Abstract
Objective To assess the risk of adverse perinatal events of vaccination of pregnant women with an MF59 adjuvanted vaccine.
Design Cross sectional multicentre study.
Setting 49 public hospitals in major cities in Argentina, from September 2010 to May 2011.
Participants 30 448 mothers (7293 vaccinated) and their 30 769 newborns.
Main outcome measure Primary composite outcome of low birth weight, preterm delivery, or fetal or early neonatal death up to seven days postpartum.
Results Vaccinated women had a lower risk of the primary composite outcome (7.0% (n=513) v 9.3% (n=2160); adjusted odds ratio 0.80, 95% confidence interval 0.72 to 0.89). The propensity score analysis showed similar results. Adjusted odds ratios for vaccinated women were 0.74 (0.65 to 0.83) for low birth weight, 0.79 (0.69 to 0.90) for preterm delivery, and 0.68 (0.42 to 1.06) for perinatal mortality. These findings were consistent in further subgroup analysis. No significant differences in maternal outcomes were found.
Conclusion This large study using primary data collection found that MF59 adjuvanted A/H1N1 influenza vaccine did not result in an increased risk of adverse perinatal events and suggested a lower risk among vaccinated women. These findings should contribute to inform stakeholders and decision makers on the prescription of vaccination against influenza A/H1N1 in pregnant women.
Introduction
Each year pandemic influenza viruses cause large number of deaths and increased morbidity worldwide. On 11 June 2009, the World Health Organization (WHO) signalled that a global pandemic of 2009 H1N1 influenza was under way.1 This outbreak was associated with higher morbidity in the United States and the southern hemisphere than elsewhere.2 3 4 This pandemic affected mainly young adults, and pregnant women were a specific vulnerable group.5 6 As in previous influenza pandemics of 1918-19 and 1957-58, several studies showed the effect of infection with 2009 H1N1 influenza among pregnant women,7 8 9 10 which resulted in increased hospital admission rates, severe illness, disproportionate mortality, and adverse perinatal outcomes, raising perinatal mortality and preterm delivery rates by up to four times.11 12 13 14 15 16 For these reasons, vaccination against influenza is considered an essential element of prenatal care. In addition, vaccination during pregnancy is beneficial for protecting infants against acquiring the infection and is effective in preventing admission of infants to hospital due to influenza in the first six months of life.17 18 19 20
Owing to expected limitations in supplies of pandemic vaccine, the WHO encouraged the development of adjuvanted vaccines,21 as a mean of improving immunogenicity of vaccine through different mechanisms such as prolonging the exposure time of antigen or direct stimulation of the immune response. Focetria (Novartis) is an inactivated virus (A/California/7/2009 (H1 N1) surface antigens) vaccine, containing MF59C as the adjuvant. An influenza vaccine using MF59 as adjuvant has been available since 1997, and serious specific secondary events have not been detected.
Data on the use of MF59 in pregnant women are scarce. Teratogenicity and postnatal disorders were not observed in studies in animals. Limited evidence available in clinical database records shows no increased risk, including in abortion rates.22 23 Safety reports have not shown a higher than expected number of adverse events but concluded that larger studies were needed to arrive at stronger conclusions about the risks associated with exposure to influenza vaccines using MF59 adjuvant during pregnancy.24 25 26 27 28 29 Despite somewhat reassuring evidence, the uptake of H1N1 specific influenza vaccine in pregnant women has been poor in several countries as a result of uncertainty, among both women and physicians, about the safety of the vaccine in pregnancy.30 31 32 33 34 35
The effect of the 2009 influenza pandemic was particularly relevant to pregnant women and children in Argentina.36 Of the 410 maternal deaths in Argentina, 95 (23%) were due to respiratory diseases, with more than half of them resulting from acute respiratory infections.37 Likewise, paediatric death rates for seasonal influenza were 10 times higher than in previous years in paediatric hospitals in Argentina.38
Following the 2009 epidemic, vaccination was considered a priority and a potentially cost effective strategy to prevent the consequences of influenza A/H1N1. The influenza season in the southern hemisphere is usually from April/May through September, peaking around mid-June-July. From February to November 2010, the Argentinean Ministry of Health launched a national immunisation programme that included pregnant women, among other risk groups. Although other influenza A/H1N1 vaccines were also available in the private market, the programme used only a single dose of the inactivated virus MF59 adjuvanted vaccine (Focetria). The recommendation was that all pregnant women should be vaccinated at any point during gestation or puerperium during the influenza season.39 40 41 42 43
This immunisation programme offered vaccine coverage to all the subgroups at risk of influenza, including pregnant women, seen in all public hospitals or primary care centres in the country. No specific selection process for vaccination took place at the centres. All pregnant women seen at public centres could receive the vaccine offered to them by the health professionals and accepted by the women or their legal guardians.
In the context of this campaign, the aim of this study was to evaluate the association of influenza A/H1N1 MF59 adjuvanted vaccine with the occurrence of major adverse perinatal outcomes. Our primary objective was to compare the occurrence of perinatal outcomes in mothers and children between pregnant women vaccinated with monovalent MF59 adjuvanted influenza A/H1N1 and a non-vaccinated group. Secondary objectives were to evaluate the association between monovalent MF59 adjuvanted influenza A/H1N1 vaccine and risk of perinatal events in subgroups defined by exposure status and baseline risk of adverse events.
Methods
This was a large multicentre study to evaluate the association of influenza A/H1N1 MF59 adjuvanted vaccine (Focetria) with the occurrence of major adverse perinatal outcomes.
Setting and population
This study was carried out in 49 hospitals in the public healthcare sector in major cities of Argentina assisting an average of 113 000 deliveries annually (nearly 15% of overall live births in Argentina), the vast majority in women of low socioeconomic status. Participating hospitals included those belonging to the Buenos Aires Metropolitan Area (AMBA) Perinatal Network (n=26) and other public hospitals from the province of Buenos Aires, Mendoza, Rosario, and Entre Rios. All hospitals provide comprehensive obstetric care, including immunisations, and pre-graduate and postgraduate training in obstetrics and gynaecology.
A consecutive sample of all women who delivered their children from September 2010 to May 2011 at the participating institutions was eligible to participate. They were invited to participate during their postpartum hospital stay, if they had either a liveborn or a stillborn infant of at least 22 weeks’ gestation or weighing at least 500 g at birth. They were excluded only if they could not be questioned owing to language barriers.
