Abstract
Background
The study was conducted to examine the hypotheses that adolescent and young adult women who perceived they are susceptible to pregnancy when birth control is not used are less likely to practice unsafe sex, discontinue oral contraception (OC), and become pregnant during a 12-month follow-up period.
Study design
We conducted secondary analyses using data collected for a randomized, controlled trial on OC adherence among 1,155 low-income women 16–24 years of age. Demographics, lifestyle variables, perceived susceptibility to pregnancy assessed at baseline and data on OC and condom use, and pregnancy status collected during 12 months of follow-up were used for the analyses.
Results
Overall, 62.3% of women accurately understood the risks of pregnancy without using any birth control method. However, perceived susceptibility was not associated with OC continuation (odds ratio (OR) 0.94, 95% confidence intervals (CI) 0.79–1.11), condom use at last sexual intercourse (OR 1.02, 95% CI 0.84–1.24), dual method use (OR 1.17, 95% CI 0.92–1.48) and subsequent pregnancy (hazards ratio 1.08, 95% CI 0.77–1.49) during the 12-month follow-up period.
Conclusions
Perceived susceptibility to pregnancy, an important component of the health belief model, does not seem to have any impact on use of birth control methods, safer sex or rate of subsequent pregnancy among low-income adolescent and young adult women.
Keywords: Perceived susceptibility to pregnancy, contraceptive adherence, safer sex, young adult women
1. Introduction
Unintended pregnancy is one of the most important adverse reproductive health outcomes for adolescent and young adult women. Nearly half of the 6.7 million pregnancies reported in the US each year are unintended; this rate is even higher among 15-of to 24-year-old women (69%) [1]. The recent unintended pregnancy rate in the US showed a slight upward trend [1], although the rate had shown a downward trend or remained static in the past several decades [2, 3]. Moreover, a 50% increase was reported among women with an income below the federal poverty line compared to a 29% decrease among women with incomes ≥200% of the poverty line [1], demonstrating that this problem is particularly severe among low-income women.
Decision-making on a preventive behavior is a complex phenomenon. The health belief model (HBM), a psychosocial model formulated in 1950s [4], is widely regarded as a tool to predict health-related preventive behavior. The very first assumption of this model is that a person will adopt a health-related behavior when he or she adequately perceives susceptibility to a serious negative consequence for not adopting the behavior. Thus, according to the HBM, appropriate perception of susceptibility to pregnancy (risks of pregnancy) without using any birth control method is the key determinant for contraceptive behavior and adherence. The objective of this study was to examine whether adolescent and young adult women who understand the risk of pregnancy are less likely to discontinue contraceptive use, practice unsafe sex and have subsequent pregnancy.
2. Methods
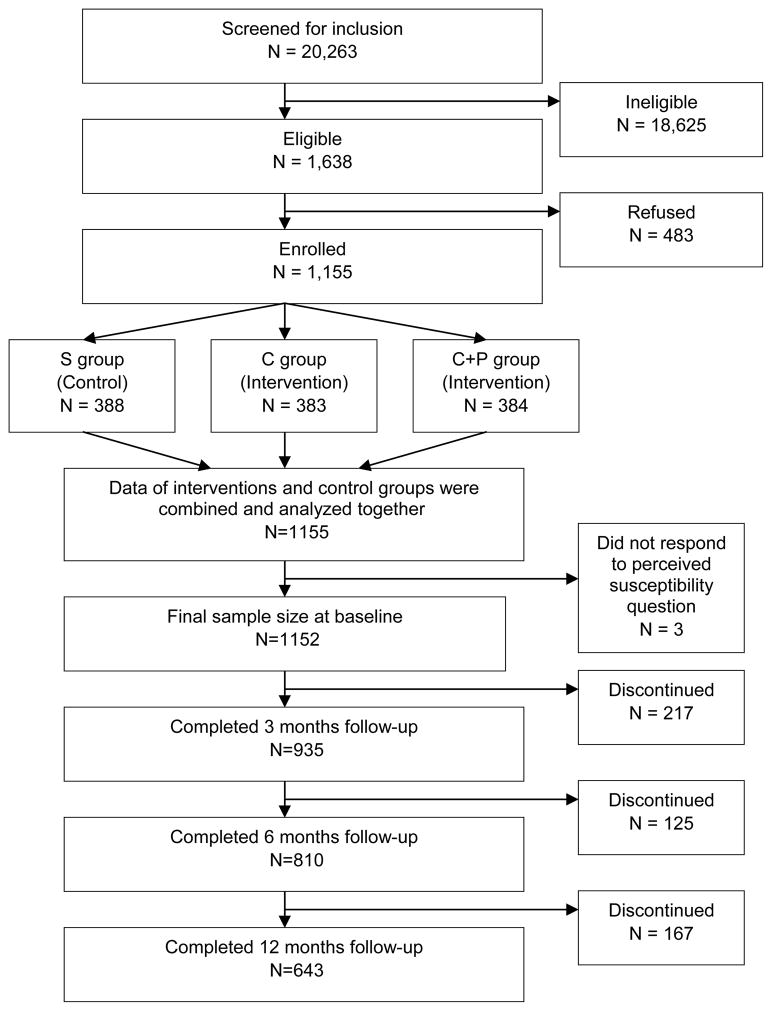
As a part of the larger study, 1155 sexually active and non-pregnant females 16 to 24 years old who requested to initiate oral contraception (OC) between July 2006 and January 2010 were invited to participate. Subjects were recruited at 5 different publicly funded reproductive health clinics. These clinics serve low-income women, of whom 80% have an annual income below US $ 30,000/yr. The methods for the larger study which was approved by the University of Texas Medical Branch Institutional Review Board prior to its initiation are reported in detail elsewhere [5]. Briefly, a total of 20,263 women were approached to determine if they were eligible for this study, of which 1,638 women were eligible (Fig. 1). The most common reasons for ineligibility were that they did not want to