Abstract
Background
Diffuse-type pigmented villonodular synovitis (PVNS) has a high local recurrence rate and as such can lead to erosive destruction of the involved joint. Multiple surgical modalities exist, but it is unknown which technique best minimizes local recurrence and surgical morbidity.
Questions/purposes
We compared recurrence rates, arthritis progression, and complications between arthroscopic and open modalities for diffuse PVNS of the knee.
Methods
We retrospectively identified 103 patients with PVNS treated between 1993 and 2011. Of these, 48 had diffuse-type PVNS of the knee treated by all-arthroscopic, open posterior with arthroscopic anterior, or open anterior and open posterior synovectomy. We recorded patient demographics, treatment profiles, recurrence rates, and arthritic progression. Minimum followup was 3 months (median, 40 months; range, 3–187 months).
Results
Recurrence rates were lower in the open/arthroscopic group compared with the arthroscopic or open/open groups: 9% versus 62% versus 64%, respectively. Arthritic progression occurred in 17% of the total study group with 8% going onto total knee arthroplasty within the followup period. We detected no difference between groups with regard to arthritic progression or progression to arthroplasty. The most common complication was hemarthrosis, which we drained in three patients (6% of the total study group), but there were no detectable differences between groups.
Conclusion
Open posterior with arthroscopic anterior synovectomy is a viable, comprehensive approach to diffuse PVNS of the knee and provides both low recurrence rates and a low postoperative complication profile. Greater numbers of recurrences may be partially explained in the arthroscopic group by technical challenges associated with posterior arthroscopic synovectomy and in the open/open group by selection bias toward more aggressive disease.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Pigmented villonodular synovitis (PVNS) is a rare proliferative disease of the synovial lining whose cellular origins are most likely to be neoplastic [10, 12, 20]. It has an estimated incidence of two cases per million of the general population [13]. The condition occurs along a spectrum of severity but is generally grouped into localized/nodular and diffuse forms. Between nodular and diffuse types and among all anatomic locations, diffuse PVNS of the knee is the most common [18]. It may cause swelling, pain, and stiffness and can produce rapid destruction of articular cartilage leading to early arthritis.
Surgical removal of all diseased synovial lining remains the standard of care for disease eradication in diffuse PVNS of the knee. Primary or adjuvant use of external beam or intraarticular radiation as a treatment modality has never been shown to be superior to surgery alone [1, 3, 15, 20]. Nevertheless, historical attempts at complete surgical synovectomy have been associated with recurrence rates as high as 30% to 46% [2, 7]. With meticulous modern techniques reported, recurrence rates have improved to the range of 8% to 20% [3, 5, 6, 19, 21] but local control remains a problem.
Although surgical synovectomy has been proven effective, the type of resection required remains controversial. Anterior and posterior open arthrotomy and synovectomy under direct visualization have been performed with recurrence rates similar to the best reported for this condition [3, 6, 19]. Open techniques are especially important in the presence of extraarticular extension of disease, which cannot be accessed with an arthroscope [3, 14]. Other authors have reported similar recurrence rates with all-arthroscopic total synovectomy using anterior and posteromedial arthroscopy portals, 30° and 70° arthroscopic lenses, and transcondylar notch views [5, 14, 21]. Still others have reported similar recurrence rates combining the two techniques using a posterior open and anterior arthroscopic approach to minimize technical difficulty and take advantage of the benefits of each [19]. Although recurrence rates across these series are somewhat similar, most are case series only and do not directly compare differences in recurrence rates or complications for the various approaches to total synovectomy. In addition, indications for treatment modalities such as open versus arthroscopic synovectomy are unclear. Although extracapsular extension of disease is well described as an absolute contraindication to arthroscopic synovectomy, other guidelines for treatment are less clear and depending on the treating center or study group, the same patient might receive vastly different approaches. The use of radiotherapy in some studies further confounds the picture [3]. The gold standard approach for achieving the lowest possible recurrence rates and morbidity remains unclear.
Therefore we compared (1) recurrence rates; (2) arthritic progression; and (3) complications for all-arthroscopic, open posterior with arthroscopic anterior, and open posterior with open anterior synovectomies.
