Abstract
Alcoholism is becoming one of the most serious issues in Korea. The purpose of this review article was to understand the present status of the treatment system for alcoholism in Korea compared to the United States and to suggest its developmental direction in Korea. Current modalities of alcoholism treatment in Korea including withdrawal treatment, pharmacotherapy, and psychosocial treatment are available according to Korean evidence-based treatment guidelines. Benzodiazepines and supportive care including vitamin and nutritional support are mainly used to treat alcohol withdrawal in Korea. Naltrexone and acamprosate are the drugs of first choice to treat chronic alcoholism. Psychosocial treatment methods such as individual psychotherapy, group psychotherapy, family therapy, cognitive behavior therapy, cue exposure therapy, 12-step facilitation therapy, self-help group therapy, and community-based treatment have been carried out to treat chronic alcoholism in Korea. However, current alcohol treatment system in Korea is not integrative compared to that in the United States. To establish the treatment system, it is important to set up an independent governmental administration on alcohol abuse, to secure experts on alcoholism, and to conduct outpatient alcoholism treatment programs and facilities in an open system including some form of continuing care.
Keywords: Alcoholism, Treatment system, Korea, United States
INTRODUCTION
Alcoholism is becoming one of the most serious issues in Korea, and alcohol consumption and its prevalence is higher in Korea than in the United States (Table 1). The Organization for Economic Co-operation and Development (OECD) Health data 2011 (1) reported that Korean adult (age 15 yr and above) per capita consumption of alcohol were 9.2 L in 2006, 9.3 L in 2007, and 9.5 L in 2008, which were higher consumption rates than those of United States (8.6 L in 2006, 8.7 L in 2007, and 8.8 L in 2008).
Table 1.
Comparison of current situation of alcoholism between Korea and the United States
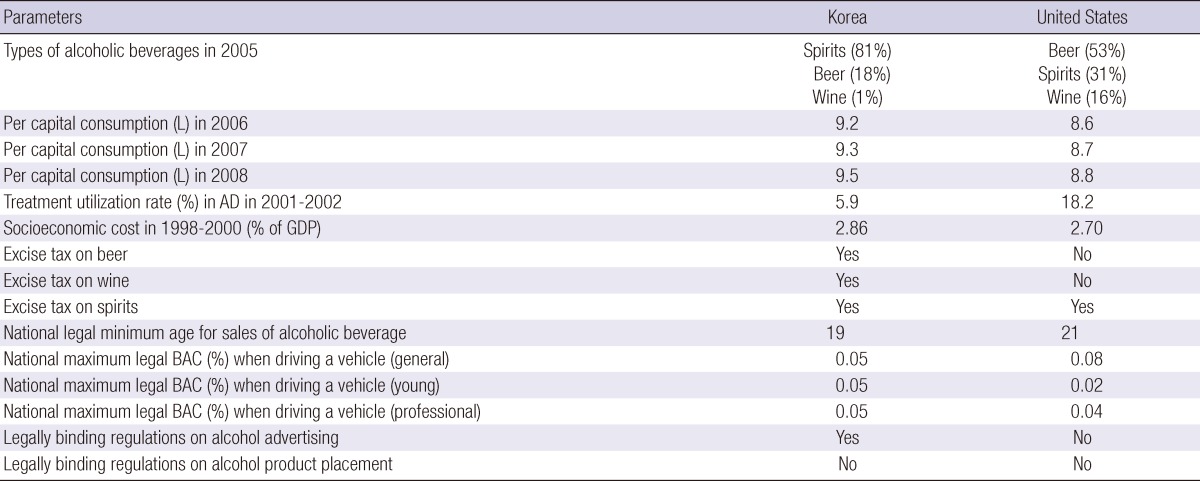
AD, alcohol dependence; GDP, Gross Domestic Product; BAC, Blood Alcohol Concentration.
