Abstract
Introduction:
Surgical intervention and anesthesia procedure lead to a series of hormonal changes in the organism, which is mainly attributed to catecholamine response to stress. Surgical intervention is resulting in significant changes in neuroendocrine regulation, metabolism and physiological functions, as part of the overall response to stress.
Research aim:
The aim of this study was to determine and evaluate the levels of hormones in patients undergoing transvesical prostatectomy under general or local anesthesia.
Material and methods:
The study included a total of 100 patients from the Clinic of Urology, Clinical Center of Sarajevo who underwent surgery by technique of transvesical prostatectomy (BPH) in which the indicators were set:: a) repeated urinary retention; b) calculosis and diverticulosis of the urinary bladder; c) urinary infection, d) repeated massive hamaturia and e) the distal obstruction that can lead to uremia.
Results:
General anesthesia may limit the perception of stimuli from injury, but does not eliminate the full response to noxious stimuli, even with deep anesthesia. All intravenous agents andvolatile anesthetics in normal doses have little effect on the endocrine and physiological functions. Neural blockade induced by regional anesthesia or local anesthetics have a direct impact on endocrine and metabolic response. Regional anesthesia with the present consciousness, but with sympathetic blockade caused a greater suppression of hormonal responses than the general balanced anesthesia. In our research we obtained: a) a significant increase in prolactin intraoperatively, for respondents under general anesthesia; b) a significant increase in TSH values intraoperatively for respondents under general anesthesia; c) a significant drop in T4 intraoperatively in patients with regional anesthetic technique; d) a significant increase in cortisol values 24 hours postoperatively in patients with regional anesthetic technique.
Key words: BPH, anesthesia, hormons level, prostatectomy.
1. INTRODUCTION
Surgical intervention and anesthesia procedure lead to a series of hormonal changes in the organism, which is mainly attributed to catecholamine response to stress (1, 2, 3). Under the term stress we mean the number of negative noxa acting on the body, and the surgery with anesthesia procedures, are also, the negative noxa. When exposed to stress the organism and hormonal response primarily are responsive pituitary, adrenal, adrenal cortex, prostate glandular tissue, and the sympathetic nervous system (4, 5).
Surgical intervention is resulting in significant changes in neuroendocrine regulation, metabolism and physiological functions as part of the overall response to stress. The reaction of the organism is manifested by distribution of blood flow, to ensure the function of vital organs and to carry out mobilization of energy sources. Hypovolemia and pain are direct stimulators of hormonal response to trauma (6, 7, 8).
After all major surgeries there is an increase in plasma concentrations of glucagon. Intraoperative low values of both insulin and elevated levels of counter-insulin hormones are powerful stimulus for gluconeogenesis (5). Cortisol, glucagon and epinephrine exhibit a synergistic effect on gluconeogenesis, protein catabolism, glucose intolerance, insulin resistance and peripheral leukocytosis. Numerous studies have shown that the resulting response in the body is not only a consequence of the action of hormones, but that the endocrine and inflammatory mediators together create an active metabolic response to stress (1, 9, 10, 11, 12, 13, 14).
Thus, neuroendocrine, metabolic and inflammatory aspects of the injury are part of an overall “stress response”. In particular, it manifests in patients undergoing surgical intervention. These reactions can occur with trauma, burns, severe infections and physical exertion. Metabolic and neuroendocrine response to surgical intervention depends on several factors, such as severity and duration of the surgical trauma, patient’s age, type of anesthesia and surgical techniques (6, 7). A number of hormones in the broad sense, which is secreted during this period, affect change in hemodynamic stability, metabolism, immune response in the body and changes in internal milieu. The study was focused on the value of the ACTH hormone, prolactin, TSH, T3, T4, cortisol, during the two different techniques of anesthesia: general and local-regional, applied during surgery transvesical prostatectomy.