Patients and Methods
We identified all 103 patients with PVNS treated by a heterogeneous group of surgeons at our tertiary center from 1993 to 2011. The treating surgeons included musculoskeletal oncologists (66%), adult reconstruction surgeons (13%), and sports medicine (21%) specialists. Data were collected by two reviewers (MC, JY) using the electronic chart and included 50% auditing of the other reviewer’s data set to minimize inaccuracies and bias. We identified 48 patients with diffuse-type PVNS of the knee who were included for study. Other inclusion criteria included an index synovectomy performed at our institution with pathologic tissue-based confirmation of the diagnosis as well as confirmation based on surgical and radiographic findings. Referrals from other institutions were allowed into the study as long as they had not yet undergone synovectomy and included eight (17%) patients referred for synovectomy after receiving the diagnosis of PVNS during diagnostic arthroscopy and biopsy at an outside institution. We excluded patients with focal PVNS, PVNS of joints other than the knee, and patients referred from other institutions after failed synovectomy. Our 48 patients were divided into three groups according to treatment: those whose index operation involved all-arthroscopic synovectomy (“all-arthroscopic,” n = 26, 42% performed by a musculoskeletal oncologist, 38% by a sports medicine specialist, 19% by an adult reconstruction specialist/generalist), open posterior with arthroscopic anterior synovectomy (“open/arthroscopic,” n = 11, 91% performed by a musculoskeletal oncologist, 9% by an adult reconstruction specialist/generalist), or open anterior with open posterior synovectomy (“open/open,” n = 11, 100% performed by a musculoskeletal oncologist). Patients were analyzed according to intention-to-treat principles using the surgical method of the index synovectomy; change of method for revision procedures was not taken into account in this analysis. The indications for all-arthroscopic surgery were (1) the absence of extracapsular disease; (2) the absence of major degenerative changes; and (3) treating surgeon comfort with the all-arthroscopic technique including posterior portals with transcondylar notch views and use of the 70° arthroscope. The indications for open posterior with arthroscopic anterior synovectomy were: (1) presence of extracapsular posterior disease; and (2) treating surgeon comfort with both open posterior and arthroscopic anterior approaches. The indications for open anterior with open posterior synovectomy were: (1) anterior or posterior extracapsular disease; and (2) treating surgeon preference for open as opposed to arthroscopic approaches. Adjunct radiotherapy was not used in any case. Four patients were lost to followup, from 2 to 8 weeks postoperatively, all the result of transition of care to a distant institution. Minimum followup was 3 months (median, 40 months; range, 3–187 months). No patients were recalled specifically for this study; all data were obtained from review of the medical record.
We recorded patient demographics and surgical treatment profiles. For categorical variables such as sex, we used a two-degree of freedom chi square test to compare the three groups. For continuous variables such as age at index surgery, time from symptom onset to index surgery, and baseline arthritis grade, we used analysis of variance to compare groups. The groups were similar with regard to sex, age at diagnosis, mean followup time, time from symptom onset to index synovectomy, and baseline arthritis grade (Table 1).
Table 1.
Group demographics are compared for the open/arthroscopic, all-arthroscopic, and open posterior/open anterior cohorts using analysis of variance
| Demographic | Open/arthroscopic | Arthroscopic | Open/open | p value |
|---|---|---|---|---|
| Male (number) | 3 | 9 | 4 | 0.90 |
| Female (number) | 8 | 17 | 7 | 0.90 |
| Age at index (years) | 34 | 32 | 24 | 0.053 |
| Time from index surgery to most recent followup (months) | 41 | 70 | 84 | 0.26 |
| Time from symptom onset to index synovectomy (months) | 55 | 32 | 22 | 0.39 |
| Baseline arthritis (Outerbridge grade) | 0.9 | 0.9 | 0.3 | 0.39 |
Use of tourniquet control for open or arthroscopic procedures was variable and surgeon-dependent. The all-arthroscopic synovectomy technique was performed by all surgeons using standard anteromedial and anterolateral portals with or without a superolateral outflow portal. Additionally, for a portion of our arthroscopic cohort (38%), a posteromedial portal, transcondylar notch views, and a 70° arthroscope were used according to the technique of Gillquist et al. [8]. In the remainder of cases in which an MRI demonstrated diffuse disease without posterior knee involvement, the surgeon elected to perform anterior synovectomy alone through standard anterior portals with a 30° lens. Noncautery arthroscopic shaver devices were used to perform complete synovectomy of the diseased synovial lining.
Posterior open synovectomy was performed in a similar fashion to that described in detail by Chin et al. [3]. Although the exact technique was dictated by disease extent and location, the approach most commonly used involved a longitudinal posterior approach with oblique angulation through the flexion crease, mobilization of both medial and lateral heads of the gastrocnemius, and medial and lateral arthrotomies with excision of diseased tissue. Extracapsular disease was meticulously dissected from the midline neurovascular elements as necessary. Extensile distal/medial-based extracapsular dissection through a medial gastrocnemius-medial soleus origin takedown was undertaken where necessary.
