Abstract
This study introduces life cycle assessment as a tool to analyze one aspect of sustainability in healthcare: the birth of a baby. The process life cycle assessment case study presented evaluates two common procedures in a hospital, a cesarean section and a vaginal birth. This case study was conducted at Magee-Womens Hospital of the University of Pittsburgh Medical Center, which delivers over 10,000 infants per year. The results show that heating, ventilation, and air conditioning (HVAC), waste disposal, and the production of the disposable custom packs comprise a large percentage of the environmental impacts. Applying the life cycle assessment tool to medical procedures allows hospital decision makers to target and guide efforts to reduce the environmental impacts of healthcare procedures.
Keywords: sustainability, life cycle assessment, vaginal birth, operating room, cesarean
1. Introduction
1.1 Sustainable Research Needs in Healthcare
Healthcare represents a rapidly growing economic sector in the United States, accounting for 17% of the total US GDP in 2009 (Bureau of Economic Analysis, 2009). In 2008, US hospitals employed over 5.3 million people and spent nearly $320 billion on goods and services from other businesses (AHA, 2011). To support this level of activity, the healthcare sector is estimated to consume 73 billion kWh of electricity annually, and its hospital facilities are the second most energy-intensive facility type per square foot in the US (Esmaeili et al., 2011; USDOE, 2009). The emissions from this electricity use alone result in an estimated tens of thousands of adverse health effects (AHA, 2010; National Research Council (U.S.) et al., 2010). In addition, medical facilities face unique infection control challenges that have led to increasing use of disposable materials and escalating waste production. Consideration of the effect on the environment, and potential subsequent health effects, is an important consideration.
The healthcare industry has begun estimating environmental impacts with studies analyzing the carbon footprint of hospitals (Maverick Lloyd Foundation, 2009; Subaiya et al., 2011) and the entire industry (Chung and Meltzer, 2009). England’s National Health Services, NHS, found their 2004 carbon footprint to be about 25% of England’s total public sector emissions at 18.6 thousand kilograms of carbon dioxide equivalent (CO2 eq) (Sustainable Development Commission, 2008). A recent study calculated the total global warming potential (GWP)1 directly caused by the US healthcare sector to be 254 billion kilograms of CO2 eq. Approximately 80% of the GWP in the healthcare sector is attributed to carbon dioxide (CO2), which is one-tenth of the total CO2 emissions in the US (Chung and Meltzer, 2009; Patrick, 2011). Although estimating GWP is important, expanding the scope of environmental impacts to include other negative environmental effects will create a more comprehensive understanding of the healthcare industry. In this study, we will introduce Life Cycle Assessment (LCA) as a tool that can analyze healthcare sustainability using multiple environmental impact categories.
1.2 Background on Process Life Cycle Assessment
Life Cycle Assessment (LCA) analyzes the environmental impacts of a product or process throughout its life cycle, including the production of raw materials, manufacturing, use, disposal, and any transportation between these steps. Process LCA follows guidelines set forth by the International Organization for Standardization (ISO 14040 and 14044) and is conducted in four stages (ISO, 1997; ISO, 2006). Stage one establishes the boundary conditions of the system and defines a functional unit for the system. This stage standardizes the results and enables equivalent comparison with other products or processes. During stage two, Life Cycle Inventory (LCI), all raw data are compiled with respect to system inputs and outputs. The LCI quantifies the materials and energy used as well as the emissions associated with each input and output. Stage three, Life Cycle Impact Assessment (LCIA), is the stage where the inventory data are translated into impact categories (e.g. ecotoxicity and global warming potential). The fourth and final stage is interpretation, where the inventory and impact assessment results are analyzed for areas within the system that have relatively high environmental impacts.
1.3 Case Study: Delivering a Baby
This research uses process LCA to quantify the environmental impacts of a vaginal delivery in a labor and delivery room (LDR) and a cesarean birth in an operating room (OR) at Magee-Womens Hospital (Magee) of the University of Pittsburgh Medical Center (UPMC). This case study was chosen to help direct the sustainability efforts for this hospital which delivers over 10,000 infants per year and is developing robust greening efforts throughout the hospital. Our goal was to help understand the relative environmental consequences of each component of the birth process in order to optimally target areas for improvement for the most common procedure in this hospital.
In order to achieve this goal, the first objective was to create a process LCA framework specific for hospitals. The second objective was to quantify the LCA data and evaluate the results for vaginal delivery and a cesarean delivery.
2 Methods
The complexities and challenges of combining life cycle assessment with the healthcare industry required that the project framework be well established. The first step was to develop collaborative partnerships between engineers and hospital staff. The second step was to establish the process LCA framework, which included data collection, LCI database selection, and LCIA results.
A research team was developed including engineers with expertise in LCA, physicians, nurses, and the hospital’s facility manager. Cultivating these relationships was necessary for obtaining an insider’s perspective of hospital operations and managerial complexities and discussing how hospital personnel could use the LCA framework and results.
