Abstract
As the first nationwide Korean prospective multicenter data collection registry, the Korea Acute Myocardial Infarction Registry (KAMIR) launched in November 2005. Through a number of innovative approaches, KAMIR suggested new horizons about acute myocardial infarction (AMI) which contains unique features of Asian patients from baseline characteristics to treatment strategy. Obesity paradox was existed in Korean AMI patients, whereas no gender differences among them. KAMIR score suggested new risk stratifying method with increased convenience and an enhanced accuracy for the prediction of adverse outcomes. Standard loading dose of clopidogrel was enough for Asian AMI patients. Triple antiplatelet therapy with aspirin, clopidogrel and cilostazol could improve clinical outcomes than dual antiplatelet therapy with aspirin and clopidogrel. Statin improved clinical outcomes even in AMI patients with very low LDL-C levels. The rate of percutaneous coronary intervention was higher and door-to-balloon time was shorter than the previous reports. Zotarolimus eluting stents as the 2nd generation drug-eluting stent (DES) was not superior to the 1st generation DES, in contrast to the western AMI studies. KAMIR made a cornerstone in the study of Korean AMI and expected to be new standards of care for AMI with the renewal of KAMIR design to overcome its pitfalls.
Keywords: Acute Myocardial Infarction, ST-Elevation Myocardial Infarction, Non-ST-Elevation Myocardial Infarction
INTRODUCTION
As the first nationwide Korean prospective multicenter data collection registry, the Korea Acute Myocardial Infarction Registry (KAMIR) launched in November 2005, reflecting real-world treatment practices and outcomes in Asian patients diagnosed with acute myocardial infarction (AMI). The registry includes 52 community and teaching hospitals with facilities for primary percutaneous coronary intervention (PCI) and on-site cardiac surgery. Comprehensive review of extensive body of reports including large scale randomized clinical trials and meta-analysis made the basement of KAMIR design. After pilot study, Steering Committee of KAMIR revised the initial design, and KAMIR began to enroll patients formally. Data were collected by a trained study coordinator at each participating intsitution using a standarized case report form and protocol. Standardized definitions of all patient-related variables, procedure-related variables, and clinical outcome-related variables were used. Standardized definitions of all variables were instituited by the Steering Commitee Board of KAMIR. Data were registered and submitted from individual institutions via password-protected Internet-based electronic case report forms. The Steering Commitee of KAMIR authorized a core study laboratory only permitted to the principal study coordinators and sub-task (division) principal investigators. From November 2005 to January 2008, the registry enrolled 14,885 patients. The success of the KAMIR led to the establishment of the Korea Working Group on Myocardial Infarction (KorMI), a subsequent study of the KAMIR, which is an ongoing open-ended registry that captures data on the complete spectrum of patients with AMI including long-term clinical follow-up. The KorMI plus KAMIR includes 40,254 patients as of July 2012. The present article decribes current status of AMI based on analyses of the KAMIR.
Ethics statements
The study was conducted according to the Declaration of Helsinki. The institutional review board of all paticipating centers approved the study protocol. The approval number was I-2008--1-009 of Chonnam National University Hospital. Written informed consent was obtained from all participating patients.
RISK FACTORS AND CLINICAL OUTCOMES OF AMI
Well known risk factors for coronary heart disease were also highly distributed in Korean AMI patients as well as other registries (Table 1) (1-5). However, KAMIR and the Heart Institute of Japan Acute Myocardial Infarction (HIJAMI) registry (5) showed higher prevalence of diabetes mellitus and less body mass index (BMI) compared with western AMI registries (1-4).
Table 1.
Comparison of baseline clinical characteristics
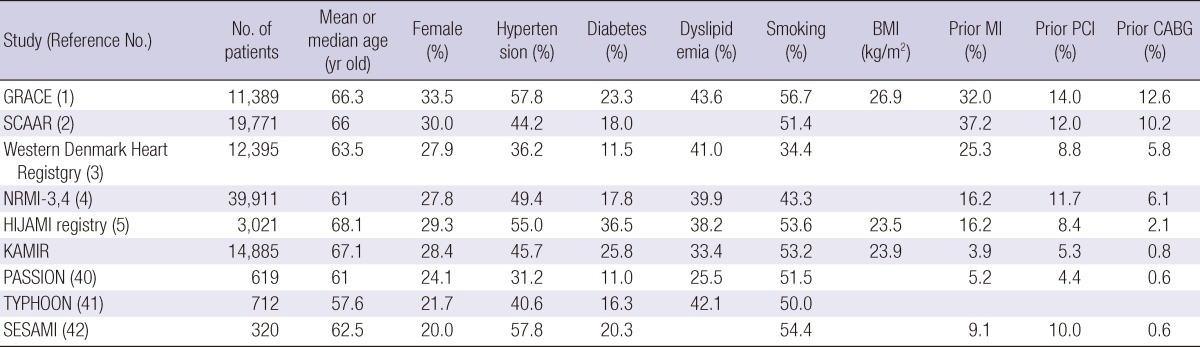
BMI, body mass index; CABG, coronary artery bypass grafting; GRACE, Global Registry of Acute Coronary Events; HIJAMI, Heart Institute of Japan Acute Myocardial Infarction registry; KAMIR, Korea Acute Myocardial Infarction Registry; MI, myocardial infarction; NRMI, National Registry of Myocardial Infarction; PASSION, Paclitaxel-Eluting Stent Versus Conventional Stent in Myocardial Infarction with ST-segment Elevation trial; SESAMI, Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction; SACCAR, Swedish Coronary Angiography and Angioplasty Registry; TYPHOON, Trial to Assess the Use of the Cypher Stent in Acute Myocardial Infarction Treated with Balloon Angioplasty.
