Abstract
Background
Study results concerning associations between body mass index (BMI) and psychological distress are conflicting. The purpose of this study was to describe the shape of the association between BMI and psychological distress in a large sample of Swedish adults.
Methods
Data was measured with the General Health Questionnaire-12 (GHQ-12), in 68,311 adults aged 18–74. Self-reported data was derived from a merger of the 2000, 2004 and 2008 Life and Health (Liv och Hälsa) questionnaires focusing general perceived distress as well as living conditions. Logistic regression analysis was used to describe the association between BMI and psychological distress when controlled for age and gender in combination.
Results
Women reported an overall higher psychological distress than men. A significant pattern of decreasing psychological distress with increasing age emerged among women in all BMI categories. Trends of this same pattern showed for men. Small or no differences were seen in psychological distress between those in normal weight, overweight, and obesity I categories (among women: 20.4%, 18.4%, 20.5%; among men: 12.8%, 11.2%, 12.9%). For both genders, any notable increase in psychological distress appeared first in the obesity II category (among women: 27.2%. Among men: 17.8%).
Conclusions
Psychological distress decreases with increasing age regardless of BMI; a pattern more obvious for women. Being categorized with obesity II leads to a markedly higher psychological distress than being categorized with normal weight, overweight or obesity I. From this, we suggest that future obesity research focusing on psychological distress could investigate the role of stigma and norm susceptibility in relationships where people are evaluated through the eyes of the other.
Keywords: BMI, Psychological distress, GHQ-12, Gender, Age
Background
In the medical model put forward by various medical and governmental health organizations, a body mass index (BMI) that is above normal is associated with a heightened risk of several diseases ([1,2]; World Health Organization, [3]). At the same time, a growing field of studies question whether BMI measurements reveal any general truth about an individual’s state of health [4-7].
The association between BMI and psychological distress is even less clear [8-15]. We follow scholars that view psychological distress as an emotional disturbance that may impact on as well as result from the social functioning and day-to-day living of individuals [16,17].
Studies on relationships between BMI and different measurements of psychological distress produced contradictory results. On the one hand, epidemiological studies have found positive correlations between BMI and psychological distress, although this was the case particularly in individuals with a BMI of 35 or higher [18,19]. BMI has also been associated with a diversity of psychological distress conditions such as low self-esteem, poor self-image, and depression; however, this association was significantly higher in individuals with a BMI above 40 [20].
On the other hand, Atlantis and Ball’s [21] population study, in which anxiety and depressive symptoms were the indicators of psychological distress, showed no association between BMI and psychological distress. Huang et al. [22] investigated a large population (n = 14,221) and found that BMI was associated to physical ill-health but not to psychological distress.
Several studies have found that various life factors influence the relationship between BMI and psychological distress. In an extensive review, Bacon and Aphramor [23] noted, however, that epidemiological studies rarely acknowledge factors like fitness, activity, nutrient intake, weight cycling, or socioeconomic status when considering the connection between BMI and psychological distress. When studies do control for these factors, increased risk of psychological distress disappears or is significantly reduced [24]. Lund et al. [25] found, for example, that unemployment among the morbidly obese affected their quality of life more than the weight did. In their study which controlled for individual’s overall health status, Loff and Crammond [26] found that the association between BMI and psychological distress disappeared.
While age is a factor that seems to affect the association between BMI and psychological distress, the extent to which it happens is unclear. Correlations have been found among the elderly [27,28]; however the studies did not control for their general state of health, such as chronic diseases and disabilities. Studies have also found that among the elderly being underweight because of an increase in general disease symptoms has a more negative impact on psychological distress than being overweight [29,30]. Some studies have found significant correlations between BMI and psychological distress among middle-aged women [31].
Several studies show that correlations between BMI and psychological distress seem to be stronger for women than for men [18]. However, there are also studies in which the results did not show gender differences regarding BMI and psychological distress [12,32].
