Abstract
Objective
Lower subjective socioeconomic status (SSS) consistently shows associations with poorer health with the strongest relationships emerging with global self-rated health. Though often interpreted as reflecting the impact of low SSS on health, the association could also arise from confounding SSS with negative affect. In this research we sought to determine if negative affect confounds, or alternatively, is on the causal pathway linking SSS to self-rated health.
Methods
300 adult participants—recruited from throughout the United States—were randomized to experience sadness, shame, or a neutral mood induction wherein they wrote about and visualized a particularly emotionally evocative event. Participants subsequently completed measures of SSS, self-rated health, depression, and negative mood.
Results
Consistent with predictions, neither SSS scores nor the association of SSS with self-rated health, depression, and chronic negative affect differed by mood induction condition, controlling for demographic factors that covary with SSS (e.g., age, gender, education, income). Moreover, chronic negative affect partially explained the relationship between SSS and self-rated health, independent of manipulated mood.
Conclusions
These findings support the utility of the measurement of SSS, and provide evidence suggesting that chronic negative affect is a likely mediator of the SSS association with global health rather than a confounder.
Keywords: socioeconomic status, subjective status, negative affect, self-rated health
Subjective socioeconomic status (SSS) is defined as a person’s subjective perceptions of their rank, relative to others, in the socioeconomic hierarchy (Adler, Epel, Castellazo, & Ickovics, 2000; Kraus, Piff, & Keltner, 2009; 2011; Singh-Manoux, Adler, & Marmot, 2003). Despite the fact that different aspects of socioeconomic status (SES) (e.g., income, education, and occupation) are only moderately intercorrelated, individuals appear able to report reliably on their overall standing—that is, several studies suggest that SSS is consistently moderately correlated with objective measures of income, education, and occupation status (e.g., Adler et al., 2000; Singh-Manoux et al., 2003). Moreover, these subjective rank perceptions of SES are related to health status across a number of diverse measures and samples, and using both longitudinal and cross-sectional research designs (Adler et al., 2000; Cohen et al., 2008; Goodman et al., 2001; Singh-Manoux et al., 2003). In a number of studies, many associations of SSS and health hold even when adjusted for objective indicators of SES, such as education and income (e.g., Adler et al., 2000; Cohen et al., 2008).
Although SSS is related to a range of health indicators, the strongest and most consistent association is with global self-reported health (Adler et al., 2000; Operario, Adler, & Williams, 2004). Given that social status is linked to many different conditions, it makes sense that a general measure of status such as SSS would correlate more strongly with a measure of general health than with the occurrence of any specific disease. However, since global health is self-reported, its association with SSS could be confounded by psychological third variables that correlate with both constructs. The present study tests whether the association of SSS with self-reported health is independent of a plausible class of confounding variables: negative mood.
SSS, Negative Mood, and Self-Rated Health
Research showing strong relationships between increased economic inequality and elevated mortality rates among the disadvantaged points to the contribution of rank to health inequality (e.g., Kawachi & Kennedy, 1997). To the extent that relative rank is important in this relationship, subjective perceptions of SES are likely to be powerful predictors of health and well-being. Research bears out this expectation. For instance, even after accounting for effects due to objective indicators of SES (e.g., education, income), SSS uniquely predicts self-rated global health (Adler et al., 2000; Franzini & Fernandez-Esquer, 2006; Hyde & Jones, 2007; Ostrove, Adler, Kupperman, & Washington, 2000), and negative affect (Adler et al., 2000; Ghaed & Gallo, 2006; Gianaros et al., 2007; Operario et al., 2004). Lower SSS individuals report poorer self-rated health and more negative affect relative to their upper SSS counterparts, and the association of SSS and self-rated health remains significant when adjusted for negative affect. Further evidence emerges from studies of health outcomes that are not subject to self-report biases. Such studies have shown, for example, that independent of objective SES indicators, lower SSS individuals show more physiological risk factors (Adler et al, 2000; Wright & Steptoe, 2005), greater susceptibility to a common cold virus (Cohen et al., 2008), and, at an ecological level, greater mortality (Kopp, Skrabski, Réthelyi, Kawachi, & Adler, 2004) relative to their upper SSS counterparts.
Despite the robust independent predictive power of SSS, it is unclear the extent to which this measure is free of psychological biases. Negative mood states correlate highly with both self-rated health (Adler et al., 2000) and with perceptions of rank (Keltner, Gruenfeld, & Anderson, 2003) and could confound the relationship between SSS and self-rated global health. That is, because the relationships between SSS, negative affect, and self-rated health are correlational, one cannot rule out the possibility that negative affect could be an underlying variable that is responsible for a spurious association between SSS and self-rated health.
The above analysis focuses on concurrent mood states. In contrast, chronic negative affective states may plausibly mediate the relationship between SSS and self-rated health, as they do in relation to objective SES and health: Individuals lower in objective indicators of SES are more likely to experience chronic negative emotion, and this association explains some of the effect of SES on health outcomes (e.g., Cohen, Kaplan, & Salonen, 1999; Fiscella & Franks, 1997; Gallo & Matthews, 2003; Matthews, Räikkönen, Gallo, & Kuller, 2008).
