Abstract
In the existing system of medical education in India, students are exposed to the hospital environment only after they start their clinical years of training. Hence, during the preclinical phase of their training most students are unaware of the relevance of basic sciences to clinical medicine. The preclinical student needs to be made aware of the relevance of basic sciences in clinical practice as early as possible during their training period.
In an attempt to achieve the above-mentioned goals, the first year medical students in a private medical school in India were exposed to a ‘clinical observership’ programme. This observership, spread over a period of eight weeks took the students by rotation through eight clinical disciplines wherein they observed the activities in these clinics and interacted with the consultants, laboratory personnel and patients. The programme was designed to introduce them to hospital scenarios and to impress upon them the fact that the basic sciences form the foundation for their clinical training. It was highly appreciated by the students, who found it very useful, interesting and motivating in its contents and delivery. A project of this nature requires careful planning, and calls for co-operation of the teachers in basic sciences, clinical consultants and administrators to make a success of such an effort. In the light of this experience and taking into account the promising educational value of such a programme, it is suggested that similar innovations may be incorporated into the academic schedule to make the preclinical training interesting, motivating and meaningful to a student who is at the threshold of being moulded into a physician.
Keywords: Preclinical students, clinical observership, clinical relevance, motivating innovative programmes, affective domain
Introduction
Graduate medical education in India extends for a period of four and half years which is followed by a year of compulsory rotating residential internship (CRRI) training, after which these graduates with an MBBS degree are qualified to practice medicine. Students enter the medical course after completing 12 years of secondary school education and fulfilling the entry requirements for the professional course. The four and half years of the medical course is divided into three phases; one year of preclinical training is followed by 18 months of instruction in paraclinical subjects and this is followed by two years of intense clinical training.
Even though there is great divergence in teaching methods amongst the various medical schools within India, in most of the medical schools, gross anatomy is taught through didactic lectures on regional anatomy and cadaver dissections, supplemented by instructions through medical images. Following the guidelines provided by the Medical Council of India, selected topics are also reinforced through integrated teaching. Instructions in physiology and biochemistry also follow a similar pattern. During the first phase of their professional career, students do not get the opportunity to understand categorically why they have to study volumes of basic science facts in the process of becoming a physician even though the faculties in basic sciences do place emphasis on the practical significance of the material learnt in the classrooms and laboratories.
It is felt that direct exposure to clinical scenarios will be a definite advantage for students to effectively learn the basic sciences and hence there is a need to introduce them to the hospital environment from the beginning of medical training.
Even though medical educationists globally have shown great concern over the trend of reducing preclinical teaching time,1,2,3 unfortunately, some other important issues which could adversely affect the quality of medical education do not seem to have been addressed effectively. Creating an awareness of clinical relevance of concepts in basic sciences (dealt with during the initial phase of undergraduate medical training) is one such major issue requiring the attention of the educationists. Most of these medical schools seem to follow a strict conventional system of basic sciences programmes.
It is important to steer students into the correct path of learning, to guide them to use the available resources profitably and to inculcate in them the healthy habit of selfdirected learning. The young medical student at the threshold of training needs to be very clear in his mind about his responsibilities as a medical student and the possible challenges that he may have to face in this arduous journey. The need of the hour seems to be ‘innovations’ in medical education, bringing in programmes which will develop the student’s ability to appreciate the value of applying the concepts of basic sciences into clinical practice. It is important that the preclinical teaching includes learning modules that are strong enough to motivate the students, clear enough to guide the student in the proper direction and friendly enough for the student to actively participate in them without inhibitions. This will enable the student to inculcate the available knowledge, develop the habit of self-enquiry, master the required skills and develop the correct attitude towards the patients.
The present programme was designed to address the above-mentioned issues. It was developed over a period of four years in a self-financing medical school in India and its final version is presented here.
The programme
The first year MBBS class was divided into eight groups of 12 to 13 students in each group. Arrangements were made for each of these groups to rotate through the following eight departments, spending an afternoon in each of them. The departments selected were: the echocardiography laboratory; cardiac catheterisation laboratory; gastroenterology; imaging sciences - X-rays and ultrasonography; imaging sciences - CT scans; nephrology; pulmonology; and transfusion medicine. Students visited each of these departments, weekly for eight consecutive weeks. Students were asked to keenly observe the activities in these clinics and to interact with the faculty during their visit. They were encouraged to arrange follow-up sessions with the clinical consultants, whenever possible. During the final session of interaction with the entire class, they shared their ‘hospital experiences’ with classmates and peers.
