Abstract
Introduction:
During the past 20 years, with huge advances in information technology and particularly, in the areas of health, various forms of electronic records have been discussed, designed or implemented. Although making health records automatically has many advantages but unfortunately in some cases, creation of an Electronic Health Record (EHR) system seems to be complicated. E-health (Electronic health) readiness assessment, as a part of the assessment before implementation is considered essential and prior to implementation. Readiness assessment aims to evaluate preparedness of each organizational component. This process can lead to the correct decision making. Therefore, identifying areas and requirements for such an assessment is so essential. Using the results of this assessment can identify deficiencies in the existing electronic health records to plan their strategies. The aim of this study was first; to show the situation of readiness assessment in EHR implementation roadmap, second, to recognize requirements associated with electronic readiness assessment and main areas of EHR readiness assessment.
Results and discussion:
This study reviewed the literature on EHR readiness assessment with the help of library and also searches engines available at Google. For our searches, we employed the following keywords and their combinations: readiness, assessment, implementation, Electronic Health Record (EHR), Information Technology, road map in the searching areas of title, keywords, abstract, and full text. In this study, more than 100 articles and reports were collected and 45 of them were selected based on their relevancy.
Key words: Readiness, Assessment, Implementation, Electronic Health Record (EHR).
1. INTRODUCTION
During the past 20 years, with huge advances in information technology and particularly in the areas of health, various forms of electronic records have been discussed, designed or implemented (1). Electronic Health Record (EHR) technology is considered as a new standard for medicine performance in USA in the 21st century (2, 3). During the past ten years many researchers have confirmed to move toward Electronic Health Records and promoted the technology based on information (4, 5). Also, in many studies the benefits of using computers in clinical activities have been discussed (2, 6, 7, 8). World Health Organization believes that Electronic Health Record includes all individual health information that provides electronic access during the person’s life for health providers. It can cover all patients (individuals) referrals including outpatient, inpatient and emergency (1).
Although making health records automatically has many advantages but unfortunately in some cases creation of an Electronic Health Record (EHR) system seems to be complicated. The problem may be due to unavailability of technology, funding, lack of technical and computer skills of personnel. Moreover, resistance and opposition of changes from electronic systems to manual systems by some health providers may create some problems (1).
Information systems researchers have identified complex problems in implementing of health information systems, especially in developing countries (9). Acceptation of any information system requires planning and good management to change (10). E-health (Electronic health) readiness assessment, as a part of the assessment before implementation, is considered essential and prior to implementation (11, 12). Readiness assessment aims to evaluate preparedness of each organization component. This process can lead to the correct decision making based on existing realities and constraints of the organization. Having a clear and defined process on how to do things can raise the success (13). Organizational resources and technical structures such as hardware and software are very essential requirements in the redesign of electronic projects (14).
A study on selection and implementation of successful electronic health records in small outpatient institutions in the United States of America showed that the EHR implementation experience has depended on several factors including technology, education, leadership, change management and unique properties of outpatient setting (15).
In general, failures are associated with evidence of negative consequences resulting from these technologies and will increase the amount of errors in using them (16, 17, 18, 19, 20, 21, 22, 23).
It can be stated that readiness assessment can offer a list of duties, and based on it, budget and time will be more accurately planned (13). Therefore, identifying areas and requirements for such an assessment is so essential. Using the results of this assessment can identify deficiencies in the existing electronic health records to plan their strategies. In this regard, it is necessary to assess readiness before any planning to implement electronic records.
The aim of this study is:
to show the situation of readiness assessment in EHR implementation roadmap;
to recognize requirements associated with electronic readiness assessment and main areas of EHR readiness assessment.
2. METHODOLOGY
This study was a review article and has been conducted with using library and electronic resources. The literature search was conducted with the help of search engines available at Google and also by using the citation and reference tracking methods. For our searches, we employed the following keywords and their combinations: readiness, assessment, implementation, Electronic Health Record (EHR), Information Technology, road map in the searching areas of title, keywords, abstract, and full text. Technical reports were excluded since research papers were focused.
