Abstract
Objective
Changes in models of health care are required to better meet the needs of diverse, underserved patient populations. Collaboration among providers is one way to promote accessible, comprehensive and continuous care in healthcare organizations. This paper describes the quantitative findings from two time points that examined providers’ views of collaboration among a sample of diverse personnel (e.g. clinical nurses, social workers, dental providers, mental health providers, clerical staff, medical assistants, public health staff, and administrators) within a federally qualified nurse managed health care centre in the United States.
Methods
The quantitative arm of a mixed-method study is presented in this paper. Two instruments, the Collaboration and Satisfaction About Care Decisions Scale and the University of the West of England Interprofessional Questionnaire (comprised of 4 subscales–Communication and Teamwork Scale, Interprofessional Learning Scale, Interprofessional Interaction Scale, and Interprofessional Relationships Scale) were administered to providers at baseline and three to eight months following six same discipline focus group discussions on collaboration, in order to evaluate whether participating in the focus group discussions changed providers’ views of collaboration. A summary of the focus group data which were published elsewhere is additionally summarized to help provide insight to the quantitative findings. Thirty-nine staff participated.
Results
Paired t-tests revealed that only one scale out of the five, Collaboration and Satisfaction About Care Decisions Scale (33.97 at time one and 37.45 at time two), significantly and positively changed after the focus group discussion (p=0.046). Providers’ views on collaboration ranged from positive to moderate views of collaboration; most measures revealed a non-significant improvement after the focus group discussions. Staff with some graduate school reported the greatest satisfaction with decisions for the patient, and those with high school reported the lowest satisfaction with decisions for the patient. Respondents with a graduate degree had the most positive views of interprofessional relationships, whilst those with either a high school degree or bachelor’s degree had the most negative views of interprofessional relationships. ANOVAs by professional role revealed the least positive views of collaboration for provider groups with lower levels of education, with upper administration reporting the most positive views on collaboration.
Conclusion
Although the discussion generated by the focus groups was expected to facilitate communication, and research has suggested that communication between providers facilitates collaboration, only one subscale evaluating providers’ views of collaboration positively and significantly changed after the focus group discussion. The wide range of views on collaboration suggests there are diverse perspectives on collaboration among the staff based on professional roles and levels of education, with upper administration and those with higher levels of education reporting the most positive views of collaboration and staff with lower levels of education reporting more negative views of collaboration. A major limitation of this study was a low time two return among support staff, comprised of primarily African American women. Due to their marginalized professional and racial status, future research needs to explore the perspectives of this important and often overlooked group of staff.
Keywords: collaborative care, hierarchy, health disparities
Introduction
Vulnerable patient populations, such as people from ethnic and racial minority groups, women, and those of lower socioeconomic status are particularly at risk for mental illness and other chronic health care concerns [1, 2] and are less likely to receive adequate care in the United States [3, 4]. These vulnerable groups are also more likely to first seek mental health care in their primary health care setting [5, 6] which makes intervention at the primary care level an important objective. Research is needed to explore providers’ perspectives on collaborative care in primary healthcare settings because new models of health care services are being developed in Western countries. D’Amour and colleagues suggest that promoting a transition to interprofessional and interorganizational collaboration is not an easy feat because effectively operationalizing this process requires addressing interactional, organizational and socio-political factors [7].
Concerns related to collaboration among providers are fundamental to disparities in health care, since “barriers to health care have been conceptualized as organizational, structural, and clinical including lack of diversity in the healthcare workforce, lack of cultural and linguistic competency, health illiteracy, and inadequate access to and coordination of care” [8, p. 13]. Butt, Markle-Reid and Browne [9] suggest that, in order to overcome health disparities in the United States, we need to adopt an approach to care that includes an array of professionals extending beyond the more traditional acute episodic health care and the services of any single profession. Integrated and collaborative health care is needed in the United States to provide more effective and coordinated delivery of accessible, continuous, and comprehensive services. Blount notes that coordinated services support a process whereby work has been done so that information is exchanged on a regular basis when patients are in treatment settings which can be collocated (e.g. behavioural health and medical services are located in the same building) or separate locations [10].
Medical Family Therapy promotes a biopsychosocial approach for the treatment of individuals and families coping with medical problems and defines collaborative care as an interdisciplinary health care treatment approach on a spectrum ranging from parallel care to collaborative networking [11–12]. Parallel care consists of a referral process with minimal overlap of services, whilst at the other end of the spectrum is collaborative networking where there is a non-hierarchical co-provision of patient care and the intentional inclusion of family, educators, and/or community in the process. The next level is informal consultation where providers maintain occasional consultation over clinical concerns. Formal consultation happens when there is a more formal, possibly contractual, arrangement between providers for ongoing consultation regarding patient care. Coprovision of care refers to sharing non-hierarchical professional responsibility for patients and often seeing patients and families jointly. Finally, collaborative networking expands the coprovision of care model to include extended family, multiple healthcare providers, and community resources [12]. Additionally, integrated care supports patients having one treatment plan with behavioural and medical elements, rather than two separate treatment plans.
Professional hierarchy among providers (e.g. primary care and mental health providers), however, can negatively affect collaboration that best serves vulnerable patient populations [11–14]. Power and gender concerns exist among professionals, such as mental health care providers, who are required to do the majority of accommodation as compared to medical providers [13]. Consideration of these contextual barriers to collaborative team work is critical since these groups of providers are confronted with a demand for interprofessional collaboration, shared goals and partnerships including explicit, complementary and interdependent roles; mutual respect; and power sharing.
