Abstract
Cardiovascular disease is one of the leading causes of death among reproductive-age women. In this study, we examine trends in the prevalence of dyslipidemia, hypertension, and related clinicians’ advice among reproductive-age women. We conducted trend analysis of these factors among non-pregnant women aged 20–49 years (n = 5,768) using National Health and Nutrition Examination Survey (NHANES) data obtained between 1999 and 2008. Multiple linear regression and logistic regression analyses were used to examine linear trends over a 10-year period after adjusting for covariates. A downward trend was observed for the proportion of women with abnormal levels of low density lipoprotein (LDL; P = 0.038) and high density lipoprotein (HDL; P = 0.008) cholesterol from 1999 to 2008. In contrast, no significant changes were observed in the prevalence of abnormal total cholesterol (P = 0.948) and triglyceride levels (P = 0.300), or hypertension (P = 0.632). Based on the self-reported data, upward trends were observed in the rates of cholesterol checking (P = 0.002), high cholesterol (P = 0.012), receiving clinicians’ advice to use lipid-lowering agents (P < 0.001) and patients’ compliance with their advice (P < 0.001). Although rates of self-reported hypertension did not change over time (P = 0.120), receiving clinicians’ advice to use antihypertensive medications (P = 0.003) and patients’ compliance with these medications (P = 0.015) also increased significantly. Overall improvements in LDL and HDL cholesterol over this time period could be due to increases in related awareness, receiving advice to use medications, and patients’ compliance with this advice. Use of antihypertensive medication has also increased among reproductive-age women in the US.
Keywords: Reproductive-age women, Cholesterol, Triglyceride, Dyslipidemia, Hypertension
Introduction
Cardiovascular disease (CVD) risk factors are widely prevalent in reproductive-age women; 66 % are currently overweight or obese [1], 11 % have dyslipidemia, and 8 % have hypertension [2]. As both dyslipidemia and hypertension have reproductive health consequences, awareness, identification and management of these conditions are important to prevent related morbidity and mortality in young women. For example, dyslipidemia is associated with polycystic ovary syndrome [3], a leading cause of infertility [4]. It has also been reported that dyslipidemia during pregnancy may exert adverse effects on the mother including preeclampsia and gestational diabetes [5–7], which are well recognized risk-factors for the development of type 2 diabetes and CVD in later life [8, 9]. Hypertension during pregnancy is also associated with preeclampsia, placental abruption, preterm delivery, low birth weight, and infant death [10–13]. Moreover, hypertensive disorders in pregnancy increase the risk of death from CVD among reproductive-age women [14].
Several US studies have used public data to report trends of major lipid fractions in the US, self-reported high cholesterol and use of lipid-lowering medications as well as the prevalence of hypertension and use of antihypertensive medications [15–21]. However, these studies have not examined the trends among women of reproductive-age using data generated during the last decade. Moreover, trends in clinicians’ advice and patients’ compliance with their advice to reduce hypercholesterolemia and hypertension have not been reported.
The objectives of this study were to examine recent trends among young women in the prevalence of dyslipidemia and hypertension as well as self-reported hyper-cholesterolemia and hypertension, clinicians’ advice to patients with regard to lipid-lowering and antihypertensive medications, and patients’ compliance with their recommendations.
Methods
Study Population
NHANES 1999–2008 is a continuous, cross-sectional survey conducted by the National Center for Health Statistics/Center for Disease Control and Prevention (NCHS/CDC). The data are released in 2-year cycles. Each cycle included a nationally representative sample of the noninstitutionalized US civilian population selected through a complex, stratified, multistage probability sampling design. Detailed methods of this survey have been published [22]. Participants first received a detailed in-person home interview, followed by a visit to a mobile examination center for the administration of additional questionnaires, a physical examination, and laboratory tests.
This study used data on reproductive-age women (20–49 years) obtained from five 2-year study cycles: 1999–2000, 2001–2002, 2003–2004, 2005–2006, and 2007–2008. The overall response rate for interviews among this group of women for each study cycle was 81.7 (1,373/1,681), 82.7 (1,562/1,888), 77.2 (1,329/1,722), 80.3 (1,504/1,872), and 80.0 % (1,459/1,824), respectively. The overall response for their completed examinations for each study cycle was 76.0 (1,277/1,681), 79.1 (1,494/1,888), 73.8 (1,271/1,722), 77.4 (1,448/1,872), and 78.3 % (1,429/1,824), respectively. A total of 7,227 reproductive age women were interviewed while 6,919 completed examination during 1999–2008. After excluding women with a positive urine pregnancy test or self-reported pregnancy (n = 1,151), the final sample included 5,768 women. NHANES 1999–2008 received approval from the National Center for Health Statistics research ethics review board. All participants provided written informed consent [22]. This study used de-identified publicly available data and thus was exempt from full review by the institutional review board at the University of Texas Medical Branch.
