Abstract
Background
Chronic suppurative otitis media (CSOM) is assumed to be a complication of acute otitis media (AOM), but the risk factors for CSOM are not clear. Objectives: 1. To study the aetiological organisms for CSOM. 2. To identify the effect of demographic factors on disease manifestation.
Method
This retrospective study included a case series of 234 patients who had been admitted to National Hospital of Sri Lanka (NHSL), with the complaint of ear discharge and from whom the specimens were sent for microscopy and culture at Department Of Microbiology, NHSL. The period of analysis was 1 year extending from 1 January 2009 to 31 December 2009.Consecutive patients who fulfilled the inclusion criteria were recruited to the retrospective analysis.
Results
Among 234 patients studied, 129 (55.1%) were male and 150 (64.1%) were under 40 yrs old. The mean age was 39.5 yrs (range 12 to 60 yrs, SD = 22.6). The mean duration of ear discharge was 1.2 yrs. (range 6 weeks to 20 yrs.) Pseudomonas species (29.5%) was the commonest microbial organism to cause ear discharge, followed by staphylococcus (20.5%) and coliform (16.7%) species. Among the fungal agents identified, candida was the most common. 23.1% of the cultures did not reveal any microbiological agent. Eighteen patients (8%) had a prior history of trauma to the affected ear and 51 patients (21.8%) were diagnosed with diabetes mellitus.
Conclusion
The commonest microbial agents implicated in CSOM was pseudomonas species followed by staphylococci and coliforms. Demographic variables such as gender or age did not seem to affect the disease manifestation significantly, though CSOM was less common among elderly and women.
Keywords: Chronic suppurative otitis media, aetiology
Background
Chronic suppurative otitis media (CSOM) is assumed to be a complication of acute otitis media (AOM), but the risk factors for CSOM are not clear. Frequent upper respiratory tract infections and poor socioeconomic conditions (overcrowded housing and poor hygiene and nutrition) may be related to the development of chronic suppurative otitis media.1-4 However, a systematic review found no clear evidence that antibiotics are effective in preventing the progression of AOM to CSOM even among children who are at high risk for the disease.5
A chronic discharging ear is one with a perforated tympanic membrane and persistent drainage from the middle ear. Unlike otitis media with effusion which is common in the West,6-8 chronic discharging ears are highly prevalent in the tropical regions including South Asia. It may often be accompanied by complications9-12 including septicaemia, meningitis, brain abscess, facial paralysis and mental retardation13 and it is believed to be responsible for more than two-thirds of deafness in children. Unfortunately, the management of the chronic discharging ear is still limited to daily ear dressing until a dry ear is achieved14 and mastoidectomy is reserved for complications.15, 16
Facilities for middle ear reconstruction and micro-otological surgery are largely lacking in sub-regions local to the National Hospital of Sri Lanka (NHSL). Other limitations to management are the paucity of specialized ENT clinics and the cost of managing these patients.
The impact of these factors on the management of the persistently discharging ears at the NHSL have necessitated the review of the burden of CSOM, the current status of management and the possible methods for improvement.
Ear discharge had been the commonest ear problem presenting to the NHSL, over recent years. Identification of the aetiological organisms not only aids in the diagnosis and improves the management of patients, but also assists in advising the patients about the modes of spread, methods of prevention and anticipating the possible complications. Also, as certain aetiological agents are more common in healthcare settings, the healthcare institutions can be directed regarding appropriate hygiene and sterility practice when relevant. Therefore in the present study we investigated the aetiological agents (bacteria, fungi) for patients admitted with ear discharge, with emphasis on the microbiological organism and the effect of demographic factors in the causation.
Methods
Study design
This study used retrospective case series analysis of inpatients who presented with chronic ear discharge at the NHSL ENT department during a one year period, from January 2009 to December 2009. Consecutive patients, who fulfilled the criteria for the study, were included in the study.
Patients
All in patients who presented to the NHSL ENT Department during the study period and had ear discharge of more than six weeks duration despite out-patient treatment were included in the study.
Exclusion criteria included:
Terminally ill patients
Patients with systemic illness such as septicaemia
Patients with ear discharge for less than six weeks
Patients who did not consent
Patients less than 10 years as they were not routine admissions to NHSL
Patients who were given a diagnosis of otitis externa in addition to CSOM.