As noted by Herbert in Rose’s publication [15, p. 5], interprofessional collaboration is the process of “promoting and optimizing active participation of all health care professions in clinical decision-making focused on patient needs whilst ensuring respect for team member contributions.” This process is expected to improve quality of care, patient safety and outcomes because the expertise and particular contributions of all health care professionals are utilized and acknowledged [15]. This shift in approaches to care can be difficult to implement among interdisciplinary providers, as problems often arise due to a number of interactional, organizational, and socio-political factors [7].
Health disparities associated with an underprivileged status necessitate research on how best to serve these vulnerable patient populations. Our study addressed this gap by focusing on providers’ views of collaboration among a group of diverse staff within an agency who serve patients who are 95% ethnic and racial minorities and predominately low-income and who have low health literacy. A better understanding of providers’ views of collaboration whilst serving underprivileged patient populations, can lead to more effective collaborative care models to address current health disparities in the United States. Furthermore, this study filled a major gap by including diverse members of the healthcare team (e.g. medical assistants, dental hygienist, dentist, nurse practitioners, clinical nurse, social work, behavioural and mental health providers, health promotion and public health staff, and administration) from all levels of staff within the Centre [14, 16, 17].
Given the sparse empirical research designed to examine providers’ views of collaboration among diverse health care groups within community health care settings in the United States, quantitative findings at two time points from a parent study (primarily qualitative with an embedded quantitative component) captured a diverse group of providers’ views of collaboration [18–19]. We also summarize the qualitative data collected from six same discipline focus groups discussion with participants to provide further insight on findings from the quantitative data (see [20] for a more detailed description of the findings from the focus group discussions).
We examined how providers’ participation in six same discipline focus group discussions exploring interdisciplinary collaboration affected providers’ views of collaboration. We hypothesized that participation in the focus group discussions would result in improved scores on the five scales designed to measure collaboration. The discussion generated by the focus groups was expected to facilitate more open communication and understanding as research has suggested that communication between providers facilitates collaboration [16]. It was, therefore, expected that participation in the focus groups would result in providers’ improved perceptions of collaboration at the healthcare centre. Five self-report quantitative scales designed to measure collaboration were completed by participants at baseline (two weeks prior to the focus groups) and again between three to eight months following the focus group discussions to evaluate changes in providers’ views of collaboration following participation in the same discipline focus groups.
Methods
Interdisciplinary staff at a nurse managed community based primary health care centre completed five self-report scales from two collaboration measures to examine providers’ views of collaboration at two time points (intended time frame was baseline or two weeks prior to focus groups and three months after focus group discussions). Qualitative findings from the six focus groups for this study is reported elsewhere [see 20]. Using the methodology described by Krueger [21], six same discipline focus groups (FG) explored experiences of collaboration among diverse healthcare providers whilst serving underprivileged patients. Due to the small size of some of the disciplines, several provider groups were combined to create a diverse group of staff members. The FGs were not designed to be an intervention, however the authors hoped it would promote deeper discussions among providers regarding their views of collaboration at the healthcare centre. The FGs explored the following research questions:
What can facilitate and/or impede collaboration?
How do provider and patient characteristics affect the collaborative process?
What are the providers’ perceptions of family and community involvement in healthcare?
Data analysis was conducted using the Miles and Huberman approach which includes three iterative processes: data reduction, data display, and conclusion drawing or verification [22].
Participants consisted of 39 staff out of a possible sampling frame of 57 (68% response rate) who were employed at the nurse managed community based primary health care centre during the time of the study. The final sample was comprised of primary care, dental care, nursing, behavioural health, health educators, physical therapy, support staff, and upper administration. This nurse managed community based primary health care centre employs over 50 people, with approximately 26 medical providers, 12 mental health providers, 5 health educators, and 7 administrators. Inclusion criteria were all adult staff at the site who worked there for at least three months and had the opportunity to collaborate with the other onsite health care providers. Staff who worked at the health centre for <3 months were excluded from this study, due to not having enough time and experience practicing the collaborative care model utilized at this nurse managed community based primary health care centre.
The mission of this nurse managed centre is to decrease health disparities through the continued development of Healthy Living Centre programs by offering transdisciplinary clinical services and health promotion programs in partnership with the local community and neighbourhoods. The programs implemented at this health centre are designed to reduce risk factors for disease and to help patients better manage existing health conditions. Diabetes education, self-efficacy programs, nutrition education, fitness, cooking classes, and behavioural health group support are the core program elements of the Healthy Living Centre. The Centre’s transdisciplinary process acknowledges the role of all providers from diverse disciplines and supports cross discipline learning. The philosophical vision at the Centre is guided by the principles of access, collaboration, equity, and community participation. The Centre also has integrated health services (e.g. primary care, behavioural health, dental, and health promotion services).
After Institutional Review Board Approval to conduct the study was obtained, data collection occurred from April 2009 until December, 2009. Approximately two weeks prior to each of the six same discipline focus groups, staff were given a packet comprised of the 5 scales from the two questionnaires designed to evaluate providers’ views of collaboration (see full description of 5 scales below). Each participant first met individually with the first author to review and sign the informed consent form and to complete questionnaires (time one). Mutually agreed upon times were arranged for the six same discipline focus group discussions to occur at the Centre and three months after the focus groups occurred, participants were again asked to complete the self-report measures on collaboration (time two). Even with many reminder emails, phone calls, and delivery of replacement questionnaire packets some questionnaires were returned up to eight months later (actual range from three to eight months for time 2 data).