In this study, more than 100 articles and reports were collected and 45 of them were selected based on their relevancy. For meeting the second aim of this article, we try to focus on standard information extracted from Medicare and Medicaid. Because of the less application of EHR readiness assessment than IT readiness assessment all over the world, this study wasn’t limited to any publish date.
3. RESULTS
The status of readiness assessment in EHR implementation roadmap
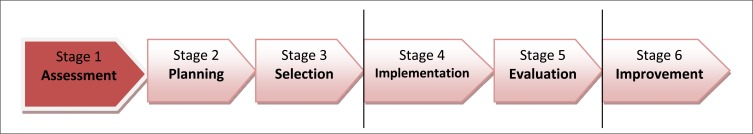
Electronic Health Record – EHR implementation roadmap shows the stages of the implementation and track of each stage. This map includes six stages (Figure 1) (24).
Figure 1.
EHR implementation roadmap
First and foremost stage of implementation of health information systems is readiness assessment for accepting and implementing of these systems. Preparation is the first important factor for staff enthusiasm to obtain the best and a better understanding of the usefulness of Electronic Health Records (15).
In fact, the first stage belongs to readiness assessment, but also is not unique for it and continues even to second and third stages. The planning stage (second stage) is performed to develop goals, opportunities and threats and generally to determine the missions. The selection stage (third stage) assesses the requirements of the organization and needs contained in Electronic Health Records (24).
Another study that was conducted by Ahlstrom, demonstrated that the first step in the life cycle of the EHR was readiness assessment, and organizational readiness must be assessed to develop a successful implementation (25).
Requirements associated with electronic readiness assessment
Comprehensive criteria must be followed in readiness assessment to show the preparation of the organization for planning (26). Generally, there are three types of basic requirements for e - readiness (electronic readiness) assessment in order to technical dimension (14):
Basic Requirements for Architecture Readiness
Several factors that judge the technical architecture readiness are important, including: a) Layered structure Judgment, based on operating systems and communication and information exchange standards, infrastructure accessibility, and availability of portal; b) Service orientation which can be judged through the share of services supported by IT, availability of fully automated services, share of data input by database queries, overall infrastructure service.
Basic Requirements for Infrastructure Readiness
Basic hardware and software: desktops/employee, mainframe availability, server availability, desktop operating system, server operating system.
External Data Exchange: data exchange with others, share of services with external data exchange.
Internal connectivity: percentage of internal connectivity between departments and agencies on different locations.
Basic Requirements for Process Readiness
Support processes: availability of major support systems.
Process automation: existence of fully automated services, share of services with IT support.
Data and information flow: share of manual data input.
Methods of customer notification.
The main areas of EHR readiness assessment
The four main areas of the EHR readiness assessment are organized as follow (26, 27):
Organizational culture
That is an assessment of overall perception of EHR, physician, staff and patient involvement, procedures for patient EHR interaction as well as methods for correcting/editing patient information, project plan development: accountability, timeline, dependencies, and role assignment for all aspects of EHR deployment. Readiness indications in this section will provide a better understanding of organizational infrastructure and a guide for planning the EHR adoption.
Management and leadership
That is an assessment of organization’s readiness to manage information, human and financial resources for current and future EHR requirements. This section details four readiness components including the executive team, financial, strategic plan, quality improvement and care management. Readiness indications in this section require increased management focus, potential process development, or planning before moving forward.
Operational readiness
That includes workflow redesign, care management, EHR policies, procedures, and protocols, EHR vendor relationship management, staffing needs for EHR implementation, training plan, training programs for project managers and IT staff involved in EHR adoption. Readiness indications in this section will identify potential process or barriers to adopting EHR and provide you with tangible guidance to improve this factor.
Technical readiness
That is an assessment of the organization’s technical environment and IT management capabilities. This section specified use of existing technology, hardware needs assessment, IT management, staffing for EHR training, implementation, maintenance, and infrastructure issues. Readiness indications in this section will identify potential areas for increased IT procurement, planning, or staff development prior to increase of EHR adoption.