Data Collection
This study analyzed serum lipids and blood pressure (BP) data, self-reported high cholesterol, high BP, use of lipid-lowering and antihypertensive medications as well as clinicians’ advice and patients’ compliance with this advice to reduce high cholesterol and BP. Demographic variables, body mass index (BMI), and waist circumference (WC) data were also included. BMI was stratified ≥25 kg/m2 (combined overweight and obesity) and BMI ≥30 kg/m2 (obesity). Age was calculated using years data. Race/ethnicity was determined by a self-report and categorized as non-Hispanic white, non-Hispanic black, Hispanic and other (American Indian, Native Alaskan, Asian or Pacific Islander, and other race not specified). Information about education level, marital status, smoking status and annual income were obtained by self-report [22].
Low-density lipoprotein (LDL) cholesterol and triglyceride (TG) levels were based on morning samples taken after fasting for 8–24 h whereas total cholesterol (TC) and high density lipoprotein (HDL) cholesterol levels were based on samples taken regardless of fasting [15, 16, 23–25]. Methods for measuring, calculating, and analyzing all lipid fractions for NHANES 1999 to 2006 surveys have previously been reported [15–18, 26]. From 2007 to 2008, the laboratory methods were same as previous years, but there were changes in the laboratory site (from the Johns Hopkins University to the University of Minnesota) and analyzing instrument (from Roche Hitachi 717 and 912 to Roche Modular P chemistry) for lipids testing [23–25]. The measurements of TC, TG and HDL cholesterol were standardized for each NHANES survey according to the CDC Lipid Standardization Program [15, 16, 27], wherein the HDL cholesterol values were found to be within the 5 % maximum allowable bias [25]. LDL cholesterol was calculated according to the Friedewald equation (serum TC-HDL cholesterol-serum TG/5) for serum TG levels ≤400 mg/dl [23, 28]. Abnormal TC (≥200 mg/dl), LDL cholesterol (≥130 mg/dl), HDL cholesterol (< 40 mg/dl), and TG (≥150 mg/dl) were categorized based on a criteria from the NCEP ATP III [29].
Self-reported data on cholesterol checking, high cholesterol, clinicians’ advice with regard to life style changes (eating less high fat/cholesterol food, controlling/losing weight, and increasing physical activity/exercise) and medication use for high cholesterol, and patients’ compliance with their clinicians’ advice were obtained by self-report. Self-reported lipid medication use was confirmed by assessing the prescription dataset for the NHANES 1999–2008.
Blood pressure (BP) was measured 3–4 times using a sphygmomanometer [20]. We calculated mean SBP and DBP (mean ± SE) as the average of these measures after excluding the first measurement [30, 31]. We also obtained self-reported data on hypertension, clinicians’ advice to use antihypertensive medication, and patients’ compliance with these medications. We assessed the prescription dataset for the NHANES 1999–2008 to confirm any antihypertensive medication use (a report of using one or more of these medications). Actual hypertension, defined as mean SBP ≥140 mm Hg or a mean DBP ≥90 mm Hg or both, or current treatment with prescription medications to control BP (< 140 mm Hg and < 90 mm Hg) was also examined [20, 21, 31, 32].
Statistical Analysis
All analyses were conducted using STATA 10 svy commands (STATA Corporation, College Station, TX) according to NHANES analytical guidelines by taking into account survey weighting for the complex survey design, which consisted of multistage, stratified, clustered samples [33]. Probability sampling weights were used in conjunction with strata and primary sampling units (psu) to weight the analysis. Simple descriptive statistics were used to describe the study population for each of the five 2-year study cycles. Variance of proportions was estimated with Taylor series linearization. We used multivariate analyses using multiple linear regression and logistic regression analyses to examine the trend of different parameters over the five 2-year survey cycles from 1999 to 2008, after adjusting for age, race/ethnicity, and survey cycles. Age and survey cycles were treated as continuous variables.