2.1 Life Cycle Assessment Framework
2.1.1 Goal, Scope, and System Boundaries
The functional unit of this study was the birth of one baby. The boundaries of the study (Figure 1) focused on a single birth including components such as energy consumption, material production, sterilization, and material disposal. Due primarily to scarcity of LCI data regarding laundry services, cleaning chemicals, and anesthetics, the use and manufacturing of these items were not included in the study. For the purpose of this research, the environmental impacts due to the hospital’s construction or building materials as well as the manufacturing of large machines within the OR and LDR were not included. With respect to the construction of the hospital, LCA studies are inconsistent (Bilec et al., 2010). Some existing research has assumed that the impacts of the construction phase are negligible (Junnila and Horvath, 2003); others report that environmental impacts associated with construction are underestimated (Hendrickson and Horvath, 2000).
Figure 1.
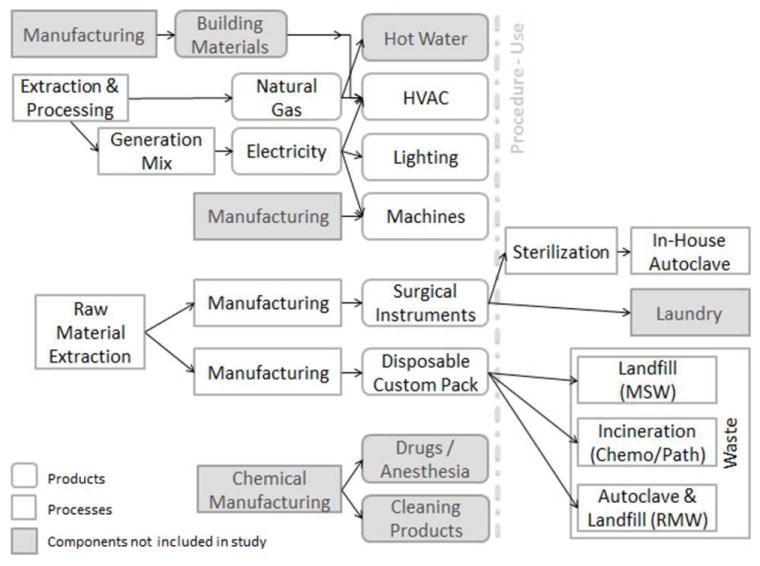
Data Flowchart for Cesarean Section and Vaginal Births
To provide system boundaries on the birth itself, this study defined vaginal birth as the expulsion of the infant and placenta only (stage 2 and 3 labor) and cesarean section as the activities occurring door to door during the surgery. This system boundary excluded the labor prior to delivery due to its poorly defined onset, wide variability in duration, location in or out of the hospital, and variability in medical interventions leading up to the birth. Setting this limit on the system boundary limits our conclusions to the birth itself, but also allowed the LCA to be feasible while still providing usable information to assist environmental efforts in our birth center. This system boundary also allowed for a comparison of the birth itself with the understanding that labor prior to delivery, and post-birth care can vary dramatically for women in both groups.
Based on a review of approximatley 15,000 births, the duration of vaginal birth used in this study was assumed to be 65 minutes (Janakiraman et al., 2010); placental delivery was assumed to be 15 minutes (Jangsten et al., 2011). We assumed a ratio of women having their first birth to women who have previously given birth of 40/60 based on Magee’s delivery patterns. Assumptions for the cesarean section were based on a door to door time for all comers of 75 minutes, including repeat and primary cesarean (Ismail and Huda, 2009). Consideration of anesthetic choices was excluded.
2.1.2 Life Cycle Inventory
Data from the hospital were collected to develop the LCI. Data collection included weighing of disposable custom packs and reusable surgical instrument packs, observing machine electrical consumption, and obtaining information from hospital specifications for lighting and heating, ventilation, and air conditioning (HVAC) parameters. In general, each component was then translated into the appropriate LCI unit process. As mentioned in Section 1.2, the LCI stage compiles the inputs and outputs of a product or process. Various published databases house the unit processes that correspond to a specific product or process, therefore database selection is important. The LCI unit processes were selected based on the following logic: (1) use US based databases (USLCI) (NREL, 2010); (2) use the most robust database (ecoinvent) (Frischknecht et al., 2005); (3) use other database if unit process was not available in either USLCI or ecoinvent. The other databases used when USLCI or ecoinvent were not applicable or available were determined by comparing the physical description and application of the material to the unit process description.
The following section is divided into two parts: LCI materials and LCI energy consumption. LCI materials describes the methods used to account for the production and end of life of the disposable custom packs and the reusable surgical instrument packs for both the cesarean section and vaginal births. The LCI energy consumption section explains methods used to determine electrical loading of machines and the energy consumption due to HVAC in both the OR in the case of cesarean section births and the LDR in the case of vaginal births.
LCI Materials
There are two unique custom packs, a disposable and a reusable, used in both types of birth at our case study hospital. Items in a disposable cesarean custom pack and disposable vaginal birth custom pack were weighed and separated by product material type. A summary of the materials, products, material production databases, and material disposal databases is shown in Table 1. If a product was comprised of more than one material, then the total weight of the product was divided evenly by the number of materials in the product. For example, a cautery tip polisher, 2.6 grams, is made of aluminum grit and polyurethane plastic; therefore, each material was assumed to be 1.3 grams of the total product. This method was used because many of the mixed material products were difficult to disassemble and accounted for a small percentage of the total custom pack. The custom packs were believed to represent the majority of the waste produced during a delivery with the exception of gloves, masks and sutures. These materials were not included in the study as they were considered to represent a small proportion of the waste.
Table 1.