Anterior open synovectomy was performed using a standard midline skin incision and medial parapatellar arthrotomy to allow eversion of the patella and inspection of both medial and lateral gutters in addition to the anterior synovial lining. When performed as part of our open posterior/open anterior synovectomy protocol, it was always performed second, after the open posterior approach.
Postoperative protocols involved early mobilization with physical therapy on the first postoperative day without bracing or continuous passive motion devices.
Need for revision was based on clinical symptoms of pain and swelling, although MRI documentation of disease progression accompanied the clinical deterioration in 43 of the 48 patients (90%). Recurrence was defined in this retrospective study as the need for revision synovectomy based on clinical symptoms and MRI with pathologic confirmation of residual disease taken at the time of revision.
Surgeon patterns of surveillance were variable but the majority of cases were followed with clinical examinations at 3, 6, and 12 months with yearly visits thereafter and MRI surveillance at 3 to 6 months postindex synovectomy and every 6 months thereafter depending on clinical suspicion. Principle outcome measures included recurrence of disease, arthritic progression, and complications. Arthritic progression was measured based on two methods. First, where direct inspection of articular cartilage health over multiple time points was possible (as in recurrence cases), we recorded Outerbridge classification of cartilage health [16] as noted by the surgical team on direct inspection at the time of index or revision synovectomy. Second, if serial weightbearing flexion radiographic studies over time were noted by the treating surgeon to have developed a new decrease in joint space or new bony erosions, patients were considered to have arthritic progression. Finally, patients who underwent TKA after synovectomy were considered to have had arthritic progression as a result of their PVNS disease.