Results
Overall, the proportion of 20–49 year old Hispanic women increased steadily over the 10-year period (P < 0.001) while other races (American Indian, Native Alaskan, Asian or Pacific Islander, and other race not specified) decreased significantly (P < 0.001) Education, marital status, household income, and current smoking status of these women did not change significantly over the intervals (Table 1).
Table 1.
Characteristics of non-pregnant reproductive-age women (20–49 years), NHANES 1999–2008
| 1999–2000 (n = 1,023) | 2001–2002 (n = 1,198) | 2003–2004 (n = 1,042) | 2005–2006 (n = 1,123) | 2007–2008 (n = 1,372) | P for trend | |
|---|---|---|---|---|---|---|
| Age, year, mean (± SE) | 35.0 (0.2) | 34.9 (0.4) | 35.4 (0.3) | 35.3 (0.3) | 35.2 (0.4) | 0.866 |
| Race/ethnicity, % (± SE) | ||||||
| White | 69.7 (3.4) | 69.0 (2.7) | 71.4 (3.6) | 71.2 (2.8) | 69.9 (3.7) | 0.194 |
| Black | 13.4 (2.0) | 13.7 (2.4) | 14.4 (2.1) | 14.5 (2.3) | 14.2 (2.5) | 0.826 |
| Hispanic | 7.2 (1.6) | 8.8 (1.0) | 9.5 (2.2) | 9.7 (1.1) | 9.6 (1.9) | <0.001* |
| Othersa | 9.6 (3.5) | 8.5 (2.5) | 4.7 (0.8) | 4.6 (1.0) | 6.4 (1.5) | <0.001* |
| Education, % (± SE) | ||||||
| Less than high school | 17.9 (1.3) | 16.8 (1.6) | 15.1 (1.4) | 13.7 (1.7) | 18.0 (1.7) | 0.100 |
| High school diploma | 25.8 (2.6) | 23.4 (1.5) | 24.6 (1.4) | 21.6 (1.3) | 20.9 (1.1) | 0.072 |
| More than high school | 56.3 (3.0) | 59.8 (2.5) | 60.3 (1.4) | 64.7 (2.5) | 61.1 (2.3) | 0.072 |
| Marital status, % (± SE) | ||||||
| Never married | 24.0 (2.1) | 22.9 (2.0) | 23.6 (1.7) | 21.3 (1.9) | 24.4 (2.4) | 0.841 |
| Married/live together | 58.0 (1.8) | 64.5 (1.9) | 60.6 (1.4) | 65.8 (2.2) | 61.7 (2.3) | 0.317 |
| Widowed/divorced/separated | 18.0 (1.4) | 12.6 (1.2) | 15.8 (1.9) | 12.8 (1.2) | 13.9 (1.0) | 0.549 |
| Household income, % (± SE) | ||||||
| <$20,000 | 19.2 (2.3) | 19.9 (1.1) | 17.4 (1.7) | 13.3 (1.1) | 16.5 (1.7) | 0.110 |
| $20,000–$34,999 | 25.9 (2.0) | 17.1 (1.2) | 20.0 (2.0) | 17.9 (1.5) | 19.8 (1.3) | 0.549 |
| $35,000–$64,999 | 24.8 (1.7) | 27.7 (1.3) | 28.5 (1.8) | 26.1 (1.3) | 23.4 (1.9) | 0.549 |
| $65,000 and above | 30.1 (3.8) | 35.2 (1.7) | 34.1 (2.7) | 42.7 (2.8) | 40.3 (3.3) | 0.110 |
| Current smoking status, % (± SE) | 30.2 (1.6) | 29.0 (1.9) | 31.3 (2.0) | 28.0 (2.1) | 26.8 (2.0) | 0.800 |
Data are weighted to the US population
Statistical significance (P < 0.05) over the 5 NHANES cycles between 1999 and 2008
Includes American Indian, Native Alaskan, Asian or Pacific Islander, and other race not specified
The prevalence of obesity (BMI ≥30 kg/m2) increased from 30.7 % in 1999–2000 to 34.2 % in 2007–2008, but did not achieve statistical significance (P = 0.100). However, when the categories of overweight and obesity were combined (≥25 kg/m2), a significant upward trend from 57.0 % in 1999–2000 to 62.2 % in 2007–2008 (P = 0.021) was observed. An upward linear trend from 47.4 % in 1999–2000 to 55.4 % in 2007–2008 was observed for abdominal obesity (WC > 88 cm) (P < 0.001). A statistically significant upward trend was also observed for mean body weight (from 74.4 to 76.1) (P = 0.036), BMI (from 27.8 to 28.4) (P = 0.039), and WC (from 89.7 to 93.1) (P < 0.001) from 1999 to 2008.
