Abstract
Objective
To review Indigenous infant mortality, stillbirth, birth weight, and preterm birth outcomes in Australia, Canada, New Zealand and the United States.
Methods
Systematic searches of published literature and a review and assessment of existing perinatal surveillance systems were undertaken. Where possible, within country comparisons of Indigenous to non-Indigenous birth outcomes are included.
Results
Indigenous/non-Indigenous infant mortality rate ratios range from 1.6 to 4.0. Stillbirth rates, where data are available, are also uniformly higher for Indigenous people. In all four countries, the disparities in Indigenous/non-Indigenous infant mortality rate ratios are most marked in the post-neonatal period. With few exceptions, the rates of leading causes of infant mortality are higher among Indigenous infants than non-Indigenous infants within all four countries. In most cases, rates of small for gestational age and preterm birth were also elevated for Indigenous compared to non-Indigenous infants.
Conclusions
There are significant disparities in Indigenous/non-Indigenous birth outcomes in Australia, Canada, New Zealand and the United States. These Indigenous/non-Indigenous birth outcome disparities fit the criteria for health inequities, as they are not only unnecessary and avoidable, but also unfair and unjust.
Keywords: Indigenous, birth outcomes, infant mortality, stillbirth, birth weight, and preterm birth, Canada, Australia, New Zealand, United States
INTRODUCTION
The population of Indigenous peoples worldwide is estimated to be 370 million persons, or approximately 6% of the world population [1,2]. Culturally, linguistically, and geographically Indigenous peoples are remarkably diverse [3]. The United Nations recognizes right of Indigenous peoples to determine their own identity or membership [4]. Practically, Indigenous peoples can be defined by their historical continuity with pre-invasion and pre-colonial societies that developed on their territories; self-differentiation from and non-dominance of other sectors of the societies now prevailing on those territories; and a determination to preserve, develop and transmit to future generations their ancestral territories, their ethnic identity, and culture [5].
The Indigenous populations of Australia, Canada, New Zealand, and the United States all share the experience of being minority populations in economically prosperous countries. In these four countries, economic, social, and health care resources have been, and continue to be, unequally distributed between the Indigenous and non-Indigenous populations [6–10]. In each country, Indigenous children and their families are more likely to be living below the poverty line and in overcrowded accommodation and are over-represented in other measures of low socioeconomic position [11]. Furthermore, there are striking health status disparities with Indigenous populations experiencing a disproportionate burden of potentially preventable mortality and morbidity from acute and chronic conditions [6–11].
The health of a nation’s infants is understood to be an important upstream indicator of the health of the population more generally, as well as a reflection of underlying social determinants of health [12]. In many Indigenous societies, infants are regarded as sacred. Their nurturance and protection is a central community function and integrally linked to the rest of the life - death -life cycle [13, 14]. Despite recent international collaborations to document and address Indigenous child and adult health disparities [6,11,15], there is a gap with respect to an international review of Indigenous birth outcomes. We provide an overview of the major birth outcomes (infant mortality, stillbirth, birth weight, and pre-term birth) for Indigenous populations in Australia, Canada, New Zealand, and the United States.
METHODS
This is an extension of a larger review of Indigenous children’s health and health assessment in the four countries [11]. In the production of this larger report, one or more leading authorities on Indigenous children’s health was engaged from each of the four countries to write a country specific chapter which included an overview of Indigenous children’s health outcomes as well as best practice examples in children’s health assessment and response [16–19]. The lead country author(s) conducted a review of the published literature on children’s health (including birth outcomes) and/or drew on previously conducted reviews [10, 20]. For example, in Canada, in collaboration with a medical information specialist, a set of keywords for population and subject headings was derived, as well as a list of databases to search. Population key words included: Native, Indian, Aboriginal, Inuit, Métis, First Nations, infants, and children. These terms were combined with the subject headings: health status, health status disparities and health surveys. Searched databases included MEDLINE, Bibliography of Native North Americans; and Health Sciences: a full-text collection. Abstracts were independently reviewed by two Aboriginal health researchers using set criteria targeting Aboriginal infant and child health more generally [17]. Articles specific to birth outcomes were then identified for the current review. Within country perinatal surveillance data sources were also included in each country’s review. These included the Australian Institute of Health and Welfare (AIHW) and the Australian Bureau of Statistics (ABS) in Australia; the Canadian Perinatal Surveillance System (CPSS), Statistics Canada and provincial and territorial ministries of health in Canada; the Perinatal and Maternal Mortality Review Committee (PMMRC) in Aotearoa/New Zealand and the Centers for Disease Control and Prevention and the National Center for Health Statistics in the United States. The focus of this review was to examine within countries measures of infant mortality; neonatal death; postneonatal death; stillbirth and fetal death; perinatal death; low birth weight (<2500 grams); high birth weight (>4000 g); small for gestational age (<10th percentile); large for gestational age (>90th percentile); and preterm birth (<37 weeks). There is some variance among the four countries in the working definitions of perinatal and infant mortality indicators (Table 1).
Table 1.
Definitions of Perinatal and Infant Mortality Indicators in Australia, Canada, Aotearoa/New Zealand, and the United States
| Definition | Australia | Canada | New Zealand | United States |
|---|---|---|---|---|
|
| ||||
| Infant mortality - death between the age of 0 and 364 days of life or death before 1 year of age | X | X | X | X |
|
| ||||
| Neonatal death | ||||
|
| ||||
| - death between the age of 0 and 27 days of life. | X | X | X | |
| - death between the age of 0 and 28 days (includes 28th day). Early neonatal death is that which occurs within the first seven days of life (including on the seventh day). Late neonatal death is that which occurs between the eighth day and the 28th day (including on the 28th day). | X | |||
|
| ||||
| Postneonatal death | ||||
|
| ||||
| - death between the age of 28 and 364 days of life. | X | X | X | |
| - death between 29th day and one year of age. | X | |||
|
| ||||
| Fetal death | ||||
|
| ||||
| - synonymous with still birth. | X | X | ||
| - death of a fetus at ≥20 weeks, or weight ≥400 g if gestation is unknown, including stillbirth and pregnancy terminations. | X | |||
| - death of a fetus at ≥20 weeks, or weight ≥500 g if gestation is unknown, including stillbirth and pregnancy terminations. | X | |||
|
| ||||
| Still birth | ||||
|
| ||||
| - death of a fetus at ≥20 weeks or birth weight ≥400 g, including terminations of pregnancy at ≥20 weeks of gestation. | X | |||
| - death of a fetus with a gestation ≥ 20 weeks, or birth weight ≥500 grams. The definition varies slightly in the province of Quebec where only the birth weight criterion applies (birth weight 3500 grams). Includes terminations of pregnancy. | X | |||
| - death of a fetus born at ≥20 weeks, weight ≥400 g if gestation is unknown. Excludes terminations of pregnancy. | X | |||
| - not a technical term. Used generally to refer to late fetal death (≥ 28 weeks or ≥ 1000 g). | X | |||
|
| ||||
| Perinatal mortality rate | ||||
|
| ||||
| - Stillbirths and neonatal deaths per 1000 total babies born alive or born dead at ≥20 weeks, or weight ≥400 g if gestation is unknown. | X | |||
| - Fetal deaths and early neonatal deaths (during the first 7 days of life including day 7) per 1000 total at ≥20 weeks, or weight ≥500 g if gestation is unknown. | X | |||
|
| ||||
| - Fetal deaths and early neonatal deaths (death during the first 7 days of life including day 7) per 1000 total births at ≥20 weeks, or weight ≥400 g if gestation is unknown. | X | |||
| - Fetal deaths and neonatal deaths per 1000 total births at ≥20 weeks, or weight ≥500 g if gestation is unknown. | X | |||
Where possible within country comparisons between Indigenous and non-Indigenous or general populations are provided. Cited within country Indigenous rate ratio comparisons may vary with respect to the comparison group. In some cases, the comparison group also contains the Indigenous population (i.e. a ‘total population’ rather than a non-Indigenous comparator).