Scales
Collaboration and satisfaction about care decisions scale
We chose this first self-report measure because it was developed to measure collaboration and satisfaction about care decisions between nurses and physicians and demonstrates good reliability and validity and is congruent with our definition of collaborative care described above [23–25]. Six items measure critical attributes of collaboration and are scored on a Likert type scale ranging from 1 (strongly disagree) to 7 (strongly agree). The seventh item that evaluates the amount of collaboration is scored on a scale ranging from 1 (no collaboration) to 7 (complete collaboration). The 2 questions on satisfaction with care decisions are also on a Likert type scale ranging from 1 (not satisfied) to 7 (very satisfied). The instrument demonstrates good internal consistency for the six items with a reported Cronbach’s alpha of 0.93. The original pilot study consisted of 32 NICU nurses and 26 paediatric residents who had recently worked in the NICU or paediatric ICU. For this study the measure was revised with the authors’ permission. The items were adapted to:
reflect general collaboration between disciplines, rather than neonatal intensive care unit nurses and paediatric residents and
overall global trends in collaboration rather than focusing on collaboration in specific instances.
University of the West of England interprofessional questionnaire
We chose the second self-report measure in our study that was comprised of 4 subscales (Communication and Teamwork Scale, the Interprofessional Learning Scale, the Interprofessional Interaction Scale, and the Interprofessional Relationships Scale) because it demonstrates good reliability and validity and was designed to measure providers’ communication, teamwork skills, and attitudes towards professional collaboration [26–27]. Each of the subscales is scored using a Likert type scale and is comprised of nine items. Responses for the Communication and Teamwork scale range from 1 (strongly agree) to 4 (strongly disagree). Scores range from a minimum of 9 to a maximum of 36, with nine to 20 indicating a positive score, 21–25 indicating neutral, and 26–36 indicating negative self-assessment of communicating and teamwork skills. Responses for the Interprofessional Learning Scale and Interprofessional Interaction Scale range from 1 (strongly agree) to 5 (strongly disagree). Scores on both scales range from a minimum of 9 to a maximum of 45, with 9 to 22 indicating a positive score, 23–31 indicating neutral, and 32–45 indicating negative attitudes towards interprofessional learning and interprofessional interaction, respectively. The three subscales from this measure have good reliability; Cronbach’s alphas were reported as 0.76, 0.84, and 0.82, respectively.
Finally, the Inter-professional Relationships is the fourth subscale from the University of the West of England Interprofessional Questionnaire and is comprised of eight items with responses scored on a Likert type scale ranging from 1 (strongly agree) to 5 (strongly disagree) [27]. Total scores in the range of 8 to 20 indicate positive scores, 21–27 indicate neutral, and 28–40 indicate negative attitudes towards respondent’s own inter-professional relationships. Reliability was established through test-retest administration to 38 additional respondents, with a resulting score of r=0.83 and the Cronbach’s alpha was reported as 0.71. Additionally, forty nursing students were used to examine original concurrent validity of these measures.
Quantitative data analysis was conducted using SPSS vs. 17.0.1. The alpha level was set at 0.05. Descriptive statistics and bivariate correlations were calculated for each of the five scales to explore the associations between the self-report measures of collaboration. Paired t-tests were then conducted to analyze participants’ data at baseline and at time two after the same discipline FG discussions to evaluate changes in their views about collaborative care. Finally, an exploration of salient providers’ contextual variables and views of collaboration, particularly race, education, and professional role were examined using a one-way analysis of variance.
Results
Quantitative findings will be presented first, followed by an overview of qualitative themes and findings which emerged from the six same discipline focus groups. Themes and findings from the focus groups help to inform the quantitative analysis of the five self-report measures of providers’ views of collaboration. At time one, the sample consisted of 39 participants. Nearly half of the staff (43.6%) ranged in age from 46–60 years of age, approximately a third (30.8%) ranged from 18–30 years of age, and 17.9% were between 31–45 years of age. The sample was primarily female (87.2% female; 12.8% male). The racial composition was 33.3% African American, 2.6% Asian, 10.3% </softEnter>Hispanic, 46.2% Non-Hispanic White, 2.6% Native American, and 5.1% Other.
Approximately a third (35.9%) of the sample worked within the primary healthcare discipline, and 17.9% worked in either the behavioural health or the dental disciplines. The rest of the sample was represented by administration, physical therapy, and holistic health education. Regarding education, over half of the sample (51.3%) had graduate degrees, and 23.1% had some college education. Similarly, 20.5% of the sample had either 6–10 years or over 20 years work experience in that profession. However, 30.8% had been in that particular position at the centre for less than a year, whilst 28.2% had been in the position at the centre for five to six years suggesting that this was a relatively new staff at the centre. They also reported that the majority of the staff was working full time with 48.7% of the sample working over 40 hours per week, and 43.6% working <40 hours per week.
