Abstract
Background:
Most studies address medical treatment of infertility and psychosocial outcomes caused by infertility-related stress, but few studies examine the infertility's impact on sexuality.
Aim:
A literature review was conducted to answer the questions: 1) How is sexual self concept impacted in infertile individuals and their partners? 2) Does infertility have a negative impact on sexual relationships? 3) Is sexual function affected by infertility? In answering these questions, we may develop a better understanding of sexuality in the context of infertility, and thus better inform infertility management. Ultimately the aim is to improve the quality of life for infertile couples.
Method:
A literature search was conducted for publications from 1990 to 2011 via the electronic databases PubMed, PsycInfo and Scopus, which focused on sexuality in infertile subjects or couples.
Results:
In this review, all studies were descriptive quantitative studies which mapped the different aspects of sexuality in the context of infertility. The results suggested that infertility and its treatment approaches for fertilisation could lead to changes in sexual self-esteem, sexual relationship and sexual function.
Conclusion:
The literature substantiated that many infertile subjects experienced trouble in various aspects of sexuality. However, further research should examine the reciprocal relations between sexual self concept, sexual relationship and sexual function in the context of infertility. How these changes affect the partners of infertile subjects should also be addressed.
Keywords: Infertility, sexuality, IVF, Assisted Reproduction Technology (ART)
Introduction
Globally 8–12% of couples experience difficulty conceiving a child.1 Although assisted reproduction technology (ART) provides the possibility of achieving pregnancy, almost 40% of people undergoing ART still cannot conceive.2,3 Infertility has been described as a stressor and a life crisis for individuals or couples, which results in a lower quality of life and marital conflicts.4–7 Furthermore, there is an increasing use of medical services for the infertile.8 Although many studies have been published about infertility diagnosis and treatments, and consensus in the literature demonstrating sexual problems as crucial contributing factors,9–12 we feel that little is known regarding the psychosexual aspects of infertility. In particular little is known about the sexuality of infertile individuals or couples in the presence of a clinical diagnosis and treatment. Facing a childless status and experiencing medical treatment, the infertile couple are likely to suffer from various psychosexual problems. In addition, the diagnosis of infertility and contributing factors such as unsuccessful treatment, continuing lack of conception and childbearing, and the absence of the role as a parent may have a negative impact on marital relations,1,4,13 thus should be given careful consideration as part of an holistic approach to case management. Research is therefore necessary to understand and address these psychosocial sexual issues.
Healthy sexuality is central to psychological well-being and quality of life,14 both the World Health Organization (WHO)15 and the World Association for Sexual Health (WAS)16 state that sexuality is an integral part of being human, it is influenced by many factors, it is diverse and cannot be separated from the essential elements of human life. Historically, we found there is a lack of consensus concerning the definition of sexuality. Woods17 describes a holistic perspective on sexuality, which suggests sexuality is concerned with biologic, psychologic, sociologic, spiritual, and cultural aspects of life. Furthermore, sexuality has three major dimensions including sexual self concept, sexual relationships and sexual function. McCabe et al18 suggest sexuality is an important aspect in people's lives, it involves a broad range of cognitions, emotions and behaviours. Master et al19 suggest that sexuality is a multidimensional phenomenon with biological, psychological, behavioural, clinical, moral, and cultural aspects. Similarly, Bernhard20 also suggests sexuality as a multidimensional phenomena, composed of biological, socioeconomic, psychological and spiritual components. In addition, McCarthy et al21 suggest sexuality is more than the physical act of intercourse, as it influences self-identity, communication, sharing pleasure, deepening intimacy and may lessen stress in one's life. However, from the above mentioned definition of sexuality, we can have a clear understanding that sexuality is not just the state of being physically able to perform a sex act or to conceive a child, but as an integral component of human life with multidimensional content. In conclusion, Woods's perspective on sexuality provides a useful conceptual framework for holistic, sexuality research, also combining with clear definition on every dimension as follows:17 1) sexual self concept refers to the image one has of oneself as a man or a woman and the evaluation of one's adequacy in masculine or feminine roles, including body image, sexual self schema and sexual esteem; 2) sexual relationships as the interpersonal relationships in which one's sexuality is shared with another; 3) sexual function is about the ability of an individual to give and receive sexual pleasure, including various physical and psychological progresses in the sexual response cycle. These have been acknowledged by various studies. 22–26
From the purpose of the study, in this paper Woods's conceptual framework of sexuality was used to make analysis pertaining to sexuality in infertile individuals or couples. We focused on changes in sexuality following infertility diagnosis and treatment and provide recommendations for future research. The following questions were addressed.
