Abstract
Background
Hip pain secondary to acetabular dysplasia can prevent participation in recreational activities.
Questions/Purposes
We retrospectively evaluated the physical activity level and pain after periacetabular osteotomy (PAO) for the treatment of symptomatic hip dysplasia.
Methods
Forty-seven female and four male patients with a mean age of 27 years underwent a PAO. Physical activity (UCLA) and pain (WOMAC) were assessed preoperatively, at 1 year, and at minimum 2 years postoperatively. Multivariable linear regression identified substantial, independent factors associated with postoperative activity level.
Results
The UCLA activity scores were on average higher at 1 year and remained higher at minimum 2 years when compared with preoperative scores. Mean postoperative WOMAC pain scores assessed at 1 year and at least 2 years were lower than mean preoperative scores. Age and preoperative physical activity level were strong independent predictors for activity level at 1 year and at minimum 2 years after surgery. Postoperative pain level was a moderate predictor for the level of activity at minimum 2-year followup.
Conclusions
Physical activity level improves after PAO. Younger age and higher activity levels before surgery and lower level of pain after surgery are predictive factors for postoperative level of activity in the short term. The data presented here may be useful to counsel the active young adult with symptomatic hip dysplasia about the improvement of level of activity to be expected after PAO.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Regular physical activity is known to improve general health and quality of life [1, 18]. Hip dysplasia leads to mechanical joint instability resulting in acetabular rim overload and pain [11]. Hip pain may prevent participation in recreational and sports activities and directly impact quality of life.
The periacetabular osteotomy (PAO), described by Ganz et al. [8], has been shown to be successful in providing pain relief and improving hip function in patients with symptomatic hip dysplasia [5, 13, 17, 20]. Numerous studies on outcomes after PAO focus on instruments of quality of life and hip function [13, 17, 20] such as the WOMAC [4], the Merle d’Aubigné-Postel hip score [6], and the Harris hip score [9]. Although these instruments provide information about patients’ functional limitations, they do not directly assess activity level and sports participation.
Patients who participated in sports before PAO may wish to resume their activities after surgery. Difficulties and wish to return to recreation often are cited by patients with hip pain as important components of their disability [3, 24]. There is limited evidence, to date, regarding physical activity level patients can expect to achieve after a PAO and which factors may affect resumption of or improvement on preoperative activity levels.
The purposes of this study were to determine (1) patient physical activity level as measured by the UCLA scale and (2) pain as measured by the WOMAC pain subscale before, at 1 year, and a minimum of 2 years after PAO. (3) We also wanted to identify potential predictive factors for activity level after PAO.
Material and Methods
After institutional review board approval, we performed a query of our institutional hip registry to identify patients who underwent a PAO from January 2007 to July 2009. Inclusion criteria were symptomatic hip dysplasia with complete medical records and completion of questionnaires obtained prospectively at three distinct times: (1) before PAO; and (2) 1 year; and (3) at minimum 2 years postoperatively. All patients had experienced hip pain for at least 3 months, had radiographic evidence of acetabular dysplasia (lateral center-edge angle ≤ 16°, anterior center-edge angle ≤ 20°, or both), and minimal (Tönnis [19] Grade 1 or 2) or no (Tönnis [19] Grade 0) radiographic evidence of osteoarthritis (OA). Exclusion criteria were advanced OA (Tönnis [19] Grade ≥ 3), a primary or concurrent diagnosis of a hip disorder other than developmental hip dysplasia, underlying neuromuscular disease, and incomplete medical records or activity score questionnaires. We did not contact any patients specifically for this study; all data were obtained from medical records, radiographs, and previously prospectively collected questionnaires.
The database query yielded 161 patients who underwent PAO within the 2.5-year period, 51 of which met all inclusion and exclusion criteria. There were 47 female and four male patients with a mean age of 27 years (SD, 11 years) and a mean BMI of 24 kg/m2 (SD, 4 kg/m2) at the time of surgery. Running (22%) and indoor gym and fitness (16%) were the most common physical activities. The minimum followup was 2 years (mean, 2.4 years; range, 2–4 years) (Table 1).