Eligible women were asked to sign an informed consent form, after which a trained interviewer extracted data from the medical record regarding maternal characteristics, evolution of the index pregnancy and delivery, and status of the newborn. Participants then completed a brief survey to complement the information. We collected data on both mother and newborn up to day seven after delivery. Mothers and newborns discharged before day seven were contacted by telephone at day seven to check their health status. During the data collection period, a supervisory team visited the participating hospitals weekly to collect and check completion of the forms and to check the quality of the information by reviewing the birth record and clinical record. Two field supervisors reviewed all forms before information was entered in the database. To monitor the quality of the data, the study steering committee appointed an independent team. In a random subsample of 20% of study participants, the information of the case reports forms was checked against the clinical records.
Exposure measurements
We defined the exposed group as women who received the influenza A/H1N1 MF59 adjuvanted vaccine during their pregnancy. We defined the exposure status and vaccination date on the basis of documentation of the vaccine application in any official registry: vaccination chart, hospital vaccine registries, or centralised registry from the Ministry of Health if available. We defined the non-exposed group as non-vaccinated pregnant women.
A subgroup of women existed who reported having received the H1N1 monovalent vaccine but for whom no official record or documentation was available. We evaluated this subgroup initially to assess any systematic difference from the exposed or non-exposed group as defined in the protocol. We did the analysis by comparing the exposed and non-exposed groups with scenarios both including and excluding this subgroup.
Outcome measurement and definitions
The primary endpoint was a composite outcome combining the occurrence of either low birth weight, preterm delivery, or fetal or early neonatal death up to seven days postpartum. We defined preterm delivery as a newborn with a gestational age of less than 37 weeks according to physical examination at birth, low birth weight as a newborn weighing less than 2500 g, and very low birth weight as a newborn weighing less than 1500 g.
Perinatal secondary outcomes
We defined congenital malformations as a newborn presenting with alterations in anatomical development occurring during intrauterine life and diagnosed during gestation or by physical examination within the first seven days after birth. We defined early neonatal mortality as death of a newborn within seven days after birth, fetal mortality as intrauterine death of the fetus in a pregnancy over 22 weeks, and perinatal mortality as early neonatal mortality plus fetal mortality. We defined low Apgar scores at five minutes as a newborn presenting with an Apgar score of less than 7 at five minutes. We defined admission to neonatal intensive care as admission of a newborn to the intensive care unit for a period longer than 48 hours.
Maternal secondary outcomes
Maternal secondary outcomes included haemorrhage during pregnancy (first, second, or third trimester), delivery, and postpartum; admission to intensive care; hospital admission during pregnancy; hypertensive disorders (pregnancy induced hypertension, pre-eclampsia, and eclampsia); and maternal death up to day seven postpartum.
Statistical analysis and data reporting
On the basis of statistics and data from the public hospital network, we assumed an overall incidence of 11% for the primary endpoint in the reference group (non-vaccinated women).44 For a one to two ratio between exposed and non-exposed women and 90% power to detect an absolute effect size of 1.5%, the estimated sample size was approximately 24 000 women. As small variations in both the final proportion of events in each group and the ratio between exposed and non-exposed women might alter this estimated sample size, we decided to recruit 30 000 women to maintain the original power estimation.
We report demographic and clinical characteristics defined by the exposure status. We estimated crude prevalence of events per group (with 95% confidence interval) and crude prevalence rate ratios for all comparisons. To evaluate differences between groups, we did bi-variable analysis by using t tests for independent samples or Wilcoxon rank tests for continuous variables according to the distribution and χ2 tests for categorical variables.
Multivariable analysis
To evaluate the independent association between exposure to vaccine and outcomes, adjusting for potential confounders, we used two main approaches: multiple logistic regression analysis and propensity score analysis.
Logistic regression analysis
After assessing the association of several covariates with both the exposure of interest and the outcome, we entered those potential confounders one by one into the model already containing the monovalent MF59 vaccine. We retained variables that changed the crude estimated effect of the vaccine on the outcome by at least 10% in the final model as confounders (number of antenatal visits, maternal age, and smoking). We considered others, such as educational and income level and parity, although the change was between 5% and 10%, on the basis of the bivariate association with both exposure and outcome and their clinical and or epidemiological significance.
Propensity score analysis
The propensity score is used to adjust for group differences and reduce confounding bias in observational studies when the exposure of interest is an intervention that has not been randomly assigned among the participants. We anticipated that vaccinated women would be systematically different from the unvaccinated group in various characteristics and that the probability of receiving the vaccine would be associated with these factors. Therefore, we estimated the probability of vaccination as a function of those variables and used that score as a single matching covariate by using a propensity score analysis. Variables included in the model were nationality; antenatal visits; educational level; income level; parity; history of hypertension, pre-eclampsia, or stillbirth; and alcohol consumption. To match exposed and unexposed women by strata of propensity score, we used a sub-classification based on fifths of estimated propensity scores, forming groups of units with similar propensity scores and similar covariate distributions. We also matched exposed and unexposed women by using one of the stratification procedures used for estimating the propensity score. Once the balancing property of the covariates was satisfied in each of the eight blocks defined by this procedure, we could consider the assignment to treatment as approximately random. This procedure used 7227 vaccinated and 22 909 non-vaccinated women, leaving less than 300 non-matches out of the analysis. Using fifths of estimated propensity score or the eight blocks of the stratification procedure yielded essentially the same results, so we decided to enter the score in the model as a five level dummy variable, in both fifths of probability of vaccination and range of probability, from 0-10% to >40% for the adjustment using conventional logistic regression.
Sensitivity analysis
Finally, we did a series of sensitivity analyses to explore different scenarios in the definition of exposure status and comparison groups and possible interactions of the effect of MF59 adjuvanted vaccine on adverse perinatal outcomes in different risk subgroups. We defined exposure status per protocol as women with documented MF59 adjuvanted vaccination. In the first alternative scenario, we considered as exposed both women defined per protocol and those who reported having received the H1N1 monovalent vaccine but for whom no official record or documentation was available. The second scenario strictly compared exposed women with documented vaccination with non-vaccinated women, excluding those whose vaccination status was only self reported.