Diabetes mellitus
Despite higher prevalence of diabetes mellitus in Korean AMI patients, KAMIR showed worse clinical outcomes among them similar to the previous studies (1, 6). Analysis using KAMIR data showed that hypertensive AMI patients accompanied with diabetes were associated with worse clinical and angiographic features, with a higher risk of development of severe heart failure, and an increased risk of in-hospital mortality and 1 yr adverse cardiac events (7). Furthermore, when diabetic AMI patients accompanied with renal insufficiency, 1-yr mortality were increased compared with those without diabetes nor renal insufficiency (adjusted hazard ratio [HR] 2.42, 95% confidence interval [CI] 1.62-3.62) (8). With regard to clinical outcomes after 1st generation drug eluting stents (DES), KAMIR analysis showed interesting results (9). Diabetes itself has been regarded as the risk factor for in-stent restenosis, which might contribute the increased overall major adverse cardiac events (MACEs). Also, many studies showed that the patients with paclitaxel-eluting stents (PES) had an increased risk for repeated revascularization compared with the patients with sirolimus-eluting stents (SES) (10-12). In the overall population, 1 yr MACE rate was significantly higher in the PES than the SES group (11.6% vs 8.6%, P = 0.014), which was mainly due to increased target lesion revascularization (TLR). In diabetic subgroup, the MACE rates were not different between the patients with PES and the patients with SES, in contrast to the nondiabetic subgroup, where PES was inferior to SES. These results suggest that diabetes differentially affects the outcome of 1st generation DES.
Obesity
Asian AMI patients showed less body mass index (BMI), which could be partially explained by ethnic differences, and dietary patterns. Generally, obesity is associated with an increased risk of developing cardiovascular disease. However, it might also be associated with better outcomes after AMI (obesity paradox). The relationship between obesity and clinical outcomes after AMI was analyzed based on KAMIR data (13, 14). Obese patients had significantly lower in-hospital and overall mortality, whereas the highest mortality was present in the lowest BMI patients. In an adjusted model, the underweight (HR, 2.88; 95% CI, 1.17-6.08) remained as mortality risk factors. Obesity paradox was existed in Korean AMI patients, and it could be explained by better use of medical treatment, hemodynamic stability, and younger age in obese AMI patients.
Gender
Female AMI patients usually constitute one third of total AMI patients across all the western and Asian studies (Table 1). There has been controversy over the disparity between men and women with regard to the management and prognosis of AMI. Many studies on gender difference after AMI have demonstrated that women had a higher mortality and usually receive less aggressive treatment than men (15, 16). Those were partially true in contemporary era proved by KAMIR analysis. Consistently KAMIR analyses across different study population showed that female gender itself was not the independent risk factor for the poor outcomes, although female AMI patients had significantly higher in-hospital mortality and long-term MACE rates (17-19). Women had longer pain-to-door time and more severe hemodynamic status than men. Also, female AMI patients were older, and had more frequent comorbidites including hypertension, diabetes, and dyslipidemia than male AMI patients. These characteristics of female AMI patients made gender effect. In the initial selection of treatment strategy, there was no gender difference between males and females in KAMIR (20).
RISK STRATIFICATION
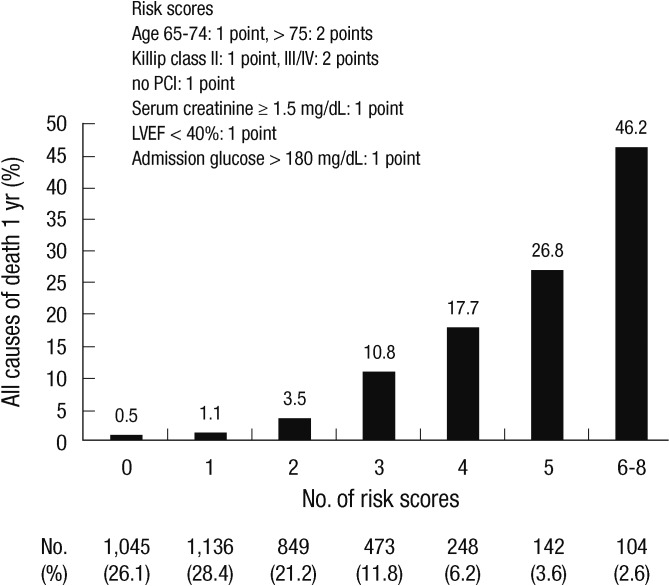
A new risk scoring system in myocardial infarction (MI)
Risk stratification determined at the time of AMI could result in a substantial benefit if appropriate interventions are made in selected high-risk patients for MACEs. Thrombolysis in Myocardial Infarction (TIMI) risk score (21) and the Global Registry of Acute Coronary Events (GRACE) risk models (1) are well known risk scoring system to assess the risk of death across an entire spectrum of MI. However, these models were developed and validated on data from the late 1990s and early 2000s. Patients and procedural characteristics have been changed. Also, none of these risk models have focused on new parameters in current clinical situations. KAMIR score was devised to overcome these limitations based on the strongest factors independently associated with one year survival (Fig. 1) (22, 23). Also, KAMIR score focused more convenient and simple bedside clinical risk scoring system. KAMIR score composed of 6 independent variables related to the 1 yr mortality: age (65-74 yr old, 1 point; > 75 yr, 2 points), Killip class (II, 1 point; > II, 2 points), serum creatinine (≥ 1.5 mg/dL, 1 point), no in-hospital PCI (1 point), left ventricular ejection fraction (< 40%, 1 point), and admission glucose (> 180 mg/dL, 1 point). The KAMIR score demonstrated significant differences in predictive accuracy for 1-yr mortality compared to the GRACE score for the developmental and validation cohorts (Table 2).