We determined differences in recurrence rates by two methods. First, we used two-degree-of-freedom Fisher’s exact test to compare absolute rates of single and multirecurrence among the three groups. In addition, we used Kaplan-Meier survival analysis with Mantel-Cox log rank test to compare recurrence-free survival times among the three groups. We determined differences in absolute rate of arthritic progression within the followup period including the need for arthroplasty using the two-degree-of-freedom Fisher’s exact test. Likewise, we determined differences in complication rates using the two-degree-of-freedom Fisher’s exact test. SPSS Statistics 19 (IBM, Armonk, NY, USA) was used for all statistical calculations.
Results
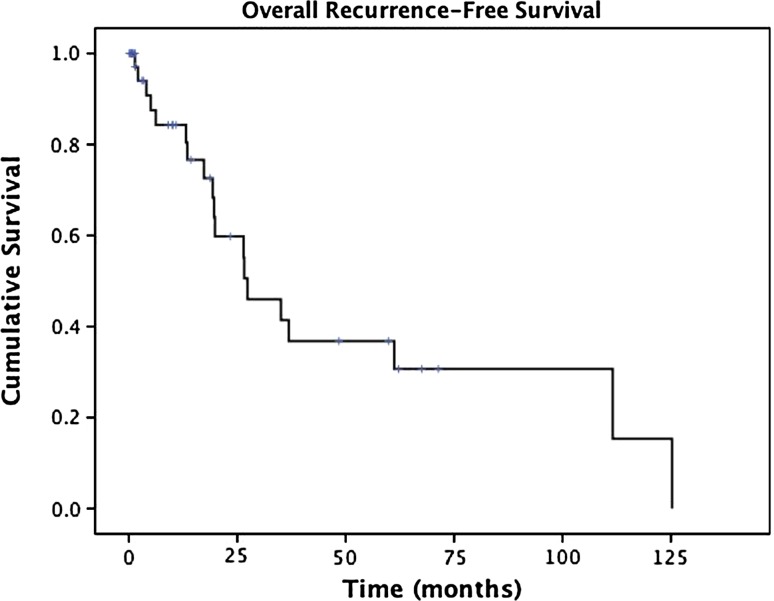
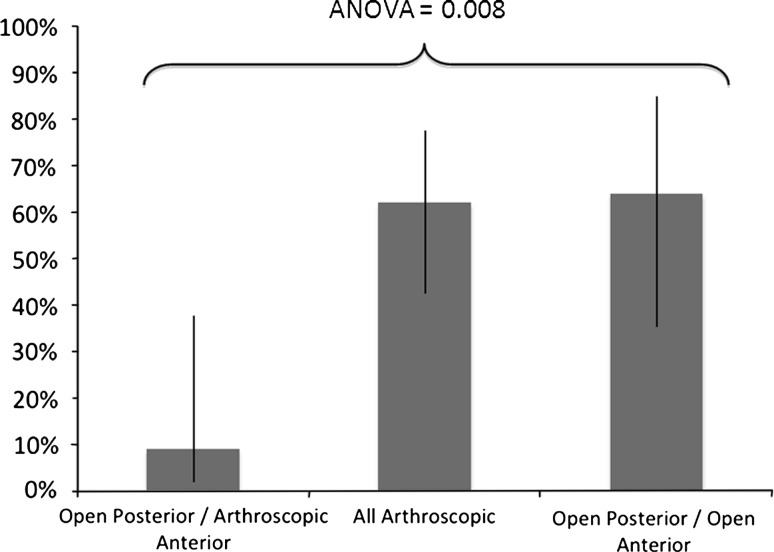
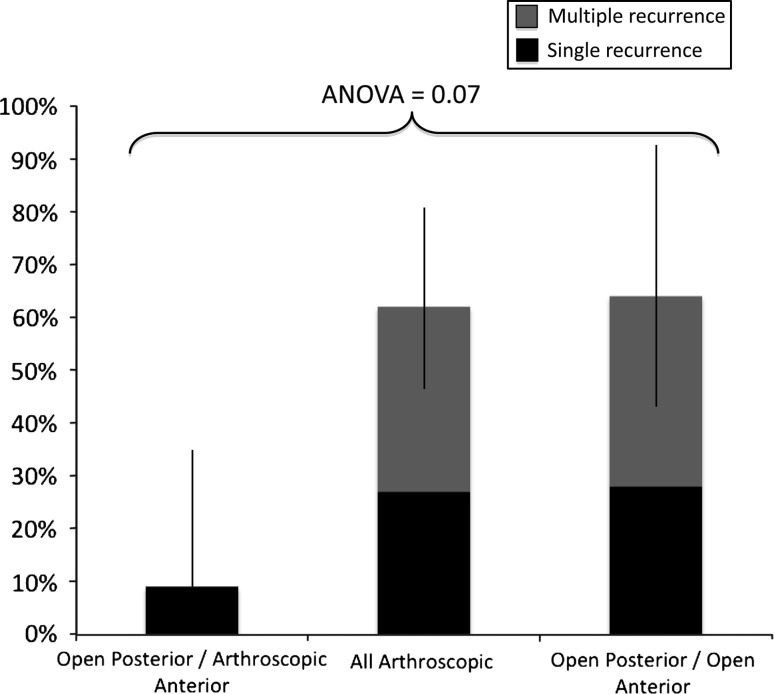
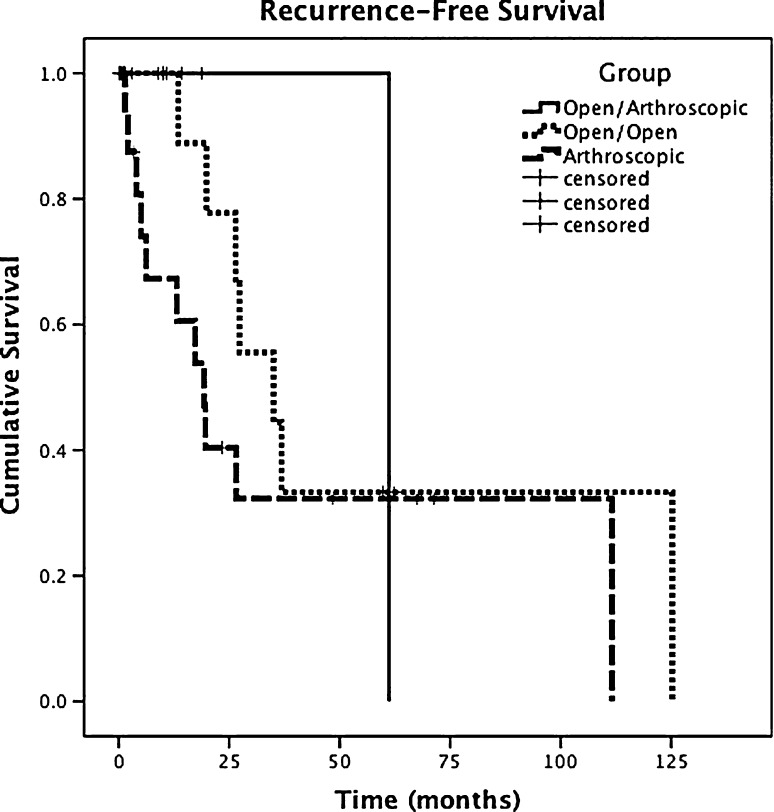
The overall rate of recurrence for the entire diffuse PVNS of the knee study group was 50% with 27% of the series experiencing multiple recurrences, defined as two or more recurrence episodes requiring revision synovectomy. Recurrence occurred at a median 27 months (95% confidence interval, 15–40 months; standard error, 6.3 months) from the index synovectomy (Fig. 1). The overall recurrence rate for the open/arthroscopic group was lower (p = 0.008) than for the all-arthroscopic or open/open groups (9% versus 62% versus 64%, respectively; Fig. 2). In addition, separating those patients who had more than one recurrence, we found that the multirecurrence rate for the open/arthroscopic group showed a trend (p = 0.07) toward being lower than that in the arthroscopic or open/open groups (0% versus 35% versus 36%, respectively; Fig. 3). Kaplan-Meier analysis (Fig. 4) of the duration of recurrence-free survival demonstrated no difference (p = 0.294) between groups.