We have intentionally avoided direct international rate comparisons for the outcomes described. In addition to the usual challenges inherent in international comparison of birth outcomes, such as variation in the definition and reporting of stillbirth versus live birth, international comparisons are also limited by differences in both the methods used to collect and classify ethnicity data and in the quality and reliability of ethnicity data in each country.
RESULTS
Australia
In June 2006, the estimated Indigenous or Aboriginal and Torres Strait Islander population in Australia was 517,200 or 2.5% of the total Australian population. The Indigenous population was younger than the non-Indigenous population with median ages of 21.0 years and 37.0 years respectively. In 2003, 39% percent of the Indigenous population was under the age of 15 years, compared to 20% of the total Australian population. The relatively youthful Indigenous population is linked to a total fertility rate for Indigenous mothers of 2.1 babies compared with 1.8 babies for non-Indigenous mothers [21]. Recorded Indigenous births are likely to underestimate actual births as the Aboriginal and Torres Strait Islander status of the parent is not always recorded or is not correctly recorded [16, 22].
Infant and Perinatal Mortality
The rates of Indigenous infant deaths in Queensland, Western Australia, South Australia and the Northern Territory declined from 15.2 per 1000 live births in 1998 to 11.6 per 1000 live births in 2006. At the same time points, non-Indigenous infant mortality rates were, respectively, 5.1 and 4.2 per 1000 live births. The disparity between Indigenous and non-Indigenous populations decreased over these years from a rate ratio of 3.0 to 2.7, which represents a 10% decrease (Table 2) [23].
Table 2.
Infant Mortality Rates, Rate Ratios and Rate Differences in Australia, including Queensland, Western Australia, South Australia and the Northern Territory, 1998–2006(a)
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | Annual change(b) | % change over period(c) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Indigenous | 15.2 | 14.7 | 14.9 | 13 | 14 | 11.6 | 11.8 | 12.6 | 11.6 | −0.5* | −24.9* |
| Non-Indigenous | 5.1 | 4.7 | 4.7 | 4.8 | 4.8 | 3.8 | 4 | 4.4 | 4.2 | −0.1* | −17.8* |
| Rate ratio (d) | 3 | 3.2 | 3.1 | 2.7 | 3 | 3.1 | 3 | 2.9 | 2.7 | 0 | −8.4 |
| Rate difference(e) | 10.2 | 10.1 | 10.1 | 8.2 | 9.3 | 7.8 | 7.8 | 8.2 | 7.4 | −0.4* | −28.5* |
Represents results with statistically significant increases or decreases at the p < 0.05 level over the period 1998–2006.
Data exclude 90 registered infant deaths where Indigenous status was not stated over the period 1998–2006 in Queensland, Western Australia, South Australia and the Northern Territory combined.
Average annual change in rates, rate ratios and rate differences determined using linear regression analysis.
Per cent change between 1998 and 2006 based on the average annual change over the period.
Mortality rate for Indigenous infants divided by the mortality rate for non-Indigenous infants.
Mortality rate for Indigenous infants minus the mortality rate for non-Indigenous infants.
Source: AIHW analysis of National Mortality Database
In 2006, Indigenous babies were over two and a half times more likely to die in the neonatal period (7.1 deaths per 1,000 live births) compared to non-Indigenous babies (2.8 deaths per 1,000 live births) and nearly twice as likely to die in the perinatal period (20.7 deaths per 1,000 live births and fetal deaths) compared with non-Indigenous babies (10.1 deaths per 1,000 live births and fetal deaths) [21].
In Western Australia, in the birth years 1984 to 2001, the post-neonatal death rate was higher than the neonatal death rate for Indigenous infants. The disparity between Indigenous and non- Indigenous post-neonatal mortality rates was more marked than the disparities in neonatal infant death, and increased over this period [24].
Cause of Death
Between 2002–2006, the major causes of death for Indigenous infants were conditions originating in the perinatal period (44%), sudden infant death syndrome (SIDS, 22%), congenital malformations (12%), respiratory diseases (8%), external causes (mainly accidents) (4%), and infectious and parasitic diseases (such as septicaemia, meningococcal infection and congenital syphilis, 4%) (Table 3). Death rates due to respiratory diseases and infectious and parasitic diseases were particularly high among Indigenous infants, and were, respectively, five and eleven times higher than those observed in non-Indigenous infants [21].
Table 3.
Causes of Infant Death (Deaths per 1,000 live births) by Aboriginal and Torres Strait Islander Status, Australia: Queensland, Western Australia, South Australia and the Northern Territory, 2002–06
| Cause of Death (ICD-10 codes) | Indigenous | Non-Indigenous | Rate Ratio |
|---|---|---|---|
| Certain conditions originating in the perinatal period (P00-P96) | 5.7 | 2.1 | 2.7* |
| Symptoms, signs, and abnormal clinical findings n.e.c. (R00-R99) | 2.7 | 0.5 | 5.7* |
| Sudden Infant death Syndrome (SIDS) (R95) | 1.1 | 0.2 | 5.4* |
| Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) | 1.5 | 1 | 1.5* |
| Diseases of the respiratory system (J00-J99) | 0.9 | 0.1 | 8.6* |
| External causes (injury & poisoning) (V01-Y99) | 0.5 | 0.1 | 3.8* |
| Certain infectious and parasitic diseases (A00-B99) | 0.3 | 0.1 | 4.2* |
| Diseases of the circulatory system (I00-I99) | 0.2 | 0.1 | 3.1* |
| Other conditionsa | 0.5 | 0.3 | 1.8* |
| Total | 12.3 | 4.2 | 2.9* |
Represents results with statistically significant differences in the Indigenous/non-Indigenous comparisons at the p < 0.05 level.
Other conditions include: neoplasms (C00-D48); diseases of blood and blood-forming organs (D50-D89); endocrine, nutritional and metabolic diseases (E00-E89); mental and behavioural disorders (F00-F99); diseases of the nervous system (G00-G99); diseases of the eye and adnexa (H00-H59); diseases of the ear and mastoid process (H60-H95); diseases of the digestive system (K00-K93); diseases of the musculoskeletal system and connective tissues M00-M99); diseases of the genitourinary system N00-N99); and diseases of the skin and subcutaneous tissue (L00-L99).