The sample for time two (staff who completed baseline measures, focus group discussion, and time 2 measures) was comprised of 31 participants out of the original 39 participants (n=3 administration, n=8 primary care providers, n=6 dental staff providers, n=7 behavioural health staff, n=6 health educators, and n=1 physical therapist) at time one. The gender distribution remained the same from time one to time two, however, the racial distribution shifted downward with 25.8% of the sample at time two being African American and 54.8% non-Hispanic White. All staff that dropped out at time two were support staff, six out of the eight were from the primary care groups, and most were African American and female. The composition of staff from the other groups remained unchanged. Demographics for education also shifted, with participants with some college education dropping to 12.9% and those with graduate degrees increasing to 61.3%. Related to this change in demographics from time one to time two was a shift in years in current position at the Centre with those working in their positions for less than a year dropping to 25.8% and those in their current positions for five to six years increasing to 32.3%. Hours worked per week did not shift substantially with the same distribution at times one and two.
Descriptive statistics were run for the two self-report measures (5 scales) of provider collaboration (time one and time two) including minimum, maximum, mean, standard deviation, and α coefficient (see Table 1).
Table 1.
Descriptive statistics at time 1 and time 2
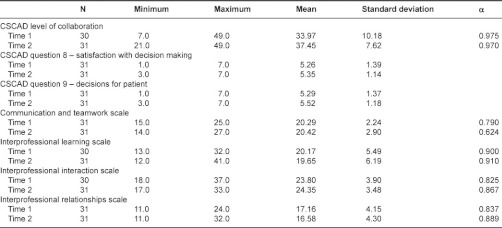
All collaboration scales at time one and time two demonstrated good reliability with Cronbach’s alphas ranging from 0.624 to 0.975. Questions eight and nine on the Collaboration and Satisfaction about Care Decisions Scale were single item scales, therefore, they did not have α coefficients. Bivariate correlations were then conducted for the five collaboration scales at time one and time two. These correlations suggested that associations on the measures of collaboration were positively and significantly associated with each other, demonstrating good validity of the collaboration questionnaires.
Paired t-tests on the measures of collaboration were conducted to evaluate changes in providers’ attitudes about collaboration after participating in the focus group discussions. Participants were asked to complete the five self-report collaboration scales again (at time two) three months after baseline, but many of the responses came as much as eight months later, which affected the significance of our results. Whilst a few of the late responses were due to providers leaving the Centre and requiring numerous attempts to reach them, the reasons for most late responses were less clear and may have been due to a design flaw in not assessing feasibility issues at the Centre as providers have heavy clinical caseloads. Additional reasons may stem from issues about power and status, given that support staff who were primarily African American and female were the non-responders for time two measures. A paired sample t-test two-tailed analysis was calculated to examine significant mean differences between time one and time two responses on the five collaboration self-report scales.
The results revealed that mean scores on the following collaboration scales changed in the expected direction after participating in the same discipline focus group discussions, with more collaboration reported at time two: Collaboration and Satisfaction about Care Decisions Scale Level of Collaboration (t(29)=–2.087, p=0.046), Question eight – Satisfaction with Decision Making (t(30)=0.361, p=0.720), Question nine – Decisions for Patient (t(30)=–0.839, p=0.408), Interprofessional Learning Scale (t(29)=0.358, p=0.723), and Interprofessional Relationship Scale (t(30)=0.809, p=0.425. However, only the change for the Collaboration and Satisfaction about Care Decisions Scale Level of Collaboration from time one to time two was statistically significant (p=0.046). The results for the Communication and Teamwork Scale (t(30)=–0.254, p=0.801) and the Interprofessional Interaction Scale (t(29)=–0.981, p=0.335) were not in the expected direction (less collaboration reported from time one to time two), and were not statistically significant.
Finally, an ANOVA was conducted to evaluate whether or not responses on the collaboration measures differed by race, education, and professional roles of staff members. First, race of staff member was evaluated. Results for the Collaboration and Satisfaction about Care Decisions Scale Level of Collaboration – Time one were significant (F(5,24)=3.642, p=0.014). Hispanic respondents reported the greatest levels of collaboration and African American staff reported the lowest levels of collaboration. Results were not statistically significant for Collaboration and Satisfaction about Care Decisions Scale Level of Collaboration – Time two.
An ANOVA was then calculated to evaluate whether or not responses on the collaboration scales varied by staff members’ levels of education. Results were significant for Collaboration and Satisfaction about Care Decisions Scale Level of Collaboration – Time one (F(4,25)=4.038, p=0.012). Staff members with graduate degrees reported the greatest levels of collaboration, whilst staff with some college and some graduate school reported the lowest levels of collaboration. The Collaboration and Satisfaction about Care Decisions Scale Question eight – Satisfaction with Decision Making – Time one was also significant (F(4,26)=4.128, p=0.010). Staff with some graduate school education reported the greatest satisfaction with decision making, and staff with high school education reported the lowest satisfaction with decision making. Another significant finding was for the Collaboration and Satisfaction about Care Decisions Scale, Question nine – Decisions for the Patient – Time one (F(4,26)=5.253, p=0.003), as staff with some graduate school education reported the greatest satisfaction with decisions for the patient, and those with high school education reported the lowest satisfaction with decisions for the patient.