Methods
Consecutive patients' medical notes were reviewed using a check list. Information obtained from each patient included,
Demographic factors such as age, gender, marital status, district of residence.
Duration of ear discharge.
Results of the culture reports of ear swab.
All the laboratory procedures were done at the NHSL Department of Microbiology.
Ethical aspects
This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethical committee of NHSL.
Data Analysis
All data were entered into the Statistical Package for Scientific Studies (SPSS) version 17.0 and standard deviations (SD), standard errors (SE), standard normal deviates (SND) and probability values were calculated to derive conclusions regarding significance levels.
Results
During the one year study period there had been 280 patients admitted for ear discharge to the ENT department for whom specimens had been sent for microscopy and culture. Of these, 234 patients met inclusion criteria so were further analyzed.
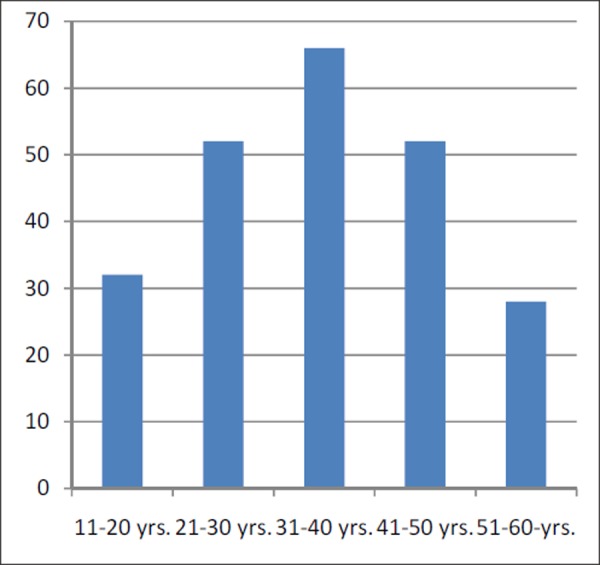
One hundred and twenty-nine patients (55.1%) were male (see Figure 1) and 150 (64.1%) were under 40 yrs old (see Figure 2). The mean age was 39.5 yrs. (age range from 12 to 60 yrs., SD=22.6).
Figure 1. Gender distribution of the studied sample.
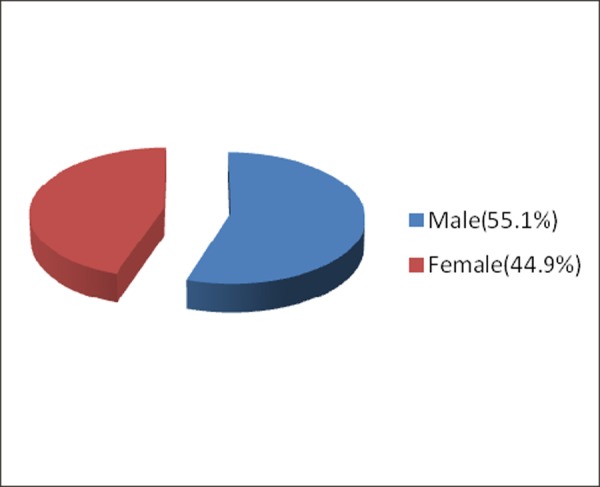
Figure 2. Age distribution of the study population.
The mean duration of ear discharge was 1.2 yrs. (range 6 weeks to 20 yrs.) Eighteen patients (8%) had a history of trauma to affected ear and 51 patients (21.8%) were diagnosed with diabetes.
The aetiological microbial organisms for ear discharge in our study are given in Figure 3. Pseudomonas species (29.5%, n = 69 positive cultures) was the commonest microbial organism to cause ear discharge, followed by Staphylococcal (20.5%; n = 48 positive cultures) and Coliform (16.7%; n = 39 positive cultures) species.
Figure 3. Aetiological micro-organisms by culture. (%).