Note: Data are reported for Queensland, Western Australia, South Australia and the Northern Territory only. These four states and territories are considered to have adequate levels of Indigenous identification in mortality data. They do not represent a quasi-Australian figure.
Source: Australian Institute of Health and Welfare (AIHW) analysis of National Mortality Database.
The rate of SIDS (per 1000 live births) among the total Australian infant population has decreased significantly over the past two decades from 1.79 in the period 1980–90 to 1.15 in the period 1997–2002. National data describing the rates of Indigenous SIDS are not available. A Western Australia study including all deaths between 1980 and 2002 found that the rate of SIDS among non-Indigenous infants decreased from 1.3 to 0.6 per 1,000 live births over this period. However, a similar decrease was not observed among Indigenous infants whose SIDS death rates were 4.9 in 1980 and 4.7 per 1,000 live births in 2002. This slower decrease among Indigenous infants relative to non-Indigenous infants resulted in an increase relative risk of SIDS death (RR= 7.9) [25].
Birth Weight
During 2003–2005, there were 3601 low birth weight babies born to Indigenous mothers, which represented 13% of all Aboriginal and Torres Strait Islander births. This was more than double the proportion of low birth weight babies born to non-Indigenous mothers (6.1 per cent) [21]. Data from 1991–2004 show an increase in the rate of low birth weight babies born to Indigenous, from 11.2 to 12.1 per 100 live births.
Preterm Birth
In the period 2001–2004, 14 per cent of all babies born to Indigenous women were born preterm, compared with 8% of babies born to non-Indigenous women [22].
Canada
In Canada, Indigenous peoples represent themselves politically and are recognized by federal and provincial governments as belonging to one of several major groups: First Nations or Indian (includes Status Indians on-reserve, Status Indians off-reserve, and non-Status Indians), Inuit, and Métis. Collectively, these groups are recognized as ‘Aboriginal’ by the Canadian constitution [26].
According to the 2006 census, just under 1.2 million persons or 4% of the total population in Canada reported Aboriginal identity. Approximately 60% identified as North American Indian, 33% identified as Métis, 4% identified as Inuit, and the remaining 3% identified with more than one Aboriginal group and/or self-reported as Status Indians but didn’t identify as Aboriginal [27]. These numbers underestimate the actual Aboriginal population in Canada as there was significant non-participation in the census by a number of First Nations (Status Indians on-reserve) communities and individuals and possibly other Aboriginal groups [27]. In 2006, 29.7% of the Aboriginal population in Canada was under the age of 15 years, compared to 17.7% of the Canadian population. The large and growing populations of First Nations/Indians, Inuit, and Métis infants, children, and youth is linked to a birth rate that is 1.5 times higher than the non-Aboriginal birth rate [27]. Specifically, the fertility rate between 1996 and 2001 was 2.9 children for First Nations/Indian women, 2.2 for Métis women, and 3.4 for Inuit women, compared to a rate of 1.5 among all Canadian women [28].
Birth outcomes are described below according to specific Aboriginal subgroup. Data which is not disaggregated into these subgroups is less useful from a public health perspective as these major categories currently define health service infrastructure and provider jurisdiction [29]. As a result of deficiencies in Canada’s perinatal surveillance system, high quality birth outcomes data are only available for provincial subgroups of First Nations or Indians, and Inuit living in Inuit inhabited areas [20].
Infant and Perinatal Mortality
Between 1981 and 2000, in British Columbia, infant mortality rates among infants born to parents who were First Nations (Status Indians living on reserve, off-reserve Status Indians or those who self-identified as ‘Aboriginal’) were 2.3 times higher in rural areas and 2.1 times higher in urban areas than those of the ‘non-First Nations’ population [30].
In Manitoba, between 1991 and 2000, infant mortality rate (IMR) among First Nations (Status Indians on reserve) and self-identified off-reserve Status Indians was 10.2 per 1,000 live births compared to a ‘non-First Nations’ rate of 5.4 [31]. IMRs for First Nations (Status Indians on reserve) and Status Indians living off-reserve produced by the First Nations and Inuit Health Branch and/or the four Western provinces have not been included in this review due to variations in IMR calculation methods and in the quality of the Aboriginal data [20,29,32].
The disparities in First Nations (Status Indians on reserve) and off-reserve Status Indian IMRs are most marked for post-neonatal infant mortality. In British Columbia, the First Nations (Status Indians on reserve) and off-reserve Status Indian neonatal IMR was 1.3 (urban) and 1.5 (rural) times the ‘non-First Nations’ neonatal IMR while the post-neonatal IMR was 3.6 times the ‘non-First Nations’ postneonatal IMR in both urban and rural areas [30]. In Manitoba, no significant difference was found in the First Nations (Status Indians on reserve) and off-reserve Status Indian neonatal IMR compared to the ‘non-First Nations’ rate, however the First Nations (Status Indians on reserve) and off-reserve Status Indian postneonatal IMR was 3.6 times the ‘non-First Nations’ postneonatal IMR [31].
The first birth cohort linkage study examining Inuit infant mortality in Quebec for the years 1995–1997 used self-reported Inuit mother tongue as a proxy for Inuit ethnicity [33]. This is a fairly reliable proxy as 86% of the Inuit population in Quebec reports an Inuit language mother tongue. This study reported an IMR of 23.1 per 1,000 live births for Inuit mother tongue infants, which was over four times the IMR for French mother tongue infants. Wilkins et al. examined IMRs for residents of census subdivisions in which 33% or more of the population was Inuit [34]. The IMR (per 1,000 births) for ‘Inuit inhabited areas’ decreased from 25.6 in 1989–1993 to 21.9 in 1994–1998 and to 18.5 deaths in 1999–2003. IMRs in Inuit inhabited areas were consistently four times total Canadian IMRs, as Canadian IMRs also fell during this period, with a net result of no change in the Inuit inhabited area/Canadian IMR disparity.
Work using a larger birth cohort (1991–2000) in Quebec found a similar disparity with IMRs (per 1000 live births) of 18.7 among Inuit mother-tongue infants compared to 4.4 among and the infants of non-First Nations and non-Inuit mother tongue [35]. This study also reported that the disparity in infant mortality is greater in the postneonatal period (7.8 per 1000) than the neonatal period (2.5 per 1000).
There is very little published information regarding Aboriginal stillbirth and perinatal mortality rates. Simonet et al. have calculated a stillbirth rate for Inuit mother tongue women in Quebec of 2.6 per 1,000 total births (live and stillbirths) [35]. For Inuit-inhabited areas, the rate was 7.4 per 1,000 births, which was 1.7 times the stillbirth rate for the rest of Canada [36].
Cause of Death
Cause of death data are sparse as consistent Aboriginal identifiers on vital registration forms are lacking. For Inuit-inhabited areas, excess mortality is observed for all major causes of infant death compared to the rest of Canada, including congenital anomalies (risk ratio (RR)=1.6), immaturity-related conditions (RR=3.0), asphyxia (RR=2.4), SIDS (RR=7.2), infection (RR=8.3), and external causes (RR=7.3) [36]. Additional studies indicate that Aboriginal infants suffer from and/or die in disproportionate numbers from congenital anomalies [31, 37], respiratory tract infection [30, 31, 33] and SIDS [30, 31, 33].