Activities in the clinics
Medical imaging: X-ray and ultrasonography: The students observed the process of taking routine plain X-rays of the chest, abdomen and the joints and the contrast procedures for GIT. They watched the procedure of ultrasonography of the abdomen in patients referred from surgery and obstetrics. In antenatal patients, they had the opportunity to visualise the foetus during different trimesters of pregnancy and the procedure of screening for congenital anomalies.
Medical imaging: CT scans: Students witnessed patients undergoing whole body CT scans and observed the resultant axial CT images. This exercise gave them the benefit of understanding three-dimensional spatial anatomy brought out by this procedure and the relevance of CT scans in clinical medicine.
Cardiac catheterisation laboratory: Students watched interventions like angiography and angioplasty. They appreciated the anatomical principles underlying these diagnostic procedures and were able to see both normal coronary arteries as well as narrowed arterial channels in different patients. These procedures gave them the opportunity to observe the dynamic anatomy of the coronary arteries.
Echocardiography: Students witnessed the basic physiological parameters being used to evaluate the functioning of the heart in the patients. This procedure helped students to understand the normal pumping function of the heart, the dynamics of cardiac blood flow and the working of the heart valves. They were also able to observe alterations in these functions.
Gastroenterology: Students had the chance to visualise endoscopy of upper and lower gastrointestinal tracts during their visit to this department. They appreciated the normal endoscopic appearance of the stomach, duodenum, colon, rectum and anal canal. They could also see the morphological changes that occur in some pathological conditions. These comparative views gave the students the chance to appreciate the normal appearance of the interior of these organs in health. A few of the ‘lucky’ batches had the chance to witness ERCP (Endoscopic retrograde cholangio pancreatography) as well, which gave them an insight into the pancreatic duct system and the extra hepatic biliary tree.
Nephrology: This observership helped students to understand the application of renal physiology in the practice of nephrology. The students were able to observe patients with electrolyte abnormalities and acid base imbalances. They were exposed to interpreting relevant laboratory data and were also able to observe patients undergoing dialysis.
Pulmonology: The students observed evaluation of patients with respiratory problems. The students saw procedures like spirometry and a few of them were also able to see bronchoscopy being performed. They were able to appreciate the application of respiratory physiology in this clinic.
Transfusion medicine and haematology laboratories: The students witnessed the procedure of blood donation, subsequent processing of blood into its components and the protocol involved in transfusing a patient. Here again, the students were able to observe the practical application of immunohaematology and laboratory haematology to the practice of medicine. Moreover, many of the students are blood donors and the visit to this department made them realise what happens to the blood they donate. Interactions with the relatives of the patients motivated a few of the students to volunteer for blood donation.
Feedback
Feedback was taken from the students in the format shown in Table 1.
Table 1. Summary of students' response.
| 1 | Was the programme beneficial to you in your learning process? | Yes (94) | No (Nil) | |||
| 1:not at all, 2: fairly well; 3:well; 4: very well; 5:excellently well | 1 | 2 | 3 | 4 | 5 | |
| 2 | How will you rate the impact the programme had on you as far as appreciating the relevance of basic sciences to clinical medicine is concerned? | − | 02 | 04 | 16 | 72 |
| 3 | How well did the programme help you in appreciating the general attitude of the patients whom you had the opportunity of interacting with during the 'clinical observership'? | − | 08 | 08 | 17 | 61 |
| 4 | Desirability of repeating the programme in the coming years | |||||
| Desirable (94) | Not desirable (Nil) | |||||
| 5 | Comment on the general nature,organization and structure of the programme. •(Responses have been discussed in the text) |
|||||
In total 94 students completed the feedback, giving a response rate of 94%. Eighty-two of these students also came for informal interviews which gave them the platform to provide more insight into their experiences of the programme.