How is sexual self concept impacted in infertile individuals and their partners?
Does infertility have a negative impact on the sexual relationship between infertile individuals and their partners?
Is sexual function affected by infertility?
Methods
Based on the purpose of this study, research articles for this literature review were searched via a range of databases, which were MedLine (Ovid), PsycInfo (Ovid) and Scopus. In addition, references lists from retrieved articles were also hand searched for relevance. Duplicated articles, or those that did not meet inclusion criteria were excluded from the review.
Search strategy
The bibliography was compiled using Infertility “OR” Childless in the title, abstract, or keywords. Since some studies linked with sexuality are explored in the context of clinical treatment, so in our review study, in-vitro fertilisation (IVF) “OR” intra-cytoplasmic sperm injection (ICSI) “OR” ART were also included as terms in the search strategy. All of these terms were in various combinations with infertile individuals or couples' sexuality. These included sexual self concept, body image, sexual esteem, communication, intimacy, relationship, sexual function/dysfunction, sexual disorder, sexual health, sex life, sexual behaviour or sexual problems. Furthermore, the databases were searched with combinations of infertile males, infertile females, infertile subject, infertile couples, spouses, or partner.
Inclusion and exclusion criteria
The literature search was based on a theoretical design rather than on a systematic review format. To be included in the review, the retrieved articles were confined to the following criteria:
Criteria 1: Peer-reviewed articles published in the English language between 1990 and 2011;
Criteria 2: The primary or secondary objective of the study was regarding sexuality in the context of infertility;
Criteria 3: The study participants comprised of infertile subjects, or infertile couples comprising infertile subjects and their partners;
Criteria 4: The study needed to report originally collected data via the validated questionnaire. Reviews, editorials and debates, letters, case reports, non-peer-reviewed articles, meeting abstracts and brief communications were excluded.
In addition, studies that discussed infertility as a consequence of other conditions such as hysterectomy, tubal ligation or cancer were to be excluded because the changes of sexuality are intrinsically linked to the baseline status, and also different health conditions might affect the subjects' sexuality.
Results
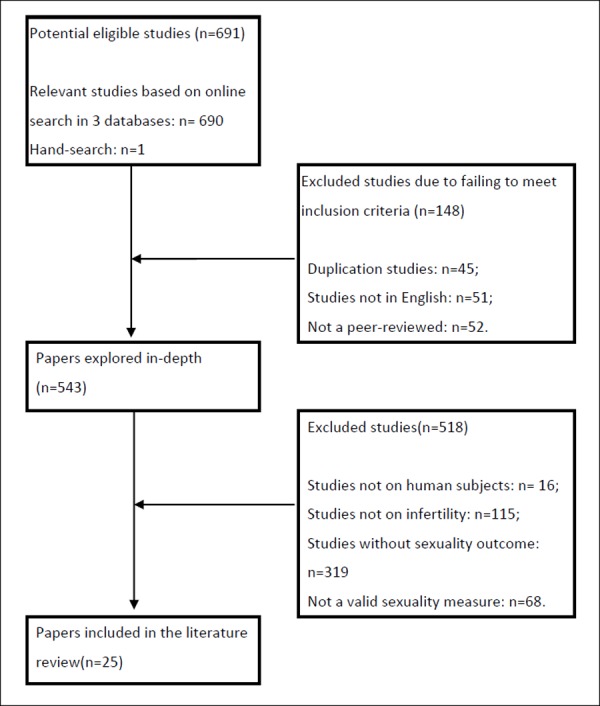
Through the literature retrieving strategy, finally 24 studies were sourced via online search. The results of this comprehensive search are outlined in Figure 1. In addition, through a hand search, one further research paper was found which met the selection criteria. Therefore, in total 25 studies were sourced which examined some aspects of sexuality in infertile individuals and couples.
Figure 1: Flowchart of literature searches performed.
All papers selected were reviewed to ensure congruency with the aim of the study. The relationship between infertility and sexuality were discussed using the following themes.
(1) How is sexual self concept impacted in infertile individuals and their partners?
Despite an extensive literature search, we found no sourced study that examined sexual self schema and body image of infertile individuals.