Disposable Custom Pack Data.
| Material | Product Examples | Material Production | Material Disposal | Cesarean Pack (g) | Vaginal Pack (g) | ||
|---|---|---|---|---|---|---|---|
| LCI Database | Database Process Name | LCI Database | Database Process Name | ||||
| Cotton | OR towels, lap sponge, gauze | IDEMAT 2001b | Cotton fabric I | ecoinvent System Processes 2.0a | Disposal, inert material, 0% water, to sanitary landfill/CH S | 491.2 | 110.7 |
| Polyvinylchloride (PVC) | Umbilical cord clamp, ear/ulcer syringe | USLCI 1.6c | Polyvinyl chloride resin, at plant/RNA | ecoinvent System Processes 2.0a | Disposal, polyvinylchloride, 0.2% water, to sanitary landfill/CH S | 342.7 | 36.5 |
| Low-density polyethylene (LDPE) | CSR wrap, gowns, drapes | USLCI 1.6c | Low density polyethylene resin, at plant/RNA | ecoinvent System Processes 2.0a | Disposal, polyethylene, 0.4% water, to sanitary landfill/CH S | 1633.1 | 281.9 |
| High-impact polystyrene (HIPS) | Needle counter | USLCI 1.6c | High impact polystyrene resin, at plant/RNA | ecoinvent System Processes 2.0a | Disposal, polystyrene, 0.2% water, to sanitary landfill/CH S | 17.3 | 12.5 |
| Ethylene vinyl acetate | Light handles, needle counter | ecoinvent System Processes 2.0 a | Ethylene vinyl acetate copolymer, at plant/RER S | ecoinvent System Processes 2.0 a | Disposal, plastics, mixture, 15.3% water, to sanitary landfill/CH S | 21.4 | 12.5 |
| Polypropylene (PP) | Trays | USLCI 1.6c | Polypropylene resin, at plant/RNA | ecoinvent System Processes 2.0a | Disposal, polypropylene, 15.9% water, to sanitary landfill/CH S | 38.2 | 61.1 |
| Polyester/Rayon | Combine dressing | IDEMAT 2001b | Polyester fabric I | ecoinvent System Processes 2.0a | Disposal, plastics, mixture, 15.3% water, to sanitary landfill/CH S | 17.3 | - |
| Stainless Steel | Cautery Pencil | IDEMAT 2001b | X90CrCoMoV 17 I | ecoinvent System Processes 2.0a | Disposal, aluminium, 0% water, to sanitary landfill/CH S | 29.4 | - |
| Aluminum grit | Cautery tip polisher | ecoinvent System Processes 2.0a | Aluminum oxide, at plant/RER S | ecoinvent System Processes 2.0a | Disposal, aluminium, 0% water, to sanitary landfill/CH S | 1.3 | - |
| Paper | Labels, inventory sheet | BUWAL 250d | Paper woody C B250 | ecoinvent System Processes 2.0a | Disposal, paper, 11.2% water, to sanitary landfill/CH S | 6.4 | - |
| Polyurethane (PU) foam | Cautery tip polisher Processes 2.0a | ecoinvent System | Polyurethane, flexible foam, at plant/RER S | ecoinvent System Processes 2.0a | Disposal, polyurethane, 0.2% water, to sanitary landfill/CH S | 1.3 | - |
RNA = North American geographical code; RER = Europe geographical code; S = system process;
= (IDEMAT);
= (NREL 2010);
= (Lalive 1996)
The contents of the disposable custom pack were assumed to have entered Magee’s waste streams. Magee calculates that 80% of their waste is disposed of in the Municipal Solid Waste (MSW) stream, and 20% enters the Regulated Medical Waste (RMW) or “Red Bag” waste stream. The MSW from Magee is transported 20 km to a municipal solid waste landfill. RMW from Magee travels approximately 50 km in total, first to an autoclave facility for sterilization and then to the municipal solid waste landfill for disposal. Placentas are disposed of according to state law, which includes transporting them nearly 600 km to an incineration plant located in North Carolina. The LCI databases chosen to represent disposal of individual materials are shown in Table 1. Databases used in waste calculations not shown in this table include: Franklin USA 98 (Franklin Associates Ltd, 1998) for transportation of wastes to disposal facilities, ecoinvent system process 2.0 (Frischknecht et al., 2005) for biowaste incineration to represent disposal of chemo/pathogenic waste, and USLCI 1.6 (NREL, 2010) for the electrical consumption of autoclaving RMW. This case study assumed that other waste streams at Magee including recycling, hazardous waste, and electronic waste, were not generated during births.
Items in a reusable surgical instrument pack for both a cesarean birth and a vaginal birth were weighed and summarized, results shown in Table 2. The reusable surgical instrument packs are largely comprised of stainless steel instruments. However, the reusable packs are wrapped in a disposable wrap and, in the case of the cesarean pack, contain OR towels which are generally disposed of in MSW rather than sterilized and reused. Databases were identified for the production of the materials within the reusable surgical instrument packs. The LCI of the disposable materials within the reusable surgical instrument pack included material production with no allocations for reuse, as well as disposal in MSW stream.
Table 2.