Preliminary findings comparing the relative impact of chronic negative affect on the association of objective versus subjective SES and self-rated health provide some evidence that chronic negative affect is on the causal pathway linking lower SSS to poorer global self-rated health. While some have questioned whether mood states affect subjective ratings of relative status, no one has suggested that mood influences reports of educational attainment and income; there is little reason to believe that recall and report of one’s highest degree or annual income would be affected by a temporary mood. Thus, if one finds a similar reduction in the association of subjective SES with self-rated health as with objective SES when adjusted for negative affect, this would suggest that there is not a sustained spurious effect of negative affect on the link between SSS and health. Consistent with the assertion that SSS is robust to mood fluctuations, Operario and colleagues (2004) found that self-reports of chronic negative affect explained similar proportions of the association between self-rated global health and measures of both SSS and objective SES (i.e., income and educational attainment). These findings suggest that chronic negative affect is likely to be on the causal pathway between SSS and self-rated health.
Despite these supportive findings, evidence that the relationship of SSS and self-rated health is not spurious would be more compelling if transient negative mood states—experienced when rating one’s SSS and one’s health—could be definitively disentangled from other characteristics which might be linked to both chronic negative affect as well as SSS. This can be accomplished through random assignment of individuals to experimental conditions in which they experience either a negative or neutral affective state when completing ratings of SSS and of self-rated health. In the present research, we test the hypothesis that SSS effects on self-rated health will be independent of experimentally induced transient negative mood states, but that chronic negative affect will partially explain the association. These proposed results would provide the first experimental evidence that SSS effects on self-rated health are not confounded by temporary mood, and that chronic negative affect serves as a potential explanatory variable linking SSS to global health.
Negative affect encompasses different affective states that vary both in terms of situational determinants and physiological responses. For example, experiences of loss are likely to engender sadness or anger, while experiences of interpersonal failure or disrespect are more likely to engender feelings of shame (Gruenwald, Kemeny, Aziz, & Fahey, 2004; MacDonald & Leary, 2005; Williams, 2007). While low SES may expose people to situations that increase the likelihood of experiencing all these emotions, feelings of shame may be more specifically linked to lower perceived rank (Keltner et al., 2003; Wilkinson, 1999) and are also associated with activation of the HPA axis and negative health outcomes (e.g., Gruenwald et al., 2004). Thus, of all the types of negative mood states, shame is among the most likely mood confound of the relationship between SSS and self-rated health.
The Present Research
The present research tested the hypotheses that SSS ratings themselves, as well as their associations with self-rated global health are independent of temporary changes in negative mood states. To that end, we recruited participants through an online website and manipulated their mood using standard procedures (Westermann, Spies, Stahl, & Hesse, 1996). Specifically, we induced participants to experience sadness, shame, or a neutral mood and subsequently assessed their current mood state, self-ratings of health, general negative affect, depression, along with measures of SSS. We expected that (1) SSS ratings would not be affected by induced negative mood, (2) the relationship of SSS to global health would be independent of induced negative mood, and demographic factors that covary with SSS or health outcomes (e.g., objective SES, age, ethnic background, gender), and (3) chronic negative mood would, in part, explain the SSS association with global self-rated health.
Method
Participants
Participants were 300 adults recruited through a website maintained by a private retail company that recruits individuals interested in participating in online studies in exchange for monetary compensation. Participants were recruited through Mechanical Turk (www.mturk.com), a widely used participant recruitment website for social and behavioral research that allows researchers to advertise studies online that can be accessed by participants via home or office computer terminals. Research indicates that participants recruited through Mechanical Turk are more representative of the overall population than typical internet recruitment samples and college student samples (Buhrmester, Kwang, & Gosling, 2011). The study received institutional review board approval and informed consent was obtained from each subject.
The majority of participants self-identified as European American (n = 227), followed by Asian American (n = 22), multiple ethnic categories (n = 20), African American (n = 18), and Latino (n = 14). The majority of participants (56.3%) were female (n = 169), and the mean age was 34 years (M = 33.84, SD = 11.59, range 18–72). Participants represented diverse SES backgrounds: 41.0% had high school as their highest education completed, and the median income of the sample was between $25,001 and $35,000 annually.
Mood Manipulation Procedure
After reading instructions, participants were randomly assigned to one of three mood states. Following procedures adapted from a meta-analysis of the effectiveness of negative mood induction, we manipulated mood by asking participants to recall a particular event that made them feel generally sad, feel shame, or to recall an emotionally neutral event (Westermann et al., 1996). Specifically, participants were instructed to “remember a specific event in your life that made you feel sad, down, or depressed” (sadness mood condition), “shamed, disrespected, or devalued” (shame condition), or to “remember a specific event in your life: waking up in the morning,” (neutral condition). Participants were further instructed to “please try to remember the event as if you were actually experiencing it again.” They were further instructed to “visualize how you were feeling at that moment, what happened to you, who was with you, when it happened, what you saw, what you heard, what you were thinking, etc…” Participants were encouraged to visualize with their eyes closed to help them remember the event. Subsequently, they were asked to provide a written description of the event in detail (Westermann et al., 1996).