Table 1.
Demographics of patients with periacetabular osteotomy
| Characteristic | Total sample (N = 51) |
|---|---|
| Age at surgery (years), mean ± SD | 27.3 ± 10.7 |
| Male sex (%) | 4 (8) |
| BMI (kg/m2), mean ± SD | 24.1 ± 3.9 |
| Activities before surgery (%) | |
| Running | 12 (22) |
| Gym | 8 (16) |
| Hockey | 3 (6) |
| Soccer | 3 (6) |
| Tennis | 3 (6) |
| Dance | 2 (4) |
| Softball | 2 (4) |
| Hiking | 2 (4) |
| Yoga | 2 (4) |
| Gymnastics | 1 (2) |
| Wrestling | 1 (2) |
| Unknown | 12 (24) |
| Activities after surgery (%) | |
| Running | 9 (17) |
| Hiking | 7(13) |
| Gym | 6 (12) |
| Softball | 3 (6) |
| Tennis | 3 (6) |
| Yoga | 3 (6) |
| Dance | 2 (4) |
| Hockey | 2 (4) |
| Soccer | 2 (4) |
| Swimming | 2 (4) |
| Gymnastics | 1 (2) |
| Snowboarding | 1 (2) |
| Volleyball | 1 (2) |
| Wrestling | 1 (2) |
| Unknown | 8 (16) |
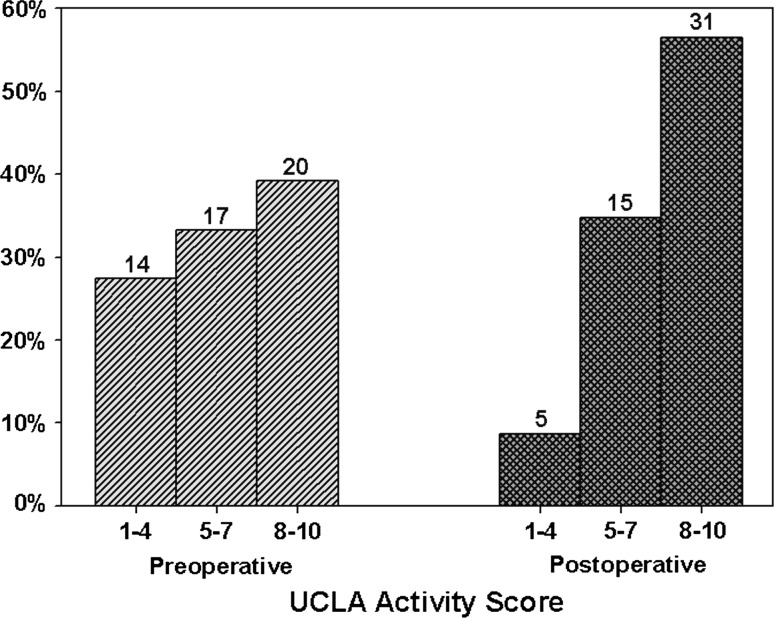
We assessed level of physical activity and pain by means of self-administered questionnaires. According to the protocol for prospective patient participation in the hip registry, most patients had completed preoperative and postoperative questionnaires at 1 year and at minimum the 2-year clinic visit. The UCLA scale was used to determine the level of physical activity [2, 25]. The UCLA scale is based on 10 descriptive activity levels [2, 25]. We divided patients into one of three general categories of activity level: (1) UCLA scores under 4 (regular participation in mild activities); (2) scores between 5 and 7 (moderate and active activities); and (3) higher than 8 (participation in very active events and impact sports). Preoperatively, 27% of patients had UCLA scores of 4 or lower, 33% had scores between 5 and 7, and 39% had scores 8 or higher. The level of pain was determined with the WOMAC pain subscale [4]. Pain over the previous month was rated in five areas as previously reported [13]: (1) walking on a flat surface; (2) climbing up or down stairs; (3) lying in bed at night; (4) sitting or lying; and (5) standing upright. The amount of pain was given a score of 0 (none), 1 (mild), 2 (moderate), 3 (severe), or 4 (extreme). We calculated a total pain score by adding the scores for the five different areas with a maximum score of 20 indicating extreme pain.