Since studies of the relationship between BMI and psychological distress points in different directions, the relationship must be further investigated [22,33,34]. Overall, very few studies have investigated how age and gender in combination affect the association between BMI and psychological distress— especially in a general population. The aim of this study is to further explore the BMI and psychological distress association by taking age and gender into account.
Method
Data sample
This study was based upon data from three surveys carried out 2000, 2004, and 2008 in a mid-Swedish region (Liv och Hälsa 2000, 2004, 2008). The sample consisted of 203,918 individuals aged 18–84 years. The response rate was 63% (128,468 individuals). Only data for those in the age group 18–74 (M = 49 SD = 16) with a BMI 18.5 to 60 (M =26 SD =4.3) were selected. This final data sample consisted of 68,311 individuals.
The survey was approved by the boards of the County Councils of Uppsala, Sörmland, Västmanland, Värmland and Örebro. The survey was conducted under the jurisdiction of the Swedish law, the Helsinki declaration and international guidelines. An approval from an ethics committee was not applicable because the data are anonymous.
Individuals with values below BMI 18.5, which were considered underweight, were excluded from this study because the focus was on overweight and obesity in comparison to normal weight. Individuals with BMI above 60, which were considered extreme values, were also excluded. Individuals above 75 years of age were excluded. Very few of these individuals had BMI measurements indicating obesity. In addition, in this age group being underweight is held to be a greater health problem than being overweight [29,30].
Instruments
The General Health Questionnaire 12 (GHQ 12) was used as a measure of psychological distress (Cronbach’s alpha = .90). Following Goldberg’s GHQ scoring method [35], the response alternatives were categorized as 0-0-1-1, which allows for a total score ranging from 0 to 12. A total score of three and above was categorized as psychological distress. The GHQ12 comprises questions about general level of happiness and symptoms of depression and anxiety symptoms over the last four weeks ([36] in [37]). The GHQ 12 avoids self-reflective bias as respondents are asked to value their general psychological distress independent of physical limitations.
We used the following four BMI classifications: normal weight (BMI 18.50–24. 99), overweight (BMI 25.00–29. 99), obesity I (BMI 30.00–34.99) and obesity II (BMI >35.00).
The sample was divided by age into six groups: 18–24, 25–34, 35–44, 45–54, 55–64, and 65–74. A weight-age variable was created by combining the four weight groups and the six age groups, resulting in 24 combinations according to the following scheme: 1 = Normal Weight/18–24 years, 2 = Normal Weight/25–34 years […], 24 = Obesity II/65–74 years.
Processing of data
Statistical software employed for the analyses was SPSS 17.0. Conventional table analysis and logistic regression analysis were used to analyze data. Confidence Interval (CI) was set to 95%. Logistic regression analysis produces odds ratios to express a relative risk that an event or a condition will occur. In the logistic regressions the reference value is 1. We used the age group 65–74 years for our reference group in every BMI category.
Results
As Table 1 shows, psychological distress decreases in relation to BMI for women and men in every age group when age and gender are taken into account except for a very small increase for men in the 25–34 years age group. This decrease is greater for women, ranging from 33.1% among the youngest to 10.1% in the oldest, compared with 17.1% in the youngest men to 6.7% among the oldest. Overall, women report a considerably greater psychological distress than men (20.0% compared to 12.2%). Women reported psychological distress ranging from 18.4 to 20.5% for the normal weight, overweight, and obesity I BMI categories. Men reported psychological distress from 11.2 to 12.9% for the same categories.
Table 1.