Birth Weight
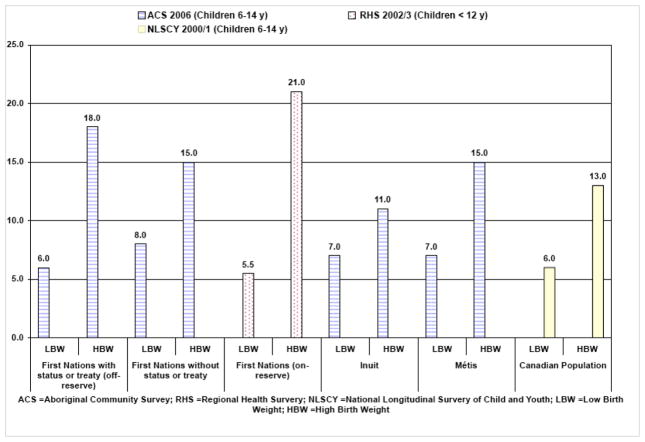
Parental reporting of birth weight on the Aboriginal Children’s Survey [38], First Nations Regional Longitudinal Health Survey [39] and National Longitudinal Survey of Children and Youth, [40] indicates that rates of low birth weight for First Nations (Status Indian living on reserve) and off-reserve Status Indians are similar to those of the Canadian population, while rates of low birth weight for non-Status Indians living off-reserve are higher than those of the Canadian population (Fig. 1). The rate of low birth weight was slightly higher for both the Inuit and Métis infants compared to the Canadian population [38,40]. Rates of high birth weight also varied, with substantially higher rates observed for First Nations living on-reserve and First Nations with status or treaty living off reserve compared to the total Canadian population(excluding First Nations reserves) [38,39,40]. Rates of high birth weight were slightly higher for non-Status Indians and Métis and slightly lower for Inuit again compared to total Canadian rates [38,40]. Studies based on birth registration for First Nations/Status Indians living on and off reserve in British Columbia and Manitoba demonstrate higher rates of large for gestational age (LGA) and lower rates of small for gestational age (SGA) for these populations compared to the non First Nations/Status Indian population [30,31]. First Nations and Inuit mother tongue populations in Quebec also have higher rates of LGA and lower rates of SGA compared to the other mother tongue groups [35].
Fig. 1.
Prevalence of Low (<2500 g) and High (>4000g) Birth Weight among Aboriginal groups and general population in Canada (source: ACS 2006, RHS 2002/3, NLSCY 2000/1).
Preterm Birth
There is no consistent national, provincial or territorial tracking of preterm birth rates among Aboriginal groups. In British Columbia, preterm birth rates among First Nations (Status Indians on reserve) and Status Indians living off-reserve were 40% to 70% higher than those of ‘non-First Nations [30]. In Manitoba, preterm birth rates among First Nations (Status Indians on reserve) and Status Indians living off-reserve are only slightly higher than those of ‘non-First Nations [31]. However, preterm birth rates are higher among Status Indians living off-reserve compared to on-reserve. For Inuit inhabited areas, the average preterm birth rate from 1990 to 2000 was 10.7%, compared to a rate of 7.4% for the rest of Canada [36]. Among a sample of Inuit women living in the Baffin Region between 1998 and 2000, 18.2% of births were preterm (before 37 weeks) and 2.4% of births were extremely preterm (before 32 weeks) [41]. These rates are similarly higher than reported rates of preterm birth in other regions of Canada for the same time period. Simonet et al., have calculated a preterm birth rate for Inuit mother tongue women in Quebec of 10.8% which is approximately 1.5 times the preterm birth rate of non-First Nations, non-Inuit mother tongue women [35].
New Zealand
According to the 2006 Census Māori - the Indigenous population in Aotearoa/New Zealand - accounted for about 15% of the total population in the 2006 census [42]. Thirty five percent of the Māori population is under 15 years of age, compared with 21.5% for the total population (which includes Māori) [43]. The drivers of Māori population growth include the younger age structure of the Māori population with more people in the child bearing years, and a higher fertility rate (2.7 in 2004 compared with 1.9 for non-Māori females)[44]. In 2007, just under 30% of babies born in New Zealand (NZ) were registered as being of Māori ethnicity [45].
Perinatal and Infant Mortality
The Perinatal and Maternal Mortality Review Committee (PMMRC) reported that, in 2007, the total perinatal related mortality rate was higher among Māori (11.4 per 1000 total babies born) compared to NZ European (9.8). Stillbirth rates were also higher among Māori (6.8 per 10,000 births) than NZ European (5.0). Similarly, the Māori neonatal mortality rate was higher (3.2 per 1000 live births) than the NZ European rate (2.2). None of these ethnic differences were statistically significant, but numbers are small as only one year of data is available [45].
Using a different method to ascertain perinatal and infant mortality rates and a different method of classifying ethnicity, Hauora: Māori Standards of Health IV reported infant mortality over the period 2000–2004. Māori infant mortality (8.1 per 1000 live births) was significantly higher than that of non-Māori infants (5.0 per 1000 live births; odds ratio 1.6; p<0.05) [46]. Māori/non-Māori disparities in infant mortality are most marked in the postneonatal period [47].
Cause of Death
In 2007, the PMMRC reported that the Maori perinatal mortality rate caused by ‘no obstetric antecedent’ was significantly higher than that of NZ European. Māori perinatal mortality rates due to antepartum haemorrhage, ‘specific perinatal conditions’, fetal growth restriction, maternal conditions, antepartum haemorrhage, and spontaneous preterm birth were higher than those of NZ Europeans but the differences were not statistically significant. Only one year of PMMRC data is available, so small numbers may preclude the detection of ‘true’ ethnic disparities in these outcomes [45] (Table 4).
Table 4.
Māori and New Zealand European Perinatal Death Classification - Specific Perinatal mortality rates (Per 1000 births) in New Zealand, 2007
| Perinatal Death Classification | Māori n = 19,463 | New Zealand European n = 28,755 | ||||
|---|---|---|---|---|---|---|
| n | % | Perinatal mortality rate | n | % | Perinatal mortality rate | |
| Congenital abnormality | 44 | 19.9 | 2.3 | 101 | 35.9 | 3.5 |
| Perinatal infection | 9 | 4.1 | 0.5 | 10 | 3.6 | 0.3 |
| Hypertension | 4 | 1.8 | 0.2 | 9 | 3.2 | 0.3 |
| Antepartum haemorrhage | 25 | 11.3 | 1.3 | 25 | 8.9 | 0.9 |
| Maternal conditions | 10 | 4.5 | 0.5 | 7 | 2.5 | 0.2 |
| Specific perinatal condition | 22 | 10 | 1.1 | 19 | 6.8 | 0.7 |
| Hypoxic peripartum | 11 | 5 | 0.6 | 15 | 5.3 | 0.5 |
| Fetal growth restriction | 18 | 8.1 | 0.9 | 15 | 5.3 | 0.5 |
| Spontaneous preterm | 36 | 16.3 | 1.8 | 32 | 11.4 | 1.1 |
| Unexplained antepartum | 33 | 14.9 | 1.7 | 47 | 16.7 | 1.6 |
| No obstetric antecedent | 9 | 4.1 | 0.5 | 1 | 0.4 | 0 |
Source: Perinatal and Maternal Mortality Review Committee (2009), p56.