In some studies, infertile self-esteem was given more attention, the results demonstrated that infertile males had lower self-esteem,27–29 which was associated with changes in stress levels over the course of treatment.30 Women on IVF were found to have lower self-esteem than controls prior to the treatment cycle,31,32 also associated with unsuccessful IVF treatment in infertile females,33,34 but effective adjustment to infertility could contribute to positive self-esteem.35 Of all the retrieved studies, two studies of infertile couples specifically focused on the term of sexual self-esteem, which suggested that infertility-related stress tended to decrease the sexual self-esteem of women more than their male partner.36,37
It is a fact that there is a scarcity of research about sexual esteem in infertile individuals and their partners, and self-esteem is addressed in more studies. This might be due to self-esteem being recognised as an important part of both a person's sexual confidence and adequacy.38 However, sexual esteem mainly refers to the tendency to evaluate one's sexuality positively and is related to others39 its discussion specifically in the context of infertility in the future will be helpful for better understanding the sexuality of infertile clients and their partners.
(2) Does infertility have a negative impact on the sexual relationship of infertile couples?
Infertile males had a lower sexual and personal quality of life compared with the male partners of couples without perceived male factor infertility.40 It was also found that the male partner in infertile couples experienced less sexual satisfaction when compared with the female partner. It was hypothesised that this was due to the psychological pressure associated with efforts to conceive, or to the forced timing of intercourse around the female's ovulatory cycle.4 Furthermore, diagnosed male factor and infertility duration of 3–6 years contributed to higher relationship instability and lower sexual satisfaction in both females and males from infertile couples.41
The sexual satisfaction of infertile females was found to be various at different stages of treatment, with the most profound change occurring during treatment. This impacted most on the couple's sexual relations. Furthermore, other studies demonstrated that females with unsuccessful IVF treatment had a lower satisfaction with married life compared to those who subsequently conceived or adopted.33,42,43 In addition, Lee et al44 suggested that the wives expressed less sexual satisfaction than their partners both in only male factor infertility and combining male-female factor infertility; also the results showed no difference in sexual satisfaction between wives and husbands in infertile couples with unexplained factor infertility; but the wives from infertile couples with female factor infertility had less sexual satisfaction than their husbands. However, other studies had contrary results which suggested infertility and its treatment did not have a negative influence on sexual relationship and satisfaction because the shared stress of infertility could make both couples more involved jointly with the same problem.45–48
(3) Is sexual function affected by infertility?
Regarding sexual function in infertile subjects, most of the retrieved studies discussed premature ejaculation and erectile dysfunction, and in females sexual desire, sexual arousal, orgasm and sexual pain.
Generally the results of findings from the retrieved studies indicated that infertility could influence sexual activity in infertile couples, and that fertility problem stress tended to decrease frequency of intercourse.29,36,49 Frequency of coitus could be regarded as an acceptable indicator of sexual satisfaction in male partners of infertile couples.50 As for the sexual function of infertile subjects, studies demonstrated premature ejaculation and erectile dysfunction were prevalent among male partners of infertile couples.51–53 In addition, a cohort observational study reported 11% of males experienced problems with erection or orgasm after the diagnosis of abnormal semen parameters, which might be psychologically related in the evaluation of infertility.54
Among infertile females, some studies demonstrated sexual dysfunctions, especially sexual arousal, as being very common.10,53,55–60 Another study indicated there was no statistically significant difference in sexual function between infertile females and females seeking elective sterilisation, but a trend was noted toward greater sexual problems in these two female groups.4
Discussion
In this review, all studies were descriptive quantitative studies which basically mapped sexuality in the context of infertility. Results suggested that infertility and associated treatment may lead to changes in sexual self-esteem, sexual relations and sexual function, which further affected the infertile couple's quality of life, and well-being.
For the infertile subjects, infertility affects self concept and role perceptions, and is a threat to personal identity. For infertile women, the negative impact on self-esteem has a greater effect on sexual confidence than it does in infertile men. Unfortunately, the retrieved studies do not record further analysis on these changes. It would be helpful if there had been an investigation of the extent and the perceived reasons for such changes. Almost no studies examine the impact of gender-specific diagnosis on changing sexual self concept in men and women, respectively. Such information would be useful along with a comparative analysis. Sexual self concept is a core component of sexuality,61 it is necessary to give more attention to the experience of infertility and its influence on one's cognitive view of self and one's sexuality. Future studies should further address how infertility and its treatment have the potential to affect the sexual self concept. This should include issues such as female's body image and infertile subject's sexual esteem, in conjunction with how infertility affects partners.