Reusable Surgical Instrument Pack Data.
| Materials | LCI Database | Database Process Name | Cesarean Pack | Vaginal Pack | Assumptions | Data Source |
|---|---|---|---|---|---|---|
| CSR Wrap (g) | USLCI 1.6a | Low density polyethylene resin, at plant/RNA | 300.0 | 0.0 | Disposable | Weighed |
| OR Towels (g) | IDEMAT 2001b | Cotton fabric I | 200.0 | - | Disposable | Weighed |
| Stainless Steel Allocation | LCI Database | Database Process Name | Cesarean Pack | Vaginal Pack | Assumptions | Data Source |
| Stainless Steel Instruments (g) | IDEMAT 2001b | X90CrCoMoV17 I | 5054.8 | 1956.3 | Reusable | Weighed |
| Decontamination Electrical Consumption (kWh/cycle/pack) | USLCI 1.6a | Electricity, at grid, Eastern US/US | 2.43 | 2.43 | 1 cycle per pack | Machine Specs |
| Autoclave Electrical Consumption (kWh/Cycle/pack) | USLCI 1.6a | Electricity, at grid, Eastern US/US | 0.14 | 0.14 | 1/10 cycle per pack | Machine Specs; Assumptions |
The LCI of the reusable stainless steel instruments included the production of the stainless steel, allocated over the anticipated life span of the instruments, as well as the electrical consumption of the cleaning process that occurs in between each use of the instruments. The stainless steel instruments were assumed to have a life span of 10 years, based on repurchasing estimates, and to be sterilized once per day, resulting in 3,650 procedures and sterilization washes per custom pack. This calculation was used to allocate the production costs of the stainless steel instruments per functional unit.
In order to assess the environmental loading from the sterilization process, the electrical consumption of the standard decontamination and autoclaving procedures was also acquired. This data collection included the electrical loading associated with the sterilization process in the “LCI Materials” section because the results of the reusable materials were impacted by the electrical consumption, while HVAC electrical loading was a separate entity. The first step in cleaning the reusable instruments is a decontamination washer. Only the electrical consumption required to run the machine was considered in the LCI, and this included the electricity to power the drying system. The second step is sterilization of the reusable instruments with an autoclave. At Magee, there are 3 industrial size autoclaves, 2 Amsco 3043 vacamatics and 1 Steris Amsco Century V160H Prevac steam sterilizer, that run approximately 10 to 12 times per day. The autoclaves reach a high “over kill” temperature of 274°F to ensure 100% sterilization. For the allocation of the autoclave, only the electricity consumption was considered, which included the control system and vacuum pump for the autoclave. Based on observations at Magee, it was assumed that 10 kits are sterilized during each autoclave cycle.
LCI Energy Consumption
In order to estimate the electrical consumption of the machinery during each birth, the machines in the OR and in the LDR were inventoried, and Magee facilities engineer and hospital staff verified the use of the equipment for each procedure. Researchers recorded machine manufacture, model, medical function, and power rating, which can be seen in the supplementary materials.
For both the OR and LDR, the fetal heart monitor with printable readouts were not included in the machine load totals because electronic monitoring is generally favored except in rare situations. The patient beds have an electrical input when used to adjust the bed; however, it is not being constantly adjusted throughout each birth and was therefore excluded. The television and radio in the LDR were assumed to be off during the birth and also not included. The electrical loading of certain variable-draw machines, such as cauterizing tools, was calculated as a maximum, and therefore conservative, value.
The electrical loading for vaginal and cesarean section births was a summation of the LDR and OR machines’ power in watts, see Table 3. Lighting information was obtained through the hospital lighting specifications. The machine loading was then multiplied by the study’s assumed birth durations- 80 minutes for vaginal birth and 75 minutes for cesarean section birth (Ismail and Huda, 2009; Janakiraman et al., 2010; Jangsten et al., 2010). The USLCI 1.6 database process “Electricity, at grid, Eastern US/US” was modified to match Pennsylvania’s electricity production mix, see Table 4.
Table 3.
Machine and Lighting Information
| OR | LDR | Data Source | |
|---|---|---|---|
| Number of Machines | 17 | 10 | Observation |
| Machine Load (watts) | 7889 | 3738 | Machine Specifications |
| Number of Lights | 10 | 11 | Hospital Specifications |
| Lighting Load (watts) | 1942 | 507 | Hospital Specifications |
Table 4.
Pennsylvania Power Generation Mix from (USEPA 2007)
| Electricity Mix | PA % |
|---|---|
| Hydro | 0.6 |
| Nuclear | 22.3 |
| Oil | 0.3 |
| Gas | 2.9 |
| Coal | 72.9 |
| Non-hydro renewables | 0.5 |
In order to attribute the heating, ventilation and air conditioning (HVAC) energy expenditure of a single room in a complex hospital system, a fundamental approach to load calculation was taken. A bin type model was used, which assumed steady-state and calculated heating, cooling and dehumidification load in a specific space. This enabled accurate estimation of HVAC loading while avoiding HVAC system modeling that would create difficulties in allocation. Bin models are well documented and commonly used in systems load calculations and sizing (American Society of Heating, 2009). The assumptions and bin energy model information used in this study can be found in supplementary data.
2.2 Life Cycle Impact Assessment
Environmental impacts from the inputs and outputs of both birth procedures were calculated using TRACI 2 version 3.01 (Tool for the Reduction and Assessment of Chemical and Other Environmental Impacts) developed by the US Environmental Protection Agency (EPA) (Bare et al., 2003). Impact categories analyzed and reported include global warming, acidification, carcinogenics, non-carcinogenics, respiratory effects, eutrophication, ozone depletion, ecotoxicity, and smog.