We also evaluated the association of the vaccine with adverse perinatal outcomes in subgroups at high risk on the basis of inadequate antenatal control (women who had fewer than four visits during pregnancy) or fifths of risk of perinatal events based on several risk factors such as parity, maternal age, pregnancy induced hypertension, haemorrhage during delivery, smoking status, and gestational age at first control.
Results
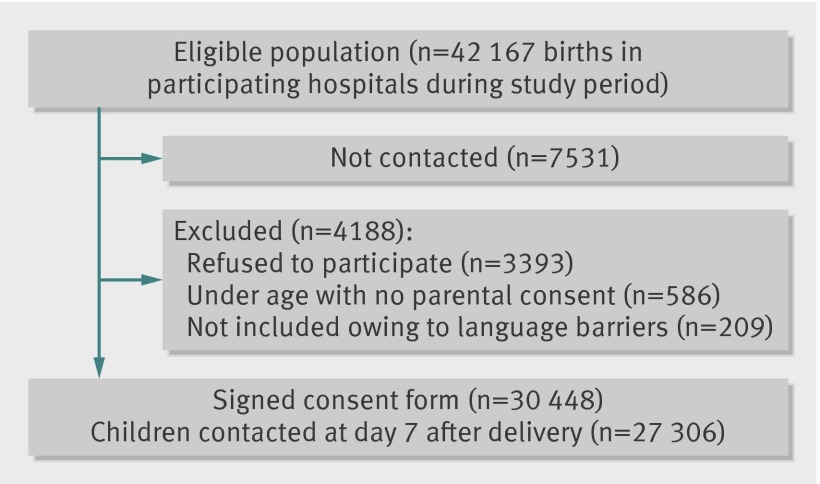
During the study period, from September 2010 to May 2011, the participating hospitals assisted 42 167 deliveries. We included 30 448 mothers and their 30 729 newborns (73% inclusion rate) and contacted 27 306 participants at day seven after delivery (88.9% follow-up) (figure). We had a local team of interviewers at each of the 49 participating hospitals, but owing to the workload at public hospitals not all women could be approached and invited to participate, although we think this phenomenon happened randomly across the different hospitals. We do not have information on vaccination status or other potential risk factors for adverse perinatal events in the 7531 women who were not approached, but their overall rate of adverse events reported by the hospitals was not different from that of women included in the study. Overall, women who refused to participate were younger and more educated, but we could not obtain data on exposure or outcomes to assess potential bias
Flow chart of study
The proportion of vaccinated women, with appropriate documentation as defined per protocol, was 24.0% (n=7293). Among them, 2874 (39.4%) received the vaccine in the first trimester, 3545 (48.6%) in the second, and 736 (10.1%) in the third; for 138 (1.9%) this was not known. In all, 27 662 (91%) women were discharged from the hospital before day seven (median 2 (interquartile range 2-3) days), and 2786 women remained in the hospital for seven or more days postpartum. Information collected at day seven by phone was mainly on complications, readmissions, or mortality of mother or child after discharge from the hospital.
Table 1 shows the distribution of selected sociodemographic and clinical characteristics and previous obstetric history of the sample among vaccinated and non-vaccinated women. On average, vaccinated women were slightly younger, had a higher educational level, and had more antenatal visits. On the other hand, vaccinated women were poorer and had fewer previous deliveries.
Table 1.
Selected baseline characteristics of participants. Values are numbers (percentages) unless stated otherwise
| Characteristic | Vaccinated H1N1 (n=7293) | Non-vaccinated H1N1 (n=23 195) |
P value |
|---|---|---|---|
| Mean (SD) maternal age (years) | 25.8 (6.2) | 26.1 (6.4) | <0.01 |
| Age group: | |||
| <19 years | 519 (7.1) | 1349 (5.8) | <0.01 |
| 19-35 years | 5935 (81.4) | 18 808 (81.1) | |
| >35 years | 839 (11.5) | 3038 (13.1) | |
| Education: | |||
| <8 years | 2216 (30.4) | 8341 (36.0) | <0.01 |
| 8-12 years | 4582 (62.8) | 13 535 (58.4) | |
| >12 years | 392 (5.4) | 904 (3.9) | |
| Foreign women | 1287 (17.6) | 5081 (21.9) | <0.01 |
| Parity: | |||
| Nulliparous | 2860 (39.2) | 7608 (32.8) | <0.01 |
| Multiparous (>3 previous deliveries ) | 1234 (16.9) | 5094 (22.0) | |
| Stable partner/married | 6528 (89.5) | 20 750 (89.5) | NS |
| Use of illicit drugs | 32 (0.4) | 134 (0.6) | NS |
| Alcohol intake | 78 (1.1) | 188 (0.8) | NS |
| Smoker | 941 (12.9) | 2863 (12.3) | NS |
| Income*: | |||
| Poverty line | 1676 (23.0) | 3652 (15.7) | <0.01 |
| Poverty line ×2 | 3548 (48.6) | 11 236 (48.4) | |
| Poverty line ×3 | 520 (7.1) | 1786 (7.7) | |
| Mean (SD) previous maternal weight: | 61.3 (19.9) | 60.9 (14.4) | NS |
| <55 kg | 2386 (32.7) | 7085 (30.5) | NS |
| 55-85 kg | 4156 (57.0) | 12 105 (52.2) | |
| >85 kg | 347 (4.8) | 1077 (4.6) | |
| Antenatal visits: | |||
| None | 49 (0.7) | 909 (3.9) | <0.01 |
| 1-4 | 1181 (16.2) | 5722 (24.7) | |
| ≥5 | 6063 (83.1) | 16 534 (71.3) | |
| Gestational age at first antenatal visit: | |||
| <14 weeks | 3422 (46.9) | 7661 (33.0) | <0.01 |
| 15-20 weeks | 1795 (24.6) | 4996 (21.5) | |
| 20-28 weeks | 971 (13.3) | 3702 (16.0) | |
| >28 weeks | 471 (6.5) | 2742 (11.8) | |
| Previous stillbirth | 203 (2.8) | 593 (2.6) | NS |
| History of hypertension | 299 (4.1) | 844 (3.6) | <0.01 |
| History of pre-eclampsia | 74 (1.0) | 166 (0.7) | <0.01 |
NS=non-significant.