For each patient, sex, age at the time of surgery, type of physical activity, BMI, previous and subsequent hip surgeries, operative findings, and postoperative complications were collected from review of medical records. We classified postoperative complications into five grades based on the type of treatment required and long-term morbidity [16]. Grade I complications require no change in postoperative care, Grade II require treatment on an outpatient basis, Grade III involve invasive procedures, Grade IV include potential life-threatening or complications with high morbidity, and Grade V involve death.
PAO was performed according to a previously described technique [8, 13] by the two senior authors (YJK, MBM). Postoperatively, patients were allowed to walk with crutch assistance for 8 weeks with touchdown weightbearing of approximately 20% of body weight as instructed to the patient during the inpatient physical therapy. Patients were allowed to weightbear as tolerated once osteotomy healing was seen on radiographs.
Preoperative and most recent postoperative AP, lateral, and false-profile [12] pelvic radiographs were available for all patients and measured by a hip preservation fellow (ENN). The lateral center-edge angle (LCEA) of Wiberg [23], the acetabular roof obliquity angle of Tönnis [19], the anterior center-edge angle (ACEA) of Lequesne and de Séze [12], grade of OA, and osteotomy healing were recorded. Grade of OA was assessed with the Tönnis grading system as previously reported [13, 19]. The osteotomies were considered healed when there was no gap between the fragments and bone bridging could be observed in the two orthogonal views.
We compared postoperative UCLA scores, WOMAC pain scores, and radiographic parameters with preoperative assessments with a paired t-test. Multivariable linear regression identified substantial, independent factors associated with UCLA activity score at 1 and at minimum of 2 years after surgery [10]. Assessment scores were reported in mean and SD. We compared patients older than 28 years (the median age of the study population) with those younger than 28 years for UCLA scores across time with a nonpaired t-test. Statistical analysis was performed using the SPSS statistical package (Version 19.0; SPSS Inc/IBM, Chicago, IL, USA). Two-tailed p < 0.05 was considered statistically significant. Minimum sample sizes of 22 (1-year UCLA) and 19 (2-year UCLA) patients would have 80% power (α = 0.05; β = 0.20) to detect at least a 0.05 difference in slopes from null (ie, 0) given observed, multivariable-adjusted R2 of 0.39 (1-year UCLA) and 0.43 (2-year UCLA). Power analysis was performed with nQuery Advisor (Version 7.0; Statistical Solutions, Saugus, MA, USA).
Results
UCLA scores were increased (p = 0.001 for 1 year and p < 0.001 for 2 years) at 1 and 2 years after surgery. The UCLA scores were on average higher at 1 year (mean difference = 0.9 ± 2.3; p < 0.001) and remained higher at minimum 2 years (mean difference = 1.0 ± 2.4; p < 0.001) when compared with preoperative scores. Preoperatively, 27% of patients had UCLA scores of 4 or lower and 39% had scores of 8 or higher. At most recent followup, only 10% of patients had scores of 4 or lower, whereas the majority of patients (61%) had scores of 8 or higher (Fig. 1). Ten patients had lower activity levels at most recent followup compared with preoperative levels (Table 2). Of these patients, only two were not participating in any sports: an 18-year-old woman was noted to be too busy for sports and a 45-year-old woman reported persistent symptoms. An 18-year-old woman changed the type of activity as a result of increased pain after surgery. The other patients reduced the frequency without changing the type of activity after surgery.
Fig. 1.
The distributions of UCLA activity scores at preoperative and at least 2-year followup are shown.
Table 2.