Alcoholism is associated with a high relapse and socioeconomic burden in Korea. The 2011 National Epidemiological Survey of Psychiatric Illnesses in Korea (2) revealed the rates of life time prevalence of alcohol use disorders/ alcohol abuse/alcohol dependence to be 13.4/8.0/5.3% (total), 20.7/13.0/7.6% (males), and 6.1/3.1/3.1% (females). This epidemiological survey (2) also found that the rates of 1-yr prevalence of alcohol use disorders/alcohol abuse/ alcohol dependence were 4.4/2.1/2.2% (total), 6.6/3.4/3.2% (males), and 2.1/0.9/1.2% (females). Furthermore, the survey suggested that the availability of mental health services related to alcohol use disorders was lower than those related to other psychiatric disorders (alcohol use disorders 8.6%; psychosis 25.0%, mood disorder 37.7%, anxiety disorder 25.1%, and total psychiatric disorder 15.3%), although there was a high prevalence of alcohol use disorders in Korea. A cross-national comparison study (3) compared the 1-yr prevalence rates of alcohol dependence and treatment utilization conducted in 2001-2002 in Korea (the Korean Epidemiologic Catchment Area survey) with the rates in the United States (the National Epidemiologic Survey on Alcohol and Related Conditions). These contemporary national surveys showed that alcohol-dependent Koreans (5.9%) were 3.93 times less likely seek treatment compared to their Americans counterparts (18.2%) whereas prevalence of alcohol dependence was higher in Korea (5.1%) compared with the United States (4.4%).
The Korean socioeconomic costs of alcohol drinking in 2000 (4) were estimated to be 14.9 trillion KRW (2.86% of GDP), which included 0.91 trillion KRW for direct costs (6.09% of the cost), 6.28 trillion KRW for reduction and loss of productivity (42.08%), 4.47 trillion KRW for loss of the workforce (29.92%), and 3.77 trillion KRW for other costs (21.91%). When the ratio of costs to GDP between Korea and the Unites States were compared (5), Korea had higher socioeconomic costs than the United States (2.86% of GDP in Korea, 2000; 2.70% of GDP in the United States, 1998).
The purpose of this review was to understand the present status of the treatment system for alcoholism compared to the United States and to suggest its developmental direction in Korea.
We searched national epidemiologic research reports (available at http://kostat.go.kr or http://stat.mw.go.kr), the NCBI PubMed database (available at http://www.ncbi.nlm.nih.gov), and the Korean Medical Database (available at http://kmbase.medric.or.kr) within the last 10 yr (2001 to 2011) using the key words: alcoholism, prevalence, treatment system, Korea, and the United States. In some cases, earlier studies from the reference lists of relevant papers (1981 to 2000) and internet websites were reviewed.
CURRENT TREATMENT MODALITIES OF ALCOHOLISM IN KOREA
Modalities of alcoholism treatment in Korea include withdrawal treatment, detoxification, education, behavioral approaches, psychotherapy (PT), pharmacotherapy, individual therapy, and group therapy including Alcoholics Anonymous (AA) according to the severity of the disorder, availability of facilities, motivation and patient's or family's choice (Table 2).
Table 2.
Comparison of current treatment modalities of alcoholism between Korea and the United States
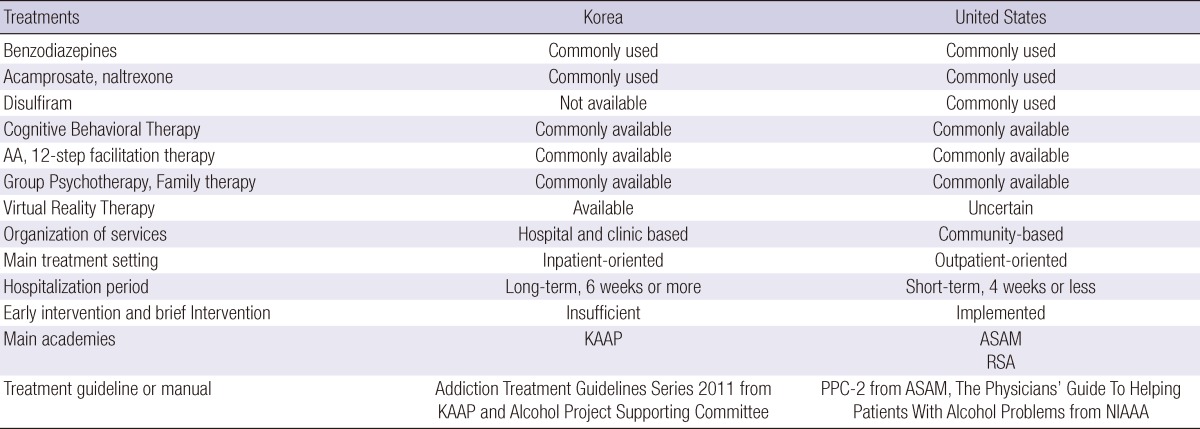
AA, Alcoholics Anonymous; KAAP, Korean Academy of Addiction Psychiatry; ASAM, American Society of Addiction Medicine; RSA, Research Society on Alcoholism; PPC-2, Patient Placement Criteria for treatment of psychoactive substance use disorder; NIAAA, National Institute on Alcohol Abuse and Alcoholism.