Description of participants’ psychological distress (n = 68,311)
| |
Women |
Men |
||||
|---|---|---|---|---|---|---|
| n | % | Psychological distress % | n | % | Psychological distress % | |
| |
36.785 |
53.8 |
20.0 |
31.526 |
46.2 |
12.2 |
| Age Groups |
|
|
|
|
|
|
| 18-24 y |
3.496 |
9.5 |
33.1 |
2.435 |
7.7 |
17.1 |
| 25-34 y |
5.509 |
15.0 |
27.6 |
3.847 |
12.2 |
17.7 |
| 35-44 y |
6.129 |
16.7 |
24.3 |
4.746 |
15.1 |
16.5 |
| 45-54 y |
6.687 |
18.2 |
20.5 |
5.262 |
16.7 |
13.9 |
| 55-64 y |
7.607 |
20.7 |
14.2 |
7.013 |
22.2 |
9.8 |
| 65-74 y |
7.357 |
20.0 |
10.1 |
8.223 |
26.1 |
6.7 |
| BMI Categories |
|
|
|
|
|
|
| Normal Weight 18.5-24.9 |
19.590 |
53.3 |
20.4 |
12.207 |
38.7 |
12.8 |
| Overweight 25.0-29.9 |
11.635 |
31.6 |
18.4 |
14.585 |
46.3 |
11.2 |
| Obesity I 30.0-34.9 |
4.106 |
11.2 |
20.5 |
3.793 |
12.0 |
12.9 |
| Obesity II >35.0 | 1.454 | 3.9 | 27.2 | 940 | 3.0 | 17.8 |
For both genders, self-reported psychological distress makes a leap from the results in the previous category to those in the obesity II category (12.9 to 17.8% for men, 20.5 to 27.2% for women).
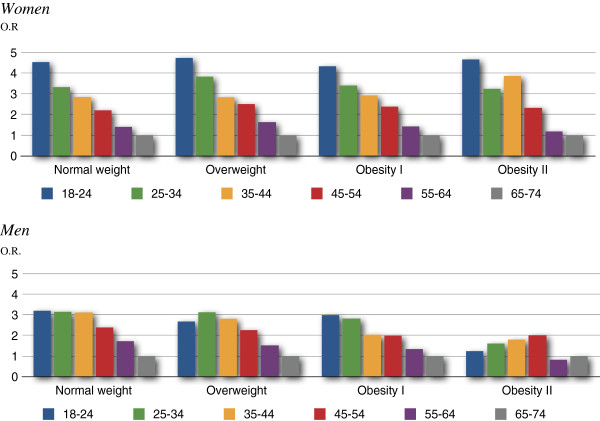
As Table 2 and Figure 1 show, the logistic regression analysis for psychological distress in relation to the 24 weight-age variables revealed a clear pattern of decreasing psychological distress with increasing age among women, in every BMI category.
Table 2.
Logistic regression for psychological distress by BMI-age variable and gender
| BMI-Age |
Women |
Men |
||||
|---|---|---|---|---|---|---|
|
Psychological distress |
Psychological distress |
|||||
| n | % (95% CI) | O.R. within BMI (p) | n | % (95% CI) | O.R. within BMI (p) | |
|
Normal W. |
19.590 |
20.4(19.9-20-9) |
2.56 |
12.207 |
12.2(11.6-12.8) |
2.43 |
|
18.5-24.9 | ||||||
| 18-24y. |
2.635 |
32.5(30.7-34.3) |
4.53(P < .001) |
1.690 |
17.5(15,7-19.3) |
3.22(P < .001) |
| 25-34y. |
3.493 |
26.1(24.6-27.6) |
3.32(P < .001) |
1.894 |
17.2(15.5-18.9) |
3.15(P < .001) |
| 35-44y. |
3.500 |
23.2(21.8-24.6) |
2.84(P < .001) |
1.731 |
17.0(15.2-18.8) |
3.12(P < .001) |
| 45-54y. |
3.469 |
19.0(17.7-20.3) |
2.20(P < .001) |
1.790 |
13.6(12.0-15.2) |
2.39(P < .001) |
| 55-64y. |
3.475 |
13.2(12.1-14.3) |
1.44(P < .001) |
2.314 |
10.2(9.0-11.4) |
1.72(P < .001) |
| 65-74y. |
3.018 |
9.6(8.6-10.6) |
1 |
2.788 |
6.2(5.3-7.1) |
1 |
|
Overweight |
11.635 |
18.4(17.7-19.1) |
2.75 |