Prostate adenoma is the most common benign neoplasm in men, so that three quarters of men over 50 have symptoms of BPH. 20-30% of men who live to age of 80 years have the need for surgical intervention. BPH is considered a disease of modern civilization, and because of the high prevalence of the disease it has an enormous socio-economic importance. In the U.S. only for the surgical treatment of BPH has been spent in 2003 about 2.5 billion dollars (15, 16).
For optimal treatment for BPH is necessary accurate diagnosis and differentiation of the diseases that can produce similar symptomatology (prostate cancer and chronic prostatitis).
It seems important that expressed signs of obstruction and associated complications accelerate the aging process and the psychological and physical deterioration of the organism, while adenomectomy provides medical and social rehabilitation of patients and quality of life that suits their age. The therapeutic choice depends on a number of factors, primarily refers to the general condition of patient, age, comorbidities, socioeconomic condition and living conditions. Patient age may not be an obstacle for surgical treatment, more important parameters are general health condition and fitness of the patient.
2. AIM OF THE RESEARCH
The aim of this study was to determine and evaluate levels of hormones in patients undergoing transvesical prostatectomy under general or local anesthesia.
Determined the level of hormone values during three time periods: before anesthesia, during surgery in enucleation of prostate glandular tissue and 24 hours after surgery.
3. PATIENTS AND METHODS
The research was retrospective-prospective, clinical, comparative, longitudinal and observational. Complete research is completely spent at the Clinic for Anesthesiology and reanimation of Clinical Center of Sarajevo University (CCUS). The study included a total of 100 patients from the Clinic of Urology, Clinical Center of Sarajevo who underwent surgery by technique of transvesical prostatectomy (BPH) in which the indicators were set: a) repeated urinary retention; b) calculosis and diverticulosis of the urinary bladder; c) urinary infection, d) repeated massive hamaturia, e) the distal obstruction that can lead to uremia (15).
According to the criteria defined the subjects were divided into two test groups:
Group I (n=50) – patients underwent surgery under general anesthesia,
Group II (n=50) – patients underwent surgery in local-regional anesthesia.
The research used two types of anesthesia: general and localregional anesthesia.
All patients included in the study (N = 100) received orally (PO) Midazolam, basal sedation in a dose of 7.5 mg, 60 minutes prior to surgery. During anesthesia are used the standard monitoring of patients included: following electrocardiogram (ECG) changes, heart rate, blood pressure, oxygen saturation (SaO2), followed by pulse oximetry and expiratory concentrations of carbon dioxide (CO2).
In the course of this research have been applied the standard methods of general and loco-regional anesthesia, which are routinely used in surgery of the prostate. Taking blood samples in order to determine the test levels of hormones relevant for this research was done by the standard procedure in the Central CCUS biochemical laboratory.
4. RESULTS
For data processing we used a statistical program SPSS 15.0 (SPSS Inc., Chicago, IL).
Data are presented and analyzed by the following statistical tests and methods:
Age of the subjects involved in research, according to predefined inclusion criteria ranged from 60-80 years, with an average value of X = 69.95 (SD ± 5.5).
According to the type of anesthesia, and the inclusion criteria, an equal number of respondents (N=50) was selected by two types of anesthesia – general and loco-regional.
In 10% of patients the haemogram was corrected during the surgery, without differences in applied anesthetic technique N=10.
According to the concomitants diagnoses observed in the distribution was a large number of different diseases, so it is aligned to sever-
al major groups, namely: a) cardiovascular diseases – 44.0%; b) diseases of the respiratory system – 4% ; c) Diabetes mellitus/DM) – 9%, d) and DM with arterial hypertension – 8%; f) other diseases – 14% (Table 3)
Table 3.
