinha H, So S, Reddel H.. Metered-Does Inhaler Tehcnique: The effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47:251–6. doi: 10.3109/02770900903580843. [DOI] [PubMed] [Google Scholar]
- 8.Basheti I, Armour C, Reddel H, Bosnic-Anticevich S.. Long-term maintenance of pharmacists’ inhaler technique demonstration skills. American Journal of Pharmaceutical Education. 2010;73(2):32. doi: 10.5688/aj730232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basheti I, Armour C, Reddel H, Bosnic-Anticevich S.. Long-term maintenance of pharmacists’ inhaler technique demonstration skills. American Journal of Pharmaceutical Education. 2009;73(2):32. doi: 10.5688/aj730232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ng T, Lim T, Abisheganaden J, Eng P, Sin F.. Factors associated with acute health care use in a national adults asthma management program. Ann Allergy Asthma Immunol. 2006;97(6):784–93. doi: 10.1016/S1081-1206(10)60970-2. [DOI] [PubMed] [Google Scholar]
- 11.Kaae S, Soendergaard B, Haugboelle L, Traulsen J.. Sustaining delivery of the first publicly reimbursed cognitie service in Denmark: a cross-case analysis. International Journal of Pharmacy Practice. 2010;18(1):21–7. doi: 10.1211/ijpp.18.01.0005. [DOI] [PubMed] [Google Scholar]
- 12.Fukuda S, Yoshinaga T, Hirata N, Ishitsuka Y, Irikura M, Irie T. et al. [Individualized inhalation instruction using check sheets by a pharmacist in community pharmacy improves inhalation techniques in asthmatic patients] [Japanese] Arerugi - Japanese Journal of Allergology. 2009;58(11):1521–9. [PubMed] [Google Scholar]
- 13.National Asthma Council Australia. Asthma Management Handbook 2006. Melbourne; NAC: 2006. [Google Scholar]
- 14.Mols F, Denollet J.. Type D personality among noncardiovascular patient populations: a systematic review. Gen Hosp Psychiatry. 2010;32(1):66–72. doi: 10.1016/j.genhosppsych.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Kaptein A, Klok T, Moss-Moris R, Brand P.. Illness perceptions: impact on self-management and control in asthma. Current Opinion in Allergy & Clinical Immunology. 2010;10(3):194–9. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]
- 16.Barlow C, Wright J, Sheasby , Turner A, Hainsworth J.. Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling. 2002;48(2):177–87. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 17.Coster S., Norman I.. Cochrane reviews of educational and self-management interventions to guide nursing practice a review. Int J Nurs Stud. 2009;46(4):508–28. doi: 10.1016/j.ijnurstu.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Smith L, Bosnic-Anticevich S, Mitchell B, Saini B, Krass I, Armour C.. Treating asthma with a self-management model of illness behaviour in an Australian community pharmacy setting. Soc Sci Med. 2007;64(7):1501–11. doi: 10.1016/j.socscimed.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Barbanel D, Eldridge S, Griffiths C.. Can a self-management program delivered by a community pharmacist improve asthma control? A randomised trial. Thorax. 2003;58(10):851–4. doi: 10.1136/thorax.58.10.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott R, Barber N, Clifford S, Horne R, Hartley E.. The cost effectiveness of a telephone-based pharmacy advisory service to improve adherence to newly prescribed medicines. Pharm World Sci. 2008;30(1):17–23. doi: 10.1007/s11096-007-9134-y. [DOI] [PubMed] [Google Scholar]
- 21.Clifford S, Barber N, Elliott R, Hartley E, Horne R.. Patient-centred advice is effective in improving adherence to medicines. Pharm World Sci. 2006;28(3):165–70. doi: 10.1007/s11096-006-9026-6. [DOI] [PubMed] [Google Scholar]
- 22.Bereznicki B, Peterson G, Jackson S, Walters E, Fitzmaurice K, Gee P.. Data-mining of medication records to improve asthma management. Med J Aust. 2008;189(1):21–5. doi: 10.5694/j.1326-5377.2008.tb01889.x. [DOI] [PubMed] [Google Scholar]
- 23.Bereznicki B, Peterson G, Jackson S, Walters H, Fitzmaurice K, Gee P.. Pharmacist-initiated general practitioner referral of patients with suboptimal asthma management. Pharm World Sci. 2008;30(6):869–75. doi: 10.1007/s11096-008-9242-3. [DOI] [PubMed] [Google Scholar]
- 24.Kritikos V, Reddel H, Bosnic-Anticevich S.. Pharmacists’ perceptions of their role in asthma management and barriers to the provision of asthma services. International Journal of Pharmacy Practice. 2010;18(4):209–16. doi: 10.1111/j.2042-7174.2010.00040.x. [DOI] [PubMed] [Google Scholar]
- 25.Blais R, Laurier C, Pare M.. Effect of feedback letters to physicians and pharmacists on the appropriate use of medication in the treatment of asthma. J Asthma. 2008;45(3):227–31. doi: 10.1080/02770900701883774. [DOI] [PubMed] [Google Scholar]
- 26.The Pharmacy Guild of Australia. The Pharmacy Guild of Australia - Mirixa Australia. 2010. Accessed 7 March 2011. Available from: http://www.guild.org.au/content.asp?id=2215.