Fig. 1.
This Kaplan-Meier survival curve for the entire series of 48 knees with diffuse PVNS demonstrates a median recurrence-free survival of 27 months (95% CI, 15–40 months) with most recurrences occurring within the first 2 years.
Fig. 2.
We found a lower recurrence rate (p = 0.008) in the open/arthroscopic (9%) group as compared with the all-arthroscopic (62%) and open posterior/open anterior (64%) groups. ANOVA = analysis of variance. 95% confidence intervals are represented by vertical bars for each group.
Fig. 3.
Multiple recurrence rates showed a trend toward being lower (p = 0.07) in the open/arthroscopic (0%) group as compared with the all-arthroscopic (35%) and open posterior/open anterior (36%) groups. ANOVA = analysis of variance. 95% confidence intervals are represented by vertical bars for each group.
Fig. 4.
A Kaplan-Meier survival analysis with Mantel-Cox log-rank test demonstrated there was no difference (p = 0.294) in the recurrence-free survival time for the open/arthroscopic, arthroscopic, and open posterior/open anterior groups.
Baseline arthritis at the time of index synovectomy was absent or Grade 0 in 66%, Grade 1 in 2%, Grade 2 in 15%, Grade 3 in 10%, and Grade 4 in 7%. Arthritic progression from baseline occurred in 17% of cases. Although seven of eight of these cases of progression occurred in the all-arthroscopic group, a difference between groups was not detected (open/arthroscopic, 9%; all-arthroscopic, 23%; open/open, 0%; p = 0.16). Seven of eight arthritic progression cases were associated with recurrence; five of eight had more than one recurrence. Eight percent (n = 4) of cases eventually went on to TKA at a mean of 81 months from the index synovectomy. Although all of these were from the all-arthroscopic group, we detected no difference between groups (open/arthroscopic, 0%; all-arthroscopic, 15%; open/open, 0%; p = 0.16).
In the entire study group, perioperative complications were uncommon (Table 2). Hemarthrosis with subsequent drainage was most common with three occurrences (6%, two cases in the all-arthroscopic group, one case in the open/arthroscopic group). Two of the three patients with hemarthroses underwent open drainage and the third needle aspiration. We also found one case of uncomplicated deep vein thrombosis in the all-arthroscopic group, one case of a small wound dehiscence treated nonoperatively in the open/open group, and one case of arthrofibrosis requiring manipulation in the open/arthroscopic group. There was no difference among the three groups with regard to any specific complication (all comparisons, p > 0.05) or overall complication rate (p = 0.79).
Table 2.
Complication profiles are compared for the open/arthroscopic, all-arthroscopic, and open posterior/open anterior cohorts*
| Complication | Open/arthroscopic | Arthroscopic | Open/open | Resolution |
|---|---|---|---|---|
| Hemarthrosis | X | Operative drainage | ||
| Hemarthrosis | X | Operative drainage | ||
| Hemarthrosis | X | Resolved with aspiration | ||
| Deep vein thrombosis | X | Therapeutic anticoagulation | ||
| Arthrofibrosis | X | Required manipulation under anesthesia; persistent flexion contracture | ||
| Wound dehiscence | X | Resolved with dressing changes |
* There were no differences among the three groups with regard to any individual complication nor was there a difference among the three groups with regard to the presence or absence of any complication (p = 0.79).