Regarding sexual relations for infertile couples, some studies demonstrated there were no significant correlations between infertility and sexual relations but other studies suggested infertility impaired sexual relations. We postulate that this result might be explained by different aspects such as gender differences in the reaction to infertility, the different stages of infertility treatment and/or different social demographics. In order to have a comprehensive understanding of sexual relations in the context of infertility, it is necessary to further consider the association between sexual self concept and sexual relations, and the quality of communication in infertile couples. However, most retrieved studies focused on the assumption that infertility might negatively affect sexual relations. Future studies should investigate factors that might positively affect sexual relations in infertile couples.
Among the infertile subjects, we found the sexual dysfunction could be a consequence of the diagnosis, investigation and treatment of infertility. The main reason for the infertile male's sexual dysfunction was related to a perception of losing his masculinity.62 Problems associated with sexual pleasure appeared to be due to the mechanical and forced sexual activities for conception purposes, which included scheduled post-coital tests, and the optimal states for sexual intercourse during the female ovulatory period. 63 Sexual dysfunction was also prevalent in female partners of infertile couples, and positively correlated with the male partner's sexual function.64
Although the retrieved studies provided some indication of the effect of infertility on sexuality, most focused on the physical aspects of sexuality such as sexual behaviour, problems or disorders.4,55,60,62,65–74 These studies did not make further analysis on the influence of age, length of conjugal relationship, the period since diagnosis and treatment, treatment stages, general health status, and socio-demographic conditions. In addition, the studies of sexuality were confined to physical aspects, and failed to address the impact on the partner or the influence this might have. Further, the studies rarely took a gender perspective to explore sexuality issues. In addition, we found very little research that focused on factors that might positively affect sexual self-esteem, sexual relationship and sexual function. It is our view that it is necessary to address sexual self concept and sexual relations and sexual function with a holistic approach.
Conclusion
The literature substantiates that sexuality can be greatly affected by infertility and its treatment, with infertile subjects experiencing difficulties in different aspects of sexuality. It is necessary for further research to examine the reciprocal relations between sexual self concept, sexual relationship and sexual function in the context of infertility. Moreover, the sexuality of infertile subjects might be influenced by their partner's reaction to the diagnosis.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare no competing interests.
FUNDING
This review is part of the corresponding author's PhD study named as Infertility and Marital Well-being among Infertile, Chinese Couples from Hei Longjiang Province in China, which is funded by Curtin Strategic International Research Scholarship (CSIRS).
ETHICS COMMITTEE APPROVAL
The corresponding author's PhD study is approved by Human Research Ethics Committee of Curtin University (Perth, Australia) and the Ethical Committee of the First Clinical College of Harbin Medical University (China).
Please cite this paper as: Tao P, Coates R, Maycock B. The impact of infertility on sexuality: A literature review. AMJ 2011, 4, 11, 620–627 http//dx.doi.org/10.4066/AMJ.2011.1055
References
- 1.World Health Organization. WHO Technical Report Series 820. Geneva: World Health Organization Publications; 1992. Recent Advances in Medically Assisted Conception; pp. 1–7. [PubMed] [Google Scholar]