- 27.Melchior L, Carter B, Helsley A, Ernest J, Friesner D.. The diabetes disease state management exemplar. Nursing Economics. 2010;28(1):7–17. [PubMed] [Google Scholar]
- 28.Ouwens M, Wollersheim H, Hermens R, Hulscher M, Grol R.. Integrated care programs for chronically ill patients: a review of systematic reviews. Int J Qual Health Care. 2005;17:141–6. doi: 10.1093/intqhc/mzi016. [DOI] [PubMed] [Google Scholar]
- 29.Krumholz H, Currie P, Riegel B, Phillips C, Peterson E, Smith R. et al. A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006;114(13):1432–45. doi: 10.1161/CIRCULATIONAHA.106.177322. [DOI] [PubMed] [Google Scholar]
- 30.Pharmaceutical Society of Australia. Professional Practice Starndards, Version 4. 2010. Accessed 5 March 2011. Available from: http://www.psa.org.au/site.php?id=6176.
- 31.McKnight A, Thomason A.. Pharmacists’ advancing roles in drug and disease management: a review of states’ legislation. Journal of the American Pharmacists Association. 2009;49(4):544–8. doi: 10.1331/JAPhA.2009.08056. [DOI] [PubMed] [Google Scholar]
- 32.Herborg H, Soendergaard B, Jorgensen T, Fonnesbaek L, Hepler C, Holst H.. Improving drug therapy for patients with asthma - part 2: Use of antiasthma medications. Journal of the American Pharmacists Association. 2001;41(4):551–9. doi: 10.1016/s1086-5802(16)31279-7. [DOI] [PubMed] [Google Scholar]
- 33.Cordina M, McElnay J, Hughes C.. Assessment of a community pharmacy-based program for patients with asthma. Pharmacotherapy. 2001;21(10):1196–203. doi: 10.1592/phco.21.15.1196.33894. [DOI] [PubMed] [Google Scholar]
- 34.Schulz M, Verheyen F, Muhlig S, Muller J, Muhlbauer K, Knop-Schneickert E. et al. Pharmaceutical care services for asthma patients: a controlled intervention study. J Clin Pharmacol. 2001;41(6):668–76. doi: 10.1177/00912700122010438. [DOI] [PubMed] [Google Scholar]
- 35.Emmerton L, Shaw J, Kheir N.. Asthma management by New Zealand pharmacists: a pharmaceutical care demonstration project. J Clin Pharm Ther. 2003;28(5):395–402. doi: 10.1046/j.0269-4727.2003.00507.x. [DOI] [PubMed] [Google Scholar]
- 36.Mangiapane S, Schulz M, Muhlig S, Ihle P, Schubert I, Waldmann H.. Community pharmacy-based pharmaceutical care for asthma patients. Ann Pharmacother. 2005;39(11):1817–22. doi: 10.1345/aph.1G180. [DOI] [PubMed] [Google Scholar]
- 37.Herborg H, Soendergaard B, Froekjaer B, Fonnesbaek L, Jorgensen T, Hepler C.. Improving drug therapy for patients with asthma - part 1: Patient outcomes. Journal of the American Pharmacists Association. 2001;41(4):539–50. doi: 10.1016/s1086-5802(16)31278-5. [DOI] [PubMed] [Google Scholar]
- 38.Saini B, Krass I, Armour C.. Specialisation in asthma :current practice and future roles. J Soc Admn Pharm. 2001;18(5):169–77. [Google Scholar]
- 39.Saini B, Jogia R, Krass I, Armour C.. Evaluation of a practice based reseach design using an asthma care model. International Journal of Pharmacy Practice. 2002;10(3):177–84. [Google Scholar]
- 40.Saini B, Smith L, Armour C, Krass I.. An educational intervention to train community pharmacists in providing specialized asthma care. American Journal of Pharmaceutical Education. 2006;70(5):118. doi: 10.5688/aj7005118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saini B, Krass I, Armour C.. Development, implementation and evaluation of a community pharmacy-based asthma care model. Ann Pharmacother. 2004;38(11):1954–60. doi: 10.1345/aph.1E045. [DOI] [PubMed] [Google Scholar]