*Data were missing for 1549 (21.2%) vaccinated women and 6521 (28.1%) non-vaccinated women; smaller amounts of data were missing for other characteristics.
Table 2 shows maternal and perinatal outcomes according to vaccination status. Vaccinated women had a lower risk of the primary composite outcome. They had fewer preterm births and fewer low and very low birthweight babies than did non-vaccinated women. Likewise, we saw a trend to fewer fetal, perinatal, and early neonatal deaths in vaccinated women; a lower proportion of Apgar score less than 7 at five minutes; and slightly more non-immune jaundice. We found no difference between the groups in the number of admissions to neonatal intensive care or in the occurrence of fetal malformations. Vaccinated women had slightly more hospital admissions, haemorrhage during pregnancy, and caesarean sections.
Table 2.
Main maternal and perinatal outcomes. Values are numbers (percentages) unless stated otherwise
| Vaccinated H1N1 (n=7293) | Non-vaccinated H1N1 (n=23 195) | P value | |
|---|---|---|---|
| Maternal outcomes | |||
| Hospital admission during pregnancy | 548 (7.5) | 1471 (6.3) | 0.002 |
| Pregnancy induced hypertension | 288 (3.9) | 833 (3.6) | NS |
| Pre-eclampsia | 124 (1.7) | 384 (1.7) | NS |
| Eclampsia | 16 (0.2) | 66 (0.3) | NS |
| Haemorrhage during pregnancy: | |||
| First trimester | 128 (1.8) | 278 (1.2) | 0.01 |
| Second trimester | 54 (0.7) | 134 (0.6) | |
| Third trimester | 49 (0.7) | 157 (0.7) | |
| Peripartum haemorrhage: | |||
| Antepartum | 25 (0.3) | 134 (0.6) | NS |
| Intrapartum | 12 (0.2) | 33 (0.1) | |
| Postpartum | 38 (0.5) | 92 (0.4) | |
| Maternal admission to intensive care | 17 (0.2) | 67 (0.3) | NS |
| Mode of delivery: | |||
| Vaginal | 5180 (71.0) | 16 900 (72.9) | 0.02 |
| Forceps/vacuum | 68 (0.9) | 228 (1.0) | |
| Caesarean section | 2039 (28.0) | 6022 (26.0) | |
| Perinatal outcomes | |||
| Primary composite outcome | 513 (7.0) | 2160 (9.3) | <0.01 |
| Preterm births (<37 weeks) | 354 (4.9) | 1505 (6.5) | <0.01 |
| Low birth weight | 357 (4.9) | 1606 (6.9) | <0.01 |
| Very low birth weight | 44 (0.6) | 306 (1.3) | <0.01 |
| Fetal mortality | 25 (0.3) | 111 (0.5) | 0.08 |
| Early neonatal mortality (from birth to day 7) | 29 (0.4) | 146 (0.6) | <0.01 |
| Perinatal mortality | 54 (0.7) | 257 (1.1) | <0.01 |
| Apgar score <7 at 5 minutes | 28 (0.4) | 127 (0.5) | 0.018 |
| Admission to neonatal intensive care | 433 (5.9) | 1523 (6.6) | NS |
| Fetal malformations | 35 (0.5) | 137 (0.6) | NS |
| Non-immune jaundice | 273 (3.7) | 706 (3.0) | 0.012 |
NS=non-significant.
When we analysed the different causes of admission during pregnancy, we could not find differences other than those for urinary tract infection, the most common cause. We saw no differences in hospital admissions for respiratory infections, hypertension, haemorrhage, diabetes, or other causes, although the low numbers may limit the analysis. Also, self reported bleeding during pregnancy was more common in vaccinated women (233 (3.2%) v 579 (2.5%), but we found no differences leading to admission. No association existed between vaccination status and hypertensive disorders or maternal admission to intensive care.
The association between the vaccine and the primary or secondary outcomes, including malformations, was similar when we analysed women by trimester of vaccination (data not shown), so we decided to consider vaccination as a dichotomous variable.
Table 3 shows the results of the multivariable analysis. Vaccinated women (n=7293) had a lower risk of the primary composite outcome (7.0% v 9.3%) compared with non-vaccinated women (crude odds ratio 0.74, 95% confidence interval 0.67 to 0.81). After adjustment for number of antenatal visits, educational and income levels, maternal age, smoking, parity, and history of hypertensive disorders, vaccination status was associated with a lower odds of the composite outcome (adjusted odds ratio 0.80, 0.72 to 0.89), preterm birth (0.79, 0.69 to 0.90), and low birth weight (0.74, 0.65 to 0.83). Although we found a difference in perinatal mortality, the adjusted odds ratio did not reach statistical significance (0.68, 0.42 to 1.06). In the propensity score analysis, the adjusted odds ratio for the primary outcome showed similar results (0.79, 0.71 to 0.87).
Table 3.
Crude and adjusted main perinatal outcomes in vaccinated and non-vaccinated women
| Outcome | No (%) | Odds ratio (95% CI) | Adjusted propensity score† (95% CI) | |||
|---|---|---|---|---|---|---|
| Vaccinated H1N1 (n=7293) | Non-vaccinated H1N1 (n=23 195) | Crude | Multiple logistic regression adjusted* | |||
| Preterm + low birth weight + perinatal mortality | 513 (7.0) | 2160 (9.3) | 0.74 (0.67 to 0.81) | 0.80 (0.72 to 0.89) | 0.79 (0.71 to 0.87) | |
| Preterm (<37 weeks) | 354 (4.9) | 1505 (6.5) | 0.73 (0.65 to 0.83) | 0.79 (0.69 to 0.90) | ||
| Low birth weight | 357 (4.9) | 1606 (6.9) | 0.69 (0.61 to 0.78) | 0.74 (0.65 to 0.83) | ||
| Perinatal mortality | 54 (7.4) | 257 (11.0) | 0.63 (0.46 to 0.86) | 0.68 (0.42 to 1.06) | ||
*Adjusted for number of antenatal visits, level of education, maternal age, income, parity, smoking, and history of pregnancy induced hypertension.
†Propensity score was entered in model as five level dummy variable, both in fifths of probability of vaccination and range of probability, from 0-10% to >40%.