Patients with lower UCLA activity levels after surgery
| Sex | Age (years) | BMI (kg/m2) | Previous hip surgery | Surgical procedure | Postoperative complications | Preoperative scores | 1-year scores | Minimum 2-year scores | Preoperative activity | Postoperative activity | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| UCLA | WOMAC | UCLA | WOMAC | UCLA | WOMAC | ||||||||
| F | 43.6 | 24.7 | 0 | PAO + FHNO | – | 7 | 10 | 5 | 4 | 5 | 8 | Running | No sports |
| F | 29.3 | 28.4 | HA | PAO | – | 8 | 11 | 9 | 2 | 6 | 3 | Gymnastics | Gymnastics |
| F | 16.6 | 20.3 | 0 | PAO + FHNO | – | 10 | 5 | 7 | 4 | 5 | 10 | Hockey | Snowboarding |
| F | 36.9 | 23.3 | 0 | PAO + FHNO | – | 8 | 3 | 4 | 0 | 4 | 0 | Hiking | Hiking |
| F | 23.8 | 22.4 | HA | PAO | – | 9 | 9 | 7 | 8 | 8 | 6 | Yoga | Yoga |
| M | 19.9 | 24.4 | 0 | PAO + FHNO | – | 9 | 5 | 9 | 1 | 8 | 2 | Running | Running |
| F | 17.5 | 22.7 | CBG femur | PAO | NPN | 10 | 9 | 10 | 0 | 8 | 0 | Softball | Softball |
| F | 16.5 | 20.3 | 0 | PAO + ITO | – | 8 | 8 | 6 | 3 | 6 | 2 | Gym | No sports |
| F | 14.3 | 16.2 | ORIO | PAO + ITO | – | 9 | 5 | 9 | 0 | 8 | 0 | Running | Running |
| F | 29.8 | 23 | 0 | PAO | – | 10 | 8 | 8 | 5 | 9 | 3 | Hiking | Hiking |
BMI = body mass index; F = female; m = male; HA = hip arthroscopy; CBG femur = curettage with bone graft of a unicameral bone cyst of the proximal femur; ORIO = open reduction and intertrochanteric osteotomy; PAO = periacetabular osteotomy; FHNO = femoral head-neck osteochondroplasty; ITO = intertrochanteric osteotomy; NPN = neurapraxia peroneal nerve.
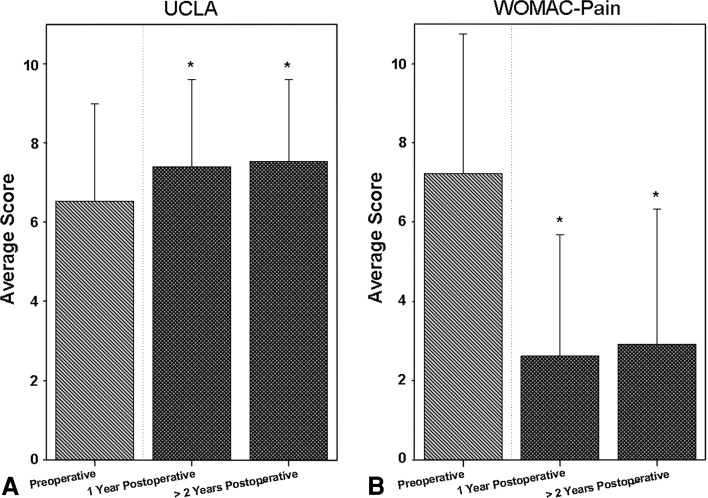
There was a concurrent decrease in WOMAC pain scores at 1 and 2 years followup (Fig. 2). Mean preoperative WOMAC pain scores were higher than mean WOMAC pain scores assessed at 1 year (mean difference = 4.6 ± 3.8; p = 0.014) and at least 2 years (mean difference = 4.3 ± 3.8; p = 0.005).
Fig. 2A–B.