- 42.Armour C, Bosnic-Anticevich S, Brillant M, Burton D, Emmerton L, Krass I. et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax. 2007;62:496–502. doi: 10.1136/thx.2006.064709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gordois A, Armour C, Brillant M, Bosnic-Anticevich S, Burton D, Emmerton L. et al. Cost-effectiveness analysis of a Pharmacy Asthma Care Program in Australia. Disease Management and Health Outcomes. 2007;15(6):387–96. [Google Scholar]
- 44.Benavides S, Rodriguez J, Maniscalco-Feichtl M.. Pharmacist involvement in improving asthma outcomes in various healthcare settings: 1997 to present. Ann Pharmacother. 2009;43(1):85–97. doi: 10.1345/aph.1K612. [DOI] [PubMed] [Google Scholar]
- 45.Johannigman M, Leifheit M, Bellman N, Pierce T, Marriott A, Bishop C.. Medication therapy management and condition care services in a community-based employer setting. Am J Health Syst Pharm. 2010;67(16):1362–7. doi: 10.2146/ajhp090583. [DOI] [PubMed] [Google Scholar]
- 46.Horning K, Hoehns J, Doucette W.. Adherence to clinical practice guidelines for 7 chronic conditions in long-term-care patients who received pharmacist disease management services versus traditional drug regimen review. Journal of Managed Care Pharmacy. 2007;13(1):28–36. doi: 10.18553/jmcp.2007.13.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shah S, Roydhouse J, Sawyer S.. Asthma education in primary healthcare settings. Curr Opin Pediatr. 2008;20(6):705–10. doi: 10.1097/MOP.0b013e32831551fa. [DOI] [PubMed] [Google Scholar]
- 48.Joyce A, Sunderland B, Burrows S, McManus A, Howat P, Maycock B.. Community pharmacy’s role in promoting healthy behaviours. Journal of Pharmacy Practice and Research. 2007;37(1) [Google Scholar]
- 49.Kritikos V, Krass I, Chan HS, Bosnic-Anticevich S.. The Validity and Reliability of Two Asthma Knowledge Questionnaires. J Asthma. 2005;42:795–801. doi: 10.1080/02770900500308627. [DOI] [PubMed] [Google Scholar]
- 50.Kritikos V, Armour C, Bosnic-Anticevich S.. Interactive small-group asthma education in the community pharmacy setting: a pilot study. J Asthma. 2007;44(1):57–64. doi: 10.1080/02770900601125755. [DOI] [PubMed] [Google Scholar]
- 51.Wibowo Y, Berbatis C, Joyce A, Sunderland V.. Analysis of enhanced pharmacy services in rural community pharmacies in Western Australia. Rural & Remote Health. 2010;10(3):1400. [PubMed] [Google Scholar]
- 52.Naik Panvelkar P, Armour C, Saini B.. Community pharmacy-based asthma services - what do patients prefer? J Asthma. 2010;47(10):1085–93. doi: 10.3109/02770903.2010.514638. [DOI] [PubMed] [Google Scholar]
- 53.Holton C, Beilby J, Harris M, Harper C, Proudfoot J, Ramsay E. et al. Systematic care for asthma in Australian general practice: a randomised controlled trial. Med J Aust. 2010;193(6):332–7. doi: 10.5694/j.1326-5377.2010.tb03943.x. [DOI] [PubMed] [Google Scholar]
- 54.Saini B, Shah S, Kearey P, Bosnic-Anticevich S, Grootjans J, Armour C.. An interprofessional learning module on asthma health promotion. American Journal of Pharmaceutical Education. 2011;75(2) doi: 10.5688/ajpe75230. Article 30. [DOI] [PMC free article] [PubMed] [Google Scholar]