Hauora
Hauora: Māori Standards of Health IV reported that for both Māori and non-Māori infants, perinatal conditions were the most common cause of death for infants under one year. Preterm birth was the main cause of death due to perinatal conditions and was significantly higher among Māori than non-Māori (odds ratio=1.8, p<0.05). Death from unknown causes was ranked second as a cause of death for Māori infants (2.4 per 1000 live births) and the third for non-Māori infants (0.4 per 1000 live births) with Māori infants nearly six times as likely to die of unknown causes than non-Māori (odds ratio=5.9, p<0.05). SIDS accounted for most deaths in the unknown cause’s category. The Māori SIDS rate was 2.0 per 1000 live births, significantly higher than the non-Māori rate of 0.4 per 1000 live births (odds ratio=5.7, p<0.05) [46].
Congenital anomalies was the third most common cause of death of Māori infants (1.2 per 1000 live births) and this rate was not significantly different from that of non-Māori infants. Accidental death was ranked fourth as a cause of death for both Māori and non-Māori infants. Māori infants were over four times as likely to die from an accident as non-Māori infants (odds ratio=4.1, p<0.05). Accidental suffocation in bed was the commonest accident resulting in death and was significantly higher among Māori (0.5 per 1000 live births) than non-Māori infants (0.1 per 1000 live births; odds ratio=4.3, p<0.05) [46]. Respiratory conditions ranked fifth as a cause of death for Māori infants (0.3 per 1000 live births) and the seventh for non-Māori infants (0.1 per 1000 live births) and the differences between the Māori and non- Māori rates were significantly different (odds ratio=4.1, p<0.05) [46].
Birth Weight and Preterm Birth
During 2002–2006, rates of SGA were 50% higher for Māori compared to European New Zealanders [47]. During 1996–2006, Māori experienced the highest preterm birth rates of any ethnic group in New Zealand.
United States
According to the most recent US Census in 2000, 4.3 million people or 1.5% of the total US population reported that they were American Indian or Alaska Native. Native Hawaiians makes up approximately 0.1% of the US population (401,000 people) [48]. In the United States there are approximately 1,129,000 American Indian/Alaska Native/NativeHawaiian children under 15 years of age. According to the 2000 U.S. Census, 3.7% of the American Indian/Alaska Native/Native Hawaiian population was under the age of 15 years, compared to 2.3% of the total American population.
Infant and Perinatal Mortality
Infant mortality rates are higher among the Native Hawaiian (9.0 per 1,000 live births) and American Indian/Alaska Native (AIAN) populations (8.3 per 1,000 live births) compared to a rate of 5.7 among White Americans [49]. The Native Hawaiian neonatal mortality rate (6.2 per 1,000 live births) is higher than both the AIAN neonatal mortality rate (4.4 per 1,000 live births) and the White neonatal mortality rate (3.8 per 1,000 live births) [49]. The postneonatal mortality rate for AIAN populations was 4.4 per 1,000 live births) and over twice that of Whites (1.9 per 1,000) [49].
Cause of Death
The leading cause of infant death in the United States in 2000 was congenital malformations, deformations and chromosomal abnormalities (congenital malformations), accounting for 21% of all infant deaths. Infant mortality rate for congenital malformations among American Indian mothers was 1.5 per 1000, but was not statistically significant from white mothers. Disorders related to short gestation and low birth weight, not elsewhere classified was the second leading cause of infant death and accounted for 16% of all infant deaths, followed by SIDS accounting for 9% infant deaths. For American Indian mothers, SIDS was 2.3 times that for white mothers. As most SIDS deaths occur during the postneonatal period, the high SIDS rates for infants of American Indian mothers account for much of their elevated risk of postneonatal mortality. For American Indian mothers, more than one-fourth (26%) of their elevated infant mortality rate, when compared with white mothers, can be accounted for by their higher SIDS rates (1.2 per 1000), and 14% by higher rates for low birth weight (1.1 per 1000) [49]. If American Indian infant mortality for SIDS and low birth weight could be reduced to white levels, the difference in the infant mortality rate between American Indian and white mothers would be reduced by 40% [49].
Comparable national Native Hawaiian cause of infant mortality data is not currently available because all reporting continues to follow the outdated U.S. Office of Management and Budget guidelines. In spite of the federal mandate to disaggregate Native Hawaiian and Other Pacific Islander data from the larger Asian race category, national data are still not publicly available on Native Hawaiians.
Birth Weight and Preterm Birth
Low birth weight or very low birth weight (birth weight less than 1500 g) is approximately 43% higher among AI/AN compared to their White American counterparts, and rates of prematurity among AI/AN are 16.6 per 1000 live births (compared to 11.3 per 1000 live births for White Americans) [49].
DISCUSSION
Understanding the Findings – A Global Perspective
In Australia, Canada, the United States and New Zealand, Indigenous peoples represent a sizeable, youthful, and growing population group. Given their younger population age structure and higher fertility rates, Indigenous populations embody a significant potential for future contribution to both Indigenous and non-Indigenous society in all four countries.
Significant and potentially preventable disparities in Indigenous/non-Indigenous birth outcomes are evident in all four countries. Stillbirth rates, where data are available, are uniformly higher for Indigenous people. In all four countries, infant mortality rates are higher among Indigenous children with Indigenous/non-Indigenous infant mortality rate ratios ranging from 1.6 to 4.0. In all four countries, the disparities in Indigenous/non-Indigenous IMR ratios are most marked in the post-neonatal period. Generally, stillbirth is associated with maternal health and access to maternity care; neonatal death is associated with access to obstetric and neonatal care; and postneonatal death is more likely to reflect social and environmental factors. These findings would suggest that health service, program, and policy responses are required across the spectrum of these domains, with special emphasis on the amelioration of Indigenous/non-Indigenous disparities in the social and environmental determinants of infant health.
With very few exceptions, mortality rates for the leading causes of death in all four countries are higher among Indigenous infants than non-Indigenous infants. Of particular concern are the consistent and significant Indigenous/non-Indigenous disparities in infant death from SIDS and respiratory tract infection, as there are existing public health strategies that can reduce both of these causes of death.
Indigenous infants in Australia, Canada, and the United States are more likely than non-Indigenous infants to be born with a low birth weight, except for First Nations/Indians in Canada. This is likely linked to the higher rates of preterm birth for Indigenous compared to non-Indigenous populations identified in all four countries. Where data was available, rates of SGA were also elevated for Indigenous compared to non-Indigenous infants except for First Nations/Indians in Canada. Interestingly, rates of HBW and LGA are increased for almost all groups of Indigenous peoples in Canada compared to the general and/or non-Indigenous populations. The increased incidence of HBW is marked for First Nations/Status Indians living on and off-reserve. While the underlying causes of this are not clear, links have been made between the relatively high and increasing rates of maternal diabetes in the First Nations/Indian population in Canada, compared to the non-Indigenous population [50]. While HBW/LGA are not routinely identified as major birth outcomes of interest, HBW and LGA are linked to adverse clinical outcomes [51]. It will be important to monitor it closely among Indigenous populations in Canada and perhaps also Australia, New Zealand and the United States, where there are emerging epidemics of chronic disease, including diabetes among Indigenous peoples [15].