- 2.Collins JA, Garner JB, Wilson EH, Wrixon W, Casper RF.. A proportional hazards analysis of the clinical characteristics of infertile couples. Am J Obstet Gynecol. 1984;148(5):527–32. doi: 10.1016/0002-9378(84)90741-5. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt L.. Infertility and assisted reproduction in Denmark. Dan Med Bull. 2006;53(4):390–417. Epidemiology and psychosocial consequences. [PubMed] [Google Scholar]
- 4.Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T.. Impact of infertility on quality of life, marital adjustment and sexual function. Urology. 2004;63(1):126–30. doi: 10.1016/j.urology.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 5.Newton CR, Sherrard W, Glavac I.. The Fertility Problem Inventory: measuring perceived infertility-related stress. Fertil Steril. 1999;72(1):54–62. doi: 10.1016/s0015-0282(99)00164-8. [DOI] [PubMed] [Google Scholar]
- 6.Chachamovich J, Chachamovich E, Fleck MP, Cordova FP, Knauth D, Passos E.. Congruence of quality of life among infertile men and women: findings from a couple-based study. Hum Reprod. 2009;24(9):2151–7. doi: 10.1093/humrep/dep177. [DOI] [PubMed] [Google Scholar]
- 7.Klemetti R, Raitanen J, Sihvo S, Saarni S, Koponen P.. Infertility, mental disorders and well-being – a nationwide survey. Acta Obstet Gynecol Scand. 2010;89(5):677–82. doi: 10.3109/00016341003623746. [DOI] [PubMed] [Google Scholar]
- 8.Templeton A, Fraser C, Thompson B.. Infertility – epidemiology and referral practice. Hum Reprod. 1991;6(10):1391–4. doi: 10.1093/oxfordjournals.humrep.a137275. [DOI] [PubMed] [Google Scholar]
- 9.Boivin J, Appleton TC, Baetens P, Baron J, Bitzer J, Corrigan E, Daniels KR, Darwish J, Guerra-Diaz D, Hammar M, McWhinnie A, Strauss B, Thorn P, Wischmann T, Kentenich H.. Guidelines for counselling in infertility: outline version. Hum Reprod. 2001;16(6):1301–4. doi: 10.1093/humrep/16.6.1301. [DOI] [PubMed] [Google Scholar]
- 10.Audu BM.. Sexual dysfunction among infertile Nigerian women. Journal of Obstetrics & Gynaecology. 2002;22(6):655–7. doi: 10.1080/0144361021000020475. [DOI] [PubMed] [Google Scholar]
- 11.Bar-Chama N, Schiff J, Yavorsky R, Diefenbach M.. Erectile dysfunction and infertility. Current Sexual Health Reports. 2007;4(1):20–3. [Google Scholar]
- 12.Herer E, Holzapfel S.. The medical causes of infertility and their effects on sexuality. Canadian Journal of Human Sexuality. 1993;2(3):113–20. [Google Scholar]
- 13.Sherrod RA.. Understanding the emotional aspects of infertility: implications for nursing practice. J Psychosoc Nurs Ment Health Serv. 2004;42(3):40–7. [PubMed] [Google Scholar]
- 14.World Health Organisation. The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine. 1995;41(10):1403–9. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Report of a technical consultation on sexual health. 2002 Available online at: http://www.who.int/reproductivehealth/publications/sexual_health/defining_sexual_health.pdf [verified August 2011] [Google Scholar]
- 16.World Association for Sexual Health. Working Definitions after WHO Technical Consultation on Sexual Health. Available online at http://www.worldsexualhealth.org/resources [verified July 2011] [Google Scholar]
- 17.Woods NF.. Toward a holistic perspective of human sexuality: alterations in sexual health and nursing diagnoses. Holist Nurs Pract. 1987;1(4):1–11. doi: 10.1097/00004650-198708000-00004. [DOI] [PubMed] [Google Scholar]
- 18.McCabe MP, Cummins RA, Romeo Y.. Relationship status, relationship quality, and health. Journal of Family Studies. 1996;2:109–20. [Google Scholar]
- 19.Master WH, Johnson VE, Kolodny RC. In: Master WH, Johnson VE, Kolodny RC, editors. New York: Harper Collins College Publishers; 1999. What is human sexuality? In Human Sexuality; pp. 21–30. [Google Scholar]
- 20.Bernhard LA.. Sexuality and sexual health care for women. Clin Obstet Gynecol. 2002;45(4):1089–98. doi: 10.1097/00003081-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy BW, Bodnar EL.. The equity model of sexuality: navigating and negotiating the similarities and differences between men and women in sexual behaviour, roles and values. Sexual and Relationship Therapy. 2005;20:225–35. [Google Scholar]