Fig. 1.
KAMIR risk score predicting 1-yr death from acute myocardial infarction. LVEF, left ventricular ejection fraction.
Table 2.
Model performance in validation cohort
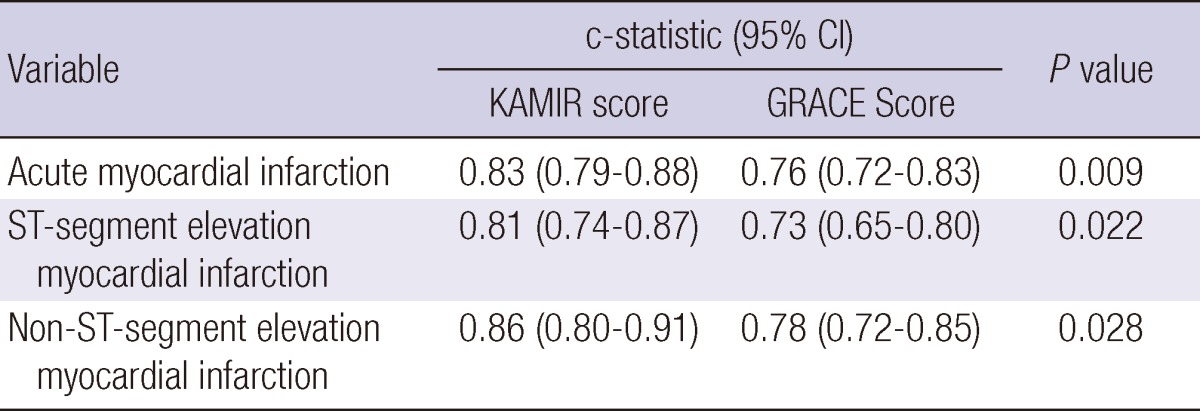
GRACE, Global Registry of Acute Coronary Events; KAMIR, Korea Acute Myocardial Infarction registry.
TREATMENT STRATEGY
Pharmacologic strategy
Clopidogrel
A 600 mg loading doses of clopidogrel double bolus led to greater platelet inhibition than 300 mg standard loading doses in stable angina and non ST-segment elevation MI (NSTEMI) undergoing PCI (24). The Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONSAMI) trial reported that a 600 mg loading dose of clopidogrel may safely reduce 30 day ischemic adverse events rates compared with a 300 mg loading dose in patients with ST-segment elevation MI (STEMI) undergoing primary PCI (25). However, most of the data about the loading doses of clopidogrel came from the Western patients. Because of relatively smaller body weight, different degree of platelet aggregation, and possible ethnic differences in clopidogrel response, the optimal clopidogrel loading dose in Asian patients may not be same as that in Western patients. Bleeding and vascular complications, in-hospital and 1 yr clinical outcomes were compared between a standard loading dose group (300 mg; n = 1,447) and a high dose loading dose group (600 mg; n = 1,217) using KAMIR data (26). There were no differences in bleeding and vascular complications and in 1- and 12-month clinical outcomes even after the propensity score-matched analysis, suggesting that the standard loading dose of clopidogrel may be as safe and similarly effective as the high loading dose in Asian STEMI patients undergoing primary PCI.
Dual antiplatelet therapy (aspirin plus clopidogrel) for at least 12 months has been the standard antiplatelet therapy after DES implantation for the fear of stent thrombosis. Cilostazol emerged as alternative antiplatelet therapy having 10 to 30 times more potent antiplatelet action than that of aspirin. However, clinical outcomes after adding cilostazol to standard dual antiplatelet therapy remained unclear. Chen et al. compared clinical outcomes between triple antiplatelet therapy (aspirin plus clopidogrel plus cilostazol) and dual antiplatelet therapy (aspirin plus clopidogrel) in patients STEMI undergoing primary PCI (27). Triple antiplatelet therapy had lower incidence of in-hospital mortality (adjusted odds ratio [OR], 0.59; 95% CI, 0.36-0.94; P = 0.026) and 8-month mortality (adjusted OR, 0.60; 95% CI, 0.41-0.89; P=0.010) than dual antiplatelet therapy with no difference in the incidence of major bleeding, suggesting superiority of triple antiplatelet therapy over dual antiplatelet therapy in STEMI patients undergoing primary PCI with DES.
Statin
Statin clearly reduces the risk of death and cardiovascular events in both the primary setting and acute coronary syndrome. Current guidelines provide recommendation for initiating statin therapy for targeting optional therapeutic goal for low density lipoprotein cholesterol (LDL-C) less than 70 mg/dL in patients at high risk of cardiovascular events. However, whether to treat very high risk patients with statin who have already baseline LDL-C levels below 70 mg/dL remains troublesome. Clinical outcomes were compared between statin group (n=607) and non-statin group (n=447) in AMI patients with baseline LDL-C levels below 70 mg/dL (28). Statin therapy reduced 1 yr MACEs (adjusted HR, 0.56; 95% CI, 0.34-0.89; P=0.015) mainly due to the risk reduction of cardiac death (HR, 0.45; 95% CI, 0.23-0.93; P=0.031) and coronary revascularization (HR, 0.45; 95% CI, 0.24-0.85; P=0.013). Statin might improve clinical outcomes even in patients with very low LDL-C levels.