The consistency of Indigenous/non-Indigenous birth outcome disparities across all four countries, across almost all major birth outcomes provides compelling evidence of Indigenous/non-Indigenous health inequity. Health inequity has been defined as “differences in health that are not only unnecessary and avoidable, but in addition unfair and unjust [52].” The persistence of these birth outcome disparities in affluent countries where the majority populations take for granted the daily expression of their rights to life, health, and livelihood is particularly problematic from a human rights and population health perspective. Furthering this sense of urgency and alarm is the fact that the challenges in the accurate identification of Indigenous individuals on vital registration records translates into a systematic underestimate of Indigenous/non-Indigenous birth outcome disparities as adverse Indigenous events are more likely to be misclassified as non-Indigenous than vice versa.
Measurement Limitations and Recommendations
Improvement of the quality and coverage of Indigenous birth outcomes data and health information systems is a priority in all four countries. A major challenge in Australia, Canada, and the United States is the accurate, consistent, and inclusive identification of Indigenous peoples on vital registration and hospitalization records. In all three countries, there is an under-registration of Indigenous births and deaths. In some cases, entire groups of Indigenous peoples are excluded from Indigenous data sets. For example, in Canada, high quality infant mortality rates are currently only available for two provincial subgroups of the First Nations/Indians and for Inuit living in Inuit inhabited areas [20]. There are no infant mortality rates for non-Status Indians and Métis [20], despite the fact that combined these two populations represent almost half of the Aboriginal identity population in Canada [27]. The major barrier to high quality Indigenous infant mortality rates in Canada is the absence of a consistent identifier on provincial and territorial infant birth and death registrations that is inclusive of all major Aboriginal groups. This exclusion of Indigenous persons or communities from basic public health surveillance based on their chosen place of residence, ethnic identity, or the use of government defined Indigenous categories over Indigenous determinations of identity and membership clearly violates the United Nations Declaration on the Rights of Indigenous Peoples.
When identifiers are present on vital statistics and hospitalization records, there is an additional challenge in ensuring that Indigenous ethnicity is correctly recorded. Misclassification of Indigenous persons as non-Indigenous is a common problem that contributes to underestimates of Indigenous/non-Indigenous health disparities. Cross-referencing of multiple databases and the use of an “ever Maori” flag has addressed this issue with some success in New Zealand.
In New Zealand, the Perinatal and Maternal Mortality Review Committee (PMMRC)’s maternal and perinatal dataset will eventually provide more rigorous and complete data but is limited at present by only having one full year (2007) of complete maternal and perinatal data. Several years of data will be required to clarify whether or not there are true Indigenous/non-Indigenous disparities in a number of birth outcomes. Direct comparison of the 2007 rates reported by the PMMRC cannot be made with previous data as the process used by PMMRC for ascertaining perinatal deaths in 2007 differs from the process used by the New Zealand Health Information Service in earlier years. In all four countries, changes in ethnic identification methods over time will impact our longitudinal understanding of birth outcomes.
Improvement is also required in the scope of available birth outcomes data. For example, while prematurity and stillbirths contribute greatly to the burden of disparities, they have attracted remarkably little attention among Indigenous populations. Some of this void can be attributed to gaps in data quality and coverage. The lack of a universally accepted definition of stillbirth makes it difficult to understand the magnitude or size of the problem. Additionally, more information and analysis is required regarding the causes of adverse birth outcomes, including their relative contributions. This will require the collection of additional information regarding social determinants of health and access to services on vital registration forms and/or the linkage of vital registration systems to other databases.
Moving Forward Under Indigenous Leadership
Indigenous peoples have clearly articulated their desire to be actively involved in the development, governance, and management of their health measurement systems [39, 53–56]. This mandate is linked to article 23 of the International Declaration on the Rights of Indigenous Peoples which recognizes the right of Indigenous peoples “to be actively involved in developing and determining health, housing and other economic and social programs affecting them and, as far as possible, to administer such programs through their own institutions [4]”. Hence, any improvement to Indigenous birth outcomes surveillance and response must be premised on solid partnerships with relevant Indigenous stakeholder groups. Ideally, such partnerships would involve Indigenous individuals and community authorities as leaders or co-leaders in the governance and day to day management of health information systems. An additional benefit of building in this type of Indigenous participation and leadership is that it facilitates the immediate uptake and application of birth outcome data into maternal, child, and family health programs and services, which are increasingly being administered by Indigenous authorities.
It is becoming more evident that strategic responses to Indigenous birth outcome inequities need to be specifically tailored to Indigenous community contexts. For example, in both Australia and New Zealand, significant decreases in the incidence of SIDS in the non-Indigenous populations were temporally linked to health promotion campaigns targeting SIDS risk factors [18, 56]. Unfortunately in both countries, similar decreases in the incidence of SIDS were not seen in Indigenous communities [16,18]. As a result, in New Zealand in 1994, a Māori specific SIDS prevention team was established. This Māoriled team developed tailored, Māori specific SIDS prevention strategies in close consultation with Māori communities. Subsequently, Māori SIDS rates have steadily fallen since 1995 [18]. Tailored response strategies are best implemented in partnership with and/or under the leadership of Indigenous community authorities as this will facilitate programs that build on local health knowledge and knowledge systems. Improvement of Indigenous birth outcome assessment and response under the leadership of and/or in partnership with Indigenous stakeholders is a priority in all four countries.
SYNOPSIS.
Indigenous birth outcomes in Australia, Canada, New Zealand and the United States are significantly worse than those of the majority non-Indigenous populations in all four countries, across every major birth outcome.
Acknowledgments
Dr. Smylie was supported by a Canadian Institutes of Health Research New Investigator award. Dr. Crengle was supported by the University of Auckland where she is a member of Te Kupenga Hauora Māori, School of Population Health, Faculty of Medicine and Health Sciences. Dr Freemantle was supported by Onemda VicHealth Koori Health Unit and by an Australian Research Council Fellowship. Dr. Taualii would like to acknowledge the Native Hawaiian Epidemiology Center, Papa Ola Lokahi, the Urban Indian Health Institute, and Seattle Indian Health Board.
References
- 1.Horton R. Indigenous peoples; time to act now for equity and health. Lancet. 2006;367(9524):1705–7. doi: 10.1016/S0140-6736(06)68745-X. [DOI] [PubMed] [Google Scholar]
- 2.Wikipedia contributors. Indigenous peoples. [Accessed January 13th, 2010];Wikipedia, The Free Encyclopedia. Available at: http://en.wikipedia.org/wiki/Indigenous_peoples.
- 3.International Work Group for Indigenous Affairs. [Accessed January 12th, 2010];Indigenous People – who are they? Available at: http://www.iwgia.org/sw641.asp.