- 22.Newshan G.. Sexuality and the HIV-positive individual. SIECUS Report. 1992;20(5):1–3. [Google Scholar]
- 23.Krebs LU.. Sexual assessment in cancer care: concepts, methods, and strategies for success. Semin Oncol Nurs. 2008;24(2):80–90. doi: 10.1016/j.soncn.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Krebs LU.. Sexual assessment: research and clinical. Nurs Clin North Am. 2007;42(4):515–29. doi: 10.1016/j.cnur.2007.07.004. v. [DOI] [PubMed] [Google Scholar]
- 25.Bruner DW, Boyd CP.. Assessing women's sexuality after cancer therapy: checking assumptions with the focus group technique. Cancer Nurs. 1999;22(6):438–47. doi: 10.1097/00002820-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Butler L, Banfield V, Sveinson T, Allen K.. Conceptualizing sexual health in cancer care. West J Nurs Res. 1998;20(6):683–99. doi: 10.1177/019394599802000603. discussion 700–5. [DOI] [PubMed] [Google Scholar]
- 27.Kedem P, Mikulincer M, Nathanson YE, Bartoov B.. Psychological aspects of male infertility. Br J Med Psychol. 1990;63:73–80. doi: 10.1111/j.2044-8341.1990.tb02858.x. (Pt 1) [DOI] [PubMed] [Google Scholar]
- 28.Pasch LA, Dunkel-Schetter C, Christensen A.. Differences between husbands' and wives' approach to infertility affect marital communication and adjustment. Fertil Steril. 2002;77(6):12417. doi: 10.1016/s0015-0282(02)03097-2. [DOI] [PubMed] [Google Scholar]
- 29.Slade P, Raval H, Buck P, Lieberman B.. A 3-year follow-up of emotional, marital and sexual functioning in couples who were infertile. Journal of Reproductive and Infant Psychology. 1992;10(4):233–43. [Google Scholar]
- 30.Schneider MG, Forthofer MS.. Associations of psychosocial factors with the stress of infertility treatment. Health Soc Work. 2005;30(3):183–91. doi: 10.1093/hsw/30.3.183. [DOI] [PubMed] [Google Scholar]
- 31.Hynes GJ, Callan VJ, Terry DJ, Gallois C.. The psychological well-being of infertile women after a failed IVF attempt: the effects of coping. Br J Med Psychol. 1992;65:269–78. doi: 10.1111/j.2044-8341.1992.tb01707.x. (Pt 3) [DOI] [PubMed] [Google Scholar]
- 32.van Balen F, Trimbos-Kemper TC.. Long-term infertile couples: a study of their well-being. J Psychosom Obstet Gynaecol. 1993;14 Suppl:53–60. [PubMed] [Google Scholar]
- 33.Bryson CA, Sykes DH, Traub AI.. In vitro fertilization: a long-term follow-up after treatment failure. Hum Fertil (Camb) 2000;3(3):214–20. doi: 10.1080/1464727002000199011. [DOI] [PubMed] [Google Scholar]
- 34.Cox SJ, Glazebrook C, Sheard C, Ndukwe G, Oates M.. Maternal self-esteem after successful treatment for infertility. Fertil Steril. 2006;85(1):84–9. doi: 10.1016/j.fertnstert.2005.07.1287. [DOI] [PubMed] [Google Scholar]
- 35.Koropatnick S, Daniluk J, Pattinson HA.. Infertility: a non-event transition. Fertil Steril. 1993 Jan;59(1):163–71. doi: 10.1016/s0015-0282(16)55633-7. [DOI] [PubMed] [Google Scholar]
- 36.Andrews FM, Abbey A, Halman LJ.. Stress from infertility, marriage factors, and subjective well-being of wives and husbands. J Health Soc Behav. 1991;32(3):238–53. [PubMed] [Google Scholar]
- 37.Lee TY, Sun GH.. Psychosocial response of Chinese infertile husbands and wives. Arch Androl. 2000;453:143–8. doi: 10.1080/01485010050193913. [DOI] [PubMed] [Google Scholar]
- 38.Burgoyne D.. How self esteem affects sexual behavior. Medical Aspects of Human Sexuality. 1982;16(12):70D–H. [Google Scholar]
- 39.Snell WE, Fisher TD, Walters AS.. The Multidimensional Sexuality Questionnaire: An objective self-report measure of psychological tendencies associated with human sexuality. Annals of Sex Research. 1993;6:27–55. [Google Scholar]
- 40.Smith JF, Walsh TJ, Shindel AW, Turek PJ, Wing H, Pasch L, Katz PP.. Sexual, marital, and social impact of a man's perceived infertility diagnosis. Journal of Sexual Medicine. 2009;6(9):2505–15. doi: 10.1111/j.1743-6109.2009.01383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drosdzol A, Skrzypulec V.. Evaluation of marital and sexual interactions of Polish infertile couples. Journal of Sexual Medicine. 2009;6(12):3335–46. doi: 10.1111/j.1743-6109.2009.01355.x. [DOI] [PubMed] [Google Scholar]