Measures
State negative mood
Participants completed the Positive and Negative Affect Scale (PANAS) directly following the manipulation. We used the PANAS negative emotion subscale which provides a list of 10 emotions (e.g., guilty, irritable, afraid) to assess the effectiveness of the mood manipulation (Watson, Clark, & Tellegen, 1991). Participants were asked to fill out this measure while thinking about how they were feeling “right at this moment,” using 5-point Likert scales (1 = very slightly or not at all, 5 = extremely). Scores on this scale can range from 1 to 5. The mean in this sample across conditions was 1.67, (SD = 0.73, α = .90).
Chronic negative affect
Directly following measures of SSS, health, and depression, participants also completed the PANAS using the same 4-point scale, but this time rating how strongly they experience each emotion in general (M = 1.72, SD = 0.71; α = .91).
SSS
Using the standard procedure (Adler et al., 2000; Kraus et al., 2009), participants were asked to rate themselves on a 10-rung ladder representing society, with those at the top (bottom) of the ladder being the best (worst) off and having the most (least) education, money, and best (worst) jobs. Higher scores on the 10-rung ladder indicated higher subjective SES (M = 5.35, SD = 1.86).
Self-rated health
Participants filled out the Short Form 12 (SF12), whose 12 items provide a measure of self-rated global health, and subscales for health impairments due to mental and physical problems (Ware, Kosinski, & Keller, 1996). The physical health items assess how much typical behaviors are impacted by one’s health, such as “climbing several flights of stairs” or “pushing a vacuum cleaner.” The mental health items ask the extent, over the past four weeks, that the person “felt calm and peaceful” or “felt downhearted and blue,” for example. We used standard scoring procedures for the physical and mental health impairment subscales (Ware, Kosinski, & Keller, 1994). As an additional overall index of general health, we used the single item global self-rated health measure: “In general, my health is” which uses a 5-point Likert scale (1 = poor, 5 = excellent; M = 2.51, SD = 0.90). This item has been used in previous research examining associations between SSS and self-rated health (Adler et al., 2000; Kopp et al., 2004), and in many epidemiological studies (e.g., Idler & Benyamini, 1997).
Depression
As a second measure of chronic negative affect, participants completed the 20-item Center for Epidemiological Studies Depression Scale (Radloff, 1977) by describing how they felt during the past week (e.g., “I thought my life had been a failure”) using a 4-point scale (1 = rarely or none of the time, 4 = most of the time). Scores on the 20 items were summed (M = 37.21, SD = 11.42; α = .93).
Objective SES
Objective SES was assessed using self-reports of educational attainment and annual income. Education was assessed using four categories (1 = did not finish high school, 2 = high school graduation, 3 = college graduation, 4 = postgraduate degree; M = 2.73, SD = 0.72). Annual income was assessed using eight categories (1 = less than $15,000, 2 = $15,001–$25,000, 3= $25,001–$35,000, 4 = $35,001–$50,000, 5 = $50,001 – $75,000, 6 = $75,001 – $100,000, 7 = $100,001 – $150,000, 8 = greater than $150,000; M = 4.29, SD = 1.90).
Results
Mood Manipulation Effects on Affect and Health
First, we determined if our manipulation of transient negative mood was successful in manipulating mood. We used a one-way Analysis of Variance (ANOVA) with the mood manipulation as our independent variable and the measure of state negative mood from the PANAS as our dependent measure. As expected, we found a significant effect for the mood manipulation F(2,297) = 17.91, p < .001. Using Fisher’s least significant difference test, we found that participants in the negative mood (M = 1.84) and the shame condition (M = 1.86) both experienced significantly greater negative mood following the manipulation than participants in the neutral condition (M = 1.36), p’s < .001. The mood manipulation explained 10.7% of variance in state negative mood, a finding consistent in magnitude with a medium to large effect size (Cohen, 1969). We conducted a similar analysis while controlling for chronic negative affect. This Analysis of Covariance still yielded significant group differences F(2,297) = 14.35, p < .001 such that neutral participants scored lower on our measure of state negative mood (M = 1.45) relative to both the shame condition (M = 1.74) and the sadness condition (M = 1.86).