Bar plots of (A) the UCLA and (B) WOMAC pain are shown for preoperative, 1-year postoperative, and at least 2-year postoperative scores. The asterisks indicate significant comparisons of scores at each time as compared with preoperative scores based on Student’s paired t-test (p < 0.05).
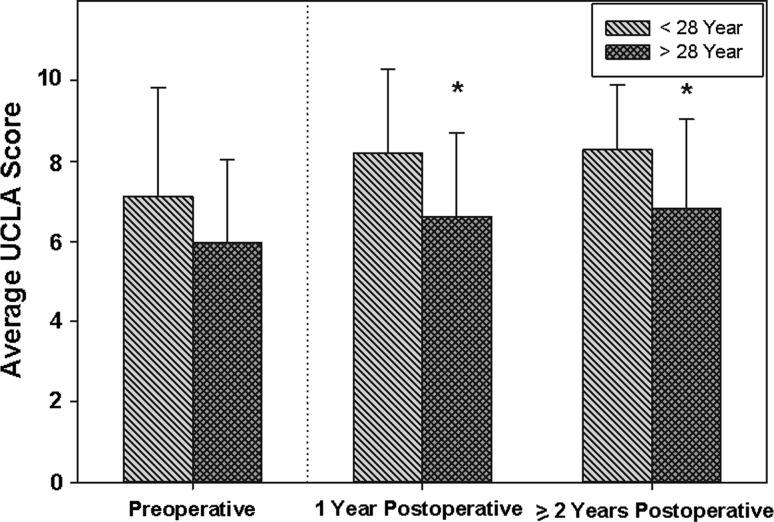
Univariate analysis of factors associated with high UCLA score at 1 year identified young age, high preoperative UCLA score, and low postoperative WOMAC pain score as having significant associations (Table 3). These were applied to a multivariate linear regression model, which suggested that age and preoperative UCLA score were significantly related to outcome. Older age was associated with decreased UCLA scores at 1 year postsurgery after adjusting for preoperative UCLA score and WOMAC pain (β = −0.1; p = 0.008). Preoperative UCLA score had a positive association with UCLA score at 1 year independent of age and WOMAC pain (β = 0.1; p = 0.007). When the same factors were used to compare preoperative UCLA scores with those from a minimum 2 years postsurgery, the significant associations identified at 1 year were maintained (Table 4). Older age at surgery was independently associated with UCLA scores at minimum 2 years after adjusting for preoperative UCLA score and WOMAC score taken 2 years after surgery (β = −0.05; p = 0.044). When comparing UCLA scores with time in patients older than 28 years (the median age of the study population) with those younger, the younger age group had a significantly higher UCLA score at 1 year (mean difference = 1.6; 95% CI = 0.4–2.8; p = 0.009) and at minimum 2 years postoperatively (mean difference = 1.5; 95% CI = 0.4–2.6; p = 0.01) (Fig. 3). High preoperative UCLA score and lower WOMAC pain scores postoperatively were positively associated with higher UCLA score at minimum 2 years postoperatively (β = 0.3, p = 0.013; and β = −0.2, p = 0.05, respectively).
Table 3.
Factors associated with UCLA score at 1 year postsurgery (N = 51)
| Variable | UCLA activity score at 1 year | |||
|---|---|---|---|---|
| Univariate | Multivariable* | |||
| β | p value | β | p value | |
| Age (years) | −0.08 | 0.004 | −0.07 | 0.008 |
| Male (%) | 0.66 | 0.57 | ||
| BMI (kg/m2) | −0.08 | 0.30 | ||
| Preoperative UCLA score | 0.46 | < 0.001 | 0.3 | 0.007 |
| Δ WOMAC pain | 0.07 | 0.44 | ||
| WOMAC pain at 1 year | −0.28 | 0.006 | −0.21 | 0.11 |
| Previous pelvic surgery | 0.48 | 0.48 | ||
| Complication | −1.15 | 0.16 | ||
| Preoperative LCEA | 0.01 | 0.99 | ||
| Preoperative ACEA | 0.01 | 0.92 | ||
| Preoperative Tönnis angle | 0.01 | 0.93 | ||
* Variables significant in univariate analysis were included in multivariable analysis; BMI = body mass index; Δ = WOMAC pain 1 year postoperatively–preoperatively; ACEA = anterior center-edge angle; LCEA = lateral center-edge angle.