3 Results and Discussion
The production of the disposable custom packs makes up a significant percentage of the ozone depletion and smog categories, due largely to the production of cotton and manufacturing of polyvinylchloride components in the packs. Waste disposal and transportation are the main contributors in the impact categories of carcinogens, non-carcinogens, eutrophication, and ecotoxicity. Machine, lighting, and HVAC loading contributed the highest percentage for both modes of delivery in the categories of global warming potential, acidification, and respiratory effects categories (see Figure 2). This was due to the production and consumption of electricity and natural gas required to run the machines, lighting, and HVAC system.
Figure 2.
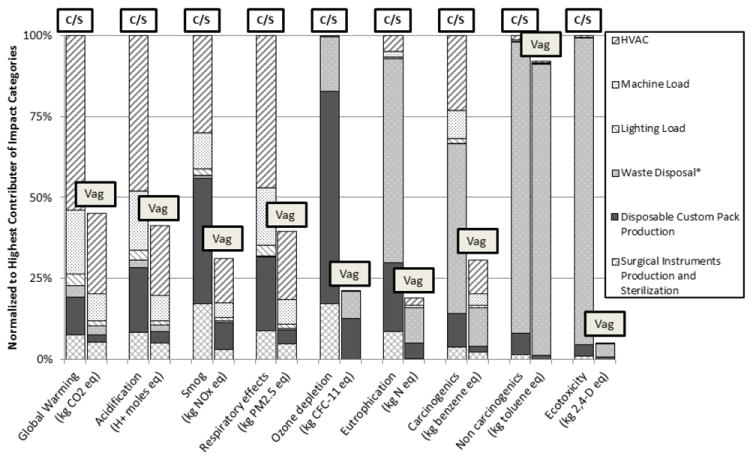
Environmental Impacts of Cesarean Section (C/S) and Vaginal (Vag) Births.
* Waste calculated for the disposable custom packs and placenta disposal.
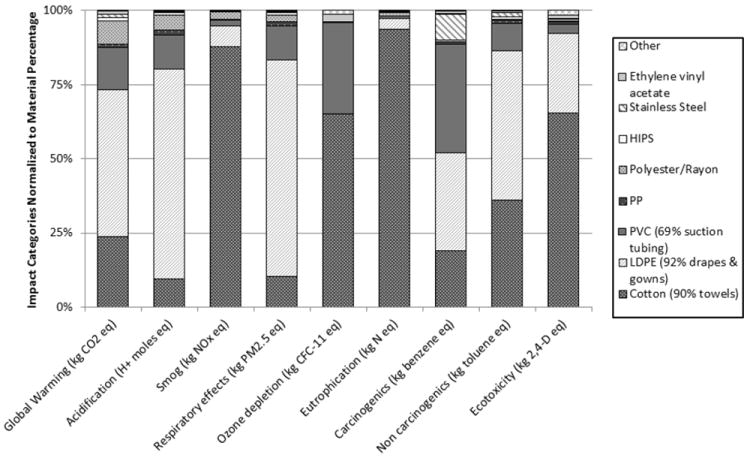
3.1 Disposable and Reusable Materials
The production of disposable and reusable materials of both birthing modes is summarized Figure 3. The production of disposable materials contributes the highest in every impact category for the cesarean section birth and five out of nine categories for the vaginal birth. Minimizing any infrequently used materials in the custom pack, and substituting reusable supplies when possible, is a high yield area for intervention. The proportionally greater effects of the vaginal reusable surgical pack are the result of a lesser quantity of disposable materials. While the cesarean section reusable surgical pack requires the same sterilization process, the larger quantity of materials in the cesarean section disposable custom pack minimizes the relative impacts of the reusable instruments in these categories.
Figure 3.
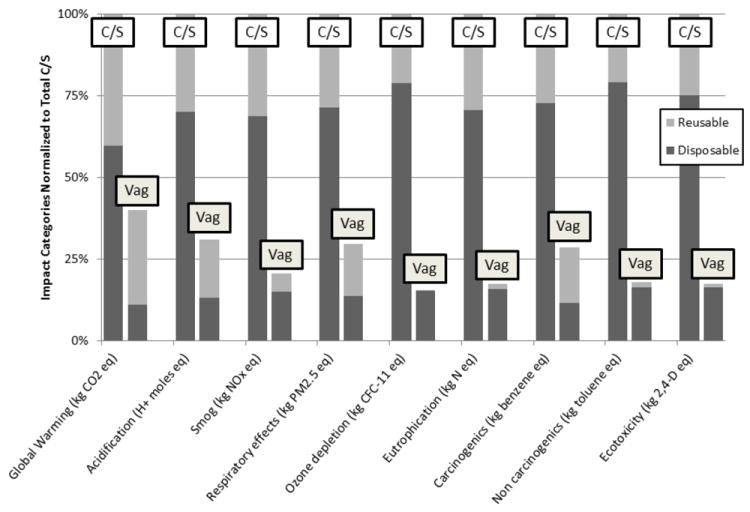
Cesarean Section (C/S) and Vaginal (Vag) Birth Disposable and Reusable Material Impacts
Significant variations in the assumed lifespan of the reusable surgical packs did not affect overall results. A sensitivity analysis of the assumed 10 year lifespan reveals negligible variation in the relative environmental impacts of reusable stainless steel instruments. Assuming a stainless steel instrument lifespan of 5 years resulted in an overall increase of 0.04% in the environmental impacts relative to the impacts of a 10 year lifespan. An assumed lifespan of 15 years resulted in a 0.1% relative decrease in environmental impacts of the stainless steel instruments. This further supports that the sterilization process, rather than the material production process, is a significant contributor to the environmental impacts associated with the reusable surgical packs.