4. CONCLUSION
Today is information age and the explosion of information technology has transformed every area of life and work (28). Information is so valuable and it must be well documented, maintained, retrieved and analyzed. In health management systems, information has a special role in planning, evaluation, training, legal aspects and research (29). In fact, the first distinction between developed and developing countries, are the production, application and utilization of information (30). So, with advent of information technology in health care, moving toward a new paradigm such as electronic health record has also begun (28). In this paradigm, Information is immediately accessible and electronic health record can also provide medical alerts and reminders. At first, it may be so expensive but it will save costs in long term (31).
Despite broad agreement on the benefits of electronic health records and other forms of health information technology, health care providers have moved so slowly to adopt these technologies (32, 33).
Lack of readiness causes weakness of organization to undergo transformation during the implementation of EHR (34). While EHR adoption has been low in some developed countries, the success of EHR adoption has also been low for developing countries, and it can be due to constrained resources, lack of required information technology support and stake holders’ awareness for moving to adopt new system (35, 36). Sufficient preparation in an organizational perspective enables to custom the system and ensures minimal workflow disruptions and irregularity during and after implementation (37). Decision makers must accept that Electronic Health (E-Health) evaluation may serve different purposes for different stakeholders (38). It must be noted that Implementing or transition to a new information system and generally technology advents may cause to fear, anxiety, and computer phobia (39, 40) and so staff acceptance for using information systems have been found to be major determinants of system success. (41). Knowing about readiness assessment and its areas, indications and requirements can facilitate to implement any information system.
5. RECOMMENDATIONS
IT capabilities and the innovative use of technology must be developed in health care organizations (28).
Administrators must be encouraged to assess the impact of pre implementation information systems on users, as well as the user’s degree of willingness to use them (42, 43).
Implementing information systems faces staff with change that may lead to resistance. Understanding of attitudes and expectations of staff can provide information serve as a starting point for a sometimes frustrating project (44).
It is required greater needs for education of staff before implementation of EHR (45).
Acknowledgement
We are grateful to Amir Hossein Siadat M.D, dermatologist and researcher of skin diseases and leishmaniasis research center for his to edit sentence structure aspects of this article.
Conflict of interest
None declared.
REFERENCES
- 1.WHO. Regional Office for the Western Pacific. Electronic Health Records: Manual for Developing Countries. WHO Library Cataloguing in Publication Data. 2006;9 [Google Scholar]
- 2.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care? JAMA. 2003;290:259–264. doi: 10.1001/jama.290.2.259. [DOI] [PubMed] [Google Scholar]
- 3.Martin JC, Avant RF, Bowman MA, et al. The future of family medicine: a collaborative project of the family medicine community. Ann Fam Med. 2004;2(1):S3–32. doi: 10.1370/afm.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Washington, DC: National Academy Press; 2002. The Computer-Based Patient Record: An Essential Technology for Health Care. [Google Scholar]
- 5.Frist WH. Shattuck Lecture: health care in the 21st century. N Engl J Med. 2005;352:267–272. doi: 10.1056/NEJMsa045011. [DOI] [PubMed] [Google Scholar]
- 6.Hersh WR. Medical informatics: improving health care through information. JAMA. 2002;288:1955–1958. doi: 10.1001/jama.288.16.1955. [DOI] [PubMed] [Google Scholar]
- 7.Bates DW, Ebell M, Gotlieb E, Zapp J, Mullins HC. A proposal for electronic medical records in U.S. primary care. J Am Med Inform Assoc. 2003;10:1–10. doi: 10.1197/jamia.M1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell E, Sullivan F. A descriptive feast but an evaluative famine: systematic review of published articles on primary care computing during 1980-97. BMJ. 2001;322:279–282. doi: 10.1136/bmj.322.7281.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Braa J, Monteir E, Sahay Networks of Action: Sustainable health information systems across developing countries. MIS Quarterly. 2004;28(3):337–362. [Google Scholar]
- 10.Eric WF, Menachemi N, Phillips MT. Predicting the Adoption of Electronic Health Records by Physicians: When Will Health Care be Paperless? Journal of American Medical Informatics Association. 2006;13(1):106–112. doi: 10.1197/jamia.M1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jennett P, Jackson A, Healy T, Ho K, Kazanjian A, Woollard R, et al. A study of a rural community’s readiness for telehealth. J Telemed Telecare. 2003;9:259–63. doi: 10.1258/135763303769211265. [DOI] [PubMed] [Google Scholar]
- 12.Demiris G, Oliver DRP, Porock D, Courtney K. Home telehealth: The Missouri telehospice project: Background and next steps. Home Health Care Technology Report. 2004;1:49, 55–7. [Google Scholar]
- 13.Kaufman JM. How can I ensure successful implementation of my EHR? Availableat: http://www.mdpso.com/documents/How_can_I_EnsureSucces_of_EHR.pdf . 2009. Apr, [Aug 4, 2010].