14.585 |
11.2(10.7-11.7) |
2.24 |
|
25.0-29.9 | ||||||
| 18-24y. |
608 |
33.4(29.7-37.1) |
4.73(P < .001) |
578 |
15.2(12.3-18.1) |
2.68(P < .001) |
| 25-34y. |
1.293 |
28.8(26.3-31.3) |
3.83(P < .001) |
1.450 |
17.4(15.5-19.3) |
3.14(P < .001) |
| 35-44y. |
1.697 |
23.0(21.0-25.0) |
2.83(P < .001) |
2.268 |
15.8(14.3-17.3) |
2.81(P < .001) |
| 45-54y. |
2.199 |
21.0(19.3-22.7) |
2.50(P < .001) |
2.633 |
13.2(11.9-14.5) |
2.26(P < .001) |
| 55-64y. |
2.873 |
14.8(13.5-16.1) |
1.63(P < .001) |
3.564 |
9.3(8.4-10.2) |
1.52(P < .001) |
| 65-74y. |
2.965 |
9.6(8.6-10.6) |
1 |
4.092 |
6.3(5.6-7.0) |
1 |
|
Obesity I |
4.106 |
20.5(19.3-21.7) |
2.58 |
3.794 |
12.9(11.9-13.9) |
2.03 |
|
30.0-34.9 | ||||||
| 18-24y. |
178 |
36.0(29.0-43.0) |
4.33(P < .001) |
108 |
21.3(16.6-29.0) |
2.99(P < .001) |
| 25-34y. |
477 |
30.6(26.5-34.7) |
3.40(P < .001) |
398 |
20.4(16.4-24.4) |
2.82(P < .001) |
| 35-44y. |
658 |
27.5(24.1-30.9) |
2.92(P < .001) |
598 |
15.6(12.7-18.5) |
2.04(P < .001) |
| 45-54y. |
745 |
23.6(20.6-26.6) |
2.38(P < .001) |
674 |
15.3(12.6-18.0) |
1.99(P < .001) |
| 55-64y. |
951 |
15.6(13.3-17.9) |
1.42(P < .01) |
907 |
10.8(9.8-11.8) |
1.34(n.s.) |
| 65-74y. |
1.097 |
11.5(9.6-13.4) |
1 |
1.109 |
8.3(6.7-9.9) |
1 |
|
Obesity II |
1.454 |
27.2(24.9-29.5) |
2.71 |
940 |
17.8(15.4-20.2) |
1.41 |
|
>35.0 | ||||||
| 18-24y. |
75 |
44.0(32.8-55.2) |
4.66(P < .001) |
59 |
16.9(7.3-26.5) |
1.24(n.s.) |
| 25-34y. |
246 |
35.4(29.4-41.4) |
3.24(P < .001) |
105 |
21.0(13.2-28.8) |
1.61(n.s.) |
| 35-44y. |
274 |
39.4(33.6-45.2) |
3.86(P < .001) |
149 |
22.8(16.1-29.5) |
1.80(P < .05) |
| 45-54y. |
274 |
28.1(22.8-33.4) |
2.32(P < .001) |
165 |
24.8(18.2-31.4) |
2.01(P < .05) |
| 55-64y. |
308 |
16.6(12.4-20.8) |
1.18(n.s.) |
228 |
11.8(7.6-16.0) |
.82(n.s.) |
| 65-74y. | 277 | 14.4(10.3-18.5) | 1 | 234 | 14.1(9.6-18.6) | 1 |
Figure 1.
Psychological distress odds ratios within BMI category ordered by age groups women.
The only exception is for the 35–44 year age group in the obesity II category, where a rise of 4 percentage points is followed by an 11.3% drop in the 45–54 year age group. In Table 2, odds ratios for women show an almost identical pattern within the first three BMI categories. These gradient ratios are statistically significant. Figure 1 shows a step-like pattern of psychological distress in women by age group for the first three BMI categories.