The Interprofessional Relationships Scale – Time one was also significant (F(4,26)=3.798, p=0.015). Staff who earned graduate degrees expressed the most positive views of interprofessional relationships, whilst those with some graduate school education expressed the most negative views of interprofessional relationships. Finally, results for the Interprofessional Relationships Scale – Time two were significant (F(4,26)=3.499, p=0.021). Respondents with graduate degrees had the most positive views of interprofessional relationships, whilst those with either a high school degree or a bachelor’s degree had the most negative views of interprofessional relationships.
An ANOVA was finally calculated to evaluate whether or not responses on the five collaboration scales varied by profession. Results were significant for CSCAD Level of Collaboration – Time one (F(5,24)=3.219, p=0.023) and for Time two (F(5,25)=3.188, p=0.023). The Collaboration and Satisfaction about Care Decisions Scale question eight – Satisfaction with Decision Making – Time two was also significant (F(5,25)=4.505, p=0.005). Another significant finding was for the Collaboration and Satisfaction about Care Decisions Scale question nine – Decisions for the Patient – Time two (F(5,25)=4.849, p=0.003). Finally, results for the Interprofessional Relationships Scale – Time two were significant (F(5,25)=2.672, p=0.046). For all scales with significant findings, providers who had Administrative roles reported the most positive views on collaboration and Dental providers reported the least positive views.
Qualitative findings from the focus groups revealed five dominant themes including (i) facilitators of collaboration, (ii) barriers to collaboration, (iii) provider characteristics and collaboration, (iv) patient characteristics and collaboration, and (v) family and community involvement. Providers who participated in the six focus groups described facilitators (communication systems, provider interactions, patient factors, structural/building issues, shared vision) and barriers (patient factors, provider interactions, volume of work, structural/building issues) to collaboration. Some non-medical staff at the Centre also stated that the medical staff tended to have more power and influence over clinical case decision making than the other providers which has caused some tension among providers at this health centre.
Additionally focus group findings revealed that provider demographics, provider work overload, provider roles, and patient demographic characteristics (e.g. cultural factors, underprivileged) were factors that providers reported affect collaboration at the health centre. Providers’ perceptions of care revealed a more patient-centred approach with limited family involvement in care. Staff in four of the six focus groups stated that patients’ demographic characteristics did not or should not affect the collaborative process with providers. However, other staff (e.g. support staff, mental health providers) recognized the multiple issues that their underprivileged patients often face. Most staff identified that they were not biased in their care and provided equal care regardless of patient characteristics, such as race, ethnicity, class, and gender, suggesting that every patient at the Centre is treated the same way.
Discussion
Diverse views of collaboration were found in the quantitative findings presented in this paper. The Inter-professional Relationships scale, and questions eight and nine on the Collaboration and Satisfaction about Care Decisions Scale indicated more positive responses at the Centre among participants. Providers’ demographic variables (e.g. race, education, and profession) were all relevant to views on collaboration. Despite research findings that suggest the presence of provider bias in health care delivery while working with ethnic and racial minorities [28], most participants in this study did not recognize how these contextual variables could be affecting their interactions with patients at the Centre. African American staff, for example, was generally in positions of lower professional status, earned less income, and had lower levels of education compared to non-Hispanic White staff at the Centre. African American participants also reported the least positive views of collaboration according to the self-report measures included in this study. This included eight support staff with positions as medical assistants within primary care or as front desk personnel.
Likewise, providers from behavioural health, dental, and nurse family partnership health educators reported the least positive scores regarding the quality of their collaboration with other providers at the Centre. This may be because of the hierarchical position of primary care in relationship to the other professional groups. In contrast, staff with graduate degrees, particularly administrators and primary care practitioners reported the most positive views of collaboration. Each member of the healthcare team plays an important role in the process of collaborative care and this includes front desk staff, medical assistants, medical and mental health providers, dental providers and administration. However, all providers’ voices have not always been heard or valued in prior research examining providers’ views of collaborative care models.
Qualitative data helped to enrich our quantitative findings. For example, according to findings from the six same discipline focus groups, providers perceived that collaboration was facilitated by having colocated services at the Centre and by using technology to facilitate sharing information about patients who often have complex lives (e.g. underprivileged status and exposure to violence and trauma) and health concerns (e.g. diabetes, chronic pain, sexually transmitted diseases, hypertension, and depression). Focus groups participants described health disparities their patients experience because of their disadvantaged social status (e.g. low income poor, racial/ethnic minorities, primarily women) and generally being in poorer health and with greater health risks when compared to more advantaged social groups.
The focus group findings revealed more information about the collaborative process between disciplines. Whilst varied disciplines attributed coordinated and collocated services as enhancing collaboration for this primarily Medicaid population, differences in views among the provider groups also emerged. There was notable tension and disagreement between the primary care and behavioural healthcare departments, specifically that primary care staff did not seem to value their inter-departmental meetings and primary care’s perception of a condescending attitude from the behavioural health department. Dental providers reported feeling marginalized at the health centre due to their location in the basement, feeling isolated, and missing out on more informal face to face contact in the upper levels of the building. Whilst this informal exchange involves privileged professional groups, dealing with the hierarchy and power within the healthcare context between primary care and other groups continues to be problematic.