use OC (57.2%), were already using OC (9.3%), had previously used OC for >1 month (22.7%) or planned to become pregnant within 12 months (3.2%). Of those eligible, 483 (30%) declined to participate, usually due to time constraints that day. Thus, 1155 women met all inclusion/exclusion criteria and agreed to be enrolled in the study and were randomized to receive either face-to-face behavioral counseling and education at their baseline clinic visit (C group; n=383) or this same intervention followed by monthly phone calls for 6 months (C+P group; n=384) or standard care (S group; n=388). No differences were observed between those who refused and those who enrolled with regard to desire for a pregnancy within the next year (p= .26) or having ever had sex (p = .09). However, Hispanic women were significantly less likely to agree to participate than white and African-American women (65% of Hispanic women vs. 80% of white and African-American women; p<.001).
Fig. 1.
Flow chart of study population.
At the initial visit, patients were asked to report their demographics, sexual behaviors and contraceptive use. Understanding the risk of pregnancy was assessed at baseline using a five-point scale with the statement: “Most young couples who do not use birth control will end up pregnant”. The response options included the following: “strongly disagree,” “disagree,” “neither agree nor disagree,” “agree,” and “strongly agree”. “Agree” and “strongly agree” were combined to identify women who perceived the risks accurately. Women with the other three responses were considered as “did not perceive the risks” group. Pregnancy ambivalence was also assessed using a question: “If you found out that you are pregnant today, how would you feel about it?” Response options were: very happy, somewhat happy, neither happy nor unhappy, somewhat unhappy and very unhappy. Those who responded “neither happy nor unhappy” were considered as “ambivalent” while the rest of the respondents together were considered as “not ambivalent”.
Pregnancies were assessed by self-report and medical record review after 3, 6, and 12 months. During the phone assessments, each subject was asked whether she had become pregnant. At the conclusion of the study, the entire UTMB medical record of each subject since beginning the study was reviewed to detect any additional unreported pregnancies over the 12-month interval. Correct use of OCs was defined as starting each pack on time and not missing any doses or correctly making up any pills missed. Those who used OC correctly and condoms consistently were considered dual users.
2.1. Statistical analysis
Univariable comparisons were performed using the chi-square test or Student’s t test, as appropriate. We examined the effect modification of different interventions on the relationship between susceptibility to pregnancy and different outcomes of interest. Since there was no effect modification (p>.20), we combined both interventions and control groups together and adjusted the effects of interventions in all multivariate models. Multivariable logistic regression models for outcomes measured at baseline and generalized estimating equations (GEE) models [6] for outcomes measured during 12 months follow-up were used to examine the association between perceived susceptibility to pregnancy and sexual behaviors, condom use, dual use of condom and OC, and OC continuation during 12 months follow-up after adjusting for covariates and effects of interventions. In addition, Cox proportional hazards models was used to examine its association with incidence of pregnancy during 12 months follow-up. Sociodemographic variables were screened for inclusion in a multivariable model. Any variables that were unevenly distributed by perceived susceptibility to pregnancy status were controlled for in the multivariable statistical procedures. All analyses were performed using STATA 11 (Stata Corporation, College Station, TX).