Sensitivity analysis
Table 4 shows crude and adjusted odds ratios for the effect of vaccination on the primary perinatal outcome in pre-specified subgroups defined by exposure status or baseline risk of events. The primary analysis considered exposed women to be only those with documented MF59 adjuvanted vaccines and considered all others as non-vaccinated, including those who reported having received the vaccine but for whom no documentation was available. This last group (n=4592) behaved as an intermediate category between women with documented vaccination and those not vaccinated in relation to the number of antenatal visits and the risk of the primary event. All the different scenarios show similar results to the primary analysis: vaccination with the MF59 adjuvanted A/H1N1 influenza vaccine was associated with a lower risk of adverse perinatal events.
Table 4.
Summary of crude and adjusted results in subgroups defined by exposure status or baseline risk of events
| No (%) exposed* | No (%) non-exposed† | Event prevalence ratio (crude) (95% CI) | Adjusted odds ratio (95% CI) | |
|---|---|---|---|---|
| Exposure | ||||
| Per protocol | 7293 (23.9) | 23 195 (76.1) | 0.76 (0.69 to 0.83) | 0.80 (0.72 to 0.89) |
| Alternative analysis 1* | 11 565 (38.6) | 18 382 (61.4) | 0.79 (0.74 to 0.85) | 0.83 (0.76 to 0.91) |
| Alternative analysis 2† | 7293 (28.0) | 18 795 (72.0) | 0.74 (0.67 to 0.81) | 0.77 (0.68 to 0.86) |
| Subgroup analysis | ||||
| Prenatal control <4 | 976 (13.4) | 6319 (86.6) | 0.73 (0.61 to 0.89) | 0.76 (0.58 to 0.97) |
| Prenatal control ≥4 | 6325 (27.3) | 16 876 (72.7) | 0.88 (0.79 to 0.98) | 0.84 (0.73 to 0.95) |
| High risk fifth | 1234 (21.1) | 4605 (78.9) | 0.72 (0.62 to 0.83) | 0.62 (0.52 to 0.75) |
| Low risk | 6010 (24.6) | 18 454 (75.4) | 0.84 (0.74 to 0.94) | 0.87 (0.77 to 0.99) |
*Women with documented H1N1 vaccine plus those who reported having received H1N1 monovalent vaccine but for whom no official record or documentation was available versus non-vaccinated women.
†Women with vaccine documentation versus non-vaccinated women, excluding those whose vaccination status was only self reported.
Discussion
This study showed that adjuvanted MF59 H1N1 vaccination during pregnancy did not result in an increased risk of adverse maternal or perinatal events in a large sample of women. In fact, vaccination was associated with a lower risk of events, both in the overall study population and in the different subgroups in the sensitivity analysis. This large multicentre study was conducted in 49 hospitals across the country during the national vaccination campaign launched by the Ministry of Health in 2010. These hospitals adequately represent the public sector in Argentina, each assisting between 1000 and 7000 deliveries a year and serving a majority of low income population with lower educational level. Our results can thus be extrapolated to other groups of similar socioeconomic background in other settings.
Strengths and limitations of study
Information on exposure, outcomes of interest, and all potential confounders came directly from the participants and their medical records at the time of delivery and follow-up contact. This allowed us to consider some possible confounders, such as maternal comorbidity or personal information, not included in other large studies based on nationwide registries or large databases.16 45 However, although the vaccination preceded the delivery and, thus, the occurrence of adverse perinatal events, and we were able to collect information on a large proportion (73%) of all deliveries attended at those hospitals during the study period, this study does not allow us to suggest a causal relation between exposure to the adjuvanted vaccine and the lower risk of the different outcomes.
Selection bias could be a potential explanation for our results. Women who participated in the study signed an informed consent form after delivery and therefore had a lower probability of severe morbidity. In addition, we did not have adequate data on women admitted to intensive care, and, given the design of the study, we did not have data on those who died. Likewise, the definition of the vaccination status might have changed the results if the women who reported having received the vaccine had had better documentation or if the association between vaccination and adverse perinatal events had differed according to women’s baseline risk of events. That is why we did several pre-specified analyses considering the different definitions of exposure and risk categories defined in the protocol after completing the analysis for the whole sample. All these analyses had consistent results, showing that vaccination during pregnancy with the MF59 adjuvanted A/H1N1 influenza vaccine did not result in an increased risk of adverse perinatal events. Although this analytical approach cannot control for all residual confounding or eliminate potential selection and information biases, we believe that these consistent findings strengthen our conclusion and suggest that vaccination with MF59 adjuvanted H1N1 vaccine may be associated with a lower risk of adverse perinatal outcomes. This provides additional reassurance of the safety of adjuvanted influenza vaccines and, in particular, on the use of the MF59 A/H1N1 influenza vaccine in pregnant women. Given the concerns that have been raised on this topic, this is of utmost importance as the use of adjuvanted vaccines is critical to achieve adequate host immune responses.
Comparison with national data
Vaccinated women had a lower risk of very low birthweight (≥1500 g) babies. In our sample, the overall proportion of very low birth weight was 1.14% (n=306), consistent with the report of the annual statistics of the Ministry of Health for 2010 (1.1%).46 Likewise, vaccinated women had a lower risk of newborns under 32 weeks of gestation (0.64% (n=47) v 1.25% (n=290)).
Our study included 2874 women vaccinated during the first trimester and did not find an association between congenital malformations and vaccination status, although this comparison may have been prevented by the low number of malformations diagnosed among vaccinated women (n=35). The overall proportion of malformations in our sample was 0.56% (n=172): 0.59% (n=137) in non-vaccinated women and 0.48% (n=35) in vaccinated women. This proportion is lower than the 0.8% reported by the national perinatal information system for the country in 2010.46 This can be explained, as data on malformations included in our study are those minor and major defects diagnosed up to the seventh day by physical examination. We did not include other complementary studies or malformations diagnosed at a later time, which could explain the difference seen from other reports on the frequency of malformations.