When we examined mood manipulation differences on our health and affect outcome variables we found significant group differences on the single item global health measure F(2, 297) = 3.64, p < .05 and on chronic negative affect F(2, 297) = 6.16, p < .01. Ratings of mental health showed a marginal difference F(2, 297) = 2.78, p = .06, while no differences among mood manipulation groups were shown on depression F(2, 297) = 2.24, p = .11, or on physical health F(2, 297) = 1.00, p = .37. Shame-induced participants reported poorer global health (Mshame = 2.72, Mneutral = 2.47; p < .05), and more chronic negative affect (Mshame = 1.92, Mneutral = 1.57; p < .05) than their neutral condition counterparts. In contrast, the sadness induction did not induce mean differences in reports on either of these variables.
Mood Effects on SSS
To test whether negative mood induced by the manipulation changed ratings of SSS, we subjected SSS ratings to the same one-way ANOVA. If SSS is subject to mood, we would expect lower SSS scores among participants in the shame and sadness conditions than among those in the neutral control condition. However, mean SSS scores were virtually identical for participants in the sadness (M = 5.36, SD = 1.80), shame (M = 5.37, SD = 1.98), and neutral (M = 5.32, SD = 1.82) conditions F(2,298) = 0.02, p = .98, which suggests that SSS ratings are not affected by fluctuations in temporary negative mood. Though we cannot statistically prove this null hypothesis, the large sample size of our design provides sufficient power to find even a small effect of mood on SSS. Below we further test the hypothesis that SSS influences on self-rated health are free of current mood by examining whether SSS associations with self-rated health persist across mood manipulation conditions.
Mood and SSS Associations with Self-Rated Health
We examined relationships between SSS and our measures of self-rated health, depression, and chronic negative affect (see correlations in Table 1). Consistent with previous research, SSS was significantly associated with all these variables. In contrast, and also in line with previous research (Adler et al., 2000), objective SES measures showed less consistent associations with health outcomes than did SSS: Educational attainment was related only to the single item global health measure, while income was significantly associated with the single item global health measure, mental health impairment, and depression but not with physical health impairment.
Table 1.
Correlations between measures of SSS, income, and educational attainment and measures of self-rated health.
| Chronic Negative Affect |
Depression | Global Health |
Mental Health Impairment |
Physical Health Impairment |
|
|---|---|---|---|---|---|
| SSS | −.21* (−.18*) | −.36* (−.35*) | .42* (.41*) | −.29* (−.31*) | −.17* (−.17*) |
| Income | −.07 (−.05) | −.18* (−.18*) | .18* (.19*) | −.17* (−.17*) | −.02 (−.02) |
| Education | −.03 (−.02) | −.12* (−.13*) | .20* (.21*) | −.10 (−.10) | −.02 (−.03) |
Note: numbers in parentheses indicate partial correlations controlling for mood induction condition
p < .05
p < .10
Having found a significant relationship between SSS and health, we next tested whether that relationship would remain significant after accounting for induced mood. For this analysis, we conducted a linear regression entering the mood manipulation as a predictor. We used contrast coding procedures with one variable that compared the effect of the neutral condition (coded “2/3”) to the two negative mood induction conditions (both coded “− 1/3”), and a second variable that compared the effect of the shame condition (coded “1/2”) to the sadness condition (coded “−1/2”) with the neutral condition coded as “0” (Cohen, Cohen, West, & Aiken, 2003). In this analysis, we entered SSS as a predictor, as well as interactions between mood induction and SSS, along with objective SES measures (income and education), age, gender (coded as “−1” for women and “1” for men), and ethnicity (coded as “−1” for non-European American participants, and “1” for European American participants) to determine if the association of SSS to self-rated health is independent of both mood and demographic characteristics.
Table 2 displays results for the regression analyses predicting chronic negative affect. As Table 2 shows, participants with induced experiences of neutral mood reported significantly lower chronic negative affect and marginally lower depression scores than participants in the sadness or shame mood induction conditions. No differences in chronic negative affect or depression were observed between the shame and sadness conditions. However, despite these mood associations with measures of chronic negative affect and depression, and consistent with our hypothesis, SSS was significantly associated with chronic negative affect and depression scores, even after accounting for our mood manipulation, age, gender, ethnicity, income, and education. In addition to SSS, younger participants reported marginally higher depression scores. No other effects were significant.
Table 2.
Regression analyses predicting chronic negative affect with SSS, manipulated mood and key demographic variables (age, gender, ethnicity, income, and education).
| Chronic Negative Affect | Depression | |
|---|---|---|
| Overall Model F(10, 289) | F = 3.53** | F = 6.10** |
| Age | −.05 | −.11+ |
| Gender | −.07 | −.05 |
| Ethnicity | −.02 | −.05 |
| SSS | −.28** | −.42** |
| Neutral v. negative | −.18** | −.12+ |
| Sad v. shame | .11 | .06 |
| SSS X neutral v. negative | .08 | .03 |
| SSS X sad v. shame | .05 | .00 |
| Income | .04 | .03 |
| Education | .01 | .00 |
Note. Numbers indicate standardized β coefficients.
p < .01,
p < .05,
p < .10
Next we examined regression analyses for the self-rated health measures. As Table 3 shows, the negative mood induction had no effect on self-rated health measures relative to the neutral condition. Participants in the sadness condition experienced marginally better health on the single item global health measure relative to participants in the shame condition. Despite this association, and again consistent with our hypothesis, SSS was still associated with the single item global health measure, mental health impairment, and physical health impairment even after accounting for manipulated mood and demographic characteristics. In addition to SSS, older participants scored lower on mental health impairment and higher on physical health impairment than their younger counterparts. Non-European American participants also scored higher on physical health impairment and reported being less healthy on the single item measure of global health relative to European American participants. No other effects were significant.