As Table 2 and Figure 1 show, there is a similar trend for men in the first three BMI categories. A small exception is for 18–24 year olds in the overweight category, where self-reported psychological distress drops compared to the following age group. Values are statistically significant at the .001 level, except for the 55–64 year age group in the obesity I category (n.s.). As Figure 1 shows, there is a trend in men of decreasing psychological distress by increasing age in the normal weight, overweight, and obesity I categories.
In the obesity II category, the association with psychological distress changes is different for women than for men. For women, the strong pattern of decreasing psychological distress by increasing age remains, with the exception of an increase for the age group 35–44. Also, in this obesity II category, odds ratios for women in the 55–64 year age group were non-significant. Men in the obesity II category did not show a trend to decreasing psychological distress by increasing age. Instead, an increase in psychological distress in the first four age groups was followed by a drop in odds ratio in the 55–64 year age group.
Discussion
For women, we found a clear step-like pattern of decreasing psychological distress with increasing age regardless of BMI, with a minor exception for obesity II. We have not been able to find this step-like pattern in any other study. Meanwhile, somewhat in line with our results, when dichotomizing age, Minniti et al. [38] found that older overweight and obese women had a better psychological status than their younger counterparts. The step-like pattern for men was similar to that of women, though less pronounced.
Regardless of BMI, women also reported a markedly higher psychological distress than men, which was noted in several other studies [18,22,27,39-41]. A possible explanation was put forward by Lim et al., ([39], who showed that, compared to men, women’s identity and self-image are to a larger extent connected to appearance and, thereby, also weight status.
Any notable increase of psychological distress in relation to BMI was seen first in the obesity II category. Several other studies have come to the conclusion that psychological distress rates are the same for normal weight and overweight persons [23,24,42-44]. What we did not expect, however in line with Knoesen et al. [45], was that this also included the obesity I category.
Possible methodological limitations exist in our study. In line with Smith (et al. [46]), we consider the General Health Questionnaire (GHQ-12) instrument a multi-dimensional and, hence, somewhat blunt measurement of psychological distress. Therefore our results should be viewed more as indications to be enhanced with the aid of more sophisticated instruments for measuring psychological distress. Another possible limitation was the small sized sample of men in the obesity II category (n = 940). This category contained not only the lowest number of respondents but also the widest spread in BMI, ranging from 35.00 to 60.00. This may have contributed to the non-significant results for psychological distress in men in the obesity II category.
A major strength of this study is the big sample size it employed. Here, we consider our results to call for future research on important cut-off points where body weight truly becomes a risk for increased psychological distress. Let us finally highlight an emerging hypothesis; one that deals with stigma and norm susceptibility.
Taking stigma into account, the mechanisms that alter the association between BMI and psychological distress at the top of the scale could be further explored by investigating the role of interpersonal relationships in which people are defined and evaluated through the eyes of the other. Deborah Carr and colleagues [47] have performed several studies on the stigmatization of obese persons. Their results show how obese persons that belong to social strata where obesity is less culturally normative are more likely to experience and perceive interpersonal mistreatment [47].
Perhaps a person’s distance to a cultural norm changes both that person’s exposure for and susceptibility to stigmatizing treatment –in turn affecting psychological distress. Considering some well-established normative claims of our self-producing society, where being male brings more advantages than being female, where being thin is more desirable than being fat and where being young is viewed as more attractive than being old, a norm /stigma susceptibility theory could help to explain the heightened psychological distress in the obesity II category.
Conclusions
Psychological distress decreases with increasing age regardless of BMI. The pattern was obvious for women, less pronounced for men. Being categorized with obesity II, being woman or being younger lead to a markedly higher psychological distress than being man, older or categorized with normal weight, overweight or obesity I.