Comparing the occurrence of the primary outcome in non-vaccinated women with national statistics for 2010, we saw a lower proportion of premature births less than 37 weeks (6.5% v 8.4%) and low birth weight (6.9% v 7.5%) and higher early neonatal mortality (6.2 v 4.0 per 1000).46
Comparison with other studies
Some recently published studies have evaluated the effect of the vaccination for H1N1 in pregnant women. A Danish study of 55 000 pregnant women based on a nationwide register based cohort studied the association of an adjuvanted inactivated AS03 pandemic A/H1N1 2009 influenza vaccine (Pandemrix; GlaxoSmithKline) with the risk of fetal death, spontaneous abortion (7-22 weeks’ gestation), and stillbirth (after 22 completed weeks’ gestation) in H1N1 vaccinated compared with unvaccinated pregnancies.45 A total of 7062 (13%) women had received the vaccine during 2009, and the researchers found no association between exposure to the H1N1 vaccine and the risk of fetal death (adjusted hazard ratio 0.79, 95% confidence interval 0.53 to 1.16) or the secondary outcomes. The authors comment about the absence of other controlled studies and that most of the information on vaccine safety in pregnant women comes from passive surveillance studies or other studies with no control groups. This study included women vaccinated at any time during pregnancy, although relatively few were vaccinated in the first trimester.47
The same authors recently published another analysis on the same register using a propensity score matched analysis to evaluate the effect of an adjuvanted influenza A/H1N1 pdm09 vaccine during pregnancy on adverse fetal outcomes, major birth defects, and small size for gestational age as primary outcomes and low birth weight and prematurity as secondary outcomes. Consistent with our findings, they reported no differences in the risk of adverse events due to the vaccine.48
Another recent study evaluated the relation between maternal H1N1 vaccination and fetal and neonatal outcomes among singleton births during the 2009-10 H1N1 pandemic, using a population based perinatal database in Ontario, Canada.49 The authors examined different perinatal outcomes (preterm birth, small for gestational age births, five minute Apgar score <7, and fetal death) and compared those events between women who did and did not receive H1N1 vaccination during pregnancy. Of the 55 570 mothers included, 23 340 (42.0%) received H1N1 vaccination. The authors considered an H1N1 vaccine alone or in combination with seasonal flu vaccine. In this study, women vaccinated during the second or third trimester were less likely to have a small for gestational age infant, preterm birth at less than 32 weeks’ gestation, and fetal death.
Finally, Heikkinen et al have recently reported the findings of a comparative cohort study that evaluated the safety of the same MF-59 adjuvanted A/H1N1 vaccine among 2295 vaccinated and 2213 unvaccinated pregnant women.50 The sample was recruited in 27 midwife practices and seven hospitals in the Netherlands, plus a small sample from two hospitals: one in Rome, Italy (n=9; 0.2%), and another in Cordoba, Argentina (n=239; 5.4%). In this study, vaccination with the MF-59 adjuvanted vaccine was not associated with any significant increase in risk of gestational diabetes, pre-eclampsia, stillbirth, low birth weight, neonatal deaths, or congenital malformations, and a significant reduction in premature births was seen in the vaccinated cohort.
Conclusions and recommendations
This large multicentre observational study showed that vaccination during pregnancy with the MF59 adjuvanted A/H1N1 influenza vaccine did not result in an increased risk of any adverse perinatal or maternal events, and, in agreement with other studies, the consistent results across different subgroups actually suggest a lower risk of events among vaccinated women. As reported by other studies, vaccine coverage in this high risk group has been relatively low. We believe that the uptake in this setting may improve if vaccination is offered through public antenatal clinics with concurrent safety education for obstetricians and vaccination providers, as well as targeted campaigns by health authorities to increase demand for vaccination by pregnant women.31 This study contributes to provide new information for both healthcare providers, especially obstetricians, and policy makers to make informed decisions about vaccination policies and increase the prescription of vaccination against influenza A/H1N1 in pregnant women.
What is already known on this topic
Influenza infection among pregnant women increases the risk of adverse events, and vaccination is considered an essential element of prenatal care
Data on the safety of MF59 adjuvanted vaccines during pregnancy are scarce
What this study adds
Vaccination during pregnancy with the MF59 adjuvanted A/H1N1 influenza vaccine did not result in an increased risk of any adverse perinatal or maternal events
Consistent results across different subgroups actually suggest a lower risk of events among vaccinated women
This study contributes to provide new information both for healthcare providers and policy makers to make informed decisions about vaccination policies
Contributors: FR and AK conceived the project, designed the study and formulated the methods, conducted the project and were project leaders, analysed and interpreted the data, wrote the first draft of the manuscript, and provided background knowledge to the data analysis and interpretation. PM coordinated the project, helped to supervise enrolment, analysed and interpreted the data, assisted in the writing and editing of the manuscript, did the literature search, and reviewed all abstracts and full text articles. AB and VW supervised enrolment, coordinated field work, interpreted the data analysis, and assisted in the writing and editing of the manuscript. AS helped to design the study and formulate the methods, interpreted the data, and assisted in the writing and editing of the manuscript. FA and APR participated in the design of the study and in the analysis and interpretation of the data and assisted in the writing and editing of the manuscript. FR is the guarantor.
Funding: This study was funded by an independent research grant from Novartis Argentina SA (Internal Protocol No V111_17TP. 2010). The investigators designed and conducted the study; performed the analysis and interpretation of the data; and are responsible for the results, conclusions, and recommendations.
Competing interests: All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: this study was funded by Novartis Argentina SA and conducted under an independent research grant to the Institute for Clinical Effectiveness and Health Policy; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study protocol was approved by the institutional review boards of the Italian Hospital and all participating hospitals. All patients gave written informed consent.
Data sharing: Further information is available on request from the corresponding author at frubinstein@iecs.org.ar. Consent for data sharing was not obtained from the participants, but the presented data are anonymised and risk of identification is low.
Cite this as: BMJ 2013;346:f393
Web Extra. Extra material supplied by the author
Members of EVA Study Research Group
References
- 1.Chan M. World now at the start of 2009 influenza pandemic: statement to the press by WHO Director-General Dr Margaret Chan. 2009. www.who.int/mediacentre/news/statements/2009/h1n1_pandemic_phase6_20090611/en/index.html.
- 2.Chowell G, Bertozzi SM, Colchero MA, Lopez-Gatell H, Alpuche-Aranda C, Hernandez M, et al. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N Engl J Med 2009;361:674-9. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. The 2009 H1N1 pandemic: summary highlights, April 2009-April 2010. 2010. www.cdc.gov/h1n1flu/cdcresponse.htm.