Table 4.
Factors associated with UCLA score at least 2 years postsurgery (N = 51)
| Variable | UCLA activity score at 2 years | |||
|---|---|---|---|---|
| Univariate | Multivariable* | |||
| β | p value | β | p value | |
| Age (years) | −0.07 | 0.007 | −0.05 | 0.044 |
| Male (%) | 0.24 | 0.83 | ||
| BMI (kg/m2) | −0.09 | 0.22 | ||
| Preoperative UCLA score | 0.38 | 0.001 | 0.28 | 0.013 |
| Δ WOMAC pain | −0.02 | 0.79 | ||
| WOMAC pain at 2 years | −0.22 | 0.008 | −0.15 | 0.050 |
| Previous pelvic surgery | 0.48 | 0.46 | ||
| Complication | −0.64 | 0.40 | ||
| Preoperative LCEA | −0.01 | 0.89 | ||
| Preoperative ACEA | −0.01 | 0.92 | ||
| Preoperative Tönnis angle | −0.01 | 0.75 | ||
* Variables significant in univariate analysis were included in multivariable analysis; BMI = body mass index; Δ = WOMAC pain 2 years postoperatively–preoperatively; ACEA = anterior center-edge angle; LCEA = lateral center-edge angle.
Fig. 3.
Bar plots of the UCLA activity score evaluated preoperative, 1 year postoperative, and at least 2 years postoperatively stratified by median age are shown. The asterisks denote significant differences in average UCLA activity score between age strata at 1 year and at least 2 years postoperatively based on Student’s t-test (p < 0.05).
The severity of acetabular dysplasia, analyzed as LCEA, ACEA, or Tönnis [19] angle measured as continuous variables, was not a predictor of activity scores at 1 year or at minimum 2 years after surgery by univariate analysis. This was found despite improvement in the radiographic parameters after surgery when compared with the preoperative assessment. The LCEA improved an average of 14.8° (95% CI = 11.5–18.1; p < 0.001), the ACEA improved an average of 13.1° (95% CI = 9.6–16.7; p < 0.001), and the Tönnis [19] angle improved an average of 11.2° (95% CI = 11.2–17.3; p < 0.001). Thirty hips (59%) had Tönnis [19] osteoarthritis Grade 0 and 21 (41%) had Grade 1 before surgery. The OA grade did not progress in 49 (96%) of the hips. In two (4%) hips, there was radiographic progression from Grade 0 to Grade 1.
Ten patients experienced complications. Three patients had localized dysesthesia in the lateral femoral cutaneous nerve distribution, which required no additional treatment (Grade I). Three patients had transient peroneal nerve palsy treated with oral gabapentin (Grade II). There were three Grade III complications; two patients had wound hematomas develop that were treated with surgical drainage and oral antibiotics, although cultures were negative in both cases. One patient (a 43-year-old woman) had a symptomatic nonunion of the ischium osteotomy requiring plating and bone graft 1 year after PAO. Although this patient did not have symptomatic improvement, her level of activity improved from a UCLA activity score of 2 to a score of 6 at 3 years of followup. One patient (a 44-year-old woman) had a pulmonary embolism develop (Grade IV) 7 days after surgery requiring intensive care unit treatment. The occurrence of a complication was not a significant predictor of UCLA activity score at 1 year (p = 0.16) or at minimum 2 years (p = 0.40) postoperatively.