Participants described challenges during the focus group discussions which were not fully captured in the quantitative findings examining providers’ views of collaboration before and after participating in the same discipline focus group discussions. Structural issues, such as the building layout (e.g. dental in the basement) and the lack of a shared and fully integrated medical/mental health record was reported as impeding communication about shared clinical cases. Time and work volume issues revealed provider overload. Primary care staff acknowledged that it was hard to take the time to discuss patients with the high patient volume currently served at the centre. Whilst productivity and reimbursement concerns were central to what was shared during the focus groups, particularly among providers from primary care, this was also one of the groups who reported the most positive views of collaboration on the self-report measures. Dental, behavioural health, and health educators reported the least positive views of the collaboration according to the time one and time two quantitative self-report measures.
Providers’ roles and duties seem to affect views of collaboration which can also influence patient care. For example, focus group findings revealed that front desk staff may hear patient information that other providers do not hear, and they often play a crucial role disseminating this information to all providers, reinforcing that listening and valuing input across all levels of staff is important to promote collaborative care. Management level providers may have more opportunities and involvement in upper level meetings which facilitates collaboration since these upper level groups tend to see each other more regularly. These reported interactions described in the focus groups may help to explain the lack of time two response for support staff in completing the quantitative questionnaires on collaboration. Perhaps front desk staff has less opportunity and structured time to meet and discuss information regarding shared patient care, and likewise did not feel they had the structured time to complete time two surveys capturing their views of collaboration at the centre.
Another important aspect communicated by the Centre staff regarding collaboration, was not only how they communicated with each other but their personal connection to their patients. Providers at all levels frequently noted during the focus group discussions their desire to provide the best health care possible to all of their patients and to advocate for them regarding referring them to other services and finding insurance and low cost medication options. These efforts seemed effective as the staff at the Centre described a great deal of word of mouth referrals within the community, suggesting that the community values their efforts and collaborative model of care.
Healthcare teams who embrace collaborative care across all levels may better address multiple and often complex health conditions for their patients. Findings from this study can inform future directions that staff at this Centre takes to further develop their collaborative process and to help improve health outcomes and/or efficiency in cost-effective delivery of patient care. Based on the results of this study, the Centre is currently functioning between levels three and four of collaboration [29] as on-site collaboration is often occurring and mental health professionals and healthcare professionals tend to have separate record systems, with the exception of a few behavioural healthcare providers imbedded within primary care who do share a medical record with the primary care providers.
Katon and Selig [30] suggest that collaboration and team care are beneficial to patient outcomes, nonetheless prior studies on collaboration have often focused on the physician-nurse collaboration, particularly nurse practitioners [26, 27, 31, 32]. However, today there is a broader group of professionals and staff working with patients in individual, collocated, and integrated models of care. Miers and Pollard [33], Irvine and colleagues [34] and Jelphs and Dickinson [35] reported that barriers related to professional divisions, power and hierarchies, stereotyping, and differing value systems among varied staff and practitioners all exist. These barriers can lead to unintentionally marginalizing those staff with less professional titles and staff who are not centrally located in primary care.
This study adds to the developing literature on collaboration care models in primary care by providing insight into the diverse perspectives of support staff, practitioners, and administrators in a federally qualified nurse managed community based primary health care centre. Perspectives about collaboration are critical given the organizational structure of collated services, trans-disciplinary focus, and the inclusion of diverse personnel. Moreover, this Centre actively seeks evidence-based information (which this study additionally provides) to inform changes that will address their efficiency and quality of care. For example, to address improved access to care, several years ago the Centre changed their policy to open access for appointments (same day appointment scheduling) rather than the more traditional scheduling to mitigate no show appointments and to improve the access of healthcare to their underprivileged patients. Accommodating patients' health care needs and providing continuous, routine care can improve patient flow and foster a better patient-provider relationship. Also, to address some of the contextual and structural factors that can influence the collaboration process changes that have taken place since the completion of this study include:
hiring more diverse providers serving in professional and administrative roles as well as bilingual staff;
development of a data base which stores information (medical and mental health) about patient care that is accessible to all Centre staff;
plans for centre expansion (land has been purchased; a campaign is underway to obtain funds for the building); and intentions to implement centre wide cultural sensitivity training.
The Centre personnel need to objectively examine their level of collaboration so that they can progress towards improved care coordination which can influence patient outcomes. Regular evaluation of all staff’s views of collaboration can inform strategic thinking, planning, and actions to determine changes needed to improve the collaboration process. Other models of primary care within the United States can benefit from our findings, by taking proactive steps to ask staff at all levels about their perspectives on collaboration (e.g. facilitators, barriers, and opportunities for change) including clinical care decisions, as well as collaborative communication and views about teamwork. Professional collaboration in this study includes a unique number and mix of diverse personnel working in an urban region at a nurse managed community based primary health care centre that seeks to provide high quality care to an underserved patient population.
This study has a number of limitations that may have affected the findings, including missing data from time two which limited input from African American female support staff. Due to this attrition, the voices of support staff were not well represented in the final quantitative results, which was one of the primary aims of this study in trying to capture the views of all staff at the Centre. Time two data collection was limited despite efforts to prevent drop-out through using numerous email reminders, dropping off hard copies of the measures on several occasions, and attending quarterly staff meeting to remind participants to complete their time two data. It would have been better to have time two measures completed immediately after the focus group discussions to more accurately measure change in views as a result of participating in the same discipline focus groups. Moreover, having same discipline focus groups could have hindered more change promoting discussions about collaboration. A primary aim of this study was to examine views about collaboration among a diverse group of providers at a nurse managed health care centre. Given the unique structure of this facility, however, generalizability may be limited to similarly structured nurse managed centres. Finally, because quantitative data were self-report, findings are based on the authenticity of responses participants provided given that observational data were not used to triangulate the individual level data.