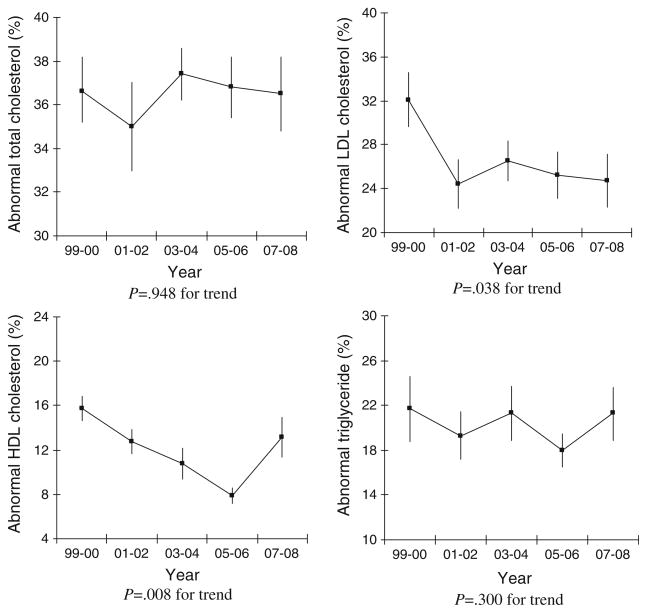
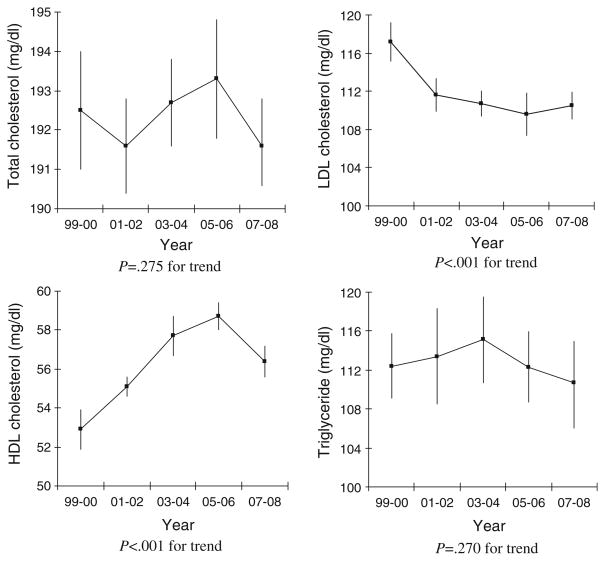
No significant changes were observed between 1999 and 2008 in the proportion of reproductive-age women with abnormal TC (P = 0.948) or TG (P = 0.300) between 1999 and 2008. The proportion of women with abnormal LDL (≥130 mg/dl) and HDL cholesterol (< 40 mg/dl) did decrease significantly from 32 % to 25 % (P = 0.038) and 16 % to 13 % (P = 0.008), respectively (Fig. 1). Trend analysis based on mean levels of LDL and HDL also showed positive directions (Fig. 2). Mean HDL cholesterol rose from 52.9 mg/dl to 56.4 mg/dl (P < 0.001), while mean LDL cholesterol declined from 117.2 mg/dl to 110.5 mg/dl (P < 0.001) over the 10-year period. Significant changes were not observed for mean TC (P = 0.275) and TG (P = 0.270) levels.
Fig. 1.
Trends in the proportion (%) of non-pregnant reproductive-age women (20–49 years) with abnormal serum lipids, NHAHES 1999–2008. The bars indicate standard errors of the measurements
Fig. 2.