Discussion
Diffuse PVNS of the knee remains a clinical challenge because of high rates of local recurrence and propensity for pain, swelling, and arthritic progression. Total synovectomy is accepted as the standard of care, but the literature describes multiple methods of accomplishing this, including open, arthroscopic, or combined techniques (Table 3). We therefore compared these surgical methods to determine differences in recurrence rate, rate of arthritic progression, and complication profiles.
Table 3.
Recent publications involving diffuse PVNS of the knee are compared with regard to study design, patient treatment, and outcome measures such as recurrence, arthritic progression, and complications
| Author | Year | Technique | Patients | Adjuvant radiotherapy | Recurrence rate | Arthritic progression | Progression to arthroplasty | Complications | Followup (years) |
|---|---|---|---|---|---|---|---|---|---|
| De Ponti et al. [5] | 2003 | All- arthroscopic | 7 | No | 20% | NR | NR | None | 5.0 |
| All-arthroscopic† | 8 | No | 75% | NR | NR | None | |||
| Ogilvie-Harris et al. [14] | 1992 | All-arthroscopic | 11 | No | 9% | 16% | 10% | NR | 4.5 |
| All-arthroscopic† | 9 | No | 56% | NR | |||||
| Zvijac et al. [21] | 1999 | All- arthroscopic | 12 | No | 14% | NR | NR | 8% stiffness requiring MUA | 3.5 |
| Flandry et al. [6] | 1994 | Open/open | 25 | No | 8% | 48% | NR | 32% stiffness requiring MUA | 4.8 |
| Chin et al. [3] | 2002 | Open/open‡ | 40 | 75% | 18% | 10% | 8% stiffness requiring MUA; 3% CRPS, 10% superficial wound infection | 5.0 | |
| Sharma and Cheng [19] | 2009 | Open/open | 16 | No | 19% | NR | NR | NR | 6.2 |
| Open/arthroscopic | 8 | No | 25% | NR | NR | NR | |||
| All-arthroscopic* | 13 | No | 92% | NR | NR | NR | |||
| Current study | 2012 | Open/open | 11 | No | 64% | 0% | 0% | 9% superficial wound infection | 3.3 |
| Open/arthroscopic | 11 | No | 9% | 9% | 0% | 9% hemarthrosis, 9% stiffness requiring MUA | |||
| All-arthroscopic* | 26 | No | 62% | 23% | 15% | 8% hemarthrosis, 4% DVT |
* Portions had subtotal synovectomy; †all had subtotal synovectomy; ‡all patients were revision synovectomy cases; PVNS = pigmented villonodular synovitis; NR = not reported; MUA = manipulation under anesthesia; CRPS = chronic regional pain syndrome; DVT = deep venous thrombosis.
Readers should note the limitations of our study. First, given the rarity of this condition, the study suffers from low patient numbers and underpowered statistical analysis. This is especially a problem in the multiple areas where we found no difference; readers should interpret these findings with caution. Second, we theorize that recurrence in PVNS may be based on the original extent of disease or subtype biology of the neoplasm. These factors were not taken into account in this analysis. Disease extent is of particular issue; because extracapsular disease is an absolute contraindication for arthroscopic synovectomy, the arthroscopic group could be biased toward lesser extent of disease. However, the all-arthroscopic group actually had higher rates of recurrence, and so the bias of different disease extent between groups is not likely to play a major role. Third, this is a retrospective analysis that is subject to bias arising from loss of followup (8%) and heterogeneous followup protocols as well as variations in treatment between surgeons. Although there was treatment variance between surgeons who might prefer arthroscopic, open, or combined techniques, the end goal of total synovectomy remains the same regardless of technique or surgeon. Finally, in analyzing recurrence in this study, we point out that the definition of recurrence has not been standardized. Most authors use a clinical definition based on swelling and pain [5, 14] but we believe tissue diagnosis and MRI findings are also important. In evaluating the literature, a purely clinical definition may underestimate recurrence, but reliance on MRI alone overestimates the true rate resulting from identification of subclinical disease or false-positives resulting from postsurgical changes. In practice, we combine patient history and physical examination with MRI findings to create an individual clinical picture when evaluating recurrence and deciding to proceed with revision synovectomy. We believe screening MRI performed 3 to 6 months after index synovectomy is an important way to establish a baseline and to monitor preclinical recurrence in high-risk individuals. Specifically, this refers to those patients with greater disease extent, bony involvement or erosions, or history of diffuse PVNS. Depending on patient preference, we even occasionally use screening MRI in patients with diffuse PVNS without high-risk characteristics, again to establish a baseline from which to evaluate future symptoms should they arise. We rarely use contrast media such as gadolinium and believe that one can adequately differentiate proliferating disease from scar or postsurgical change without incurring the cost or risks of contrast media.