PERCUTANEOUS CORONARY INTERVENTION
PCI has become the pivotal step in the management of AMI. KAMIR data showed that primary PCI was done in 75% of STEMI patients, and early invasive strategy was done in 48.5% NSTEMI patients. The rate of receiving reperfusion therapy among eligible STEMI patients also seemed to be higher than the previous reports. Primary PCI was performed in 29% eligible STEMI patients from the data of the National Registry of Myocardial Infarction (NRMI) in the USA (29) and in 27% from the Register of Information and Knowledge about Swedish Heart Intensive Care Admissions (RIKS-HIA) in Sweden (30). Moreover, the median door-to-balloon time was 90 min, which means that one-half of patients undergoing primary PCI received reperfusion in recommended time in KAMIR. From the data in NRMI-3 and -4, fewer than one-half of patients with STEMI received reperfusion in the recommended door-to-balloon time, and the mean door-to-balloon time was 108 min (95% CI, 160.5-109.4 min) (31). The growing interest in primary PCI and easy accessibility to the large-volume hospitals capable of performing PCI, most of which participated in the KAMIR, may account for the higher performance of primary PCI in KAMIR than in those reports.
Thrombolytic therapy is the treatment of choice for patients with STEMI when primary PCI is not available within 90 min. However, the best subsequent management of patients after thrombolytic therapy is unclear. Sim et al. evaluated the effect and optimal time of elective PCI after successful thrombolytic therapy (32). MACEs rates were significantly lower in patients who underwent PCI within 48 hr of thrombolytic therapy compared with those who underwent PCI later (4.1% vs 14.9%, P = 0.026) without no differences in hospital complications. In conclusion, early elective PCI within 48 hr of successful thrombolytic therapy for AMI might be safe and beneficial compared with PCI performed later.
Initial treatment strategy in non ST-segment elevation myocardial infarction
Recent studies indicate that early invasive strategy for high-risk patients with NSTEMI yields improved outcomes compared with early conservative strategy (33). In terms of overall population, KAMIR also showed better short-term and long-term clinical outcomes in patients with early invasive strategy (within 48 hr PCI) than late invasive strategy (34). However, when NSTEMI patients were categorized based on TIMI risk score, there was no significant difference of long term clinical outcomes in patients with low to moderate TIMI risk score, whereas significant difference in patients with high TIMI risk score (≥5 points) (34). Also, in NSTEMI patients with severe chronic kidney disease (CKD) (glomerular filtration rate [GFR] <30 mL/min/1.73 m2), early invasive strategy did not reduce 1 yr mortality compared with conservative treatment (35). Contrary, in NSTEMI patients with mild (60-89 mL/min/1.73 m2) to moderate (30-59 mL/min/1.73 m2) CKD patients had mortality benefit with early invasive treatment. Furthermore, early invasive strategy (within 24 hr PCI) was superior to the deferred invasive strategy (after 24 hr PCI) in patients with mild CKD. In the timing of an invasive strategy in patients with NSTEMI, KAMIR suggested early invasive strategy might improve clinical outcomes compared with early conservative treatment. However, risk stratification should be prior to the selection of initial treatment strategy.
Comparison of the efficacy and safety of drug eluting stents vs bare metal stents
DES has caused drastic changes in interventional cardiology. The recent guidelines also recommend to use DES as alternative to bare-metal stent (BMS) for primary PCI in STEMI. The DES penetration rate was 91% in both patients with STEMI and NSTEMI in KAMIR. That in KAMIR is notably higher than in that in other registry reports (2, 3, 36, 37), representing unique characteristic in Korean PCI practice as well as contemporary trends in PCI (Table 3).
Table 3.
Comparison of characteristics of the trials
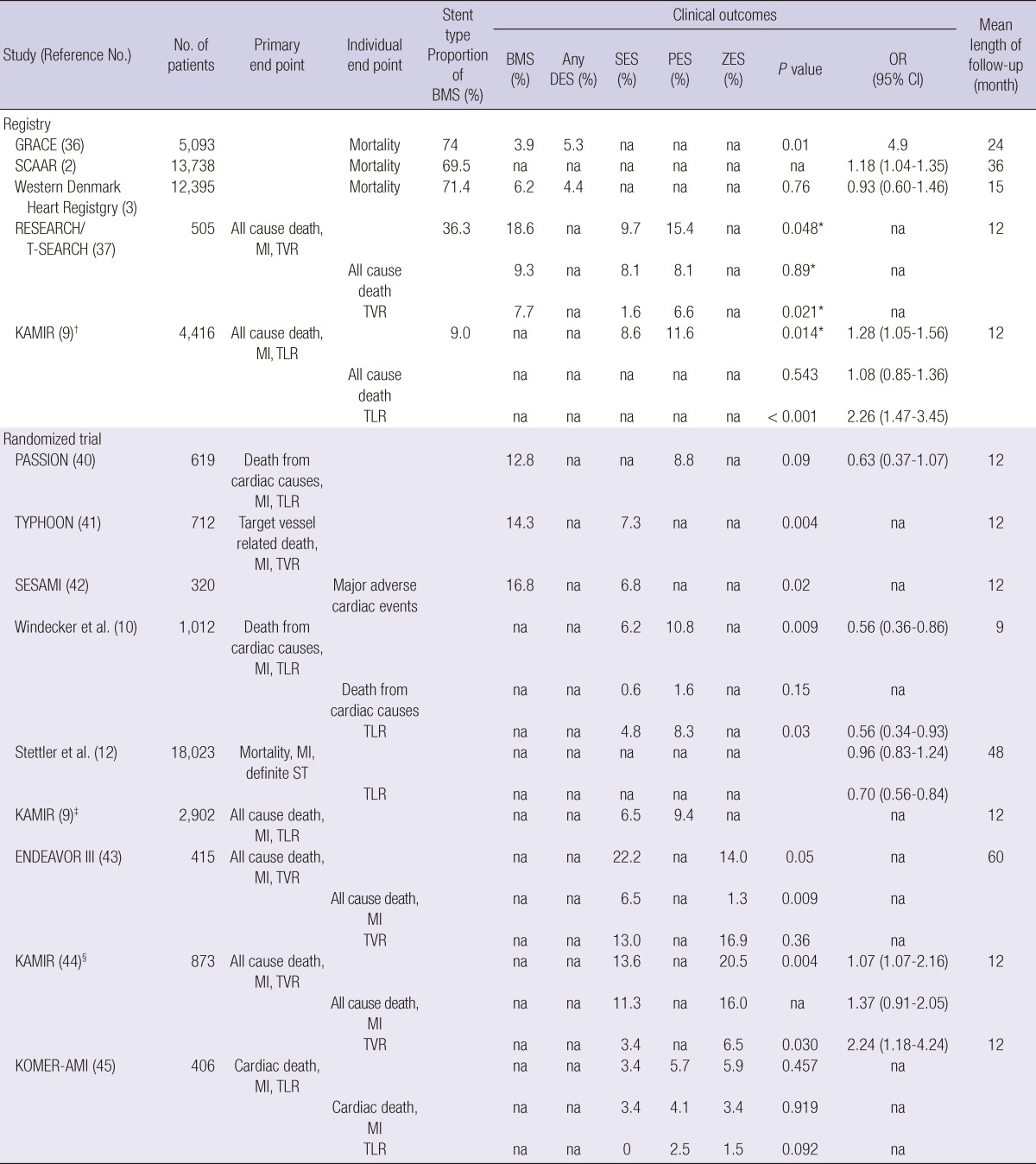