Trends in mean lipid fractions among non-pregnant reproductive-age women (20–49 years), NHANES 1999–2008. The bars indicate standard errors of the measurements
Based on self-reported data, we observed that the proportion of women who had their cholesterol level checked and were labeled to have hypercholesterolemia increased significantly over the 10-year period (P = 0.002 and P = 0.012, respectively) (Table 2). In addition, the proportion of women who received advice from a clinician to reduce their cholesterol level and were compliant with this advice also increased. The proportion of women who were labeled as hypertensive on ≥2 occasions did increase from 10 % in 1999–2000 to 13 % in 2007–2008, but did not achieve statistical significance (P = 0.120) (Table 3). The proportion who received advice from their clinician to use medication for hypertension increased significantly from 8 % to 12 % (P = 0.003) and their compliance with this recommendation increased from 6 % to 9 % (P = 0.015) during this same period. However, the proportion of women with actual hypertension did not change significantly (P = 0.632) over the 10-year period.
Table 2.
Trends in self-reported cholesterol and cholesterol-related behaviors among non-pregnant reproductive-age women (20–49 years), NHANES 1999–2008
| 1999–2000 (n = 1,001) % (± SE) |
2001–2002 (n = 1,137) % (± SE) |
2003–2004 (n = 1,019) % (± SE) |
2005–2006 (n = 1,077) % (± SE) |
2007–2008 (n = 1,314) % (± SE) |
P for trend | |
|---|---|---|---|---|---|---|
| Ever had blood cholesterol checked | 61.3 (2.9) | 61.4 (1.9) | 64.1 (1.7) | 67.2 (2.0) | 65.2 (1.9) | 0.002* |
| Ever told to have high cholesterol level | 15.6 (1.2) | 12.6 (1.1) | 15.9 (1.6) | 17.7 (1.2) | 18.6 (1.1) | 0.012* |
| Ever told to eat less fat to reduce cholesterol | 12.4 (1.3) | 9.6 (1.0) | 12.2 (1.2) | 14.5 (1.0) | 15.0 (1.2) | 0.025* |
| Now eating food with less fat and cholesterol | 8.7 (1.1) | 6.2 (0.9) | 9.1 (1.0) | 11.0 (0.9) | 11.2 (1.0) | 0.002* |
| Ever told to reduce weight to reduce cholesterol | 8.1 (1.2) | 6.0 (0.8) | 8.6 (1.2) | 10.2 (1.0) | 10.4 (0.8) | 0.004* |
| Now controlling weight/losing weight | 5.5 (0.8) | 3.6 (0.7) | 6.2 (0.9) | 8.0 (0.7) | 8.4 (0.6) | < 0.001* |
| Ever told to exercise more to reduce cholesterol | 9.5 (1.0) | 7.9 (1.3) | 10.7 (1.4) | 11.2 (1.2) | 13.2 (1.0) | 0.006* |
| Now increasing exercise/activity | 6.7 (0.7) | 4.6 (0.7) | 6.8 (1.3) | 8.2 (1.0) | 9.9 (0.9) | 0.002* |
| Ever told to take prescribed medicine | 2.6 (0.8) | 2.3 (0.6) | 4.9 (0.9) | 5.9 (1.0) | 7.4 (0.9) | < 0.001* |
| Now taking prescribed medicine | 1.7 (0.5) | 1.9 (0.5) | 3.3 (0.8) | 3.5 (0.6) | 4.4 (0.6) | < 0.001* |
Data are weighted to the US population
Statistical significance (P < 0.05) over the 5 NHANES cycles between 1999 and 2008
Table 3.