3. Results
Among the 1155 participants, 644 (55.8%) were between 16 and 19 years of age and 511 (44.2%) were 20–24 years old. Distribution among racial/ethnic groups was representative of the clinics’ patient bases: 54.2% were Hispanic (N=626); 18.6% were black (N=215); 24.8% were white (N=287); and 2.3% were other (N=27). Most women were single/never married (78%), and about a quarter worked >20 h per week.
Of the 1155 women, 1152 answered the question related to perception of pregnancy without using birth control method. Among them, 62.3% (718/1152) understood the risk of pregnancy when birth control is not used. Bivariate analyses of baseline characteristics revealed that adolescents who understood the risks of pregnancy were more likely to be older, married and unemployed, and less likely to be ambivalent about pregnancy (Table 1). However, these two groups did not differ by race/ethnicity, past sexual behavior (except condom use), OC continuation, condom use, and dual method of use based on 12 months of follow-up. Overall, 163 women became pregnant during 12 months of follow-up. However, incidence of pregnancy did not differ between these two groups (13.8% vs. 14.4%; p=.81) (Table 1).
Table 1.
Characteristics of participants by perceived susceptibility to pregnancy status
| Characteristics | Perceived susceptibility to pregnancy (n=1152)
|
p value | |
|---|---|---|---|
| No (n=434) | Yes (n=718) | ||
| Demographic characteristics | |||
| Age,years, n (%) | <.01 | ||
| 16–19 | 266 (61.3) | 377 (52.5) | |
| 20–24 | 168 (38.7) | 341 (47.5) | |
| Race, n (%) | .18 | ||
| White | 115 (26.5) | 172 (24.0) | |
| Black | 88 (20.3) | 127 (17.7) | |
| Hispanic | 218 (50.2) | 405 (56.4) | |
| Other* | 13 (3.0) | 14 (2.0) | |
| Marital status, n (%) | .02 | ||
| Never married | 357 (82.5) | 549 (76.7) | |
| Married, divorced, or separated | 76 (17.6) | 167 (23.3) | |
| Education, n (%) | .08 | ||
| Did not complete HS or get GED | 224 (52.1) | 333 (46.8) | |
| At least HS graduate | 206 (47.9) | 379 (53.2) | |
| Employment status, n (%) | .04 | ||
| Does not work | 248 (57.4) | 457 (63.7) | |
| Employed (full/part time) | 183 (42.5) | 260 (36.3) | |
| No. of prior pregnancies, mean (±SD)† | 1.5 (0.7) | 1.5 (0.8) | .46 |
| Pregnancy ambivalence, n (%) | 130 (30.5) | 147 (20.6) | <.001 |
| Sexual behaviors and use of birth control methods in the past | |||
| Sexual partners in the last year, n (%) | .09 | ||
| 0–2 | 358 (83.8) | 627 (87.5) | |
| ≥3 | 69 (16.2) | 90 (12.6) | |
| Sexual partners lifetime, n (%) | .07 | ||
| 0–2 | 193 (45.6) | 363 (51.3) | |
| ≥3 | 230 (54.4) | 345 (48.7) | |
| Age at first sexual intercourse, n (%) | .17 | ||
| ≤15 | 236 (56.9) | 424 (61.1) | |
| ≥16 | 179 (43.1) | 270 (38.9) | |
| Used condom at last sexual intercourse, n (%) | 205 (51.9) | 294 (44.0) | .01 |
| Did not use any birth control methods at last sexual intercourse, n (%) | 178 (41.1) | 318 (44.3) | .29 |
| Did not use any birth control methods in the past, n (%) | 64 (14.9) | 116 (16.2) | .55 |
| Outcome during 12 months of follow-up after recruiting for OC use | |||
| Correct use of pill pack, mean (±SD) | 5.7 (4.2) | 5.3 (3.9) | .12 |
| Incidence of pregnancy, n (%) | 60 (13.8) | 103 (14.4) | .81 |
| OC continuation, n (%)⧺ | |||
| 3 mo | 240 (68.6) | 387 (66.2) | .45 |
| 6 mo | 155 (51.3) | 262 (51.6) | .95 |
| 12 mo | 90 (37.0) | 132 (33.0) | .30 |
| Dual use of OC and condoms, n (%)⧺ | |||
| 3 mo | 67 (19.1) | 129 (22.1) | .29 |
| 6 mo | 69 (22.9) | 115 (22.6) | .95 |
| 12 mo | 55 (22.6) | 106 (26.5) | .27 |