- 14.The Saudi e-Government Program–Yesser. IT Readiness Assessment for Government Organizations. Availableat: http://www.yesser.gov.sa/english/documents/IT_Readiness_Assessment_booklet_en.pdf . [Aug 17, 2010].
- 15.Lorenzi NM, Kouroubali A, Detmer DE, Bloomrosen M. How to successfully select and implement electronic health records (EHR) in small ambulatory practice settings. BMC Medical Informatics and Decision Making. 2009;9:15. doi: 10.1186/1472-6947-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ash J, Berg M, Coiera EW. Some unintended consequences of information technology in health care: The nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;11(2):104–12. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. J Am Med Assoc. 2005;293(10):1197–203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 18.Campbell E, Sittig D, Ash J, Guappone K, Dykstra R. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13(5):547–56. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wetter T. To decay is system: The challenges of keeping a health information system alive. Int J Med Inf. 2007;76S:S252–S60. doi: 10.1016/j.ijmedinf.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 20.Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care -An interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–49. doi: 10.1197/jamia.M2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silverstein S. Sociotechnologic issues in clinical computing: Common examples of healthcare IT difficulties. Available at: http://www.ischool.drexel.edu/faculty/ssilverstein/failurecases/?loc_home . [Aug 4, 2010].
- 22.Vogelsmeier AA, Halbersleben JRB, Scott-Cawiezell JR. Technology implementation and workarounds in the nursing home. J Am Med Inform Assoc. 2008;15(1):114–19. doi: 10.1197/jamia.M2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koppel R, Wetterneck T, Telles JL, Karsh B-T. Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc. 2008;15(4):408–23. doi: 10.1197/jamia.M2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.EHR Implementation Roadmap 2005 pilot. DOQ IT. Available at: http://www.ehcca.com/presentations/hitsummit2/3_03_2_h1.pdf . [Feb 4, 2010].
- 25.Ahlstrom J WIPFLI CAPs and consultants. Electronic Health Records (EHR) – Assessing Organizational Readiness. Available at: http://www.wipfli.com/resources/images/11935.pdf . [Feb5, 2010].
- 26.Community Clinic EHR Readiness Assessment Tool.xls, Introduction & Instructions. Availableat: http://www.norc.org/6275/Module2/Community%20Clinic%20EHR%20Readiness%20Assessment%20Tool.pdf . 2008. [Feb 10, 2010]. pp. 1–23.
- 27.EHR Readiness Assessment. DOQ IT. Available at: https://www.bcmsonline.org/main/files/ehr-readiness-assessment-DOQIT.pdf . [Sep 21, 2010].