Trends in the self-reported and actual rates of hypertension among non-pregnant reproductive-age women (20–49 years) in the NHANES 1999–2008
| 1999–2000 (n = 1,015) % (± SE) |
2001–2002 (n = 1,193) % (± SE) |
2003–2004 (n = 1,041) % (± SE) |
2005–2006 (n = 1,118) % (± SE) |
2007–2008 (n = 1,371) % (± SE) |
P for trend | |
|---|---|---|---|---|---|---|
| Ever told to have high blood pressure | 12.4 (1.6) | 14.5 (1.1) | 16.1 (1.4) | 15.6 (2.2) | 16.3 (1.5) | 0.107 |
| Ever told to have high blood pressure on two or more visits | 9.6 (1.2) | 10.7 (0.9) | 11.3 (0.9) | 12.0 (1.8) | 12.9 (1.3) | 0.120 |
| Ever told to take prescribed medicine | 7.7 (0.9) | 9.3 (0.9) | 9.4 (1.0) | 10.4 (1.5) | 12.0 (1.3) | 0.003* |
| Now taking prescribed medicine | 5.6 (0.9) | 6.7 (0.8) | 6.8 (0.9) | 7.0 (0.8) | 8.6 (1.0) | 0.015* |
| Actual hypertensiona | 12.0 (1.2) | 12.1 (1.2) | 11.6 (0.8) | 10.7 (1.3) | 12.4 (1.1) | 0.632 |
Data are weighted to the US population
P for trend denotes statistical significance (< 0.05) over the 5 NHANES cycles between 1999 and 2008
Actual hypertension as mean systolic blood pressure (BP) ≥140 mm Hg, diastolic BP ≥90 mm Hg, or both, or participants currently taking antihypertensive medication to control BP (< 140 and < 90 mm Hg)
Discussion
We found a significant downward trend in mean LDL cholesterol and the percentage of women with abnormal LDL cholesterol (≥130 mg/dl) between 1999 and 2008. Similar trends have been observed in prior studies examining NHANES data on all adults (1999–2000 vs. 2005–2006 periods and 1988–1994 vs. 1999–2002/1999–2006 waves) [15–17]. However, we did not find any significant changes in mean TC or the prevalence of abnormal TC (≥200 mg/dl) in contrast to Cohen et al. [16], who observed significantly downward trends of these values in all adults when comparing the 1988–1994 and 1999–2006 waves. This prior study found greater decreases in mean TC among older age groups than younger which could explain the difference between their findings and ours. Moreover, our observation that mean HDL cholesterol increased and abnormal HDL cholesterol (< 40 mg/dl) decreased significantly between 1999 and 2008 is consistent with a prior study which compared these values between 1988–1994 and 1999–2006 among adults [16]. Improvements in LDL and HDL cholesterol levels during this interval could be due to the fact that an increased proportion of women reported checking their blood cholesterol, having been diagnosed with high cholesterol, receiving advice from their clinicians to modify their lifestyle or using medication to reduce their cholesterol.
We observed that mean TG and the prevalence of abnormal TG (≥150 mg/dl) did not show any upward trend among reproductive-age women in the last decade. Cohen et al. [16], on the other hand, found an upward trend in mean TG and the prevalence of abnormal TG based on all adults when comparing the 1988–1994 to the 1999–2006 NHANES waves. It has been reported that dietary and lifestyle modifications, including body weight control, regular physical activity, less fat intake, low carbohydrate diet, and smoking cessation, are first-line therapy for all lipid disorders, especially hypertriglyceridemia [29, 34]. Significant increases in recommendations for lifestyle modification and patients’ compliance with these among reproductive-age women since 1999–2000 may have played an important role in this regard. However, our finding that abdominal obesity (WC > 88 cm) and combined overweight and obesity (≥25 kg/m2) significantly increased among these women over the 10 years is concerning. As elevated triglyceride levels are strongly correlated with increased WC and BMI [35–37], measures need to be taken to control obesity to avoid adverse consequence on lipids and other risks for CVD.
Our finding that the prevalence of hypertension did not change significantly among reproductive-age women between 1999 and 2008 is in agreement with Egan et al.’s study [21] based on all adult women for the same time frame. Although the proportion of women with self-reported hypertension on ≥2 occasions did not increase significantly over time, the rates gradually reached almost the same level of actual hypertension (12.9 % vs. 12.4 %) during the 2007–2008 period, which indicates gradual increase in awareness regarding hypertension. The self-reported rates of receiving clinicians’ advice to use antihypertensive medications and patients’ compliance with these medications were consistent with the findings reported by several other studies based on data from different NHANES cycles [21, 31, 38].
Identifying dyslipidemia and hypertension is very important in reproductive-age women to prevent pregnancy related complications as well as CVD in later life. Our study observed a gradual improvement in lipid profiles, an unchanged hypertension prevalence, and higher frequency of clinicians’ advice and patient compliance with this advice over the 10-year period. Early interventions targeted at this group may help improve the scenario even further. Future trend analysis with regard to dyslipidemia and hypertension related complications, such as polycystic ovary syndrome, infertility, preeclampsia, placenta abruption, preterm delivery, low birth weight, and infant death over time may shed more light on the impact of these improvements among young women.