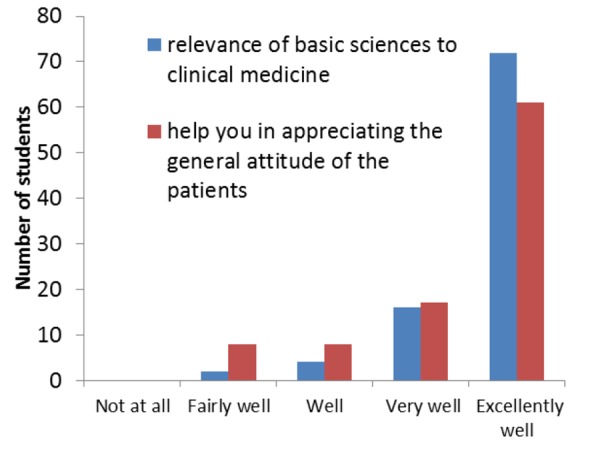
Students felt the positive impact of the programme in appreciating the relevance of basic sciences to clinical medicine as revealed by the feedback (median and mode responses were both “excellently well”- Fig 1). This also helped to create a sense of empathy in the minds of the students towards patients, thus contributing to the affective domain of learning (median and mode responses were both “excellently well”- Fig 1).
Most of the qualitative comments were of a general nature, reflecting their appreciation for the opportunity given to them for the hospital experiences, and appreciating the pains taken to organise the unique learning module. Some of them had which brought out the fact that they had the chance to appreciate the patients’ attitudes during their visits.
This was followed by interviews with students (82%) who volunteered to talk about the programme. All the students appreciated this observership for its content and delivery. They seemed to have been made aware of the implications of the extensive preclinical course content. The programme enlightened them on the role of the diagnostic specialties, many of which were new to most of the students. The interviews with the students brought out the fact that by the end of these visits, most had developed a sense of belonging to the hospital fraternity. Hospital visits became very popular with the class as a whole and they felt that these were sessions of active learning, and stood in contrast to the conventional stream of teaching sessions they were used to
Figure 1. Students' rating of the programme.
Many of them felt that this observership could be extended throughout the year and include more clinical specialties. The students were also unanimous in their opinion that it should be continued in the subsequent years.
Discussion
In India, students enter medical college, at the age of 18, which is in sharp contrast to many other countries where graduation is a prerequisite to start medical education. At the time when they start their studies in a medical school, most are too young to understand the responsibility they have taken up.
During the preclinical year, students have most of their training in classrooms and laboratories which are quite often alienated from the teaching hospitals. For most of them, classes feel like an extension of the biology programmes, which they had in the secondary schools. The only difference they feel about these sessions is the presence of cadavers in gross anatomy laboratories, which make them realise that they are in a medical school. They do not get to sense the atmosphere of the ‘hospital’ and quite often, do not understand why they are asked to learn seemingly large volumes of anatomical details and eventually resort to rote memory in learning the course content for scoring in the examinations. This stands out conspicuously as a deterrent to the general philosophy of education where the stress needs to be on developing the ability to apply basic concepts that students learn in preclinical sciences and not the mastery of memorising factual details. Conventional methods seem to fail in motivating them well enough to learn the basic principles in an effective way such that what is learnt is retained for use during their clinical years of training and thereafter. All the above flaws seen in the medical curricula of many medical schools, warrants innovations to be drafted into the teaching techniques, to transform it into a student-oriented system which will help to achieve the goals of medical education.
The current programme of clinical observership has helped to address the above-mentioned issues of the students to achieve the desired effects. The programme has helped to steer the students in the proper direction of ‘learning to retain’ rather than to memorise a seemingly unrelated plethora of information. This ‘clinical observership’ has helped them to sort out in their minds ‘why’ they need to study the amount of basic sciences they are required to learn during their coursework in the preclinical years, and more importantly to consider the clinical years of training as a continuum of preclinical training. It is true that once the student is convinced about the logical reasoning behind an academic exercise, he will pursue the training with the correct spirit.