Conclusion
Since collaborative care requires active partnerships from staff at all levels, input from support staff and from racial and ethnic minority groups of providers is critical. Due to their marginalised professional and racial status some staff may have felt less empowered to participate in this mixed method research study and may not have believed their opinions through completion of the instruments mattered. This study will facilitate the Centre’s understanding of how issues of power and privilege could be affecting their providers’ views of collaboration. Since the conclusion of data collection, findings from this study were presented to all staff at a Centre-wide meeting and based on feedback during this meeting, all levels of staff are now working toward more active partnerships among all levels of staff.
Findings from this study provided valuable insights regarding the collaborative process at this site specifically, and about collaborative care in general. Additional research is needed to examine how collaborative care occurs in different healthcare settings that have varied professional groups and models of care and serve diverse patient populations. Addressing limitations from this study when designing future research will enable improved comparisons when examining perspectives on collaboration at this Centre and other sites serving similarly diverse patient populations. This process will also more fully explore how collaboration differs depending on the interactions within diverse provider groups. Additionally, whilst this research was designed to examine the perspectives of all levels of health care providers, exploring the perspectives of the patients and families being treated, will further enrich our understanding of collaborative care and how to address health disparities from a more systemic perspective.
Acknowledgments
We want to acknowledge and thank all of the staff at The Eleventh Street Family Health Services of Drexel University in Philadelphia. Special thanks to Dr. Patricia Gerrity and Jane Franks for giving us the opportunity to work with you and your staff to improve the excellent care the health centre is already providing.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sections.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Contributor Information
Patricia Bruner, Department Couple and Family Therapy, Drexel University, Philadelphia, PA, USA.
Roberta Waite, College of Nursing and Health Professions, Drexel University, Philadelphia, PA, USA.
Maureen P Davey, Department Couple and Family Therapy, Drexel University, Philadelphia, PA, USA.
Reviewers
Susan Brajtman, RN PhD, Associate Professor, School of Nursing, University of Ottawa, Canada
Jennifer Hodgson, PhD, Associate Professor of Child Development and Family Relations, College of Human Ecology, Adjunct Professor in the Departments of Family Medicine and Internal Medicine, East Carolina University, Rivers RW 130, Greenville, NC 27858-4353, USA
Angela Lamson, PhD, Family Therapy Clinic, Marriage and Family Therapy/Medical Family Therapy Program, Department of Child Development & Family Relations, East Carolina University, Greenville, NC 27858-4353, USA
Dan Marlowe, PhD, Director of Behavioral Science and Community Medicine, Duke/SRAHEC Family Medicine Residency Program, Consulting Associate in the Department of Psychiatry and Behavioral Science, Duke University Medical Center, 1601 Owen Drive, Fayetteville, NC 28304-3425, USA
References
- 1.Kessler R, Berglund P, Bruce M, Koch J, Laska E, Wang P. The prevalence and correlates of untreated serious mental illness. Health Services Research. 2001;36:987–1007. [PMC free article] [PubMed] [Google Scholar]
- 2.Mauksch L, Tucker S, Katon W, Russo J, Cameros J, Walker E. Mental illness, functional impairment, and patient preferences for collaborative care in an uninsured, primary care population. The Journal of Family Practice. 2001;50:41–7. [PubMed] [Google Scholar]
- 3.Brown D, Hernandez A, Saint-Jean G, Evans S, Tafari I, Brewster L. A participatory action research pilot study of urban health disparities using rapid assessment response and evaluation. Health Policy and Ethics. 2008;98:28–38. doi: 10.2105/AJPH.2006.091363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen E, Paterson L. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychology. 2006;25:704–14. doi: 10.1037/0278-6133.25.6.704. [DOI] [PubMed] [Google Scholar]
- 5.Oxman T, Dietrich A, Schulberg H. The depression care manager and mental health specialist as collaborators within primary care. American Journal of Geriatric Psychiatry. 2003;11:507–16. [PubMed] [Google Scholar]
- 6.Unutzer J, Schoenbaum M, Druss B, Katon W. Transforming mental health care at the interface with general medicine: Report for the President’s commission. Psychiatric Services. 2006;57(1):37–47. doi: 10.1176/appi.ps.57.1.37. [DOI] [PubMed] [Google Scholar]
- 7.D'Amour D, Goulet L, Labadie J, Martín-Rodriguez L, Pineault R. A model and typology of collaboration between professionals in healthcare organizations. BMC Health Services Research. 2008;8:188–211. doi: 10.1186/1472-6963-8-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nash DB, Reifsnyder J, Fabius RJ, Pracilio VP. Population Health: creating a culture of wellness. Google Books. [cited 2011 27 June]. Available from: http://books.google.com/books/about/Population_Health.html?id=-X2HAWROnEQC. [Google Scholar]