The strengths of our study include use of a database with a nationally representative large sample, standardized protocols, in-person household interviews, and standard laboratory procedures. Despite these strengths, the study has several limitations. First, cross-sectional survey data prevents our ability to establish causal relationships or pathways to the trends we observed. Second, although the collection of examination and laboratory data were standardized, self-reported data from interviews and questionnaires are subject to bias. Third, our study population was limited to 20–49 year old women. Thus, our findings may not be applicable to older women who are at higher risk of hypertension, lipid disorders and CVD. Fourth, statistical significance trends may not be always meaningful as one extreme value may have influenced the significance level of the trend test. So caution should be taken when interpreting statistical significance. Finally, BP measurements were performed only at a single time point while a clinical diagnosis of hypertension is based on the average of ≥2 properly measured BP readings on 2 separate occasions. It is therefore possible that some subjects were misclassified with regard to their hypertension status.
In conclusion, the results from this study suggest that reproductive-age women have been experiencing a gradual improvement in both LDL and HDL cholesterol levels, although other lipid fractions and prevalence of hypertension remain almost unchanged. Overall improvement with regard to LDL and HDL cholesterol among reproductive-age women may be due to an increase in awareness, or clinician recommendations to modify their lifestyle and use medications as well as improvement in patient compliance with this advice.
Contributor Information
Tabassum H. Laz, Email: tahaquel@utmb.edu.
Mahbubur Rahman, Email: marahman@utmb.edu.
Abbey B. Berenson, Email: abberens@utmb.edu.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. [Accessed September 22, 2011];National center for health statistics: Health data interactive. Available at: http://www.cdc.gov/nchs/hdi.htm.
- 3.Boomsma CM, Fauser BC, Macklon NS. Pregnancy complications in women with polycystic ovary syndrome. Seminars in Reproductive Medicine. 2008;26(1):72–84. doi: 10.1055/s-2007-992927. [DOI] [PubMed] [Google Scholar]
- 4.Phelan N, O’Connor A, Kyaw-Tun T, Correia N, Boran G, Roche HM, et al. Lipoprotein subclass patterns in women with polycystic ovary syndrome (PCOS) compared with equally insulin-resistant women without PCOS. The Journal of Clinical Endocrinology and Metabolism. 2010;95(8):3933–3939. doi: 10.1210/jc.2009-2444. [DOI] [PubMed] [Google Scholar]
- 5.Catov JM, Ness RB, Wellons MF, Jacobs DR, Roberts JM, Gunderson EP. Prepregnancy lipids related to preterm birth risk: The Coronary Artery Risk Development in Young Adults Study. Journal of Clinical Endocrinology and Metabolism. 2010;95(8):3711–3718. doi: 10.1210/jc.2009-2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nature Clinical Practice Endocrinology & Metabolism. 2007;3(10):696–704. doi: 10.1038/ncpendmet0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiznitzer A, Mayer A, Novack V, Sheiner E, Gilutz H, Malhotra A, et al. Association of lipid levels during gestation with preeclampsia and getational diabetes mellitus: A population-based study. American Journal of Obstetrics and Gynecology. 2009;201:482.el–488.el. doi: 10.1016/j.ajog.2009.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Craici IM, Wagner SJ, Hayman SR, Garovic VD. Pre-eclamptic pregnancies: An opportunity to identify women at risk for future cardiovascular disease. Womens Health. 2008;4:133–135. doi: 10.2217/17455057.4.2.133. [DOI] [PubMed] [Google Scholar]
- 9.Golden SH, Bennett WL, Baptist-Roberts K, Wilson MN, Barone B, Gary TL, et al. Antepartum glucose tolerance test results as predictor of type 2 diabetes mellitus in women with a history of gestational diabetes mellitus: A systematic review. Gender Medicine. 2009;6:109–122. doi: 10.1016/j.genm.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: Systematic review of controlled studies. BMJ. 2005;330(7491):565. doi: 10.1136/bmj.38380.674340.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrer RL, Sibai BM, Mulrow CD, Chiquette E, Stevens KR, Cornell J. Management of mild chronic hypertension during pregnancy: A review. Obstetrics and Gynecology. 2000;96(5 Pt 2):849–860. doi: 10.1016/s0029-7844(00)00938-8. [DOI] [PubMed] [Google Scholar]
- 12.Livingston JC, Maxwell BD, Sibai BM. Chronic hypertension in pregnancy. Minerva Ginecologica. 2003;55(1):1–13. [PubMed] [Google Scholar]
- 13.Simpson LL. Maternal medical disease: Risk of antepartum fetal death. Seminars in Perinatology. 2002;26(1):42–50. doi: 10.1053/sper.2002.29838. [DOI] [PubMed] [Google Scholar]