Of the disposable materials, cotton, LDPE (low density polyethylene), and PVC (polyvinyl chloride) were the most consequential materials in all of the impact categories. Specifically, blue OR towels represented 90% of the cotton, gowns and drapes represent 92% of the LDPE, and suction tubing represented 69% of the PVC. Minimizing blue towel use, or substituting a more sustainable material, such as dye-free 100% biodegradable cotton, would lessen the environmental impact of this material. Although the laundry process was not considered in this LCA, as blue towels are typically disposed of in waste, consideration should be given to washing and reusing blue towels given the high environmental burden of producing cotton. The second major category for disposable materials was LDPE plastic, used in gowns and drapes. Reusable gowns and drapes would minimize use of this plastic, but further LCA analysis is needed to help quantify the degree to which this might be expected to lessen environmental impacts.
Cost effective alternatives to PVC tubing are being used in Magee’s Neonatal Intensive Care Units (NICU’s) to avoid neonatal exposure. These alternatives should be further researched and considered for use in the operating room as well.
The results show that the cesarean section birth has a higher environmental footprint compared to a vaginal birth, which is an indication of procedure complexity. The increasing reliance on disposable materials for both procedures contributes to higher levels of hospital waste, which could be diverted through the use of reusable materials. Efforts to reduce reliance on disposable products have the potential to reduce waste and environmental cost. Developing custom disposable packs that eliminate unused supplies, substitute equivalent materials with a lower environmental footprint, and are designed for efficiency is another important target area for environmental efforts.
3.2 Waste and Disposal
The total impacts from Figure 2 suggest that waste disposal, which includes transportation and the actual disposal process, contributes the highest percentage to the impact categories carcinogens, non-carcinogens, eutrophication, and ecotoxicity. With the exception of ecotoxicity, these categories are made up of over 60% plastic disposal to landfill, with polyethylene (PE) representing at least half of that number (see Figure 5). PE is a major component, by weight, of both disposable custom packs. The disposal of aluminum from cesarean section custom packs represents over 70% of the ecotoxicity category for cesarean section waste transportation and disposal. The RMW waste at Magee is landfilled at the same site as the MSW waste; thus, this transportation related impact is combined in Figure 5. Transportation of waste does not contribute significantly to the four impact categories examined in Figure 5 as transportation usually results in CO2 emissions associated with global warming potential and other impact categories not examined.
Figure 5.
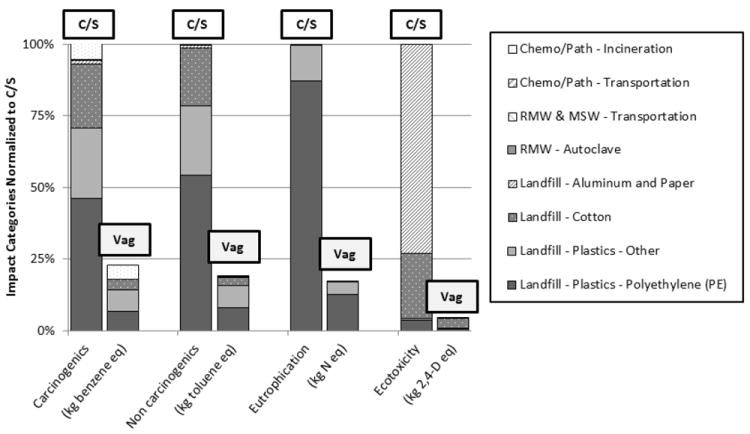
End of Life Impacts for Cesarean Section (C/S) and Vaginal (Vag) Births
There is no comprehensive US LCI database for waste disposal and for this reason ecoinvent 2.0 was used in this study (Moreno et al., 2011). Ecoinvent uses data from Switzerland and includes short-term emissions to air from incineration of landfill gas and leachate as well as treatment of leachate in wastewater treatment systems and municipal incineration of sludge. It is not standard practice in the US to incinerate municipal solid waste sludge, so this category may overestimate US landfill emissions. Additionally, ecoinvent 2.0 accounts for long-term emissions to groundwater after the base lining of the landfill fails, resulting in the allocation of a range of environmental impacts to a specific material type. For example, leaching of heavy metals into groundwater is included in the impacts from cotton disposal when cotton itself contains no heavy metals. For future work, available literature should be used to create more accurate waste disposal models (Barlaz, 2006; Gentil et al., 2010).
3.3 Machines, Lighting, and HVAC
Because of the associated impacts with consuming fossil fuels, the machines, lighting, and HVAC loading contributed the highest percentage to global warming potential, acidification, and respiratory effects for both modes of delivery. The HVAC system is in operation 24 hours a day, regardless of whether or not a birth is occurring and would, therefore, be expected to have an even higher relative impact when looking at the entire birthing unit over time. Optimizing the HVAC, instituting set back programs when the room is not in use and basing the number of required air turnovers on evidence in the infectious disease literature would be high yield areas for intervention, resulting in significant environmental and cost savings. Similarly, implementing occupancy sensors and low energy lighting could reduce the amount of electricity consumed and associated impacts. Further analysis of the HVAC system can be found in the supplementary material.