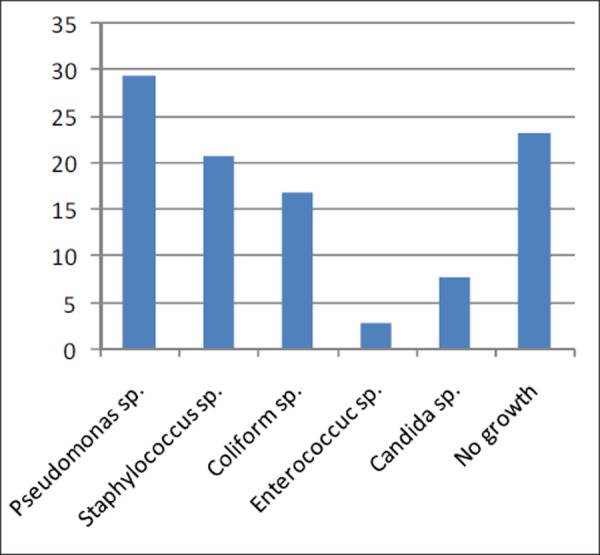
Among the fungal agents, Candida (7.7%; n = 18 positive cultures) had been the commonest organism to be detected in ear discharge. 23.1% of the cultures did not reveal any microbiological agent.
The analysis of the effect of the demographic factors in the diagnosis of CSOM revealed no significant associations between age and gender groups with CSOM (p>0.05). However, CSOM was less common among elderly patients compared to other age groups and females appeared to be less commonly affected compared to males.
Discussion
Demographic variables such as gender or age groups from 11 – 60 yrs. did not seem to affect the disease prevalence significantly, although CSOM was less common among elderly.
In our study it was evident that, the commonest aetiological agents for CSOM were Pseudomonas species followed by Staphylococci and Coliforms respectively. This contrasts with another study carried out in the tropics,17 in which the most common causal organisms isolated in patients with discharging ears were Staphylococcus aureus (44%), with 8.9% being MRSA (methicillin-resistant Staphylococcus aureus). Pseudomonas aeruginosa (39%) was the next most common organism followed by Streptococcus sp. (4.6%). Together Staphylococcus aureus and Pseudomonas aeruginosa made up 83% of the total organisms.
In the same study17 the age of patients ranged from one month to 71 years, with the most commonly affected age group being 15–25 years (33%). Males outnumbered the females by 2.3:1 and these differences were found to be significant.
In our study, although it is noted that patients under 10 years of age were excluded, no age group was at a statistically significant risk for developing CSOM. Though males (55.1%) were more commonly affected than female patients (44.9%), the difference observed was not statistically significant (SND =1.27, p>0.05).
In our study it was evident that 23.1% of the cultures did not yield any microbial growths. Effectiveness of prior empirical antibiotic therapy, poor techniques of obtaining the ear swabs and sending swabs for cultures when the diagnosis is uncertain may account for this finding.
The finding from this study that 8% of the sample had a prior history of trauma and 21.8% had diabetes suggests a need to further research the risk factors for CSOM among the same population.
Little is known of the aetiology, serotypes or susceptibility of the pathogens causing non-resolving CSOM in patients receiving care from specialists in private practice in developed or in developing countries. In a study carried out for this purpose18, Streptococcus pneumoniae was found to be the most common pathogen (35 positive cultures), followed by Haemophilus influenzae (n = 9), Staphylococcus aureus (n = 6), Moraxella catarrhalis (n = 2), Streptococcus pyogenes (n = 2) and Pseudomonas aeruginosa (n = 1).
In another study19 of immunosuppressed patients, the prevalence of the common pathogens was similar among HIV-infected and non-infected children (56.5% vs. 54.9% of the ears). However, Staphylococcus aureus was significantly more frequent in severely immunosuppressed patients.
Conclusion
The commonest aetiological agents for CSOM were identified as Pseudomonas species followed by Staphylococci and Coliforms. Demographic variables such as gender or age groups from 11 – 60 yrs. did not seem to affect the disease prevalence significantly, although CSOM was less common among elderly and women. Observations regarding the aetiological and demographic factors differed from findings from other countries in the tropical regions.
This paper has been presented at the following academic sessions.
8th Annual academic sessions of the College of Otorhino Laryngologists and head and neck surgeons of Sri Lanka. 2010.