Table 3.
Regression analyses predicting self-rated health with SSS, manipulated mood, and key demographic variables (age, gender, ethnicity, income, and education).
| Global Health | Mental Health Impairment |
Physical Health Impairment |
|
|---|---|---|---|
| Overall Model F(10, 289) | F = 6.43** | F = 4.54** | F = 3.11** |
| Age | −.07 | −.19* | .18** |
| Gender | .03 | −.01 | −.09 |
| Ethnicity | .13* | −.01 | −.16* |
| SSS | .41** | −.36** | −.25** |
| Neutral v. negative | .03 | −.10 | −.01 |
| Sad v. shame | −.13* | .08 | −.03 |
| SSS X neutral v. negative | .03 | .01 | .04 |
| SSS X sad v. shame | .04 | .04 | −.06 |
| Income | −.01 | .00 | .03 |
| Education | .09 | .04 | −.03 |
Note. Numbers indicate standardized β coefficients.
p < .01,
p < .05,
p < .10
In a parallel analysis we conducted a similar linear regression where we predicted chronic negative affect and self-rated health with SSS, age, gender, ethnicity, income, and education. We used the PANAS measure of current mood rather than the experimental group to which participants were assigned as a predictor in this analysis to control for reports of current negative mood indexed using a continuous measure of the construct. In the analysis, SSS was still significantly associated with chronic negative affect β = −.19, t(289) = −3.18, p < .01, depression β = −.36, t(289) = −5.75, p < .01, the single item global health measure β = .39, t(289) = −5.83, p < .01, mental health impairment β = −.32, t(289) = −4.67, p < .01, and physical health impairment β = −.24, t(289) = −3.28, p < .01 after accounting for current negative mood. Overall, the results from these analyses suggest that SSS associations to chronic negative affect and self-rated health are robust to temporary fluctuations in negative mood.
Is Chronic Negative Affect on the Causal Pathway Between SSS and Self-Rated Health?
Next, we tested whether chronic negative affect may lie on the causal pathway between SSS and self-rated health. To this end, we conducted parallel mediation analyses (Baron & Kenny, 1986) predicting the single item measure of global health, mental health impairment, and physical health impairment with SSS as our independent variable, chronic negative affect—measured by the CESD and PANAS—as our mediator, while controlling for the PANAS measure of current negative mood, objective SES, age, gender, and ethnicity.
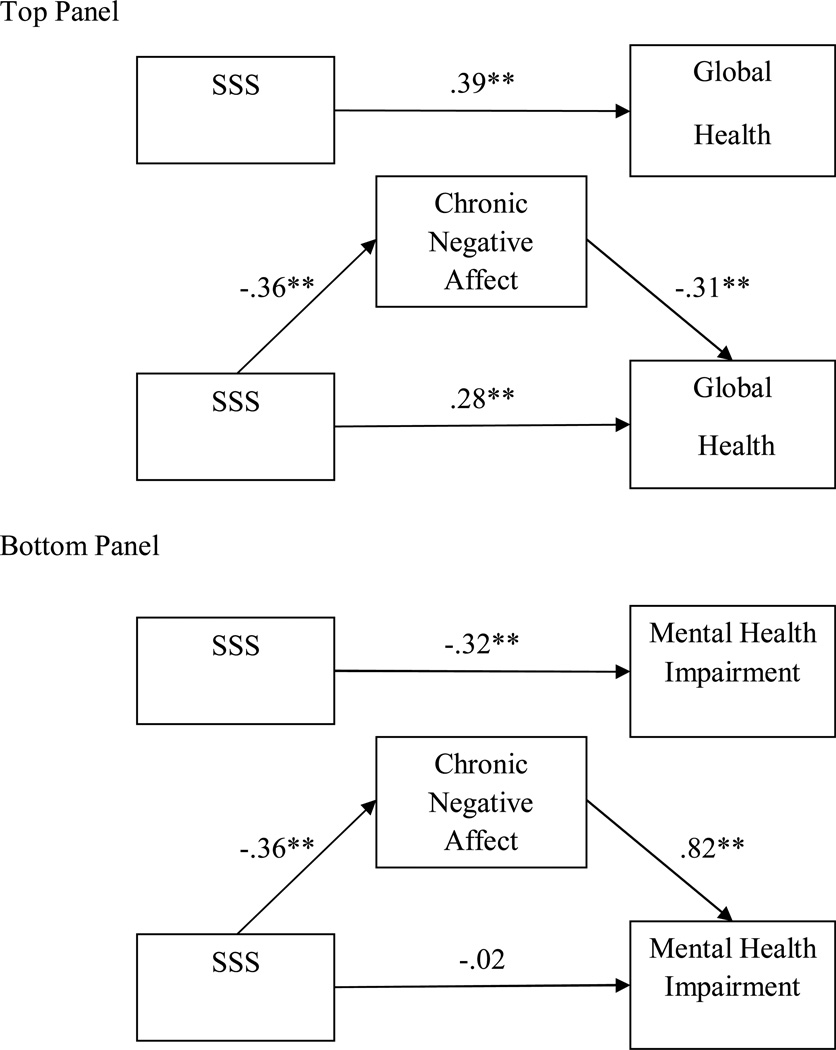
Our prediction was that chronic negative affect would mediate the relationship between SSS and self-rated health. Our first analysis examined chronic negative affect—measured by depression scores from the CESD—in relation to SSS and the single item global health measure. In this analysis, the path linking SSS to chronic negative affect was significant t(292) = −5.47, p < .01, as was the path linking chronic negative affect to self-rated global health t(292) = −4.76, p < .01. In addition, the originally significant relationship between SSS and self-rated global health t(293) = 5.83, p < .01 was reduced but was still significant when accounting for chronic negative affect t(292) = 4.11, p < .01. We tested the indirect path of SSS to self-rated global health through chronic negative affect using a bootstrapping procedure with 2,000 resamples (Preacher & Hayes, 2004; 2008). The analysis yielded a significant indirect effect with a 95% confidence interval between .03 and .09 indicating a significant partial mediation of SSS on self-rated global health, through chronic negative affect (see top panel of Figure 1).
Figure 1.
The top panel displays the model of the relationship between SSS and the single item global self-rated health measure mediated by chronic negative affect—measured with CESD scores. The bottom panel displays the model of the relationship between SSS and mental health impairment mediated by CESD chronic negative affect. Each model controls for key demographic variables (income, education, age, gender, and ethnicity) and current negative mood measured by the PANAS. The “*” indicates that p < .05 and the “**” indicates that p < .01.