4 Conclusion
For all births, the processes contributing the most to environmental impacts were energy consumption due to HVAC, the end of life impacts of the disposable custom packs, and the production of the disposable custom packs. Therefore strategies should target these categories to reduce the overall the environmental impact of birthing options.
The production of both the disposable custom pack and reusable surgical pack for the cesarean section resulted in higher environmental impacts than the disposable and reusable materials in the vaginal birth packs. Understanding the differences in environmental impacts between disposable and reusable materials is an important consideration when evaluating the assembly of the custom packs and the necessity of certain materials and products contained within them. Future studies of the products and material composition in the disposable packs will further assist in preferred purchasing and environmentally conscious hospital decision-making.
For consistency in this research, standard LCI databases were used to represent waste impacts, but in future work, the LCI processes should be refined using cite specific data to more accurately portray end of life of medical materials. In addition to waste audits, energy auditing of medical equipment may increase the accuracy of LCA results.
Supplementary Material
Figure 4.
Environmental Impacts for the Production of Cesarean Section Disposable Materials
Table 5.
Bin Energy Model Input Variables
| Input Variable | Description | Unit | OR Data | LDR Data |
|---|---|---|---|---|
| Wall Constructiona | Wall area | ft2 | - | 86 |
| Wall U-value (ASHRAE 2004) | W/m2K | - | 0.36 | |
| Occupancy | Average number of people in room | people | 9 | 5 |
| Equipment Heat Load | Electricity consumption of machines and lighting | Watts | 9231 | 3429 |
| Air Changes | Number of air changes in the room per hour (ANSI 2010)) | Air changes/hour | 20 | 10 |
| Flow Rate/ Room Volume | Volume of the room | ft3 | 4200 | 3200 |
| Inside Temperature (avg) | (ANSI 2010) | °F | 66-70 | 68-73 |
| Air Temperature Prior to room Entrance | Air temperature in circulating air before it is heated at room entrance | °F | 52 | 52 |
| Outside Temperature (avg) | Yearly average from local weather station (National Renewable Energy Lab 2011) | °F | Pittsburgh Weather | Pittsburgh Weather |
| Humidity Set Point | (ANSI 2010) | % | 45-60 | 30-60 |
| Chiller Efficiency | Specific to hospital chiller | % | 80 | 80 |
| Boiler Efficiency | Specific to hospital boiler | % | 80 | 80 |
| Duration | Single year, 24 hours/day | Hours | 8765.8 | 8765.8 |
Because the OR has no exterior walls, wall construction was not used in bin calculations.
Table 6.
Variations in Birth Durations
| Mean Duration (min) | Median (min) | Data Source | |
|---|---|---|---|
| Nullipara (40%) | 117 | 83 | (Janakiraman, Ecker et al. 2010; Jangsten, Mattsson et al. 2011) |
| Multipara (60%) | 56 | 30 | (Janakiraman, Ecker et al. 2010; Jangsten, Mattsson et al. 2011) |
| Labor and Delivery Room Total Average | 80.4 | 51.2 | = 0.4(Min nullipara) + 0.6(Min Multipara) |
| Operating Room Average | 75 | 30 | (Ismail and Huda 2009) |
Highlights.
Life Cycle Assessment helps identify the environmental impacts of medical procedures
Disposable custom packs represent a large portion of environmental impacts of births
Electricity loading contributes to global warming potential and respiratory effects
Impact improvements should focus on air conditioning and disposable custom packs
Acknowledgments
The authors are grateful for the reviewers’ comments that significantly improved the paper. We would also like to thank Drew Chidester, Sam McMahon, David Gosnell, Judy Focareta, and Magee Staff. The project described was supported by NSF IGERT Award No. 050434. This publication was made possible by Grant Number ULI RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Disclosure Statement
Authors Campion, Thiel, DeBlois, and Bilec are employees of the University of Pittsburgh employee. Author Woods is an employee of Magee-Womens Hospital of UPMC. Landis is an employee of Arizona State University. Further financial support for these authors comes from Grant Number ULI RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research (Campion, Thiel, Landis, Bilec, and Woods) and Award No. 050434 from the National Science Foundation (NSF) Integrative Graduate Education and Research Traineeship (IGERT) (Thiel, DeBlois).