We found the lowest rates of local recurrence with open posterior and arthroscopic anterior synovectomy. Our recurrence rate is similar to that reported by Sharma and Cheng in a recent study [19]. Their work featured a subgroup of eight patients with diffuse PVNS of the knee who were treated with open posterior/arthroscopic anterior synovectomy with a recurrence rate of 25%. The authors combine this group with an all-arthroscopic group (no posterior arthroscopy, 92% recurrence) in performing Kaplan-Meier survival comparison to an open/open synovectomy group (19% recurrence) and conclude that the open/open group had better 2- and 5-year recurrence-free survival. The recurrence rate we report for our all-arthroscopic group (62%) is similar to the Sharma all-arthroscopic cohort in that it is much higher than most previous reports for all-arthroscopic synovectomy, which have reported from 9% to 20% recurrence [5, 14, 21]. The higher recurrence rate in our arthroscopic cohort is more consistent with the recurrence rate reported for incomplete or subtotal synovectomies [3, 14, 19]. This may be because only a portion of our all-arthroscopic cohort (38%) underwent true total arthroscopic synovectomy with posterior portals, transcondylar notch views, and 70° arthroscopic lenses, or it may be related to technical issues with proper visualization. Theoretically, arthroscopic visualization and débridement is ideal because of the magnification and precision of its instruments, but the technique can be hindered by technical difficulties, especially in the posterior compartment of the knee. In any case, it is intuitive that a high recurrence rate is to be expected when a limited anterior synovectomy is performed despite gross posterior disease. However, in our series, those cases in which anterior synovectomy alone was performed were carefully screened using MRI and had an absence of posterior disease. This brings up the possibility that MRI is not an accurate gauge of the disease status of synovial tissue. It is possible that all knees with the diagnosis of diffuse PVNS should undergo either further biopsy testing of the posterior knee or rather should proceed directly to total synovectomy involving all portions of the knee. Further work is needed to make this recommendation, because these specifics are not adequately addressed in our study. Finally, for open/open total synovectomy, we found higher rates of recurrence than reported previously. Several studies report from 8% to 19% recurrence for diffuse PVNS of the knee treated with open anterior and posterior synovectomy [6, 19], and Chin et al. [3] found only 18% recurrence in 40 patients despite the fact that all cases had already failed one or more total synovectomies and 75% received adjuvant intraarticular dysprosium. In our series, the 64% recurrence rate in the open/open cohort is less similar to these studies and again more consistent with the recurrence rate reported for incomplete synovectomies [3, 14, 19]. We believe this could be related to selection bias toward open treatment of more florid or aggressive disease. It is also possible, if this selection bias exists, that the surgeon would overestimate recurrence by overreading surveillance MRI studies and be more prone to recommend revision synovectomy.
Arthritic progression in diffuse PVNS of the knee has not been well studied. We found a moderate rate of progression of Outerbridge grade or subjective joint space narrowing over the followup period (17%). The majority of these cases were associated with multiple recurrences and thus it is difficult to separate PVNS disease-related cartilage degeneration from the effects of iatrogenic surgical trauma. Progression of arthritis to the point of arthroplasty is an important outcome measure and represents the ultimate failure point in joint preservation. Our rate of conversion to arthroplasty (8%) is similar to the reported rates of 5% to 10% [4, 11, 14].
Lastly, we report a low perioperative complication rate in our series with no detected difference between groups (Table 1). This is in contrast to some studies that have reported complications such as arthrofibrosis as high as 32% in open anterior/open posterior procedures [6, 17]. Our complication rates are consistent with the all-arthroscopic series we have reviewed, which report zero or very low rates of perioperative complications [5, 9, 14, 21]. However, we cannot claim there is no statistical difference with regard to complication rates between groups because of the low power of the study and the rarity of complication events.
Diffuse PVNS of the knee has a high overall recurrence rate regardless of treatment. Nevertheless, our work demonstrates that open posterior/arthroscopic anterior synovectomy is a viable, comprehensive approach to this disease and provides both low recurrence rates and a low postoperative complication profile. Future study should involve multicenter cooperation to increase study group numbers and should establish standardized methods of defining recurrence to define the gold standard for local control in diffuse PVNS of the knee.