Concomitant disease of the respondents
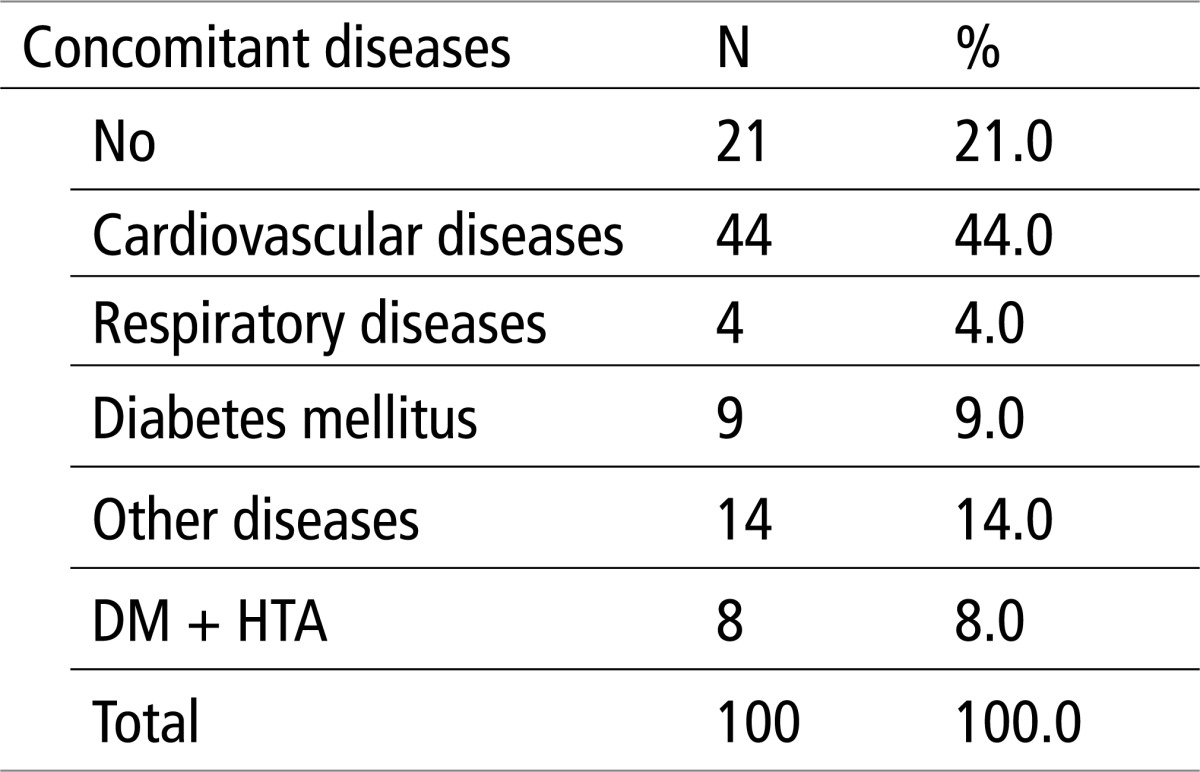 |
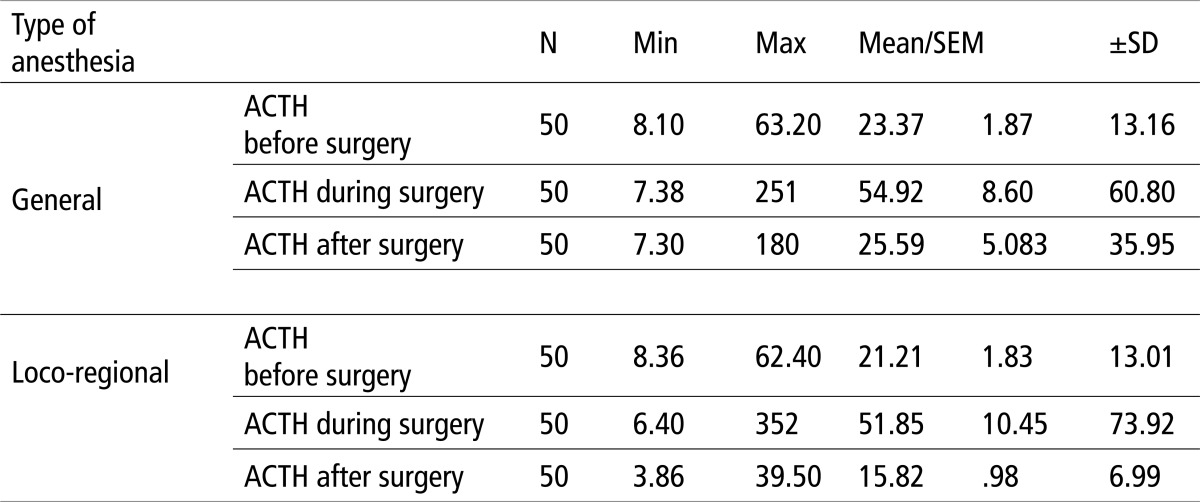
Table shows the number of respondents, the minimum and maximum values of ACTH, the mean and standard error and standard deviation of the two types of anesthesia (15).