Footnotes
Operating Room (OR)
Labor and Delivery Room (LDR)
Life Cycle Assessment (LCA)
Life Cycle Inventory (LCI)
Life Cycle Impact Assessment (LCIA)
Magee-Womens Hospital (Magee)
Heating, Ventilation and Air Conditioning (HVAC)
Regulated Medical Waste (RMW)
Municipal Solid Waste (MSW)
Global Warming Potential (GWP)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- AHA. Sustainability Roadmap for Hospitals. Chicago, IL: 2010. Sustainability Roadmap for Hospitals - Energy. [Google Scholar]
- AHA. The Economic Contribution of Hospitals. American Hospital Association, AHA. 2011 [Google Scholar]
- American Society of Heating R, and Air Conditioning Engineers, inc. 2009. ASHRAE Handbook - Fundamentals (SI Version) Atlanta, GA: 2009. [Google Scholar]
- Bare JC, Norris GA, Pennington DW, McKone T. TRACI: The tool for the reduction and assessment of chemical and other environmental impacts. Journal of Industrial Ecology. 2003;6:49–78. [Google Scholar]
- Barlaz MA. Forest products decomposition in municipal solid waste landfills. Waste Management. 2006;26:321–333. doi: 10.1016/j.wasman.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Bilec MM, Ries RJ, Matthews HS. Life-cycle assessment modeling of construction processes for buildings. Journal of Infrastructure Systems. 2010;16:199–205. [Google Scholar]
- Bureau of Economic Analysis. Gross Domestic Product by Metropolitan Area. 2009 [Google Scholar]
- Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA - Journal of the American Medical Association. 2009;302:1970–1972. doi: 10.1001/jama.2009.1610. [DOI] [PubMed] [Google Scholar]
- Esmaeili MA, Jahromi A, Twomey J, Yildirim B, Overcash M, Elsken T, et al. Energy consumption of VA hospital CT scans. Chicago, IL: 2011. [Google Scholar]
- Franklin Associates Ltd. Franklin USA 98. 1998 Online at: http://www.fal.com/ and http://www.sylvatica.com/
- Frischknecht R, Jungbluth N, Althaus H, Doka G, Dones R, Heck T, et al. The ecoinvent Database: Overview and Methodological Framework (7 pp) The International Journal of Life Cycle Assessment. 2005;10:3–9. [Google Scholar]
- Gentil EC, Damgaard A, Hauschild M, Finnveden G, Eriksson O, Thorneloe S, et al. Models for waste life cycle assessment: Review of technical assumptions. Waste Management. 2010;30:2636–2648. doi: 10.1016/j.wasman.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Hendrickson C, Horvath A. Resource use and environmental emissions of U.S. construction sectors. Journal of Construction Engineering and Management. 2000;126:38–44. [Google Scholar]
- Ismail S, Huda A. An observational study of anaesthesia and surgical time in elective caesarean section: spinal compared with general anaesthesia. International Journal of Obstetric Anesthesia. 2009;18:352–355. doi: 10.1016/j.ijoa.2009.02.013. [DOI] [PubMed] [Google Scholar]
- ISO. ISO 14040. Environmental Management - Life Cycle Assessment - Principles and Framework. International Organization for Standardization. 1997 [Google Scholar]
- ISO. Environmental management -- Life cycle assessment -- Requirements and guidelines. International Organization for Standardization; Switzerland: 2006. [Google Scholar]
- Janakiraman V, Ecker J, Kaimal AJ. Comparing the Second Stage in Induced and Spontaneous Labor. Obstetrics & Gynecology. 2010;116:606–611. doi: 10.1097/AOG.0b013e3181eeb968. [DOI] [PubMed] [Google Scholar]
- Jangsten E, Hellström A-L, Berg M. Management of the third stage of labour--focus group discussions with Swedish midwives. Midwifery. 2010;26:609–614. doi: 10.1016/j.midw.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Jangsten E, Mattsson LÅ, Lyckestam I, Hellström AL, Berg M. A comparison of active management and expectant management of the third stage of labour: a Swedish randomised controlled trial. BJOG: An International Journal Of Obstetrics And Gynaecology. 2011;118:362–369. doi: 10.1111/j.1471-0528.2010.02800.x. [DOI] [PubMed] [Google Scholar]
- Junnila S, Horvath A. Life-cycle environmental effects of an office building. Journal of Infrastructure Systems. 2003;9:157–166. [Google Scholar]
- Maverick Lloyd Foundation. Eco-Health Footprint Calculator. 2011. Dartmouth-Hitchcock: 2009. [Google Scholar]
- Moreno ER, Weidema PB, Bauer C, Nemecek T, Vadenbo OC, Wernet G. Ecoinvent Report 5(v3) The ecoinvent Centre; St. Gallen: 2011. Documentation of changes implemented in ecoinvent Data 3.0. [Google Scholar]
- National Research Council (U.S.), Committee on Health E, and Other External Costs and Benefits of Energy Production and Consumption, National Research Council, National Research Council (U.S.). Board on Environmental Studies and Toxicology, National Research Council (U.S.)., Board on Energy and Environmental Systems NRCUS, Board on Science T, and Economic Policy, National Academies Press (U.S.) Hidden costs of energy: unpriced consequences of energy production and use. Natl Academy Press; 2010. [Google Scholar]
- Labratory NRE, editor. NREL. U S Life-Cycle Inventory Database (USLCI) National Renewable Energy Labratory; 2010. [Google Scholar]
- Patrick K. Sustainable Healthcare: Getting more from less. BMJ. 2011;342:d2425. [Google Scholar]
- Subaiya S, Hogg E, Roberts I. Reducing the environmental impact of trials: A comparison of the carbon footprint of the CRASH-1 and CRASH-2 clinical trials. Trials. 2011;12 doi: 10.1186/1745-6215-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sustainable Development Commission. NHS England Carbon Emissions Carbon Footprinting Report. London: NHS; 2008. [Google Scholar]
- USDOE. Energy Information Administration Office of Energy Markets and End Use. U S Department of Energy; Washington, DC: 2009. Annual Energy Review 2008; p. 446. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