A consensus on the status of alcoholism treatment in Korea has been reached primarily by the Korean Academy of Addiction Psychiatry (KAAP) from presentations at conferences, questionnaire surveys, and discussions among experts. Based on the highlights of such consensus that there is a need for standardized and evidence-based treatment methods, the KAAP and the Alcohol Project Supporting Committee (APSC) established treatment guidelines in 2011 (6). In this section, current treatment modalities of alcoholism based on the treatment guidelines and the consensus of experts in Korea (6, 7) is described.
The treatment of alcohol withdrawal
Korean clinicians assess risks of alcohol withdrawal by evaluating the patient's current drinking pattern, the presence of withdrawal symptoms, use of other related substances, and the presence of comorbid physical or psychiatric disorders. Then if needed, pharmacotherapy is recommended in an outpatient clinic or in an inpatient ward.
Benzodiazepines such as chlordiazepoxide and lorazepam are mainly used to treat alcohol withdrawal in Korea. Particularly for elderly patients or patients with severe liver diseases, recent brain damage, respiratory failure, or undetermined physical conditions, lorazepam is primarily used. Administration regimens include symptom-triggered therapy, loading dose therapy, and fixed-schedule therapy. For severe withdrawal cases, 6-12 mg of lorazepam is orally administered daily and maximally 20 mg per day. Generally, after the resolution of withdrawal symptoms, benzodiazepines are reduced and subsequently terminated. It may be used as a prophylactic agent for alcohol withdrawal in Korea.
For all patients experiencing withdrawal, in order to prevent Wernicke Korsakoff syndrome, 100-300 mg of thiamine is administered orally prior to the administration of carbohydrates. For cases of poor food intake, in addition to oral administration, thiamine may be injected intramuscularly; but for patients with blood coagulation diseases, intramuscular injection is avoided. Thiamine is administered for approximately 1-3 months and terminated. Nonetheless, continuous oral administration may be recommended for cases of continuous drinking. In addition, supportive care such as correction of dehydration and electrolyte imbalance, environmental support (to minimize stimulation and reduce anxiety), vitamin and nutritional support, and supportive PT, may be administered.
Anticonvulsant agents are not recommended for the prevention of withdrawal symptoms, and are generally not used in addition to benzodiazepines. Nonetheless, for the patients who are being treated for seizure disorder or bipolar disorder, regardless of the presence of withdrawal symptoms, anticonvulsant agents are maintained.
Antipsychotic agents lower the seizure threshold and thus increase the risk of seizures. Therefore, they are not used alone to treat hallucination, delirium, or anxiety due to alcohol withdrawal. Nonetheless, for patients whose symptoms are unresponsive to sufficient benzodiazepines, antipsychotic agents may be administered in conjunction with benzodiazepines for the treatment of hallucination, delirium, and anxiety induced by alcohol withdrawal.
Pharmacological treatment of chronic alcoholism
The drugs of first choice to treat alcoholism are naltrexone and acamprosate in Korea. For hospitalized patients, medications to treat alcoholism are not required, and it is difficult to evaluate their effectiveness in the setting. The prerequisite to drug treatment is alcohol treatment in an outpatient-based setting. However, drugs may be administered after the detoxification period to assess compliance and the side effects of drugs.