*P value: sirolimus eluting stent vs paclitaxel eluting stent; †KAMIR, before propensity score matching; ††KAMIR, after propensity score matching comparing the clinical outcomes in patients with sirolimus eluting stent and in patients with paclitaxel eluting stent; §KAMIR, comparing the clinical outcomes in patients with sirolimus eluting stent and in patients with zotarolimus eluting stent. BMS, bare metal stent; DES, drug eluting stent; ENDEAVOR, Randomized Comparison of Zotarolimus-Eluting and Paclitaxel-Eluting Stents in Patients with Coronary Artery Disease; GRACE, Global Registry of Acute Coronary Events; KAMIR, Korea Acute Myocardial Infarction Registry; KOMER-AMI, Korean Multicentre Endeavor-Acute Myocardial Infarction; MI, myocardial infarction; na; non-available; OR, odds ratio; PASSION, Paclitaxel-Eluting Stent Versus Conventional Stent in Myocardial Infarction with ST-segment Elevation trial; PES, paclitaxel eluting stent; RESEARCH/T-SEARCH, Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital (RESEARCH) and Taxus-Stent Evaluated at Rotterdam Cardiology Hospital (T-SEARCH) registry; SCAAR, Swedish Coronary Angiography and Angioplasty Registry; SESAMI, Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction; TLR, target lesion revascularization; TVR, target vessel revascularization; TYPHOON, Trial to Assess the Use of the Cypher Stent in Acute Myocardial Infarction Treated with Balloon Angioplasty; SES, sirolimus eluting stent; ZES, zotarolimus eluting stent.
In various subsets among AMI patients, comparison between BMS and DES or among DES subclass was made using KAMIR data. Sim et al. compared clinical outcomes of BMS vs DES in large coronary arteries (≥3.5 mm) with lesions <25 mm in 985 AMI patients undergoing PCI (38). During 1 yr follow-up, the rates of target lesion revascularization (TLR) and target vessel revascularization (TVR) were lower in the DES group (2.5% vs 5.9%, P=0.032 and 3.1% vs 5.9%, P=0.041) than BMS group with no difference in the rate of death or MI and MACEs, suggesting usefulness of DES in large vessels in AMI patients over BMS without compromising overall safety. Bae et al. compared clinical outcomes of BMS vs DES in 2,175 AMI patients with CKD (GFR <60 mL/min) (39). One year MACEs were significantly higher in the BMS group (44% vs 26%, P<0.05) than DES group which was mainly due to death rather than repeat intervention (44% vs 26%, P<0.05). They concluded that DES implantation exhibits a favorable 1-yr clinical outcome than BMS implantation in AMI patients with CKD.
Comparison of the efficacy and safety among drug eluting stents
With regard to first generation DES, KAMIR investigators (9) reported that the patients with SES had a lower risk for repeated revascularization compared with patients receiving PES, similar to randomized trials (10, 11) and collaborative network meta-analysis comprising 40 randomized trials (12). Also, Korean AMI patients showed similar 1 yr clinical outcomes compared with those trials (Table 3) (10, 11, 40-42). With regard to comparison between first generation DES and second generation DES, KAMIR showed different results from other trials (Table 3). The Randomized Comparison of Zotarolimus-Eluting and Paclitaxel-Eluting Stents in Patients with Coronary Artery Disease (ENDEAVOR III) trial showed significant lower MACEs in zotarolimus (ZES) implanted patients compared with SES implantation patients (14.0% vs 22.2%, P=0.05), mainly driven by the risk reduction of hard end-point (death, MI) with no difference in TVR rate (43). In contrast, KAMIR showed significant lower MACEs in SES implanted patients compared with ZES implantation patients (13.6% vs 20.5%, P=0.004), mainly driven by the risk reduction of TVR with no difference in the rate of hard end-point (death, MI) (44). This difference was supported by the Korean Multicentre Endeavor (KOMER)-AMI trial (45), randomized trial in Korea to evaluate the efficacy and safety of ZES, SES, PES. KOMER-AMI trial showed that a trend towards a lower rate of TLR in SES implanted patients than ZES implanted patients (0% vs 1.5%, P=0.092) with no difference in hard end-point (cardiac death, MI). This difference suggested that clinical outcomes treated with second generation DES in Asians might act in a different manner compared with western population, whereas those treated with first generation DES were similar to other trials. Therefore, further trials are needed to clarify universal clinical outcomes about second generation DES, taking into consideration of racial differences.