ACKNOWLEDGEMENTS
Nil
Footnotes
PEER REVIEW
Not commissioned, externally peer reviewed
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
Nil
Please cite this paper as: Dayasena RP, Dayasiri MBKC, Jayasuriya C, Perera DSC; Aetiological agents in chronic suppurative otitis media in Sri Lanka. AMJ 2011, 4, 2, 101-4 Doi: http://dx.doi.org/10.4066/AMJ.2011.549
References
- 1.Homoe P.. Otitis media in Greenland. Studies on historical,epidemiological, microbiological, and immunological aspects. Int J Circumpolar Health. 2001;60((suppl 2)):1–54. [PubMed] [Google Scholar]
- 2.Tos M.. Sequelae of secretory otitis media and the relationship to chronic suppurative otitis media. Ann Otol Rhinol Laryngol. 1990;99:18–9. [Google Scholar]
- 3.Daly KA, Hunter LL, Levine SC. et al. Relationships between otitis media sequelae and age. Laryngoscope. 1998;108:1306–10. doi: 10.1097/00005537-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Verhoeff M, Van der V, Rovers MM, Sanders EA, Schilder AG. Chronic suppurative otitis media: A review. International Journal of Pediatric Otorhinolaryngology. 2006;70:1–12. doi: 10.1016/j.ijporl.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Leach AJ, Morris P.S.. Antibiotics for the prevention of acute and chronic suppurative otitis media in children. Cochrane Database of Systematic Reviews. 2006;(4) doi: 10.1002/14651858.CD004401.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okeowo PA. Observation on the incidence of secretory otitis media in Nigeria. J Tropic Paediatr. 1985;31:295–8. doi: 10.1093/tropej/31.6.295. [DOI] [PubMed] [Google Scholar]
- 7.Olusanya BO, Okolo AA, Ijaduola GTA. The hearing profile of Nigerian school children. Int J Paediatr Otorhinolaryngol. 2000;55(3):173–9. doi: 10.1016/s0165-5876(00)00393-1. [DOI] [PubMed] [Google Scholar]
- 8.Mcpherson B, Holborow CA. A study of deafness in West Africa: the Gambian Hearing Health Project. Int. J Pediatr Otorhinolaryngol. 1985;10:115–135. doi: 10.1016/s0165-5876(85)80024-0. [DOI] [PubMed] [Google Scholar]
- 9.Ogisi FO. Impedance screening for otitis media with effusion in Nigerian children. J.L.O. 1988;102:986–8. doi: 10.1017/s0022215100107078. [DOI] [PubMed] [Google Scholar]
- 10.Amedofu GK, Opoku-Buabeng J, Ose-Bagyina A, Antwi B.. Hearing loss among school children in Ghana. Ghana Med J. 2003;37(4):148–52. [Google Scholar]
- 11.Seely DR, Gloyd SS, Wright ADO. Hearing loss prevalence and risk factors among Sierra Leonian children. Arch Otolaryngol. H & S Surg. 1995121:853–8. doi: 10.1001/archotol.1995.01890080023004. [DOI] [PubMed] [Google Scholar]
- 12.Berman S.. Otitis media in developing countries. Paediatrics. 1995;96(1):126–31. [PubMed] [Google Scholar]
- 13.Okafor B.C. The chronic discharging ear in Nigeria. JLO. 1984;98:113–9. doi: 10.1017/s0022215100146298. [DOI] [PubMed] [Google Scholar]
- 14.Brobby GW. Peculiarities of middle ear infections in Ghana. Ghana Med J. 1988;22(3):68–73. [Google Scholar]
- 15.Lasisi OA, Nwaorgu OGB, Grandawa HI, Isa A.. A fifteen year review of otologic surgery in Ibadan, Nigeria: Problems and prospects. Nig J Surg Research. 2002;4(1–2):45–9. [Google Scholar]
- 16.Lasisi AO.. The Chronic Discharging Ear in The Subsaharan Africa-Need For Improved Management. The Internet Journal of Otorhinolaryngology. 2008;7(2) [Google Scholar]
- 17.Ahmed B, Hydri AS, Afridi AAK, Ejaz A, Farooq S, Zaidi SK.. Microbiology of ear discharge in Quetta. J Coll Physicians Surg Pak Sep. 2005;15(9):58–34. [PubMed] [Google Scholar]
- 18.Huebner RE, Wasas AS, Hockman M, Klugman KP. Bacterial aetiology of non-resolving otitis media in South African children. Journal of Laryngology & Otology. 2003;117(3):169–72. doi: 10.1258/002221503321192430. [DOI] [PubMed] [Google Scholar]
- 19.Marchisio P, Principi N, Sorella S, Sala E, Tornaghi R.. Etiology of acute otitis media in human immunodeficiency virus-infected children. The Pediatric Infectious Disease Journal. 1996 Jan;15(1):58–61. doi: 10.1097/00006454-199601000-00013. [DOI] [PubMed] [Google Scholar]