Many of the students during their preclinical training period are ignorant of the variety of fields of specialisations available for a young doctor. Counselling for a professional career, done in a few medical schools, is usually taken up during the CRRI training period when the young qualifying doctors are busy preparing to take up the ‘postgraduate entrance examinations’ in an effort to get into the much desired residency programmes (post graduation). It would indeed be better if career options are provided earlier during the professional training. This programme has shown students the areas available for specialisation, the challenges they offer and the attached responsibilities. The influence of technological advances in the medical field has resulted in newer specialties emerging as a result of the hybridisation of earlier disciplines. The challenges offered by these new areas could be inviting and could prove to be attractive for young medical students. Interventional cardiology and interventional radiology are relatively newly evolved specialties, which the students had a chance to learn about during this observership. This programme has, therefore, helped many young medical students to identify specialising areas early in their career.
It is generally accepted that the most difficult domain to impart training to is the affective domain.4,5 Probably, the most significant role this programme has been instrumental in developing is the fact that it has helped the students to build up a sense of empathy towards the patients and their relatives. This could be interpreted as a sequel to observing the interaction of the consultants and hospital personnel towards the patients. This, in turn, has made them realise some of the essential qualities they need to imbibe to be an efficient doctor. It is highly desirable to have this aspect built into the personality of a doctor in the making early in his career. All of these amount to developing professionalism in medicine, a highly desirable personality trait in a medical student. The regular hospital visits for a period of eight weeks have contributed tremendously in shifting the paradigm of the students towards developing a sense of empathy in their minds towards patients and their families.
The departments selected for this programme are those where the students do not usually get posted during their CRRI training. In this regard, the ‘clinical observership’ becomes a unique programme wherein students get the chance to get exposed to the specialties, which they otherwise would not have appreciated during their undergraduate medical career.
It is worthwhile noting the fact that this programme or a similar one which aims to prepare students better for a clinical career has to have clinical consultants willing to participate, co-operation between the basic sciences faculty and hospital administration and consent of the preclinical programme coordinators to let the students off for this non-formal instructional exercise from their strict academic time schedule.
Interviews with the students revealed that this endeavour has succeeded in instilling professionalism in their behaviour and more importantly they seem to have developed the much- needed sense of involvement in what they have taken up in their lives. This is in conformation to the old Chinese adage ‘Tell me, I forget. Show me, I may remember. Involve me and I’ll understand’. It is important for the medical educationists to ensure that the student gets involved in whatever he is meant to be doing and the present programme has been able to achieve this goal.
The clinical observership programme, though designed for and implemented in an Indian medical educational scenario, could prove to be a desirable adjunct to the initial stages of medical training in any other country, since it has tried to address a group of issues, which are concerned with motivation, logical reasoning, self- directed approaches to learning issues, and creating a desirable paradigm shift in the mindset of the young medical student, all of which are requirements in the global medical education scenario.
ACKNOWLEDGEMENTS
The authors wish to thank the clinical consultants, colleagues in basic sciences and the college and hospital administration; PSG Institute of Medical Sciences & Research, Coimbatore; India for their support in conducting this programme.
The authors acknowledge the help of Dr. Mark Norrish, Associate Professor of Behavioural Sciences, Oman Medical College, Sohar; Sultanate of Oman in the analysis of the data.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
Please cite this paper as: Kumar PA and Kumar PN. Clinical observership: A desirable adjunct to preclinical training. AMJ 2011, 4, 6, 294-299 http//dx.doi.org/10.4066/AMJ.2011.836
References
- 1.Reidenberg JS, Laitman JT. The new face of gross anatomy. Anat Rec. 2002;269:341–43. doi: 10.1002/ar.10076. [DOI] [PubMed] [Google Scholar]
- 2.Older J. Anatomy: A must for teaching the next generation. Surgeon. 2004;2(2):79–90. doi: 10.1016/s1479-666x(04)80050-7. [DOI] [PubMed] [Google Scholar]
- 3.Mclachlan JC, Patten D. Anatomy teaching: ghosts of the past, present and future. Med Educ. 2006;40(3):243–53. doi: 10.1111/j.1365-2929.2006.02401.x. [DOI] [PubMed] [Google Scholar]
- 4.Ross JM, Stanley IM. A system of affective learning behaviors for medical education. Family Practice. 1985;2(4):213–218. doi: 10.1093/fampra/2.4.213. [DOI] [PubMed] [Google Scholar]
- 5.Amin Z, Eng KH. 2. Singapore: World Scientific Publishing Co Pvt Ltd; 2009. Basics in medical education; pp. 76–77. [Google Scholar]