- 9.Butt G, Markle-Reid M, Browne G. Interprofessional partnerships in chronic illness care: a conceptual model for measuring partnership effectiveness. International Journal of Integrated Care [serial online] 2008 May 14;8 doi: 10.5334/ijic.235. [cited 2011 3 August]. Available from http://www.ijic.org. URN:NBN:NL:UI:10-1-100477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blount A. Integrated primary care: organizing the evidence. Families, systems & health. 1992 [cited 2022 26 June]. Available from: http://www.integratedprimarycare.com/organizing_the_evidence.pdf. [Google Scholar]
- 11.McDaniel S, Hepworth J, Doherty W. Medical family therapy: a biopsychosocial approach to families with health problems. New York: Basic Books; 1992. [Google Scholar]
- 12.Seaburn D, Lorenz A, Gunn W, Gawinski B, Mauksch L. Models of collaboration: a guide for mental health professionals working with health care practitioners. New York: Basic Books; 1996. [Google Scholar]
- 13.Gerdes J, Yuen E, Wood G, Frey C. Assessing collaboration with mental health providers: The primary care perspective. Families, Systems & Health. 2001;19:429–43. [Google Scholar]
- 14.Todahl J, Linville D, Smith T, Barnes M, Miller J. A qualitative study of collaborative health care in a primary care setting. Families, Systems & Health. 2006;24:45–64. [Google Scholar]
- 15.Rose L. Interprofessional collaboration in the ICU: how to define? Nursing in Critical Care. 2011;16(1):5–10. doi: 10.1111/j.1478-5153.2010.00398.x. [DOI] [PubMed] [Google Scholar]
- 16.Miller HL, Hall SE, Hunley SA. Value perceptions of integrative health care: a study of primary care physicians and professional clinical counselors. Journal of Contemporary Psychotherapy. 2004;34:117–24. [Google Scholar]
- 17.Bischof GH, Lieser ML, Taratuta CG, Fox AD. Power and gender issues from the voices of medical family therapists. In: Prouty Lyness AM, editor. Feminist perspectives in medical family therapy. New York: Haworth Press Inc.; 2003. pp. 23–54. [Google Scholar]
- 18.Reddy M, Jansen B. A model for understanding collaborative information behavior in context: A study of two healthcare teams. Information Processing and Management. 2008;44(1):256–73. [Google Scholar]
- 19.Halvorsen K, Granas A, Stensland P. International Journal of Pharmacy Practice. Wiley Online Library. 1994. A qualitative study of physicians' and nurses' experiences of multidisciplinary collaboration with pharmacists participating at case conferences. [cited 2011 27 June 27]. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.2042-7174.2011.00129.x/abstract. [DOI] [PubMed] [Google Scholar]
- 20.Davey M, Brunner P, Waite R. Culturally sensitive collaborative care models: exploration of a community based health centre. Family Systems and Health (July, 2011, Accepted) doi: 10.1037/a0025025. [DOI] [PubMed] [Google Scholar]
- 21.Krueger RA. FGs: A practical guide for applied research. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 22.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 23.Baggs J. Development of an instrument to measure collaboration and satisfaction about care decisions. Journal of advanced Nursing. 1994;20:178–82. doi: 10.1046/j.1365-2648.1994.20010176.x. [DOI] [PubMed] [Google Scholar]
- 24.Pollard K, Miers M, Gilchrist M. Collaborative learning for collaborative working? Initial findings from a longitudinal study of health and social care students. Health and Social Care in the Community. 2004;12:346–58. doi: 10.1111/j.1365-2524.2004.00504.x. [DOI] [PubMed] [Google Scholar]
- 25.Pollard K, Miers M, Gilchrist M. Second year skepticism: Pre-qualifying health and social care students’ midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. Journal of Interprofessional Care. 2005;19:251–68. doi: 10.1080/13561820400024225. [DOI] [PubMed] [Google Scholar]
- 26.Wing P, O'Grady E, Langeher M. Changes in the legal environment of nurse practitioners 1991–2000. American Journal of Nurse Practice. 2005;9(2):25–39. [Google Scholar]
- 27.American College of Physicians. Nurse practitioners in primary care: a policy monograph of the American College of Physicians. Philadelphia (PA): ACP; 2009. [Google Scholar]
- 28.Breland-Noble AM, Bell C, Nicolas G. Family first: the development of an evidence-based family intervention for increasing participation in psychiatric clinical care the research in depressed African American adolescents. Family Process. 2006;45:153–69. doi: 10.1111/j.1545-5300.2006.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doherty WJ. The why’s and levels of collaborative family healthcare. Families Systems Medicine. 1995;13:275–81. [Google Scholar]
- 30.Katon W, Selig M. Population-based care of depression: team care approaches to improving outcomes. Journal of Occupational and Environmental Medicine. 2008;50(4):459–67. doi: 10.1097/JOM.0b013e318168efb7. [DOI] [PubMed] [Google Scholar]
- 31.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press; 2001. [PubMed] [Google Scholar]
- 32.Institute of Medicine. Health professions education: a bridge to quality. Washington (DC): National Academies Press; 2003. [PubMed] [Google Scholar]
- 33.Miers M, Pollard K. The role of nurses in interprofessional health and social care teams. Nursing Management. 2009;15(9):30–36. doi: 10.7748/nm2009.02.15.9.30.c6882. [DOI] [PubMed] [Google Scholar]
- 34.Irvine R, Kerridge I, McPhee J. lnterprofessionalism and ethics: consensus or clash of cultures? Journal of Interprofessional Care. 2002;16:199–209. doi: 10.1080/13561820220146649. [DOI] [PubMed] [Google Scholar]
- 35.Jelphs K, Dickinson H. Working in Teams. Bristol: The Policy Press; 2008. [Google Scholar]