Acamprosate
Acamprosate is a gamma-aminobutyric acid (GABA) agonist and glutamate antagonist. It is most effective for patients with an abstinence goal, rather than preventing excessive drinking in non-abstinent patients. Acamprosate is contraindicated in patients with renal insufficiency or severe hepatic failure. Its main side effects are diarrhea and somnolence. The treatment must be started during the abstinence period. The therapeutic dose is from 1,332 mg to 1,998 mg per day according to the patient's weight. It is recommended that acamprosate should be maintained for a minimum of 6 months to 1 yr in Korea.
Namkoong et al. (8) conducted an 8-week multi-center randomized, double-blind, placebo-controlled study to assess the effectiveness of acamprosate in Korean alcohol dependence. Acamprosate failed to show any treatment advantages over the placebo in the study. This is contradictory to the previous reports (9-11) which proved the effectiveness of acamprosate treatment. The sample characteristics (i.e., a more severe form of alcohol dependence, a lower level of social support, a short interval between the last drink and the first medication), the dosage issues of acamprosate, the short period (8 weeks) of study, and the various concomitant psychosocial treatments, may all explain the negative findings of the study.
Naltrexone
Naltrexone is an opioid antagonist and reduces the rewarding effect of alcohol. It is more effective for preventing relapse to heavy or problem drinking and reducing high levels of alcohol consumption than for maintaining abstinence from alcohol. It is contraindicated for patients with acute hepatitis, severe liver failure, or who are on opioid medication such as codeine, morphine, oxycodone, and methadone. Patients with significant depression or more severe alcohol dependence respond less well to naltrexone. It may be administered after the alcohol withdrawal symptoms, and is safe to use during the drinking period or the withdrawal period. Its side effects are nausea, vomiting, anorexia, headache, dizziness, fatigue, and anxiety. The therapeutic dose of naltrexone is 25-100 mg. It is recommended that naltrexone should be maintained for a minimum of 6 months to 1 yr in Korea.
Namkoong et al. (12) conducted a 10-week open-label study on the drug compliance of naltrexone in 93 Korean outpatients with alcohol dependence. The estimated compliance measured by the Medication Event Monitoring System (MEMS) was observed to be 80.4%±20.6%. The treatment outcome such as percentage of days abstinent, percentage of heavy drinking days, and mean alcohol amount consumed per drinking occasion was consistently correlated with the estimate of compliance.
Kim et al. (13) conducted a 12-week prospective study on the efficacy of naltrexone, and the genotype in 32 Korean subjects with alcohol dependence. The results showed that the time to the first relapse of the Asp40 variant genotype group (G carrier, A/G or G/G) was observed to be significantly longer than that of the Asn40 genotype group (A/A) (hazard ratio [A/A vs G carrier]=13.623, P=0.014). This is the first study reported in Asia, and its results are in accordance with the European studies. Since the frequency of the Asn40 genotype is high among the Asian populations, it is proposed that naltrexone may be an effective treatment for Korean alcohol dependence.
Other medications
Topiramate (14), gabapentin (15), baclofen (16), and aripiprazole (17) may reduce the recurrence of alcohol use disorders. Nevertheless, further studies including randomized controlled trials are required in Korea. They are not recommended as first-choice drugs in Korea.
Psychosocial treatment of chronic alcoholism
Psychosocial interventions or treatments imply non-drug treatments that have been widely applied to treat alcohol use disorders. Psychosocial interventions have been used by diverse therapists in the primary care setting, outpatient clinics, hospitals, residential institutions, and other diverse treatment environments for individual patient or groups.
Psychosocial treatment methods such as individual PT, group therapy (or group PT), family therapy, cognitive behavior therapy (CBT), cue exposure therapy, 12-step facilitation therapy, self-help group therapy, and community-based treatment (via therapeutic communities, crisis interventions, halfway houses, and community residential facilities) have been carried out in Korea. These are carried out primarily in the form of inpatient treatment rather than outpatient treatment in Korea. Among these psychosocial treatments, 12-step facilitation therapy, cognitive behavior therapy, and coping skills training have been primarily used. In addition, when required, parallel drug treatments have been performed.