Discussion
There is limited evidence in the literature regarding the level of activity patients can expect to achieve after PAO and which factors may impact resumption of, or improvement on, preoperative activity levels. Physical activity is an important concern for young adults undergoing hip surgery. Therefore, in this study of 51 patients undergoing PAO for the treatment of symptomatic hip dysplasia, we sought to determine the level of physical activity assessed by the UCLA scale and pain assessed by the WOMAC index at three distinct times: before PAO, at 1 year postoperatively, and at least 2 years postoperatively. We also wanted to identify predictive factors for the level of physical activity achieved after a PAO.
There are several limitations to the current study. First, information about specific physical activities was collected retrospectively. We therefore could not analyze the influence of activity type on postoperative activity level. In addition, we have limited information on patients’ specific reasons for their limitations in activity other than the variables measured, which could have influenced the change in activity level after surgery. However, serial UCLA scores were prospectively collected at each clinic visit, allowing for comparative analyses of the activity levels. Notably, the UCLA scale does not detail the intensity of physical activity. However, it has been tested for validity and shown to correlate with objective measurements of physical activity as assessed by a pedometer [25]. In addition, the short-term followup in our study precludes any conclusions or recommendations related to the risk of progressive joint damage after PAO based on activity level. However, the available data did show PAO can alleviate pain and improve the level of physical activity 1 year after surgery, which is sustained at an average of 2.4 years.
In this series, the mean postoperative UCLA and WOMAC pain scores, at 1 year and at minimum 2 years followup, substantially improved when compared with the preoperative scores. When considering pain relief and level of daily function as assessed by the WOMAC, previous studies have shown PAO is an effective surgical option for treatment of symptomatic hip dysplasia in the young adult [13, 20]. However, a previous study suggests the WOMAC may not be suitable for predicting the amount of physical activity after hip surgery, which would require the use of an additional outcome measure [22]. To our knowledge, only one previous investigation has assessed physical activity in patients with symptomatic hip dysplasia undergoing PAO [21]. van Bergayk and Garbuz [21] reported objective improvement in participation in sports activities as measured by the Tegner score in 21 patients after PAO. All but one patient in their cohort had an increase in activity level. In the current series there was an average improvement of 1 point on the UCLA scale with a mean UCLA score of 7.5 at 1 year after surgery and similar results at minimum 2 years. At most recent followup, only 10% of patients had scores of 4 or lower, whereas the majority of patients (61%) were participating in either very active or impact sports (scores of 8 or higher). The Tegner score was designed to assess activity after knee surgery. We believe the UCLA scale is a more appropriate tool to measure activity level after PAO. It has been shown to discriminate between insufficiently and sufficiently active patients and to have the greatest reliability in patients with hip disorders when compared with other instruments, including the Tegner score [14].
Difficulties with and the wish to return to recreational activities often are cited by patients with hip pain as an important disability [3, 24]. Symptomatic hip dysplasia in healthy, active young adults is commonly diagnosed without advanced OA. These patients may wish to resume or improve their physical activities after surgical treatment. Our data suggest that PAO can provide pain relief and improvement in the level of activity in symptomatic young adults with hip dysplasia in the short term while preserving the native hip.
In this study, multivariate regression analysis identified age and preoperative level of physical activity as independent predictors of postoperative activity level at 1 year and minimum 2-year followups. Pain at minimum 2-year followup was moderately associated with lower UCLA scores. Our findings are in line with previous studies that showed physical activity is influenced by age in the general population [7, 15]. We showed the role of age as predictive of UCLA score after PAO; at all three times, patients younger than 28 years had considerably higher levels of activity than patients older than 28 years. Our data also showed that the higher preoperative activity level was associated with an increased activity level 1 year and at minimum 2 years after surgery. Multivariate analysis showed this effect was independent of age and WOMAC pain. To our knowledge, our study is the first to investigate predictor factors for activity level after PAO. In this study, patients with lower preoperative activity scores remained less active after surgery.