Future obesity research could investigate more thoroughly where and why an increasing weight becomes a risk for heightened psychological distress. Here we would suggest an exploration of the role of interpersonal relationships in which people are defined and evaluated through the eyes of the other, perhaps a study resting on the basis of a norm/stigma susceptibility theory.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SB initiated the study and held the overall responsibility. She designed the study, gathered background material, analyzed data, performed data base searches, prepared and completed the manuscript. UR performed data base searches, compiled parts of the background articles, revised the manuscript critically and made a draft to the introduction. BS continuously revised the design and the data analyses as well as the article’s intellectual content. All authors have read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Susanne Brandheim, Email: susanne.brandheim@kau.se.
Ulla Rantakeisu, Email: ulla.rantakeisu@kau.se.
Bengt Starrin, Email: bengt.starrin@kau.se.
Acknowledgements
The Life and Health (Liv & Hälsa) questionnaires (2000, 2004 & 2008) were financially funded by the Swedish county Council of Värmland.
References
- International Obesity Task Force. EU platform on diet, physical activity and health. Brussels: International Obesity Task Force; 2005. [Google Scholar]
- Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [No authors listed] [DOI] [PubMed] [Google Scholar]
- World Health Organization. http://www.euro.who.int/en/what-we-do/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi.
- Cobb N. Governance through publicity: anti-social behavior orders, young people, and the problematization of the right to anonymity. J Law Soc. 2007;34(3):342–373. doi: 10.1111/j.1467-6478.2007.00396.x. [DOI] [Google Scholar]
- Evans B, Colls R. Measuring fatness, governing bodies: the spatialities of the body mass index (BMI) in anti-obesity politics. Antipode. 2009;41(5):1051–1083. doi: 10.1111/j.1467-8330.2009.00706.x. [DOI] [Google Scholar]
- Oliver JE. The politics of pathology: How obesity became an epidemic disease. Perspect Biol Med. 2006;49(4):611–627. doi: 10.1353/pbm.2006.0062. [DOI] [PubMed] [Google Scholar]
- Rail G, Holmes D, Murray SJ. The politics of evidence on ‘domestic terrorists’: obesity discourses and their effects. Soc Theory Health. 2010;8:259–279. doi: 10.1057/sth.2009.10. [DOI] [Google Scholar]
- Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes. 2008;32(6):881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- Cornelisse-Vermaat JR. et al. Body mass index, perceived health, and happiness: their determinants and structural relationships. Soc Indic Res. 2006;79:143–158. doi: 10.1007/s11205-005-4097-7. [DOI] [Google Scholar]
- Herman KM, Hopman WM, Vandenkerkhof EG, Rosenberg MW. Physical activity, body mass index, and health-related quality of life in Canadian adults. Med Sci Sports Exerc. 2012;44(4):625–636. doi: 10.1249/MSS.0b013e31823a90ae. [DOI] [PubMed] [Google Scholar]
- Kelly SJ, Daniel M, Dal Grande E. et al. Mental ill-health across the continuum of body mass index. BMC Publ Health. 2011;11:765. doi: 10.1186/1471-2458-11-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J, Koehn S, Happell B, Dwyer T, Moxham L. Implications of excess weight on mental wellbeing. Aust Health Rev. 2010;34(3):368–374. doi: 10.1071/AH09708. [DOI] [PubMed] [Google Scholar]
- Perez M, Warren CS. The relationship between quality of life, binge-eating disorder, and obesity status in an ethnically diverse sample. Obesity. 2012;20:879–885. doi: 10.1038/oby.2011.89. [DOI] [PubMed] [Google Scholar]