According to the Korean addiction treatment guidelines, psychosocial intervention including group therapy, motivation enhancement therapy, CBT (coping skills training, exploration of high-risk situations, therapy to prevent recurrence, behavioral couples therapy, etc.), continuous intensive case management, rehabilitation programs at residential institutions, regular participation in AA meetings, and individual psychodynamic therapy are recommended. Psychoeducational intervention is also recommended as a form of adjuvant treatment.
Intensive inpatient treatment
The intensive inpatient treatment program of alcohol dependence in Korea usually provides a 2 or 3-step program that takes 6-10 weeks to complete in a closed ward. Step 1 comprises 1-2 weeks of detoxification and basic education. This is followed by 4-8 weeks of intensive education (Step 2). Some mental hospitals provide 2 weeks of intensive education in a closed or semi-closed ward (Step 2) and 6 weeks in an open ward (Step 3). These programs include 12-step alcohol treatment, CBT, art therapy, group PT, individual PT, self-help therapy, meditation and medication.
Outpatient individual and group PT
In Korea, individual PT for alcoholism generally has a supportive PT mode and consists of sessions every 2 to 4 weeks lasting 15 to 30 min per session in a standard outpatient setting. Group PT has a cognitive-behavioral PT mode and consists of weekly group meeting, each lasting 60-90 min, usually administered by 1 psychiatrist and 1 nurse or social worker. Group members have the opportunity to obtain peer support and experts' comments and to model their behavior after that of others in the group.
Kim et al. (18) performed a long-term comparative trial with an aim of evaluating the effectiveness of continuing group PT for Korean outpatients with alcohol dependence. This study, which was undertaken for 6 yr, was a quasi-experimental trial with 177 alcohol-dependent patients who had completed 10-week inpatient alcohol treatment program each. Group PT was a cognitive-behavioral PT mode, and individual PT was a supportive PT mode in an outpatient setting. Abstinence rates of the combined PT group (outpatient individual PT plus group PT, n=94) were significantly higher relative to those of the outpatient individual PT-only group (comparison group, n=83) (log rank [Mantel-Cox], chi-squared=22.58, df=1, P<0.001). Outpatient group PT was a significant predictive factor for the alcohol abstinence rate (B=-0.710, df=1, P<0.001, Exp [B]=0.492, [95% confidence interval (CI): 0.355-0.680]), and even after controlling for confounding factors, outpatient group PT was a significant predictive factor for the alcohol abstinence rate (B=-0.671, df=1, P<0.001, Exp [B]=0.511, [95% CI: 0.366-0.715]). Our findings indicate that for patients with alcohol dependence, who had completed the inpatient alcohol treatment, outpatient group PT appears to be an effective form of continuing care or aftercare within the context of an outpatient service system in Korea.
AA
AA was started in 1935 by a New York stockbroker (William Wilson) and an Akron, OH, physician (Robert Smith) in the United States (19). It is a mutual movement world-wide, which states that the "primary purpose is to stay sober" and aid other alcoholics to achieve abstinence from alcohol. Its objective is to effect enough change in the thought process of alcoholics "to bring about recovery from alcoholism" through a transcendent awakening. Such transcendent awakening is achieved by adhering to the Twelve Steps. In addition, sobriety is furthered by volunteering for AA and regular AA meeting attendance or contact with AA members (20).
In Korea, the first AA meeting was held by an Irish priest at a Catholic church in 1983. As of October 2011, 182 meetings have been organized in various locations nationwide. AA in Korea operates actively, and the organization's of the 16th AA Korea International Convention was held in December 2011 (http://www.aakorea.co.kr/).
Brief intervention
Jung et al. (21) performed a randomized controlled trial with an aim of evaluating the effects of brief intervention to promote insight among the 41 Korean alcohol-dependent patients who had been admitted to an alcohol treatment center. Patients in the intervention group (IG), while focusing on insight enhancement, participated in the five sessions of brief individual intervention. The IG showed significant improvement (P<0.05) in the distribution of insight level and in the insight score. However, the control group did not show such significant improvement. As insight has a positive effect on the motivation for treatment, and may play a critical role in the recovery process, this brief form of intervention focused on the insight enhancement may be an effective modality to improve the insight among alcohol-dependent patients.