- 42.Benazon N, Wright J, Sabourin S.. Stress, sexual, satisfaction and marital adjustment in infertile couples. Journal of Sex & Marital Therapy. 1992;18(4):273–84. doi: 10.1080/00926239208412852. [DOI] [PubMed] [Google Scholar]
- 43.Pepe MV, Byrne T.. Women's perceptions of immediate and long-term effects of failed infertility treatment on marital and sexual satisfaction. Family Relations: An Interdisciplinary Journal of Applied Family Studies. 1991;40(3):303–9. [Google Scholar]
- 44.Lee TY, Sun GH, Chao SC.. The effect of an infertility diagnosis on the distress marital and sexual satisfaction between husbands and wives in Taiwan. Hum Reprod. 2001;16(8):1762–7. doi: 10.1093/humrep/16.8.1762. [DOI] [PubMed] [Google Scholar]
- 45.Muller MJ, Schilling G, Haidl G.. Sexual satisfaction in male infertility. Arch Androl. 1999;42(3):137–43. doi: 10.1080/014850199262797. [DOI] [PubMed] [Google Scholar]
- 46.Repokari L, Punamaki RL, Unkila-Kallio L, Vilska S, Poikkeus P, Sinkkonen J, Almqvist F, Tiitinen A, Tulppala M.. Infertility treatment and marital relationships: A 1-year prospective study among successfully treated ART couples and their controls. Hum Reprod. 2007;22(5):1481–91. doi: 10.1093/humrep/dem013. [DOI] [PubMed] [Google Scholar]
- 47.Oddens BJ, den Tonkelaar I, Nieuwenhuyse H.. Psychosocial experiences in women facing fertility problems – a comparative survey. Hum Reprod. 1999;14(1):255–61. doi: 10.1093/humrep/14.1.255. [DOI] [PubMed] [Google Scholar]
- 48.Oei SG, Helmerhorst FM, Bloemenkamp KW, Keirse MJ.. Effect of the postcoital test on the sexual relationship of infertile couples: a randomized controlled trial. Fertil Steril. 1996;65(4):771–5. doi: 10.1016/s0015-0282(16)58212-0. [DOI] [PubMed] [Google Scholar]
- 49.Jindal UN, Dhall GI.. Psychosexual problems of infertile women in India. Int J Fertil. 1990;35(4):222–5. [PubMed] [Google Scholar]
- 50.Ramezanzadeh F, Aghssa MM, Jafarabadi M, Zayeri F.. Alterations of sexual desire and satisfaction in male partners of infertile couples. Fertil Steril. 2006;85(1):139–43. doi: 10.1016/j.fertnstert.2005.07.1285. [DOI] [PubMed] [Google Scholar]
- 51.Shindel AW, Nelson CJ, Naughton CK, Mulhall JP.. Premature ejaculation in infertile couples: Prevalence and correlates. Journal of Sexual Medicine. 2008;5(2):485–91. doi: 10.1111/j.1743-6109.2007.00690.x. [DOI] [PubMed] [Google Scholar]
- 52.Shindel AW, Nelson CJ, Naughton CK, Ohebshalom M, Mulhall JP.. Sexual function and quality of life in the male partner of infertile couples: prevalence and correlates of dysfunction. J Urol. 2008;179(3):1056–9. doi: 10.1016/j.juro.2007.10.069. [DOI] [PubMed] [Google Scholar]
- 53.Jain K, Radhakrishnan G, Agrawal P.. Infertility and psychosexual disorders: relationship in infertile couples. Indian J Med Sci. 2000;54(1):1–7. [PubMed] [Google Scholar]
- 54.Saleh RA, Ranga GM, Raina R, Nelson DR, Agarwal A.. Sexual dysfunction in men undergoing infertility evaluation: a cohort observational study. Fertil Steril. 2003;79(4):909–12. doi: 10.1016/s0015-0282(02)04921-x. [DOI] [PubMed] [Google Scholar]
- 55.Millheiser LS, Helmer AE, Quintero RB, Westphal LM, Milki AA, Lathi RB.. Is infertility a risk factor for female sexual dysfunction? A case-control study. Fertil Steril. 2010;94(6):2022–5. doi: 10.1016/j.fertnstert.2010.01.037. [DOI] [PubMed] [Google Scholar]
- 56.Tayebi N, Ardakani SMY.. The prevalence of sexual dysfunctions in infertile women. Middle East Fertility Society Journal. 2007;12(3):184–7. [Google Scholar]
- 57.Carter J, Applegarth L, Josephs L, Grill E, Baser RE, Rosenwaks Z.. A cross-sectional cohort study of infertile women awaiting oocyte donation: the emotional, sexual, and quality-of-life impact. Fertil Steril. 2011;95(2):711–6 e1. doi: 10.1016/j.fertnstert.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 58.Oskay UY, Beji NK, Serdaroglu H.. The issue of infertility and sexual function in Turkish women. Sexuality and Disability. 2010;28(2):71–9. [Google Scholar]