Next we examined a mediation analysis for participants’ mental health impairment scores. In the analysis, the path from chronic negative affect to mental health impairment t(292) = 19.34, p < .01 was significant. Moreover, accounting for chronic negative affect rendered the originally significant relationship between SSS and mental health impairment t(293) = −4.67, p < .01 non-significant t(292) = −0.53, p = .60 (see bottom panel of Figure 1). The 95% confidence interval of the indirect effect was between −2.42 and −1.10 indicating a significant indirect effect of SSS on mental health impairment, through chronic negative affect. Interestingly, chronic negative affect was unrelated to physical health impairment t(293) = 0.70, p = .48 in our mediation model and thus could not explain the association between SSS and physical health impairment (Baron & Kenny, 1986).
We also conducted a parallel analysis using chronic negative affect measured through the PANAS. In the analysis examining mental health impairment, the path from chronic negative affect to mental health impairment was significant t(292) = −3.09, p < .05. Moreover, accounting for chronic negative affect reduced the original relationship between SSS and mental health impairment t(293) = −4.65, p < .01, though the reduced relationship was still significant t(292) = 03.45, p < .01. The 95% confidence interval of the indirect effect was −1.25 to −0.24 indicating a significant indirect effect of SSS on mental health impairment through chronic negative affect. In parallel mediation analyses, the PANAS chronic negative affect measure was unrelated to physical health impairment t(293) = −1.43, p = .15 and self-rated global health t(293) = .19, p = .85. Overall, these mediation analyses suggest that lower SSS impacts self-rated global health and mental health impairment, in part, through increased chronic negative affect, even when controlling for transient mood changes and demographic factors.
Discussion
In this study our goals were to determine (1) if ratings of SSS shift based on fluctuations in temporary mood states, (2) whether negative affect experienced at the time individuals report their SSS and their self-rated health acts as a confounding third variable, and (3) whether chronic negative affect lies on the causal pathway linking SSS to health. Statistical analyses in previous studies provide some initial evidence suggesting that rank, more than mood, underlies SSS ratings (Kraus et al., 2011), and that SSS relates in similar ways to global self-rated health as do reports of objective SES when adjusted for negative affect (Operario et al., 2004).
The earlier evidence was limited, however, because it was not possible to disentangle cross-sectional ratings of negative affect from ratings of SSS and global self-rated health. Results from our experiment provide new and stronger tests of likely causal directions of these consistently associated variables. In the current study, temporary shifts in negative mood had no effect on SSS ratings, nor did they impact associations of SSS to chronic negative affect, depression, or self-reports of mental and physical health impairment. These findings provide important evidence that associations between SSS and self-rated global health are independent of temporary shifts in mood states. Given the robust predictive power of self-rated health in predicting mortality (Idler & Benyamini, 1997), understanding associations between SSS and self-rated health has potentially far-reaching consequences for our understanding of long-term health outcomes associated with SES. Moroever, our finding that chronic negative affect partially explained the relationships between SSS and self-rated global health and mental health impairment, reinforces prior findings and provides additional evidence that chronically experienced negative affect explains, rather than confounds the link between SSS and self-rated health. These effects remained significant even after controlling for demographic factors—such as education, income, gender, age, and ethnicity—that covary with SSS and self-rated health.