Lower postoperative pain assessed by the WOMAC index also was found to be a predictive factor for higher postoperative activity level by univariate analysis. However, multivariate regression analysis did not replicate this as a major finding. At minimum 2 years postoperative followup, lower WOMAC pain scores were only moderately associated with higher UCLA scores. Our cohort’s reported improvement in mean pain scores after PAO is in line with previous retrospective studies [5, 13, 17, 20]. Although improvement in hip pain and function are the central goals of PAO, a previous study suggests approximately 10% of patients with symptomatic hip dysplasia undergoing PAO will experience persistent pain in the hip after surgery [13]. We found the level of pain at most recent followup was a predictor for the level of activity after PAO, but improvement in pain, assessed by change in WOMAC pain scores, was not a predictor. Therefore, our data suggest that even if patients obtain symptomatic improvement, it is the level of pain at followup that more substantially influences regaining or improving the activity level after surgery.
Our study of 51 patients undergoing PAO for treatment of symptomatic hip dysplasia showed the level of physical activity assessed by the UCLA scale improved after surgery. Age at the time of surgery and preoperative level of physical activity were strong independent predictors of the level of physical activity at 1 year and at minimum 2 years after surgery. Pain assessed by WOMAC index was a moderate predictor for the level of activity at most recent followup. The younger and more active a patient was before surgery and the lower the pain was at final followup, the greater the activity level at 1 year after surgery and at minimum followup of 2 years. A successful outcome of PAO should not only include pain relief and improvement in function, but also improvement in activity level for the active young adult with symptomatic hip dysplasia. The data presented here may be useful to counsel patients for the level of activity they can expect after PAO.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at Children’s Hospital Boston, Boston, MA, USA.
References
- 1.American College of Sports Medicine Position Stand The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol. 1986;5:231–241. doi: 10.1007/BF02032362. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright Rw. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 7.Fleg JL, Morrell CH, Bos AG, Brant LJ, Talbot LA, Wright JG, Lakatta EG. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112:674–682. doi: 10.1161/CIRCULATIONAHA.105.545459. [DOI] [PubMed] [Google Scholar]
- 8.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 9.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 10.Katz MH. Multivariable Analysis: A Practical Guide for Clinicians and Public Health Researchers. New York, NY, USA: Cambridge University Press; 2011. [Google Scholar]
- 11.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 12.Lequesne M, de Sèze S. [False profile of the pelvis: a new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies] [in French] Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed] [Google Scholar]
- 13.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 14.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958–965. doi: 10.1007/s11999-008-0358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sallis JF, Owen N. Physical Activity & Behavioral Medicine. Thousand Oaks, CA, USA: Sage; 1998. [Google Scholar]
- 16.Sink EL, Beaule PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132–1136. doi: 10.2106/JBJS.J.00794. [DOI] [PubMed] [Google Scholar]
- 17.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Surgeon General’s report on physical activity and health. From the Centers for Disease Control and Prevention. JAMA. 1996;276:522. [PubMed]
- 19.Tönnis D. General radiograph of the hip joint. In: Tönnis D, editor. Congenital Dysplasia, Dislocation of the Hip. New York, NY, USA: Springer; 1987. pp. 100–142. [Google Scholar]
- 20.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 21.van Bergayk AB, Garbuz DS. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br. 2002;84:339–343. doi: 10.1302/0301-620X.84B3.12421. [DOI] [PubMed] [Google Scholar]
- 22.Wagenmakers R, Stevens M, van den Akker-Scheek I, Zijlstra W, Groothoff JW. Predictive value of the Western Ontario and McMaster Universities Osteoarthritis Index for the amount of physical activity after total hip arthroplasty. Phys Ther. 2008;88:211–218. doi: 10.2522/ptj.20060321. [DOI] [PubMed] [Google Scholar]
- 23.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83:28–38. [Google Scholar]
- 24.Wright JG, Rudicel S, Feinstein AR. Ask patients what they want: evaluation of individual complaints before total hip replacement. J Bone Joint Surg Br. 1994;76:229–234. [PubMed] [Google Scholar]
- 25.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]