CONCLUSION
KAMIR revealed numerous unknown characteristics and results in Korean AMI patients. Korean AMI patients had similar clinical risk factors and outcomes compared with western AMI patients. However, Korean AMI patients had higher prevalence of diabetes mellitus and lower BMI contrary to western AMI patients. KAMIR score was easy and accurate for the prediction of adverse clinical outcomes. KAMIR also suggested new treatment strategy in Asian AMI patients. Standard loading dose of clopidogrel was enough for Asian AMI patients, and statin improved clinical outcomes even in patients with very low LDL-C levels. ZES, the 2nd generation DES, was not superior to SES or PES, the 1st generation DES. KAMIR has several limitations, such as retrospective analysis design and weak clinical follow-up parameters. KorMI, as the sequent study of KAMIR, reinforced these weak points and is expected to get better results with more than 38,000 enrolled AMI patients. In conclusion, KAMIR made a cornerstone in the study of Korean AMI, has been evolving itself to overcome the pitfall of KAMIR, and expected to be new standards of care for Asian AMI.
Footnotes
KAMIR was carried out with the support of the Korean Circulation Society (KCS) in the memorandum of the 50th anniversary KCS. This study was supported by a grant of the Korea Healthcare technology R&D project, Ministry for Health, Welfare and Family Affairs (A084869), Korea.
References
- 1.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG, Flather MD, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 2.Lagerqvist B, James SK, Stenestrand U, Lindbäck J, Nilsson T, Wallentin L. Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med. 2007;356:1009–1019. doi: 10.1056/NEJMoa067722. [DOI] [PubMed] [Google Scholar]
- 3.Jensen LO, Maeng M, Kaltoft A, Thayssen P, Hansen HH, Bottcher M, Lassen JF, Krussel LR, Rasmussen K, Hansen KN, et al. Stent thrombosis, myocardial infarction, and death after drug-eluting and bare-metal stent coronary interventions. J Am Coll Cardiol. 2007;50:463–470. doi: 10.1016/j.jacc.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Fazel R, Krumholz HM, Bates ER, French WJ, Frederick PD, Nallamothu BK. Choice of reperfusion strategy at hospitals with primary percutaneous coronary intervention: a National Registry of Myocardial Infarction analysis. Circulation. 2009;120:2455–2461. doi: 10.1161/CIRCULATIONAHA.109.860544. [DOI] [PubMed] [Google Scholar]
- 5.Okura N, Ogawa H, Katoh J, Yamauchi T, Hagiwara N. Long-term prognosis of patients with acute myocardial infarction in the era of acute revascularization (from the Heart Institute of Japan Acute Myocardial Infarction [HIJAMI] registry) Int J Cardiol. 2012;159:205–210. doi: 10.1016/j.ijcard.2011.02.072. [DOI] [PubMed] [Google Scholar]
- 6.Abbud ZA, Shindler DM, Wilson AC, Kostis JB Myocardial Infarction Data Acquisition System Study Group. Effect of diabetes mellitus on short- and long-term mortality rates of patients with acute myocardial infarction: a statewide study. Am Heart J. 1995;130:51–58. doi: 10.1016/0002-8703(95)90235-x. [DOI] [PubMed] [Google Scholar]
- 7.Lee MG, Jeong MH, Ahn Y, Chae SC, Hur SH, Hong TJ, Kim YJ, Seong IW, Chae JK, Rhew JY, et al. Comparison of clinical outcomes following acute myocardial infarctions in hypertensive patients with or without diabetes. Korean Circ J. 2009;39:243–250. doi: 10.4070/kcj.2009.39.6.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim CS, Choi JS, Park JW, Bae EH, Ma SK, Jeong MH, Kim YJ, Cho MC, Kim CJ, Kim SW. Concomitant renal insufficiency and diabetes mellitus as prognostic factors for acute myocardial infarction. Cardiovasc Diabetol. 2011;10:95. doi: 10.1186/1475-2840-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho Y, Yang HM, Park KW, Chung WY, Choi DJ, Seo WW, Jeong KT, Chae SC, Lee MY, Hur SH, et al. Paclitaxel-versus sirolimus-eluting stents for treatment of ST-segment elevation myocardial infarction: with analyses for diabetic and nondiabetic subpopulation. JACC Cardiovasc Interv. 2010;3:498–506. doi: 10.1016/j.jcin.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Windecker S, Remondino A, Eberli FR, Jüni P, Räber L, Wenaweser P, Togni M, Billinger M, Tüller D, Seiler C, et al. Sirolimus-eluting and paclitaxel-eluting stents for coronary revascularization. N Engl J Med. 2005;353:653–662. doi: 10.1056/NEJMoa051175. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Park SW, Lee SW, Park DW, Yun SC, Lee CW, Hong MK, Kim HS, Ko JK, Park JH, et al. Sirolimus-eluting stent versus paclitaxel-eluting stent for patients with long coronary artery disease. Circulation. 2006;114:2148–2153. doi: 10.1161/CIRCULATIONAHA.106.666396. [DOI] [PubMed] [Google Scholar]
- 12.Stettler C, Wandel S, Allemann S, Kastrati A, Morice MC, Schömig A, Pfisterer ME, Stone GW, Leon MB, de Lezo JS, et al. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007;370:937–948. doi: 10.1016/S0140-6736(07)61444-5. [DOI] [PubMed] [Google Scholar]