Caveats and Future Directions
Notwithstanding the strength of the findings from the present investigation, several limitations to this research are worth noting. First, participants in the present sample were adults recruited from an online retail website. Prior recruitment using this online method has yielded data that is as reliable as that found with more traditional collection methods (e.g., Buhrmester et al., 2011). Moreover, SES demographic data from the current sample reflect that of the overall US population. Specifically, the median household income of the present sample was consistent with the median income reported in the 2009 current US population survey (Denavas-Walt, Proctor, & Smith, 2010). However, this remains a self-selected group that is not necessarily a true representative sample. For example, the sample may not reflect the extreme ends of the SES spectrum (e.g., wealthy individuals, people without computer access or with limited literacy). While there is no reason to believe that responses to the experimental manipulation or subsequent ratings of SSS and health were impacted by this truncated SES range, future research would benefit from including samples representing the full range of SES, so that the observed effects could be generalized with more confidence.
Although the sample included participants from different ethnic backgrounds, the majority were European-American and there were insufficient numbers to evaluate specific ethnic groups. Given previous findings that SSS associations to health vary by ethnic background (Adler et al., 2000) it will be important for future research to determine if the effects found in the current sample generalize to specific ethnic groups. Along these lines, only a small subset (10.3%) of participants was above the age of 50, and as such, the generalizeability of this research to older populations is limited.
Although our findings are consistent with our argument that chronic negative affect can best be understood as a mediator on a causal pathway from SSS to global health, rather than as a confound, our data are cross-sectional, making this conclusion promising, but preliminary. Future research would benefit from examining longitudinal associations between SSS, chronic negative affect, and self-rated health so that causal inferences can be drawn with more confidence. As well, the exact mechanisms by which chronic negative affect partially explains the relationship between SSS and self-rated health have yet to be uncovered. For instance, it is possible that perceptions of SSS vis-à-vis others lead to daily expectations for stigmatization, social rejection, or financial uncertainty that elevate negative mood, and over time, reduce global health. Future research is necessary to test this prediction.
Related to the finding that chronic negative affect may mediate relations between SSS and self-rated health, it would be interesting to assess the mediating role of discrete emotions—such as self-rated shame—given the central role of shame experiences for low status groups in society (Keltner et al., 2003), and previous research linking shame to poorer health (Gruenwald et al., 2004). It is possible that negative affect mediates relations between SSS and self-rated health through chronic shame experiences. Given that the current measures of negative affect—the PANAS and the CESD—were not designed to assess discrete emotions, future research is necessary to test this prediction.
Finally, the current research was designed to determine if associations of SSS to self-rated health were independent of transient negative mood. Other psychological variables—aside from negative affect—covary with SSS, such as perceptions of stress (Adler et al., 2000), personal sense of control (Kraus et al., 2009), or social support (Adler et al., 2000), and it will be important for future research to conduct similar studies in which these constructs are experimentally manipulated to determine if these variables lie on the causal pathway linking SSS to self-rated health, or if they confound that relationship. In light of the effect of the shame induction on self-rated global health and chronic negative affect, it is important to consider the nature of self-ratings of health. That a subtle manipulation of transient shame was effective in temporarily shifting perceptions of health and general affect suggests the powerful implications of shame for health more generally, as other researchers suggest (Gruenwald et al., 2004). Our finding that transient mood can modify perception and/or reporting of global health suggests that future research should take into account the contexts and conditions in which self-ratings of global health are completed.
Conclusion
SSS is an important aspect of everyday life, having robust associations to our global health. In this research we have provided evidence that this rank-based facet of SES shapes health in ways that are independent of temporary mood swings and other demographic factors. These findings illustrate the importance of understanding how subjective and objective facets of SES affect our life outcomes.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/HEA
Contributor Information
Michael W. Kraus, University of California, San Francisco
Nancy Adler, University of California, San Francisco.
Teh-Way David Chen, University of California, Berkeley.