As the Table 4 shows the largest increase in ACTH values are recorded during surgery in both types of applied techniques of anesthesia, with a slightly higher maximum values achieved when using the technique of local-regional anesthesia, but the mean values , however maintained within the referent ranges for both types of anesthesia.
Table 4.
ACTH values in relation to the type of anesthesia
 |
5. DISCUSSION AND CONCLUSION
The prostate is a glandular-muscular organ whose secretory epithelial cells secrete prostate specific antigen (PSA), acid phosphatase, enzymes and amino peptide. The basal cells of these glands contain androgen receptors and secreted acidic phosphate-rich ATP. Neoplasms probably originate from these cells. Neuroendocrine prostate cells known as AUPD (Amine Uptake Precursor Decarboxylase) contain and secrete biogenic amines, serotonin, bombesin, gastrin, calcitonin, somatostatin, thyeostimulating hormone (TSH), horiogonadotropin, hromogranin A and B.
Secretory function of prostate and other accessory glands has been reduced by inflammation of the prostate and seminal bladder.
General anesthesia may limit the perception of stimuli from injury, but does not eliminate the full response to noxious stimuli, even with deep anesthesia. All intravenous agents and volatile anesthetics in normal doses have little effect on the endocrine and physiological functions. Neural blockade induced by regional anesthesia or local anesthetics have a direct impact on endocrine and metabolic response. The basic mechanism of neural blockade of stress response to surgical intervention is completely preventing pain signals from the operating field reach the CNS. Inhibitory effects of neural blockade on endocrine and metabolic response during surgical procedures also apply to the afferent and efferent pathways (1).
Regional anesthesia causes complete sensory block, which prevents the poor stimulus in the area of the surgical field. This is not the case with general anesthesia, which generally does not prevent surgical stimuli or CNS reactions and stress responses, and Sometimes the creation of abnormal reflexes (14).
The results show the following hormonal responses:
Noted is the increase in ACTH values during surgery in case of regional and general anesthesia, with a slightly greater increase among respondents under general anesthesia.
In the postoperative period ACTH values returned to preoperative values, with slightly lower values in subjects under regional anesthesia.
The values of prolactin (PRL) indicate an increase in value during the surgery in both applied techniques of anesthesia, with a significantly higher maximum values registered with general anesthesia (3554µIJ/L). High levels of PRL are maintained also postoperatively after 24 hours, but were greater in case of regional anesthesia (maximum value recorded 1074µIJ/L) than in general (recorded maximum value 720µIJ/L).
The values of TSH were elevated during surgery in both anesthetic techniques, with a significantly higher maximum values registered with general anesthesia.
The values of TSH postoperatively after 24 hours showed a return to baseline in both the applied technique of anesthesia.
The values of T3 hormones fluctuate in the downward direction, which is particularly evident at the minimum values for both types of anesthesia.
The values of T3 hormone post-operatively after 24 hours are still in a downward trend in both anesthetic techniques.
The values of T4 hormone in subjects under general anesthesia did not show significant deviations from the mean values either intra-operatively or postoperatively.
The values of T4 hormone in subjects with applied regional anesthetic technique showed significant decline in the intraoperative value, with a gradual increase in the value postoperatively. Postoperatively after 24 hours the registered values do not reach the preoperative values.
Noted is the increase in cortisol values both intraoperatively and 24 hours postoperatively for both anesthetic techniques.