- 13.Kang WY, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, et al. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol. 2010;55:84–91. doi: 10.1016/j.jjcc.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Park JS, Kim W, Shin DG, Kim YJ, Kim DS, Choi DJ, Han KR, Kim CJ, Cho MC, et al. Impact of body mass index and waist-to-hip ratio on clinical outcomes in patients with ST-segment elevation acute myocardial infarction (from the Korean Acute Myocardial Infarction Registry) Am J Cardiol. 2008;102:957–965. doi: 10.1016/j.amjcard.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 15.Chandra NC, Ziegelstein RC, Rogers WJ, Tiefenbrunn AJ, Gore JM, French WJ, Rubison M. Observations of the treatment of women in the United States with myocardial infarction: a report from the National Registry of Myocardial Infarction-I. Arch Intern Med. 1998;158:981–988. doi: 10.1001/archinte.158.9.981. [DOI] [PubMed] [Google Scholar]
- 16.Tamis-Holland JE, Palazzo A, Stebbins AL, Slater JN, Boland J, Ellis SG, Hochman JS. Benefits of direct angioplasty for women and men with acute myocardial infarction: results of the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes Angioplasty (GUSTO II-B) Angioplasty Substudy. Am Heart J. 2004;147:133–139. doi: 10.1016/j.ahj.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Park JS, Kim YJ, Shin DG, Jeong MH, Ahn YK, Chung WS, Seung KB, Kim CJ, Cho MC, Jang YS, et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: from the Korean Acute Myocardial Infarction Registry (KAMIR) study. Clin Cardiol. 2010;33:E1–E6. doi: 10.1002/clc.20557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woo JS, Kim W, Ha SJ, Kim SJ, Kang WY, Jeong MH. Impact of gender differences on long-term outcomes after successful percutaneous coronary intervention in patients with acute myocardial infarction. Int J Cardiol. 2010;145:516–518. doi: 10.1016/j.ijcard.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 19.Kang SH, Suh JW, Yoon CH, Cho MC, Kim YJ, Chae SC, Yoon JH, Gwon HC, Han KR, Kim JH, et al. Sex differences in management and mortality of patients with ST-elevation myocardial infarction (from the Korean Acute Myocardial Infarction National Registry) Am J Cardiol. 2012;109:787–793. doi: 10.1016/j.amjcard.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Lee KH, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi D, et al. Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol. 2008;130:227–234. doi: 10.1016/j.ijcard.2007.08.044. [DOI] [PubMed] [Google Scholar]
- 21.Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, Mautner B, Corbalan R, Radley D, Braunwald E. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 22.Kim HK, Jeong MH, Ahn Y, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, et al. A new risk score system for the assessment of clinical outcomes in patients with non-ST-segment elevation myocardial infarction. Int J Cardiol. 2010;145:450–454. doi: 10.1016/j.ijcard.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Kim HK, Jeong MH, Ahn Y, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, et al. Hospital discharge risk score system for the assessment of clinical outcomes in patients with acute myocardial infarction (Korea Acute Myocardial Infarction Registry [KAMIR] score) Am J Cardiol. 2011;107:965–971. doi: 10.1016/j.amjcard.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 24.L'Allier PL, Ducrocq G, Pranno N, Noble S, Ibrahim R, Grégoire JC, Azzari F, Nozza A, Berry C, Doucet S, et al. Clopidogrel 600-mg double loading dose achieves stronger platelet inhibition than conventional regimens: results from the PREPAIR randomized study. J Am Coll Cardiol. 2008;51:1066–1072. doi: 10.1016/j.jacc.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 25.Dangas G, Mehran R, Guagliumi G, Caixeta A, Witzenbichler B, Aoki J, Peruga JZ, Brodie BR, Dudek D, Kornowski R, et al. Role of clopidogrel loading dose in patients with ST-segment elevation myocardial infarction undergoing primary angioplasty: results from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. J Am Coll Cardiol. 2009;54:1438–1446. doi: 10.1016/j.jacc.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 26.Choi CU, Rha SW, Oh DJ, Poddar KL, Na JO, Kim JW, Lim HE, Kim EJ, Park CG, Seo HS, et al. Standard versus high loading doses of clopidogrel in Asian ST-segment elevation myocardial infarction patients undergoing percutaneous coronary intervention: insights from the Korea Acute Myocardial Infarction Registry. Am Heart J. 2011;161:373–382. doi: 10.1016/j.ahj.2010.10.031. [DOI] [PubMed] [Google Scholar]
- 27.Chen KY, Rha SW, Li YJ, Poddar KL, Jin Z, Minami Y, Wang L, Kim EJ, Park CG, Seo HS, et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation. 2009;119:3207–3214. doi: 10.1161/CIRCULATIONAHA.108.822791. [DOI] [PubMed] [Google Scholar]
- 28.Lee KH, Jeong MH, Kim HM, Ahn Y, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, et al. Benefit of early statin therapy in patients with acute myocardial infarction who have extremely low low-density lipoprotein cholesterol. J Am Coll Cardiol. 2011;58:1664–1671. doi: 10.1016/j.jacc.2011.05.057. [DOI] [PubMed] [Google Scholar]
- 29.Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, Cutlip DE, Bates ER, Frederick PD, Miller DP, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation. 2006;114:2019–2025. doi: 10.1161/CIRCULATIONAHA.106.638353. [DOI] [PubMed] [Google Scholar]