- 4.United nations permanent forum on indigenous issues. United nations declaration on the rights of indigenous peoples. Geneva: United Nations; 2007. [Accessed January 12th, 2010]. Available at: http://issuu.com/karinzylsaw/docs/un_declaration_rights_indigenous_peoples?mode=embed&layout=http%3A%2F%2Fskin.issuu.com%2Fv%2Fdark%2Flayout.xml&showFlipBtn=true. [Google Scholar]
- 5.Cobo JRM. Study on the problem of discrimination against indigenous populations. Geneva: United Nations; 1986. UN Doc. E/CN.4/Sub.2/1986/7. [Google Scholar]
- 6.Anderson I, Crengle S, Kamaka ML, Chen TH, Palafox N, Jackson-Pulver L. Indigenous health in Australia, New Zealand, and the Pacific. Lancet. 2006;367(9524):1775–85. doi: 10.1016/S0140-6736(06)68773-4. [DOI] [PubMed] [Google Scholar]
- 7.Smylie J. The Health of Aboriginal People. In: Rapheal D, editor. Social determinant of health – canadian perspectives. 2. Toronto: Canadian Scholars Press; 2008. [Google Scholar]
- 8.Robson B, Harris R. Hauora: Māori Standards of Health IV. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare; 2007. [Google Scholar]
- 9.U.S. Commission on Civil Rights. Broken promises: evaluating the Native American health care system. Washington: U.S. Commission on Civil Rights; 2004. [Accessed January 12th, 2010]. Available at: http://www.usccr.gov/pubs/nahealth/nabroken.pdf. [Google Scholar]
- 10.Freemantle J, McAullay D, Officer K, Anderson I. Darwin: cooperative research centre for aboriginal health. Perth: Kulunga Research Network, Telethon institute for child health research, University of Western Australia; 2007. Australia Indigenous health - within an international context. [Google Scholar]
- 11.Smylie J, Adomako P. Indigenous Children’s Health Report: Health Assessment in Action. Toronto: St. Michael’s Hospital; 2009. [Google Scholar]
- 12.Reidpath DD, Allotey P. Infant mortality rate as an indicator of population health. J Epidemiol Comm Health. 2003;57(5):344–6. doi: 10.1136/jech.57.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aboriginal Healing and Wellness Strategy. Aboriginal healthy babies healthy children program overview. Toronto: Aboriginal Healing and Wellness Strategy; 2009. [Accessed January 12th, 2009]. Available at: http://www.ahwsontario.ca/programs/ahbhc/ahbhc_top.html. [Google Scholar]
- 14.National Aboriginal Community Controlled Health Organization. Definitions - Aboriginal Health. National Aboriginal Community Controlled Health Organization; 2008. [Accessed January 12th, 2010]. Available at: http://www.naccho.org.au/definitions/abhealth.html. [Google Scholar]
- 15.Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet. 2009;374(9683):65–75. doi: 10.1016/S0140-6736(09)60914-4. [DOI] [PubMed] [Google Scholar]
- 16.Freemantle J, McAullay D. Health of aboriginal and torres strait islander children in australia. In: Smylie J, Adomako P, editors. Indigenous Children’s Health Report: Health Assessment in Action. Toronto: Saint Michael’s Hospital; 2009. [Accessed June 26th, 2009]. Available at: http://www.stmichaelshospital.com/crich/indigenous_childrens_health_report.php. [Google Scholar]
- 17.McShane K, Smylie J, Adomako P. Health of first nations, inuit and métis children in canada. In: Smylie J, Adomako P, editors. Indigenous Children’s Health Report: Health Assessment in Action. Toronto: Saint Michael’s Hospital; 2009. [Accessed June 26th, 2009]. Available at: http://www.stmichaelshospital.com/crich/indigenous_childrens_health_report.php. [Google Scholar]
- 18.Crengle S. Health of Maori Children in Aotearoa/New Zealand. In: Smylie J, Adomako P, editors. Indigenous Children’s Health Report: Health Assessment in Action. Toronto: Saint Michael’s Hospital; 2009. [Accessed June 26th, 2009]. Available at: http://www.stmichaelshospital.com/crich/indigenous_childrens_health_report.php. [Google Scholar]
- 19.Taualii M. Health of Indigenous Children in the United States. In: Smylie J, Adomako P, editors. Indigenous Children’s Health Report: Health Assessment in Action. Toronto: Saint Michael’s Hospital; 2009. [Accessed June 26th, 2009]. Available at: http://www.stmichaelshospital.com/crich/indigenous_childrens_health_report.php. [Google Scholar]
- 20.Smylie J, Fell D, Ohlsson A the Joint Working Group on First Nations, Indian Inuit and Métis Infant Mortality of the Canadian Perinatal Surveillance System. A review of Aboriginal infant mortality rates in Canada – striking and persistent Aboriginal/non-Aboriginal inequities. Can J Public Health. 2010;101(2):143–48. doi: 10.1007/BF03404361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Australian Institute of Health and Welfare (AIHW), Australian Bureau of Statistics (ABS) The health and welfare of Australia’s Aboriginal and Torres Straight Islander Peoples. Canberra: AIHW and ABS; 2008. AIHW cat. no. 15; ABS cat. no. 4704.0.55.001. [Google Scholar]
- 22.Australian Bureau of Statistics. Births Australia, 2006. Canberra: Australian Bureau of Statistics; 2007. Cat. No. 33010.0. [Google Scholar]
- 23.Australian Bureau of Statistics. Experimental Estimates of Aboriginal and Torres Straight Islander Australians. Canberra: Australian Bureau of Statistics; 2007. Cat. No. 3238.0.55.001. [Google Scholar]
- 24.Freemantle CJ, Read AW, de Klerk NH, McAullay D, Anderson I, Stanley FJ. Patterns, trends and increasing disparities in mortality for Aboriginal and non-Aboriginal infants born in Western Australia, 1980–2001: population database study. Lancet. 2006;367(9254):1758–66. doi: 10.1016/S0140-6736(06)68771-0. [DOI] [PubMed] [Google Scholar]
- 25.Freemantle CJ, Read AW, de Klerk NH, McAullay D, Anderson I, Stanley FJ. Sudden Infant Death Syndrome - Aboriginal and non-Aboriginal disparities among infants born in Western Australia from 1980–2001 inclusive. J Paediatr Child Health. 2006;42(7–8):445–51. doi: 10.1111/j.1440-1754.2006.00895.x. [DOI] [PubMed] [Google Scholar]
- 26.Government of Canada. Constitution Act, Section 35. Ottawa: Government of Canada; 1982. [Google Scholar]
- 27.Statistics Canada. Aboriginal Peoples in Canada in 2006: Inuit, Métis, and First Nations, 2006; Census. Ottawa: Ministry of Industry; 2008. Catalogue number 7-558-XIE. [Google Scholar]
- 28.Statistics Canada. Women in Canada 2005. Ottawa: Statistics Canada; 2005. Catalogue Number 89-503-XIE. [Google Scholar]