- 4.Pan American Health Organization. Pandemic (H1N1) 2009. http://new.paho.org/hq/index.php?option=com_content&task=blogcategory&id=805&Itemid=569&lang=en.
- 5.Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 2009;374:451-8. [DOI] [PubMed] [Google Scholar]
- 6.Kort B, Cefalo R, Baker B. Fatal influenza pneumonia in pregnancy. Am J Perinatol 1986;3:179-82. [DOI] [PubMed] [Google Scholar]
- 7.Naleway A, Smith W, Mullooly J. Delivering influenza vaccine to pregnant women. Epidemiol Rev 2006;28:47-53. [DOI] [PubMed] [Google Scholar]
- 8.Dodds L, McNeil SA, Fell DB, Allen VM, Coombs A, Scott J, et al. Impact of influenza exposure on rates of hospital admissions and physician visits because of respiratory illness among pregnant women. CMAJ 2007;176:463-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louie JK, Acosta M, Jamieson DJ, Honein MA. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med 2010;362:27-35. [DOI] [PubMed] [Google Scholar]
- 10.Neuzil K, Reed G, Mitchel F. Impact of influenza on acute cardiopulmonary hospitalization in pregnant women. Am J Epidemiol 1998;148:1094-102. [DOI] [PubMed] [Google Scholar]
- 11.Creanga AA, Johnson TF, Graitcer SB, Hartman LK, Al-Samarrai T, Schwarz AG, et al. Severity of 2009 pandemic influenza A (H1N1) virus infection in pregnant women. Obstet Gynecol 2010;115:717-26. [DOI] [PubMed] [Google Scholar]
- 12.Dubar G, Azria E, Tesnière A, Dupont H, Le Ray C, Baugnon T, et al, for the French Registry on 2009 A/H1N1v during pregnancy. French experience of 2009 A/H1N1v influenza in pregnant women. PLoS One 2010;5:e13112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hewagama S, Walker SP, Stuart RL, Gordon C, Johnson PDR, Friedman D, et al. 2009 H1N1 influenza A and pregnancy outcomes in Victoria, Australia. Clin Infect Dis 2010;50:686-90. [DOI] [PubMed] [Google Scholar]
- 14.Louie JK, Acosta M, Jamieson DJ, Honein MA, for the California Pandemic (H1N1) Working Group. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med 2010;362:27-35. [DOI] [PubMed] [Google Scholar]
- 15.The ANZIC Influenza Investigators and Australasian Maternity Outcomes Surveillance System. Critical illness due to 2009 A/H1N1 influenza in pregnant and postpartum women: population based cohort study. BMJ 2010;340:c1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pierce M, Kurinczuk JJ, Spark P, Brocklehurst P, Knight M, for UKOSS. Perinatal outcomes after maternal 2009/H1N1 infection: national cohort study. BMJ 2011;342:d3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Puleston RL, Bugg G, Hoschler K, Konje J, Thornton J, Stephenson I, et al. Observational study to investigate vertically acquired passive immunity in babies of mothers vaccinated against H1N1v during pregnancy. Health Technol Assess 2010;14:1-82. [DOI] [PubMed] [Google Scholar]
- 18.Zuccotti G, Pogliani L, Pariani E. Transplacental antibody transfer following maternal immunization with a pandemic 2009 influenza A(H1N1) MF59-adjuvanted vaccine. JAMA 2010;304:2360-1. [DOI] [PubMed] [Google Scholar]
- 19.Benowitz I, Esposito DB, Gracey KD, Shapiro ED, Vazquez M. Influenza vaccine given to pregnant women reduces hospitalization due to influenza in their infants. Clin Infect Dis 2010;51:1355-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eick AA, Uyeki TM, Klimov A, Hall H, Reid R, Santosham M, et al. Maternal influenza vaccination and effect on influenza virus infection in young infants. Arch Pediatr Adolesc Med 2011;165:104-11. [DOI] [PubMed] [Google Scholar]
- 21.Hanquet G, Van Damme P, Brasseur D, De Cuyper X, Gregor S, Holmberg M, et al. Lessons learnt from pandemic A(H1N1) 2009 influenza vaccination: highlights of a European workshop in Brussels (22 March 2010). Vaccine 2011;29:370-7. [DOI] [PubMed] [Google Scholar]
- 22.Tsai T, Kyaw MH, Novicki D, Nacci P, Rai S, Clemens R. Exposure to MF59- adjuvanted influenza vaccines during pregnancy: a retrospective analysis. Vaccine 2010;28:1877-80. [DOI] [PubMed] [Google Scholar]
- 23.Clark TW, Pareek M, Hoschler K, Dillon H, Nicholson KG, Groth N, et al. Trial of 2009 influenza A/H1N1 monovalent MF59-adjuvanted vaccine. N Engl J Med 361:2424. [DOI] [PubMed]
- 24.Moro PL, Broder K, Zheteyeva Y, Walton K, Rohan P, Sutherland A, et al. Adverse events in pregnant women following administration of trivalent inactivated influenza vaccine and live attenuated influenza vaccine in the vaccine adverse event reporting system, 1990-2009. Am J Obstet Gynecol 2011;204:146.e1-7. [DOI] [PubMed] [Google Scholar]
- 25.Folkenberg M, Callréus T, Svanström H, Valentiner-Branth P, Hviid A. Spontaneous reporting of adverse events following immunisation against pandemic influenza in Denmark November 2009-March 2010. Vaccine 2011;29:1180-4. [DOI] [PubMed] [Google Scholar]
- 26.Lacroix I, Damase-Michel C, Kreft-Jais C, Castot A, Montastruc JL, for the French Association of Regional Pharmacovigilance Centres. 2009 H1N1 influenza vaccines in pregnant women: the French pharmacovigilance survey. Vaccine 2011;29:1357-8. [DOI] [PubMed] [Google Scholar]
- 27.Härmark L, van Hunsel F, Hak E, van Grootheest K. Monitoring the safety of influenza A/H1N1 vaccine using web-based intensive monitoring. Vaccine 2011;29:1941-7. [DOI] [PubMed] [Google Scholar]
- 28.European Medicines Agency. Focetria Vacuna para la pandemia gripal (antígeno superficial, desactivados, coadyuvantes) A/California/7/2009 (H1N1). EMEA, 2009 (available at www.colmed5.org.ar/Noticias/focetria.pdf). (Ref doc: EMEA/681665/2009 EMEA/H/C/710.)