- 30.Stenestrand U, Lindbäck J, Wallentin L. Long-term outcome of primary percutaneous coronary intervention vs prehospital and in-hospital thrombolysis for patients with ST-elevation myocardial infarction. JAMA. 2006;296:1749–1756. doi: 10.1001/jama.296.14.1749. [DOI] [PubMed] [Google Scholar]
- 31.McNamara RL, Herrin J, Bradley EH, Portnay EL, Curtis JP, Wang Y, Magid DJ, Blaney M, Krumholz HM. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol. 2006;47:45–51. doi: 10.1016/j.jacc.2005.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sim DS, Jeong MH, Ahn Y, Kim YJ, Chae SC, Hong TJ, Seong IW, Chae JK, Kim CJ, Cho MC, et al. Safety and benefit of early elective percutaneous coronary intervention after successful thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 2009;103:1333–1338. doi: 10.1016/j.amjcard.2009.01.339. [DOI] [PubMed] [Google Scholar]
- 33.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 34.Jeong HC, Ahn Y, Jeong MH, Chae SC, Hur SH, Hong TJ, Kim YJ, Seong IW, Chae JK, Rhew JY, et al. Long-term clinical outcomes according to initial management and thrombolysis in myocardial infarction risk score in patients with acute non-ST-segment elevation myocardial infarction. Yonsei Med J. 2010;51:58–68. doi: 10.3349/ymj.2010.51.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hachinohe D, Jeong MH, Saito S, Ahmed K, Hwang SH, Lee MG, Sim DS, Park KH, Kim JH, Hong YJ, et al. Management of non-ST-segment elevation acute myocardial infarction in patients with chronic kidney disease (from the Korea Acute Myocardial Infarction Registry) Am J Cardiol. 2011;108:206–213. doi: 10.1016/j.amjcard.2011.03.025. [DOI] [PubMed] [Google Scholar]
- 36.Steg PG, Fox KA, Eagle KA, Furman M, Van de Werf F, Montalescot G, Goodman SG, Avezum A, Huang W, Gore JM. Mortality following placement of drug-eluting and bare-metal stents for ST-segment elevation acute myocardial infarction in the Global Registry of Acute Coronary Events. Eur Heart J. 2009;30:321–329. doi: 10.1093/eurheartj/ehn604. [DOI] [PubMed] [Google Scholar]
- 37.Daemen J, Tanimoto S, Garcia-Garcia HM, Kukreja N, van de Sande M, Sianos G, de Jaegere PP, van Domburg RT, Serruys PW. Comparison of three-year clinical outcome of sirolimus- and paclitaxel-eluting stents versus bare metal stents in patients with ST-segment elevation myocardial infarction (from the RESEARCH and T-SEARCH Registries) Am J Cardiol. 2007;99:1027–1032. doi: 10.1016/j.amjcard.2006.11.070. [DOI] [PubMed] [Google Scholar]
- 38.Sim DS, Jeong MH, Ahn Y, Kim YJ, Chae SC, Hong TJ, Seong IW, Chae JK, Kim CJ, Cho MC, et al. Effectiveness of drug-eluting stents versus bare-metal stents in large coronary arteries in patients with acute myocardial infarction. J Korean Med Sci. 2011;26:521–527. doi: 10.3346/jkms.2011.26.4.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bae EH, Lim SY, Choi YH, Suh SH, Cho KH, Choi JS, Kim CS, Park JW, Ma SK, Jeong MH, et al. Drug-eluting vs. bare-metal stents for treatment of acute myocardial infarction with renal insufficiency. Circ J. 2011;75:2798–2804. doi: 10.1253/circj.cj-11-0586. [DOI] [PubMed] [Google Scholar]
- 40.Laarman GJ, Suttorp MJ, Dirksen MT, van Heerebeek L, Kiemeneij F, Slagboom T, van der Wieken LR, Tijssen JG, Rensing BJ, Patterson M. Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention. N Engl J Med. 2006;355:1105–1113. doi: 10.1056/NEJMoa062598. [DOI] [PubMed] [Google Scholar]
- 41.Spaulding C, Henry P, Teiger E, Beatt K, Bramucci E, Carrié D, Slama MS, Merkely B, Erglis A, Margheri M, et al. Sirolimus-eluting versus uncoated stents in acute myocardial infarction. N Engl J Med. 2006;355:1093–1104. doi: 10.1056/NEJMoa062006. [DOI] [PubMed] [Google Scholar]
- 42.Menichelli M, Parma A, Pucci E, Fiorilli R, De Felice F, Nazzaro M, Giulivi A, Alborino D, Azzellino A, Violini R. Randomized trial of sirolimus-eluting stent versus bare-metal stent in acute myocardial infarction (SESAMI) J Am Coll Cardiol. 2007;49:1924–1930. doi: 10.1016/j.jacc.2007.01.081. [DOI] [PubMed] [Google Scholar]
- 43.Kandzari DE, Mauri L, Popma JJ, Turco MA, Gurbel PA, Fitzgerald PJ, Leon MB. Late-term clinical outcomes with zotarolimus- and sirolimus-eluting stents. 5-year follow-up of the ENDEAVOR III (A Randomized Controlled Trial of the Medtronic Endeavor Drug [ABT-578] Eluting Coronary Stent System Versus the Cypher Sirolimus-Eluting Coronary Stent System in De Novo Native Coronary Artery Lesions) JACC Cardiovasc Interv. 2011;4:543–550. doi: 10.1016/j.jcin.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 44.Kim HK, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, et al. Comparison of outcomes between Zotarolimus-and sirolimus-eluting stents in patients with ST-segment elevation acute myocardial infarction. Am J Cardiol. 2010;105:813–818. doi: 10.1016/j.amjcard.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 45.Kang WC, Ahn T, Lee K, Han SH, Shin EK, Jeong MH, Yoon JH, Park JS, Bae JH, Hur SH, et al. Comparison of zotarolimus-eluting stents versus sirolimus-eluting stents versus paclitaxel-eluting stents for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: results from the Korean Multicentre Endeavor (KOMER) acute myocardial infarction (AMI) trial. EuroIntervention. 2011;7:936–943. doi: 10.4244/EIJV7I8A148. [DOI] [PubMed] [Google Scholar]