- 28.Nilforoushzadeh MA, Heidari A, Siadat AH, Moradi S, Habibi M. Development of Information Technology in the field of dermatology. Iranian journal of dermatology. 2008;11(3):118–122. [Google Scholar]
- 29.Ajami S, Kalbasi F, Mahnaz K. Application of Medical Records in Research from the Viewpoint of Isfahan Educational Hospitals’ Researchers. Health Information Management. 2007;4(1):71–79. (in Persian) [Google Scholar]
- 30.Ajami S, Tavakoli Moghadam O. A Comparative Study on Health Information Management System with Standards in Ayatolah Kashani Hospital in Isfahan, Iran. Health Information Management. 2006;1(3):63–71. (in Persian) [Google Scholar]
- 31.Schoen C, Osborn R, Huynh PT, Doty M, Peugh J, Zapert K. On the front lines of care: primary care doctors’ office systems, experiences, and views in seven countries. Health Aff (Millwood) 2006;25:w555–w571. doi: 10.1377/hlthaff.25.w555. [DOI] [PubMed] [Google Scholar]
- 32.Jha A, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris T, Shields A, Rosenbaum S, Blumenthal D. Use of Electronic Health Records in U.S. Hospitals. N Engl J Med. 2009;360:1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 33.Brender J. London, UK: Elsevier Inc; 2006. Evaluation Methods for Health Informatics. [Google Scholar]
- 34.Watts C, Ibegbulam I. Access to electronic healthcare information resources in developing countries: experiences from the Medical Library, College of Medicine, University of Nigeria. Available at: http://72.14.253.104/search?q=cache:wT53fzH_TXEJ:www.ifla.org/IV/ifla71/papers/164e-Watts_Ibegbulam.pdf+%22ICT+infrastructure%22+healthcare+%22developing +countries%22&hl=en&ct=clnk&cd=1&gl=au . [19 Sep, 2010].
- 35.Diero L, Rotich JK, Bii J, Mamlin BW, Einterz RM, Kalamai IZ, Tierney WM. A computer-based medical record system and personal digital assistants to assess and follow patients with respiratory tract infections visiting a rural Kenyan health centre. BMC Med Inform Decis Mak. 2006;10(6):21. doi: 10.1186/1472-6947-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fullerton C, Aponte P, Hopkins R, Bragg D, Ballard DJ. Lessons learned from pilot site implementation of an ambulatory electronic health record. Baylor University Medical Center Proceedings (Baylor Univ Med Cent Proc) 2006 Oct;19(4):303–9. doi: 10.1080/08998280.2006.11928188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gagnon MP, Scott RE. Striving for evidence in e-health evaluation: lessons from health technology assessment. Journal of Telemedicine and Telecare. 2005;11:34–36. doi: 10.1258/135763305775124722. [DOI] [PubMed] [Google Scholar]
- 38.Jacobson SF, Holder ME, Dearner JF. Computer anxiety among nursing students, educators, staff and administrators. Computers in Nursing. 1989;7(6):266–272. [PubMed] [Google Scholar]
- 39.Wolfe K. Getting a grip on “computer phobia”. AAOHN Journal. 1991;39(7):352–353. [PubMed] [Google Scholar]
- 40.Goddard BL. Termination of a contract to implement an enterprise electronic medical record system. Journal of American Medical Information Association. 2000;7(6):564–568. doi: 10.1136/jamia.2000.0070564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whitehouse C. Preparing to introduce a computer into a health centre. British Medical journal. 1981;283:107–110. doi: 10.1136/bmj.283.6284.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gluck J. The computerized medical record system: meeting the challenge for nursing. Journal of Nursing Administration. 1979;12:17–24. [PubMed] [Google Scholar]
- 43.MacLane S. Designing an EMR planning process based on staff attitudes toward and opinions about computers in healthcare. CIN: Computers, Informatics, Nursing. 2005;23(2):85–92. doi: 10.1097/00024665-200503000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Moody LE, Slocumb E, Berg B, Jackson D. Electronic health records documentation in nursing: nurses’ perceptions, attitudes and preferences. CIN: Computers, Informatics, Nursing. 2004;22(6):337–344. doi: 10.1097/00024665-200411000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Ajami S. e Health; Strengths and Weaknesses. Journal of Iranian Medical Records Association. 2005;4(2):23–24. (in Persian) [Google Scholar]