Noted is the significant increase in cortisol values 24 hours postoperatively in patients with regional anesthesia.
Regional anesthesia with the present consciousness, but with sympathetic blockade caused a greater suppression of hormonal responses, than the general balanced anesthesia.
The most striking results of this study were obtained by using sophisticated statistical methods of descriptive statistics and binary logistic regression analysis indicazed:
A significant increase in prolactin intraoperatively, for respondents under general anesthesia.
A significant increase in TSH values intraoperatively for respondents under general anesthesia.
A significant drop in T4 intraoperatively in patients with regional anesthetic technique.
A significant increase in cortisol values 24 hours postoperatively in patients with regional anesthetic technique.
Table 1.
Stress caused changes in the organism
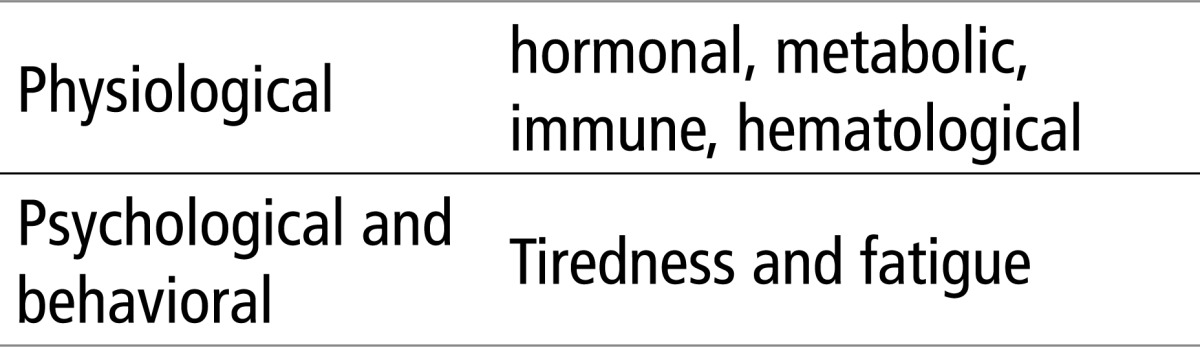 |
Table 2.
Hormonal changes during surgeries
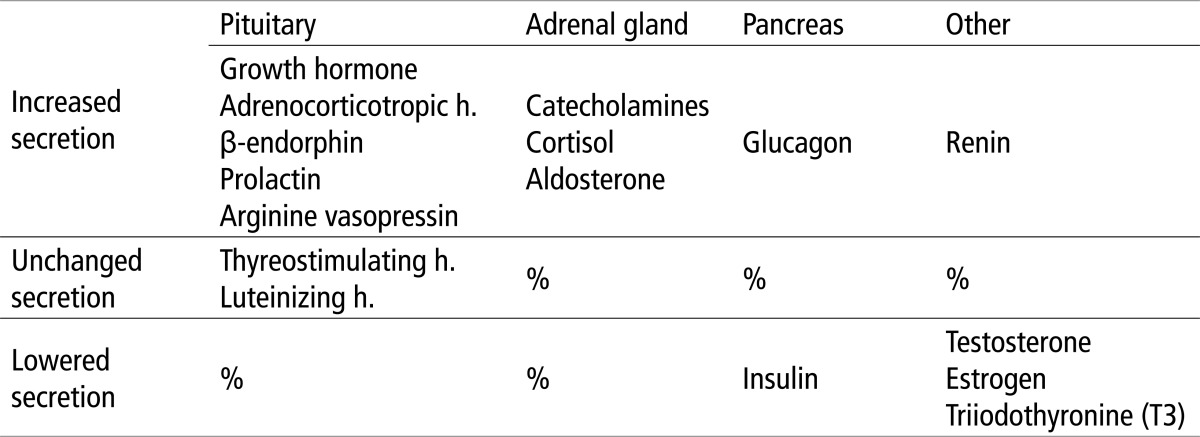 |
Table 5.