References
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social class with psychological functioning: preliminary data in healthy White women. Health Psychology. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Buhrmester MD, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A new source of cheap, yet high-quality, data? Perspectives on Psychological Science. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press; 1969. [Google Scholar]
- Cohen S, Alper CM, Doyle WJ, Adler N, Treanor JJ, Turner RB. Objective and subjective socioeconomic status and susceptibility to the common cold. Health Psychology. 2008;27:268–274. doi: 10.1037/0278-6133.27.2.268. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken L. Applied multiple regression/correlation analysis for the behavioral sciences. Mahwah, New Jersey: Lawrence Erlbaum; 2003. [Google Scholar]
- Cohen S, Kaplan GA, Salonen JT. The role of psychological characteristics in the relation between socioeconomic status and perceived health. Journal of Applied Social Psychology. 1999;29:445–468. [Google Scholar]
- Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Social Science and Medicine. 2006;63:788–804. doi: 10.1016/j.socscimed.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P. Does psychological distress contribute to racial and socioeconomic disparities in mortality? Social Science & Medicine. 1997;45:1805–1809. doi: 10.1016/s0277-9536(97)00111-1. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Ghaed SG, Gallo LC. Subjective social status, objective socioeconomic status, and cardiovascular risk in women. Health Psychology. 2007;26:668–674. doi: 10.1037/0278-6133.26.6.668. [DOI] [PubMed] [Google Scholar]
- Gianaros PJ, Horenstein JA, Cohen S, Matthews KA, Brown SM, Flory JD, Critchley HD, Manuck SB, Hariri AR. Perigenual anterior cingulated morphology covaries with perceived social standing. Social Cognitive and Affective Neuroscience. 2007;2:161–173. doi: 10.1093/scan/nsm013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: Development and evaluation of a new indicator. Pediatrics. 2001;108:1–8. doi: 10.1542/peds.108.2.e31. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Kemeny ME, Aziz N, Fahey JL. Acute threat to the social self: Shame, social self-esteem, and cortisol activity. Psychosomatic Medicine. 2004;66:915–924. doi: 10.1097/01.psy.0000143639.61693.ef. [DOI] [PubMed] [Google Scholar]
- Hyde M, Jones IR. The long shadow of work—does time since labour market exit affect the association between socioeconomic position and health in a post-working population. Journal of Epidemiological and Community Health. 2007;61:533–539. doi: 10.1136/jech.2006.051284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP. Health and social cohesion: Why care about income inequality? British Medical Journal. 1997;314:1037–1040. doi: 10.1136/bmj.314.7086.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keltner D, Gruenfeld DH, Anderson C. Power, approach and inhibition. Psychological Review. 2003;110:265–284. doi: 10.1037/0033-295x.110.2.265. [DOI] [PubMed] [Google Scholar]
- Kopp M, Skrabski A, Réthelyi J, Kawachi I, Adler NE. Self-rated health, subjective social status, and middle-aged mortality in a changing society. Behavioral Medicine. 2004;30:65–72. doi: 10.3200/BMED.30.2.65-72. [DOI] [PubMed] [Google Scholar]
- Kraus MW, Piff PK, Keltner D. Social class, sense of control, and social explanation. Journal of Personality and Social Psychology. 2009;97:992–1004. doi: 10.1037/a0016357. [DOI] [PubMed] [Google Scholar]
- Kraus MW, Piff PK, Keltner D. Social class as culture: The convergence of resources and rank in the social realm. Current Directions in Psychological Science. 2011;100:246–250. [Google Scholar]
- MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin. 2005;131(2):202–223. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Räikkönen K, Gallo L, Kuller LH. Association between socioeconomic status and metabolic syndrome in women: Testing the reserve capacity model. Health Psychology. 2008;27:576–583. doi: 10.1037/0278-6133.27.5.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychology and Health. 2004;19:237–246. [Google Scholar]
- Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and Subjective Assessments of Socioeconomic Status and Their Relationship to Self-Rated Health in an Ethnically Diverse Sample of Pregnant Women. Health Psychology. 2000;19:613–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its associations with measures of ill-health in the Whitehall II study. Social Science & Medicine. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Kosinski M, Keller SD. SF-36 physical and mental summaries scales: A user’s manual. Boston: Health Institute, New England Medical Center; 1994. [Google Scholar]
- Ware JE, Jr, Kosinski M, Keller SD. A 12 Item Short Form Health Survey: Construction of scales and preliminary test of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of a brief measure of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1991;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Westermann R, Spies K, Stahl G, Hesse FW. Relative effectiveness and validity of mood induction procedures: A meta-analysis. European Journal of Social Psychology. 1996;26:557–580. [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. Annals of the New York Academy of Sciences. 1999;896:48–63. doi: 10.1111/j.1749-6632.1999.tb08104.x. [DOI] [PubMed] [Google Scholar]
- Williams KD. Ostracism. Annual Review of Psychology. 2007;58:425–452. doi: 10.1146/annurev.psych.58.110405.085641. [DOI] [PubMed] [Google Scholar]
- Wright CW, Steptoe A. Subjective socioeconomic position, gender and cortisol responses to waking in an elderly population. Psychoneuroendocrinology. 2005;30:582–590. doi: 10.1016/j.psyneuen.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Denavas-Walt C, Proctor D, Smith JC. U.S. Census Bureau, Current Population Reports. Income, poverty, and health insurance coverage in the United States: 2009. Washington, DC: 2010. [Google Scholar]