Acknowledgments
We thank Jay Irrgang, PhD, for contributions to the statistical work.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Blanco CE, Leon HO, Guthrie TB. Combined partial arthroscopic synovectomy and radiation therapy for diffuse pigmented villonodular synovitis of the knee. Arthroscopy. 2001;17:527–531. doi: 10.1053/jars.2001.24068. [DOI] [PubMed] [Google Scholar]
- 2.Byers PD, Cotton RE, Deacon OW, Lowy M, Newman PH, Sissons HA, Thomson AD. The diagnosis and treatment of pigmented villonodular synovitis. J Bone Joint Surg Br. 1968;50:290–305. [PubMed] [Google Scholar]
- 3.Chin KR, Barr SJ, Winalski C, Zurakowski D, Brick GW. Treatment of advanced primary and recurrent diffuse pigmented villonodular synovitis of the knee. J Bone Joint Surg Am. 2002;84:2192–2202. doi: 10.2106/00004623-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Chin KR, Brick GW. Extraarticular pigmented villonodular synovitis: a cause for failed knee arthroscopy. Clin Orthop Relat Res. 2002;404:330–338. doi: 10.1097/00003086-200211000-00049. [DOI] [PubMed] [Google Scholar]
- 5.De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2003;19:602–607. doi: 10.1016/S0749-8063(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 6.Flandry FC, Hughston JC, Jacobson KE, Barrack RL, McCann SB, Kurtz DM. Surgical treatment of diffuse pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 1994;300:183–192. [PubMed] [Google Scholar]
- 7.Gaanowitz SP, D’Antonio J, Mankin HL. The pathogenesis and long term end results of pigmented villonodular synovitis. Clin Orthop Relat Res. 1976;114:335–351. [PubMed] [Google Scholar]
- 8.Gillquist J, Hagberg G, Oretorp N. Arthroscopic visualization of the posteromedial compartment of the knee joint. Orthop Clin North Am. 1979;10:545–547. [PubMed] [Google Scholar]
- 9.Klein W, Jensen KU. Arthroscopic synovectomy of the knee joint: indication, technique, and follow-up results. Arthroscopy. 1988;4:63–71. doi: 10.1016/S0749-8063(88)80066-5. [DOI] [PubMed] [Google Scholar]
- 10.Kramer DE, Frassica FJ, Frassica DA, Cosgarea AJ. Pigmented villonodular synovitis of the knee: diagnosis and treatment. J Knee Surg. 2009;22:243–254. doi: 10.1055/s-0030-1247756. [DOI] [PubMed] [Google Scholar]
- 11.Mankin H, Trahan C, Hornicek F. Pigmented villonodular synovitis of joints. J Surg Oncol. 2011;103:386–389. doi: 10.1002/jso.21835. [DOI] [PubMed] [Google Scholar]
- 12.Mendenhall WM, Mendenhall CM, Reith JD, Scarborough MT, Gibbs CP, Mendenhall NP. Pigmented villonodular synovitis. Am J Clin Oncol. 2006;29:548–550. doi: 10.1097/01.coc.0000239142.48188.f6. [DOI] [PubMed] [Google Scholar]
- 13.Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine. 1980;59:223–238. doi: 10.1097/00005792-198005000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Ogilvie-Harris DJ, McLean J, Zarnett ME. Pigmented villonodular synovitis of the knee. The results of total arthroscopic synovectomy, partial arthroscopic synovectomy, and arthroscopic local excision. J Bone Joint Surg Am. 1992;74:119–123. [PubMed] [Google Scholar]
- 15.Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: a retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum. 2011;40:539–546. doi: 10.1016/j.semarthrit.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 17.Pettrone FA. Meniscectomy: arthrotomy versus arthroscopy. Am J Sports Med. 1982;10:355–359. doi: 10.1177/036354658201000607. [DOI] [PubMed] [Google Scholar]
- 18.Schwartz HS, Unni KK, Pritchard DJ. Pigmented villonodular synovitis. A retrospective review of affected large joints. Clin Orthop Relat Res. 1989;247:243–255. [PubMed] [Google Scholar]
- 19.Sharma V, Cheng EY. Outcomes after excision of pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 2009;467:2852–2858. doi: 10.1007/s11999-009-0922-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tyler WK, Vidal AF, Williams RJ, Healey JH. Pigmented villonodular synovitis. J Am Acad Orthop Surg. 2006;14:376–385. doi: 10.5435/00124635-200606000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Zvijac JE, Lau AC, Hechtman KS, Uribe JW, Tjin-A-Tsoi EW. Arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 1999;15:613–617. doi: 10.1053/ar.1999.v15.015061. [DOI] [PubMed] [Google Scholar]