The results of the Kolmogorov–Smirnov test for normality of distribution for the hormones values
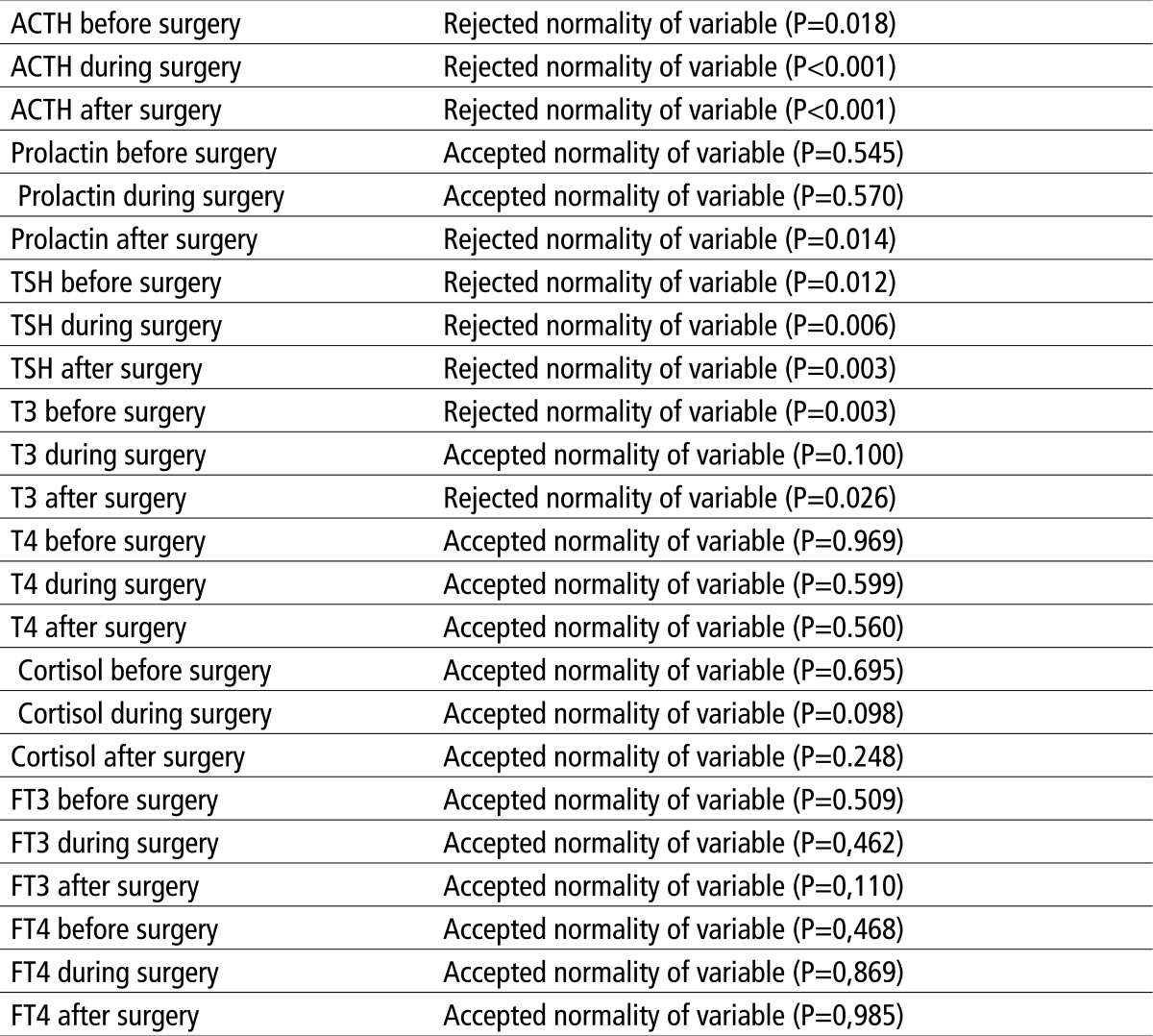 |
Conflict of interest
None declared.