- 29.Smylie J, Anderson M. Understanding the health of Indigenous peoples in Canada – key methodologic and conceptual challenges. CMAJ. 2006;75(6):602–5. doi: 10.1503/cmaj.060940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luo ZC, Kierans WJ, Wilkins R, Liston RM, Uh SH, Kramer MS. Infant mortality among first nations versus non-first nations in british columbia: temporal trends in rural versus urban areas, 1981–2000. Int J Epidemiol. 2004;33(6):1252–9. doi: 10.1093/ije/dyh290. [DOI] [PubMed] [Google Scholar]
- 31.Luo ZC, Wilkins R, Heaman M, et al. Neighbourhood socioeconomic characteristics, birth outcomes and infant mortality among First Nations and non-First Nations in Manitoba, Canada. Open J Women’s Health. 2010;4:55–61. doi: 10.2174/1874291201004020055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Green ME. Report prepared for Health Information and Analysis Division – First Nations and Inuit Health Branch. Ottawa: Health Canada; 2007. Reporting infant morality rates for Aboriginal populations in Canada: A jurisdictional review of methodologies. [Google Scholar]
- 33.Luo ZC, Wilkins R, Platt RW, Kramer MS. For the Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. Risks of adverse pregnancy outcomes among Inuit and North American Indian women in Quebec, 1985–97. Paediatr Perinat Epidemiol. 2004;18(1):40–50. doi: 10.1111/j.1365-3016.2003.00529.x. [DOI] [PubMed] [Google Scholar]
- 34.Wilkins R, Uppal S, Finès P, Senécal S, Guimond E, Dion R. Health Rep. 1. Vol. 19. Ottawa: Statistics Canada; 2008. [Accessed August 25, 2008]. Life expectancy in the Inuit-inhabited areas of Canada, 1989 to 2003; pp. 7–19. Catalogue 82-003. Available at: http://www.statcan.ca/english/freepub/82-003-XIE/82-003-XIE2008001.pdf. [PubMed] [Google Scholar]
- 35.Simonet F, Wilkins R, Heaman M, et al. Individual- and community-level disparities in birth outcomes and infant mortality among First Nations, Inuit and other populations in Quebec. Open J Women’s Health. 2010;4:18–24. doi: 10.2174/1874291201004020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo ZC, Senécal S, Simonet F, Guimond E, Penney C, Wilkins R. Birth outcomes in the Inuit-inhabited areas of Canada. CMAJ. 2010;182(3):235–42. doi: 10.1503/cmaj.082042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arbour L, Gilpin C, Millor-Roy V, et al. Heart defects and other malformations in the Inuit in Canada: a baseline study. Int J Circumpolar Health. 2004;63(3):251–66. doi: 10.3402/ijch.v63i3.17720. [DOI] [PubMed] [Google Scholar]
- 38.Statistics Canada. The 2006 Profile of Aboriginal Children, Youth and Adults. Ottawa: Statistics Canada; [Accessed February 28, 2009]. Available at: http://www12.statcan.gc.ca/census-recensement/2006/dp-pd/89-635/index.cfm?Lang=eng. [Google Scholar]
- 39.First Nations Information Governance Committee. First Nations Regional Longitudinal Health Survey (RHS) 2002/03: Results for Adults, Youth and Children Living in First Nations Communities. 2. Ottawa: Assembly of First Nations; 2007. [Accessed February 28th, 2009]. Available at: http://www.rhs-ers.ca/english/pdf/rhs2002-03reports/rhs2002-03-technicalreport-afn.pdf. [Google Scholar]
- 40.Statistics Canada. National Longitudinal Survey of Children and Youth. Cycle. 2000/2001;4 [Google Scholar]
- 41.Muggah E, Way D, Muirhead M, Baskerville B. Preterm delivery among Inuit women in the Baffin Region of the Canadian Arctic. Int J Circumpolar Health. 2004;63(Suppl 2):242–7. doi: 10.3402/ijch.v63i0.17910. [DOI] [PubMed] [Google Scholar]
- 42.Statistics New Zealand. Census 2006. Wellington: Statistics New Zealand; 2007. QuickStats About Māori. [Google Scholar]
- 43.Statistics New Zealand. Census 2006. Wellington: Statistics New Zealand; 2007. QuickStats about New Zealand’s Population and Dwellings. [Google Scholar]
- 44.Cormack D. The Māori Population. In: Robson B, Harris R, editors. Hauora: Māori Standards of Health IV. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare; 2007. [Google Scholar]
- 45.Perinatal and maternal mortality review committee. Perinatal and maternal mortality in New Zealand 2007: Third Report to the Minister of Health July 2008 to June 2009. Wellington: Perinatal and Maternal Mortality Review Committee; 2009. [Google Scholar]
- 46.Robson B, Purdie G. Mortality. In: Robson Harris R., editor. Hauora: Māori Standards of Health IV. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare; 2007. [Google Scholar]
- 47.Craig E, Jackson C, Han DY NZCYES Steering Committee. Monitoring the Health of New Zealand children and young people: Indicator Handbook. Auckland: Pediatric Society of New Zealand, New Zealand Child and Youth Epidemiology Service; 2007. [Google Scholar]
- 48.US Census. Census of Population, Public Law 94–171. [Google Scholar]
- 49.Mathews TJ, Menacker F, MacDorman MF. Infant mortality statistics from the 2000 period linked birth/infant death dataset. National Vital Statistics Report. 2002;50(12) [PubMed] [Google Scholar]
- 50.Whincup PH, Kaye SJ, Owen CG, et al. Birth weight and risk of type 2 diabetes: a systematic review. JAMA. 2008;300(24):2886–97. doi: 10.1001/jama.2008.886. [DOI] [PubMed] [Google Scholar]
- 51.Wilstrom I, Axelsson O, Bergstrom R, Meirik O. Traumatic injury in large-for-date infants. Acta Obstet Gynecol Scand. 1988;67(3):259–64. doi: 10.3109/00016348809004216. [DOI] [PubMed] [Google Scholar]
- 52.Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429–45. doi: 10.2190/986L-LHQ6-2VTE-YRRN. [DOI] [PubMed] [Google Scholar]
- 53.Brant Catellano M. Ethics of Aboriginal Research. J Aborig Health. 2004;1:98–114. [Google Scholar]
- 54.Onemda VicHealth Koori Health Unit. Koori Hands: A community report on Onemda VicHealth Koori Health Unit’s Research Workshops in 2007. Onemda VicHealth Koori Health Unit, The University of Melbourne; Melbourne: 2008. We Can Like Research. [Google Scholar]
- 55.Smylie J, Anderson I, Ratima M, Crengle S, Anderson M. “Who is Measuring and Why?” Indigenous Health Performance Measurement Systems in Canada, Australia, and New Zealand. Lancet. 2006;367(2):2029–31. doi: 10.1016/S0140-6736(06)68893-4. [DOI] [PubMed] [Google Scholar]
- 56.Australian Bureau of Statistics. SIDS in Australia 1981–2000 A Statistical Overview. Australian Bureau of Statistics; 2003. [Accessed January 12th, 2010]. Available at: http://www.sidsandkids.org/documents/finalsidspaper2003_002.pdf. [Google Scholar]