| Partner used condom at last sex, n (%)⧺ | |||
| 3 mo | 140 (53.6) | 251 (53.6) | .99 |
| 6 mo | 123 (45.9) | 229 (49.5) | .35 |
| 12 mo | 102 (42.0) | 180 (55.1) | .44 |
| Did not use any contraception, n (%)⧺ | |||
| 3 mo | 42 (12.0) | 56 (9.6) | .24 |
| 6 mo | 71 (23.5) | 94 (18.5) | .09 |
| 12 mo | 73 (30.0) | 124 (31.0) | .80 |
SD: Standard deviation.
Asians/American Indians/Alaskan/Native Hawaiian.
Based on women who had at least one pregnancy.
Based number of observation available at 3, 6 and 12 months follow-up.
Sociodemographic variables that met the screening criteria for inclusion in the multivariable model were age, marital and employment status. Effects of interventions were adjusted in all multivariate models. Multivariable analyses showed that women who understood the risks of pregnancy without contraceptive use did not have higher odds of engaging in safer sex, using OC, condoms, or both OC and condoms compared to those who did not perceive susceptibility to becoming pregnant after adjusting for covariates and effects of interventions (Table 2). For example, using 12 months follow-up data, women who understood the risks of pregnancy were 17% more likely (OR=1.17) to have used dual method (both condom and OC); but, this result was not statistically significant. However, they were less likely to be ambivalent about pregnancy based on both cross sectional ambivalence data collected at baseline and longitudinal data collected during 12 months of follow-up. Understanding the risks of pregnancy was not associated with incidence of pregnancy.
Table 2.
Association of perceived susceptibility to pregnancy with unsafe sex, OC adherence, dual method use, and incidence of pregnancy during 12 months of follow-up
| Dependent variables | OR (95% CI)* |
|---|---|
| Data collected at baseline | |
| Used condom at last sexual intercourse⧺ | 0.81 (0.63–1.06) |
| Did not use any birth control methods at last sexual intercourse⧺ | 1.04 (0.81–1.33) |
| Did not use any birth control methods in the past⧺ | 1.07 (0.76–1.52) |
| Pregnancy ambivalence⧺ | 0.57 (0.43–0.75) |
| Data collected during 12 months of follow-up | |
| OC continuation¶ | 0.94 (0.79–1.11) |
| Used condom at last sexual intercourse¶ | 1.02 (0.84–1.24) |
| Did not use any birth control methods¶ | 0.89 (0.69–1.14) |
| Dual use of birth control method¶ | 1.17 (0.92–1.48) |
| Pregnancy ambivalence¶ | 0.65 (0.53–0.79) |
| Incidence of pregnancy during 12 months of follow-up† | 1.08 (0.77–1.49) |
ORs (95% CI) were based on multivariable logistic regression analysis or generalized estimating equation models
Separate models were built based on each of the dependent variables.
Adjusted by age, race/ethnicity, education, martial status, working status and intervention methods
Exposure variable was whether the participants had perceived susceptibility to pregnancy (yes vs. no)
Based on logistic regression models.
Based on generalized estimating equation models.
Based on Cox proportional hazard model and should be read as hazard ratio instead of odds ratio.
4. Discussion
This report adds to the literature that accurate perception of the consequences of not using any contraceptive method does not necessarily increase the odds of continuing OC use, dual method use, or condom use among adolescent and young adult women. Thus, the findings suggest that the first component of the HBM does not work for adolescent and young adult women with regard to pregnancy prevention behavior, implying that other components of the HBM may not work in this population.