- 14.Rich-Edwards JW, McElrath TF, Karumanchi SA, Seely EW. Breathing life into the life course approach: Pregnancy history and cardiovascular disease in women. Hypertension. 2010;56:331–334. doi: 10.1161/HYPERTENSIONAHA.110.156810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, et al. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–1781. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 16.Cohen JD, Cziraky MJ, Cai Q, Wallace A, Wasser T, Crouse JR, et al. 30-year trends in serum lipids among United States adults: Results from the National Health and Nutrition Examination Surveys II, III, and 1999–2006. American Journal of Cardiology. 2010;106:969–975. doi: 10.1016/j.amjcard.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 17.Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low-density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009;302:2104–2110. doi: 10.1001/jama.2009.1672. [DOI] [PubMed] [Google Scholar]
- 18.Hyre AD, Muntner P, Menke A, Raggi P, Jiang A. Trends in ATP-III-defined High blood cholesterol prevalence, awareness, treatment and control among US adults. Annals of Epidemiology. 2007;17:548–555. doi: 10.1016/j.annepidem.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 19.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: Impact of the 2001 National Cholesterol Education Program Guideline. Annals of Pharmacotherapy. 2008;42:1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 20.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 21.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. [Accessed April 17, 2011];National health and nutrition examination survey: Questionnaires, datasets, and related documentation. Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 23.Centers for Disease Control and Prevention. National health and nutrition examination survey 2007–2008 data documentation, code book, and frequencies. [Accessed on April 17, 2011];Triglycerides and LDL-cholesterol (TRIGLY_E) Available at: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/TRIGLY_E.htm.
- 24.Centers for Disease Control and Prevention. National health and nutrition examination survey: 2007–2008 data documentation, code book, and frequencies. [Accessed on April 17 2011];Total cholesterol (TCHOL_E) Available at: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/TCHOL_E.htm.
- 25.Centers for Disease Control and Prevention. National health and nutrition examination survey 2007–2008 data documentation, code book, and frequencies. [Accessed on April 17, 2011];HDL-cholesterol (HDL_E) Available at: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/HDL_E.htm.
- 26.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: Findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. 2003;107:2185–2189. doi: 10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 27.Myers GL, Cooper GR, Winn CL, Smith SJ. The Centers for Disease Control-National Heart, Lung and Blood Institute Lipid Standardization Program. An approach to accurate and precise lipid measurements. Clinics in Laboratory Medicine. 1989;9:105–135. [PubMed] [Google Scholar]
- 28.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry. 1972;18:499–502. [PubMed] [Google Scholar]
- 29.National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment Panel III). Third report of the national cholesterol education program (NCEP): Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment Panel III). Final report. Circulation. 106:3143–3421. [PubMed] [Google Scholar]
- 30.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 31.Ong KL, Cheung BMY, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment and control of hypertension among United States Adults, 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 32.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. [Accessed on April 17, 2011];National health and nutrition examination survey (NHANES): Analytic and reporting guidelines. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf.
- 34.Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481–1501. doi: 10.1161/CIRCULATIONAHA.107.181546. [DOI] [PubMed] [Google Scholar]
- 35.Carr MC, Brunzell JD. Abdominal obesity and dyslipidemia in the metabolic syndrome: Importance of Type 2 diabetes and Familial combined hyperlipidemia in coronary artery disease risk. The Journal of Clinical Endocrinology and Metabolism. 2004;89:2601–2607. doi: 10.1210/jc.2004-0432. [DOI] [PubMed] [Google Scholar]
- 36.Franssen R, Monajemi H, Stroes ES, Kastelein JJ. Obesity and dyslipidemia. Endocrinology and Metabolism Clinics of North America. 2008;37:623–633. doi: 10.1016/j.ecl.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Tanko LB, Bagger YZ, Qin G, Alexandersen P, Larsen PJ, Christiansen C. Enlarged waist combined with elevated triglycerides is a strong predictor of atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation. 2005;111:1883–1890. doi: 10.1161/01.CIR.0000161801.65408.8D. [DOI] [PubMed] [Google Scholar]
- 38.Gu Q, Paulose-Ram R, Dillon C, Burt V. Antihypertensive medication use among US adults with hypertension. Circulation. 2006;113:213–221. doi: 10.1161/CIRCULATIONAHA.105.542290. [DOI] [PubMed] [Google Scholar]