- 59.Abbasalizadeh F., Fardy-Azar Z., Ranjbar-Koucheksaray F.. Correlation of Infertility and Sexual Dysfunction. Research Journal of Biological Sciences. 2008;3(1):52–6. [Google Scholar]
- 60.Khademi A, Alleyassin A, Amini M, Ghaemi M.. Evaluation of sexual dysfunction prevalence in infertile couples. Journal of Sexual Medicine. 2008;5(6):1402–10. doi: 10.1111/j.1743-6109.2007.00687.x. [DOI] [PubMed] [Google Scholar]
- 61.Andersen BL.. Surviving cancer: the importance of sexual self-concept. Med Pediatr Oncol. 1999;33(1):15–23. doi: 10.1002/(sici)1096-911x(199907)33:1<15::aid-mpo4>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 62.Lenzi A, Lombardo F, Salacone P, Gandini L, Jannini EA.. Stress, sexual dysfunctions, and male infertility. J Endocrinol Invest. 2003;26(3 Suppl):72–6. [PubMed] [Google Scholar]
- 63.Elia J, Delfino M, Imbrogno N, Mazzilli F.. The impact of a diagnosis of couple subfertility on male sexual function. Journal of Endocrinological Investigation. 2010;33(2):74–6. doi: 10.1007/BF03346556. [DOI] [PubMed] [Google Scholar]
- 64.Nelson CJ, Shindel AW, Naughton CK, Ohebshalom M, Mulhall JP.. Prevalence and predictors of sexual problems, relationship, stress and depression in female partners of infertile couples. Journal of Sexual Medicine. 2008;5(8):1907–14. doi: 10.1111/j.1743-6109.2008.00880.x. [DOI] [PubMed] [Google Scholar]
- 65.Bar-Hava M, Azem F, Yovel I, Lessing JB, Amit A, Abramov L, Militscher I, Chen J.. The interrelationship between coping strategies and sexual functioning in in vitro fertilization patients. J Sex Marital Ther. 2001;27(5):389–94. doi: 10.1080/713846818. [DOI] [PubMed] [Google Scholar]
- 66.Coeffin-Driol C, Giami A.. The impact of infertility and its treatment on sexual life and marital relationships: review of the literature. Gynecol Obstet Fertil. 2004;32(7–8):624–37. doi: 10.1016/j.gyobfe.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 67.Fagan PJ, Schmidt Jr, CW, Rock JA, Damewood MD, Halle E, Wise TN.. Sexual functioning and psychologic evaluation of in vitro fertilization couples. Fertil Steril. 1986;46(4):668–72. doi: 10.1016/s0015-0282(16)49646-9. [DOI] [PubMed] [Google Scholar]
- 68.Leiblum SR, Aviv A, Hamer R.. Life after infertility treatment: a long-term investigation of marital and sexual function. Hum Reprod. 1998;13(12):3569–74. doi: 10.1093/humrep/13.12.3569. [DOI] [PubMed] [Google Scholar]
- 69.Shindel AW, Nelson CJ, Naughton CK, Ohebshalom M, Mulhall JP. Sexual function and quality of life in the male partner of infertile couples: prevalence and correlates of dysfunction. J Urol. 2008;179(3):1056–9. doi: 10.1016/j.juro.2007.10.069. [DOI] [PubMed] [Google Scholar]
- 70.Nelson CJ, Shindel AW, Naughton CK, Ohebshalom M, Mulhall JP.. Prevalence and predictors of sexual problems, relationship, stress and depression in female partners of infertile couples. Journal of Sexual Medicine. 2008;5(8):1907–14. doi: 10.1111/j.1743-6109.2008.00880.x. [DOI] [PubMed] [Google Scholar]
- 71.Janssen OE, Hahn S, Tan S, Benson S, Elsenbruch S.. Mood and sexual function in polycystic ovary syndrome. Semin Reprod Med. 2008;26(1):45–52. doi: 10.1055/s-2007-992924. [DOI] [PubMed] [Google Scholar]
- 72.Drosdzol A, Skrzypulec V.. Quality of life and sexual functioning of Polish infertile couples. Eur J Contracept Reprod Health Care. 2008;13(3):271–81. doi: 10.1080/13625180802049187. [DOI] [PubMed] [Google Scholar]
- 73.Boorjian S, Hopps CV, Ghaly SW, Parker M, Mulhall JP.. The utility of sildenafil citrate for infertile men with sexual dysfunction: a pilot study. BJU Int. 2007;100(3):603–6. doi: 10.1111/j.1464-410X.2007.07038.x. [DOI] [PubMed] [Google Scholar]
- 74.Nene UA, Coyaji K, Apte H.. Infertility: a label of choice in the case of sexually dysfunctional couples. Patient Educ Couns. 2005;59(3):234–8. doi: 10.1016/j.pec.2005.08.005. [DOI] [PubMed] [Google Scholar]