Our observation that understanding the risks of pregnancy does not change contraceptive behavior is a departure from the popular belief that perceived susceptibility is positively associated with preventive health behaviors. For example, in a meta-analysis based on 42 studies, Katapodi et al. [7] observed that perceived susceptibility to breast cancer is associated with mammography screening behaviors. The underlying theory behind this discrepancy could be due to the fact that certain situations practiced regularly have less influence on a health behavior [8]. As using birth control method is a regular phenomenon, our findings support this theory.
Our findings indicate that the majority of adolescent and young adult women understand their risks of pregnancy, but do not practice accordingly. This may be because OC users must remember to take their medication every day. This daily use of OC or using condoms during each act of sexual intercourse could be an enormous undertaking and difficult for most young women to maintain. This is consistent with the observations of prior studies that almost half of adolescent women discontinue OC use within 6 months of obtaining a prescription [9, 10]. Further, 33% of 13- to 19-year-old and 18% of 20- to 22-year-old women reported that they did not use any contraception for at least one month after stopping their birth control pills, even though they did not want to become pregnant [11]. Together, these studies suggest that OCs may not be the best method for adolescent women to prevent unintended pregnancies. One recent study also reported that lower contraceptive knowledge score, underestimation of OC effectiveness and negative attitude towards condom use were associated with higher risk of unintended pregnancy [12]. One notable finding of this study was that women who understood the risks of pregnancy were less likely to be ambivalent about it. However, it did not have any impact on their contraceptive behaviors as we reported in this study. Thus, when counseling these young women, information about longer acting methods (intrauterine device or subdermal contraceptive implants) and effectiveness of each contraceptive method along with their pros and cons should be disseminated.
This study has several strengths. We recruited a large number of adolescent and young adult women and followed them for an extended period of time. Moreover, the medical records of each subject were reviewed to detect any additional unreported pregnancies during the follow-up period. Several study limitations should also be noted. We did not ask participants whether the pregnancy they reported was unintended. However, pregnancies that occurred during the 12 month follow-up were most likely unintended as we excluded women at baseline who desired to become pregnant in the next year. Moreover, we limited our study to 16- to 24-year-old OC users, so we do not know whether similar findings would be observed in older reproductive-age women or other contraceptive method users.
In conclusion, acknowledging risk of pregnancy does not translate into safer sexual behaviors among adolescent and young adult women. Thus, these women are at increased risk for unintended pregnancy, and require additional counseling on how to decrease these high risk behaviors and long-acting contraceptive use.
Acknowledgments
This study was supported by an award from the Maternal and Child Health Bureau, Health Resources and Services Administration (R40MC06634, Berenson) and a midcareer investigator award in patient-oriented research (K24HD043659, Berenson), from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the MCHB, HRSA, NICHD, or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect. 1998;30:24–9. 46. [PubMed] [Google Scholar]
- 3.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 4.Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2:328–35. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 5.Berenson AB, Rahman M. Effect of counseling and phone calls on oral contraceptives and condom adherence: A randomized controlled trial. Contraception. 2012 doi: 10.1016/j.contraception.2012.06.007. July 25 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 7.Katapodi M, Lee K, Facione N, Dodd M. Predictors of breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analysis. Prev Med. 2004;38:388– 402. doi: 10.1016/j.ypmed.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Miller S. Applying cognitive-social theory to health protective behavior: breast self-examination in cancer screening. Psychol Bull. 1996;119:70–94. doi: 10.1037/0033-2909.119.1.70. [DOI] [PubMed] [Google Scholar]
- 9.Berenson AB, Wiemann CM. Contraceptive use among adolescent mothers at 6 months postpartum. Obstet Gynecol. 1997;89:999–1005. doi: 10.1016/s0029-7844(97)00123-3. [DOI] [PubMed] [Google Scholar]
- 10.Wiemann CM, Berenson AB. An investigation into why adolescents may reject Norplant. Pediatrics. 1996;97:185–91. [PubMed] [Google Scholar]
- 11.Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179:577–82. doi: 10.1016/s0002-9378(98)70047-x. [DOI] [PubMed] [Google Scholar]
- 12.Frost JJ, Lindberg LD, Finer LB. Young adults’ contraceptive knowledge, norms and attitudes: associations with risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:107–16. doi: 10.1363/4410712. [DOI] [PubMed] [Google Scholar]