- 29.Lim SH, Lee JH, Kim BC, Jung SU, Park YB, Lee CS. Adverse reaction of influenza A/H1N1 2009 virus vaccination in pregnant women and its effect on newborns. Vaccine 2010;28:7455-6. [DOI] [PubMed] [Google Scholar]
- 30.Bone A, Guthmann JP, Nicolau J, Lévy-Bruhl D. Population and risk group uptake of H1N1 influenza vaccine in mainland France 2009-2010: results of a national vaccination campaign. Vaccine 2010;28:8157-61. [DOI] [PubMed] [Google Scholar]
- 31.White SW, Petersen RW, Quinlivan JA. Pandemic (H1N1) 2009 influenza vaccine uptake in pregnant women entering the 2010 influenza season in Western Australia. Med J Aust 2010;193:405-7. [DOI] [PubMed] [Google Scholar]
- 32.Ahluwalia IB, Jamieson DJ, Rasmussen SA, D’Angelo D, Goodman D, Kim H. Correlates of seasonal influenza vaccine coverage among pregnant women in Georgia and Rhode Island. Obstet Gynecol 2010;116:949-55. [DOI] [PubMed] [Google Scholar]
- 33.Afinogenova VP, Kyt’ko OV. Influenza vaccination during pregnancy [Russian]. Zh Mikrobiol Epidemiol Immunobiol 2010;(4):114-7. [PubMed]
- 34.Pérez-Rubio A, Eiros Bouza JM, Castrodeza Sanz JJ. Evaluation of the influenza a H1N1 vaccination in Castilla and Leon regions, Spain. Med Clin (Barc) 2010;135:543-5. [DOI] [PubMed] [Google Scholar]
- 35.Lau JT, Cai Y, Tsui HY, Choi KC. Prevalence of influenza vaccination and associated factors among pregnant women in Hong Kong. Vaccine 2010;28:5389-97. [DOI] [PubMed] [Google Scholar]
- 36.Lineamentos técnicos gripe 2011. Campaña Nacional de Vacunación Antigripal Argentina, 2011. Ministerio de Salud de la Nación, 2011 (available at www.msal.gov.ar/gripe2011/5_equipos/info_equipos/lineamientos_tecnicos_gripe_2011.pdf).
- 37.Dirección de Estadísticas e Información de Salud. Estadísticas vitales: información básica—año 2009. Ministerio de Salud de la Nación, 2010 (available at www.deis.gov.ar/Publicaciones/Archivos/Serie5Nro53.pdf).
- 38.Libster R, Bugna J, Coviello S, Hijano DR, Dunaiewsky M, Reynoso N, et al. Pediatric hospitalizations associated with 2009 pandemic influenza A/H1N1 in Argentina. N Engl J Med 2010;362:45-55. [DOI] [PubMed] [Google Scholar]
- 39.American College of Obstetricians and Gynecologists Committee on Obstetrics Practice. Committee Opinion No. 468: influenza vaccination during pregnancy. Obstet Gynecol 2010;116:1006-7. [DOI] [PubMed] [Google Scholar]
- 40.Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep 2010;59(RR-8):1-62. [PubMed] [Google Scholar]
- 41.World Health Organization. WHO recommendations on pandemic (H1N1) 2009 vaccines. 2010. www.who.int/csr/disease/swineflu/notes/h1n1_vaccine_20090713/en/index.html.
- 42.Nokleby H, Nicoll A. Risk groups and other target groups—preliminary ECDC guidance for developing influenza vaccination recommendations for the season 2010-11. Euro Surveill 2010;15:19525. [PubMed] [Google Scholar]
- 43. Ohfuji S, Fukushima W, Deguchi M, Kawabata K, Yoshida H, Hatayama H, et al. Immunogenicity of a monovalent 2009 influenza A/H1N1 vaccine among pregnant women: lowered antibody response by prior seasonal vaccination. J Infect Dis 2011;203:1301-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karolinski A, Mercer R, Bolzán A. Proyecto investigacion operative: Utilidad del Sistema Informatico Perinatal (SIP): gestion para lavigilancia epidemiologica de la sifilis materna y sifilis congenita en una red de hospitales publicos del area metropolitana de BuenosAires, Argentina. CLAP/SMR, 2012. (CLAP/SMR Publicacion cientifica 1592) (available at http://new.paho.org/clap/index.php?option=com_joomlabook&Itemid=259&task=display&id=176).
- 45.Pasternak B, Svanström H, Mølgaard-Nielsen D, Krause TG, Emborg HD, Melbye M, et al. Vaccination against pandemic A/H1N1 2009 influenza in pregnancy and risk of fetal death: cohort study in Denmark. BMJ 2012;344:e2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dirección de Estadísticas e Información de Salud. Estadísticas vitals: información Básica—año 2010. Ministerio de Salud de la Nación, 2011 (available at www.deis.gov.ar/Publicaciones/Archivos/Serie5Nro54.pdf).
- 47.Knight M, Lim B. Immunization against influenza during pregnancy: the benefits outweigh the risks. BMJ 2012;344:e3091. [DOI] [PubMed] [Google Scholar]
- 48.Pasternak B, Svanström H, Mølgaard-Nielsen D, Krause T, Emborg H-D, Melbye M, et al. Risk of adverse fetal outcomes following administration of a pandemic influenza A (H1N1) vaccine during pregnancy. JAMA 2012;308:165-74. [DOI] [PubMed] [Google Scholar]
- 49.Fell DB, Sprague AE, Liu N, Yasseen AS 3rd, Wen SW, Smith G, et al, for the Better Outcomes Registry & Network (BORN) Ontario. H1N1 influenza vaccination during pregnancy and fetal and neonatal outcomes. Am J Public Health 2012;102:e33-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Heikkinen T, Young J, van Beek E, Franke H, Verstraeten T, Weil J, et al. Safety of MF59-adjuvanted A/H1N1 influenza vaccine in pregnancy: a comparative cohort study. Am J Obstet Gynecol 2012;207:177.e1-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Members of EVA Study Research Group