- Renzaho A, Wooden M, Houng B. Associations between body mass index and health-related quality of life among Australian adults. Qual Life Res. 2010;19(4):515–520. doi: 10.1007/s11136-010-9610-z. [DOI] [PubMed] [Google Scholar]
- Takahashi Y, Sakai M, Tokuda Y. et al. The relation between self-reported body weight and health-related quality of life: a cross-sectional study in Japan. J Public Health. 2011;33(4):518–526. doi: 10.1093/pubmed/fdr042. [DOI] [PubMed] [Google Scholar]
- Stafford M, Newbold BK, Ross NA. Psychological distress among immigrants and visible minorities in Canada: a contextual analysis. Int J Soc Psychiatry. 2011;57(4):428–441. doi: 10.1177/0020764010365407. [DOI] [PubMed] [Google Scholar]
- Wheaton B. The twain meets: distress, disorder and the continuing conundrum of categories (comment on Horwitz) Health. 2007;11:303–319. doi: 10.1177/1363459307077545. [DOI] [PubMed] [Google Scholar]
- Marcus MD, Wildes JE. Obesity: is it a mental disorder? Int J Eat Disord. 2009;42(8):739–753. doi: 10.1002/eat.20725. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Kotwal R, Malhotra S, Nelson EB, Keck PE, Nemeroff CB. Are mood disorders and obesity related? A review for the mental health professional. J Clin Psychiatry. 2004;65(5):634–651. doi: 10.4088/JCP.v65n0507. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, Sarwer DB, Fabricatore AN, Crerand CE, Lipschutz PE, Faulconbridge L, Raper SE, Williams NN. Comparison of psychosocial status in treatment-seeking women with class III vs. Class I–II obesity. Obesity. 2006;14:90–98. doi: 10.1038/oby.2006.288. [DOI] [PubMed] [Google Scholar]
- Atlantis E, Ball K. Associations between weight perception and psychological distress. Int J Obes. 2008;32(4):315–323. doi: 10.1038/sj.ijo.0803762. [DOI] [PubMed] [Google Scholar]
- Huang IC, Frangakis C, Wu AW. The relationship of excess body weight and health-related quality of life: evidence from a population study in Taiwan. Int J Obes. 2006;30:1250–1259. doi: 10.1038/sj.ijo.0803250. [DOI] [PubMed] [Google Scholar]
- Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J. 2011;10:9. doi: 10.1186/1475-2891-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos P, Saguy A, Ernsberger P, Oliver E, Gaesser G. The epidemiology of overweight and obesity: public health crisis or moral panic? Int J Epidemiol. 2005;35:55–60. doi: 10.1093/ije/dyi254. [DOI] [PubMed] [Google Scholar]
- Lund RS, Karlsen TI, Hofso D. et al. Employment is associated with the health-related quality of life of morbidly obese persons. Obes Surg. 2011;21(11):1704–1709. doi: 10.1007/s11695-010-0289-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loff B, Crammond BR. Wanted: politicians to champion health (not obesity) Med J Aust. 2010;192(7):397–399. doi: 10.5694/j.1326-5377.2010.tb03563.x. [DOI] [PubMed] [Google Scholar]
- Dixon JB. The effect of obesity on health outcomes. Mol Cell Endocrinol. 2010;316:104–108. doi: 10.1016/j.mce.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Doll HA, Petersen SEK, Stewart-Brown SL. Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res. 2000;8:160–170. doi: 10.1038/oby.2000.17. [DOI] [PubMed] [Google Scholar]
- Chang HH, Yen ST. Association between obesity and depression: evidence from a longitudinal sample of the elderly in Taiwan. Aging Ment Health. 2012;16(2):173–180. doi: 10.1080/13607863.2011.605053. [DOI] [PubMed] [Google Scholar]
- Dey DK, Rothenberg E, Sundh V, Bosaeus I, Steen B. Body mass index, weight change and mortality in the elderly. A 15 y longitudinal population study of 70 y olds. Eur J Clin Nutr. 2001;55(6):482–492. doi: 10.1038/sj.ejcn.1601208. [DOI] [PubMed] [Google Scholar]