REFERENCES
- 1.Celic-Spuzic E. Magistarski rad. Sarajevo: Medicinski fakultet Univerziteta u Sarajevu; 2011. Uticaj vrste anestezije na promjene nivoa ACTH, Prolaktina, TSH, T3, T4 kortizola, pracenih tokom i nakon uradjenih transvezikalnih prostatektomija. [Google Scholar]
- 2.Chiu WC, Carlson DE, Lilly MP. Acute Trauma Response. In: Fink G, McEwen B, Ronald de Kloet E, Rubin R, Chrousos G, Steptoe A, et al., editors. Encyclopedia of stress. 2th. San Diego; San Francisco; New York...etc: Academic Press; 2007. pp. 15–21. [Google Scholar]
- 3.Prašo M. Tuzla: Univerzitet u Tuzli; 2006. Uticaj inhalacione i intravenske anestezije na imunološki odgovor organizma. [Google Scholar]
- 4.Sheeran P, Hall GM. Cytokines in anaestesthesia. Br J Anaesth. 1997;78:201–219. doi: 10.1093/bja/78.2.201. [DOI] [PubMed] [Google Scholar]
- 5.Lalevic P. 4 izd. Beograd: Zavod za udžbenike i nastavna sredstva; 1999. Anesteziologija. [Google Scholar]
- 6.Burton D, Nicholson G, Hall G. Endocrine and metabolic response to surgery. Continuing Education in Anaesthesia. Critical Care & Pain. 2004;4(5):144–47. [Google Scholar]
- 7.Schricker T, Carli F, Schreiber M, Wachter U, Geisser W, Lattermann R, et al. Propofol/Sufentanil Anesthesia Suppresses the Metabolic and Endocrine Response During, Not After, Lower Abdominal Surgery. Anesthesia & Analgesia. 2000;90:450–455. doi: 10.1097/00000539-200002000-00039. [DOI] [PubMed] [Google Scholar]
- 8.Kovač T, Lepšanovic L. Beograd-Zagreb: Medicinska knjiga; 1988. Endokrinologija. [Google Scholar]
- 9.Guyton AC, Hall JE. 11 izd. Zagreb: Medicinska naklada; 2006. Medicinska fiziologija; pp. 905–960. [Google Scholar]
- 10.Harrison TR, Isselbacher KJ, Braunwald E, Wilson JD, Martin JB, Fauci AS, et al., editors. Placebo, Split. 13 izd. 1997. Principi interne medicine (hrvatski prevod) pp. 1653–1929. [Google Scholar]
- 11.Adhikary S, Korula M. The stress response and its implications in surgery and anaesthesia. Psychosom Med. 2000;54:275–287. [Google Scholar]
- 12.Matthews C. Enhanced Recovery Following Surgery. ATOTW. 2010;204:1–9. [Google Scholar]
- 13.Absolom A, Pledger D, Kong A. Adrenocortical function in critically ill patients 24 h after a single dose of etomidate. Anaesthesia. 1999;54:861–867. doi: 10.1046/j.1365-2044.1999.01003.x. [DOI] [PubMed] [Google Scholar]
- 14.Jukic M, Majeric–Kogler V, Husedžinovic I, Sekulic A, Žunic J. 1 izd. Zagreb: Medicinska naklada; 2005. Klinička anesteziologija. [Google Scholar]
- 15.Celic-Spuzic E. Effect of Anesthesia on the Changes in the Hormones Levels During and After Transvesical Prostatectomy. Med Arh. 2011;65(6):348–353. doi: 10.5455/medarh.2011.65.348-353. [PubMed] [Google Scholar]
- 16.Aron DC, Findling JW, Tyrrell JB. Hypothalamus and Pytuitary Gland. In: Greenspan FS, Gardner DG, editors. Basic and Clinical Endocrinology. 7th ed. New York; Chicago; San Francisco, etc: Lange Medical Books, McGraw-Hill; 2004. pp. 106–175. [Google Scholar]