- Carroll DD, Blanck HM, Serdula MK, Brown DR. Obesity, physical activity, and depressive symptoms in a cohort of adults aged 51–61. J Aging Health. 2010;22(3):384–398. doi: 10.1177/0898264309359421. [DOI] [PubMed] [Google Scholar]
- Larsson U, Karlsson J, Sullivan M. Impact of overweight and obesity on health related quality of life – a Swedish populations study. Int J Obes. 2002;26:417–424. doi: 10.1038/sj.ijo.0801919. [DOI] [PubMed] [Google Scholar]
- Hopman WM, Berger C, Joseph L, Barr SI, Gao Y, Prior JC, Poliquin S, Towheed T, Anastassiades T. CaMos Research Group. The association between body mass index and health-related quality of life: data from CaMos, a stratified population study. Qual Life Res. 2007;16(10):1595–1603. doi: 10.1007/s11136-007-9273-6. [DOI] [PubMed] [Google Scholar]
- Vasiljevic N, Ralevic S, Marinkovic J, Kovec N, Maksimovic M, Milosevic GS, Tomic J. The assessment of health-related quality of life in relation to the body mass index value in the urban population of Belgrade. Health Qual Life Outcomes. 2008;6:106. doi: 10.1186/1477-7525-6-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DP. The detection of psychiatric illness by questionnaire. Oxford: Oxford University Press; 1972. [Google Scholar]
- Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O. et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27(1):191–197. doi: 10.1017/S0033291796004242. [DOI] [PubMed] [Google Scholar]
- Puustinen PJ, Koponen H, Kautiainen H, Mäntyselkä P, Vanhala M. Psychological distress measured by the GHQ-12 and mortality: a prospective population-based study. Scand J Public Health. 2011;39:577. doi: 10.1177/1403494811414244. [DOI] [PubMed] [Google Scholar]
- Minniti A, Bissoli L, Di Francesco V. et al. Comparison of physical and psychological status in younger and older overweight-obese women. Nutr Metab Cardiovasc Dis. 2011;21(12):909–914. doi: 10.1016/j.numecd.2010.02.025. [DOI] [PubMed] [Google Scholar]
- Lim W, Thomas KS, Bardwell WA, Dimsdale JE. Which measure of obesity Are related to depressive symptoms and in whom? Psychosomatics. 2008;49(1):23–28. doi: 10.1176/appi.psy.49.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannucci E, Petroni ML, Villanova N, Rotella CM, Apolone G, Marchesini G. Clinical and psychological correlates of health-related quality of life in obese patients. Health Qual Life Outcomes. 2010;23(8):90. doi: 10.1186/1477-7525-8-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannucci E, Ricca V, Barciulli E, Di Bernardo M, Travaglini R, Cabras PL, Rotella CM. Quality of life and overweight: the obesity related well-being (Orwell 97) questionnaire. Addict Behav. 1999;24(3):345–357. doi: 10.1016/S0306-4603(98)00055-0. [DOI] [PubMed] [Google Scholar]
- Aphramor L. Validity of claims made in weight management research: a narrative review of dietetic articles. Nutr J. 2010;9:30. doi: 10.1186/1475-2891-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacon L. Health at Every Size: The Surprising Truth about Your Weight. 2. Dallas: BenBella Books; 2010. [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Knoesen NP, Mancuso SG, Thomas S. et al. Relationship between severity of obesity and mental health: an Australian community survey. Asia Pac Psychiatr. 2012;4(1):67–75. doi: 10.1111/j.1758-5872.2011.00164.x. [DOI] [Google Scholar]
- Smith AB, Fallowfield LJ, Stark DP, Velikova G, Jenkins V. A rasch and confirmatory factor analysis of the general health questionnaire (GHQ) – 12. Health Qual Life Outcomes. 2010;8:45. doi: 10.1186/1477-7525-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Jaffe KJ, Friedman MA. Perceived interpersonal mistreatment among obese Americans: Do race, class, and gender matter? Obesity. 2008;16:60–68. doi: 10.1038/oby.2008.453. [DOI] [PMC free article] [PubMed] [Google Scholar]