Virtual reality therapy
Lee et al. (22) conducted an age, education, alcohol consumption matched trial with the object of evaluating the effects of a virtual reality training program (VRTP) in Korean male alcohol-dependent inpatients. This is the first multisensory stimulation virtual reality therapy for alcohol-dependent patients. The virtual reality therapy (VRT) consisted of a succession of scenes that were associated with relaxation, simulating a high-risk situation (virtual alcohol cues) and then an aversive stimulation. Alcohol-dependent patients were exposed to such sequence of 10 VRTP sessions (VRTP group, n=20) and CBT sessions (CBT group, n=18). The VRTP group displayed a larger reduction in craving, when compared to the CBT group (F=8.73, P=0.01). There was a complete increase in EEG alpha power in Fp2-A2 (z=2.91, P<0.01) and F8-A2 (z=3.80, P<0.01) in the pattern of the change of 16 EEG leads in the VRTP group, between the pre-intervention and the 10th VRTP session, but not in the CBT group.
ALCOHOL TREATMENT SYSTEMS IN KOREA AND THE UNITED STATES
Table 3 presents the comparison of current situation and alcohol treatment systems between Korea and the United States.
Table 3.
Comparison of alcoholism treatment systems between Korea and the United States
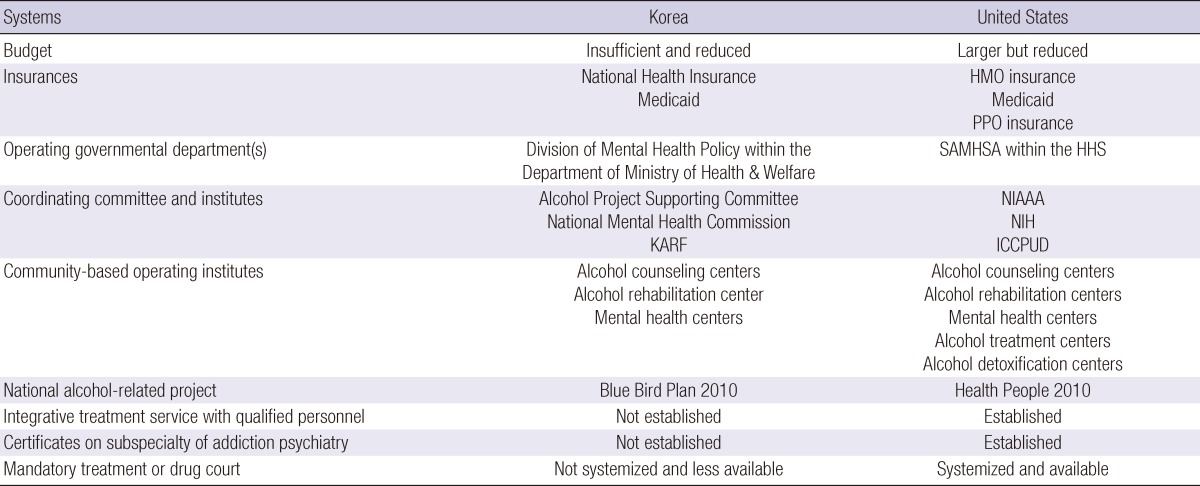
HMO, Health Maintenance Organization; PPO, Preferred Providers Organization; SAMHSA, Substance Abuse and Mental Health Services Administration; HHS, Department of Health and Human Services; KARF, Korean Alcohol Research Foundation; NIAAA, National Institute on Alcohol Abuse and Alcoholism; NIH, National Institutes of Health; ICCPUD, Interagency Coordinating Committee on the Prevention of Underage Drinking.
Alcohol treatment systems in Korea
In Korea, based on the forms of legal support given in Article 48 and 52 of the Korean Mental Health Law, the alcohol treatment delivery system is primarily carried out via alcohol counseling centers that are established and managed in the cities and sections with a population of more than 200,000 people. Some services are also delivered by mental health centers. Alcohol counseling centers provide prevention and rehabilitation services to alcohol-dependent individuals and their families, in order to help them resolve community alcohol problems, and to improve the health of the individuals. The business projects of alcohol counseling centers include the founding of policies and systems to alcohol issues, academic research activities and seminars related to alcohol, prevention and public relations activities to promote alertness regarding the importance of alcohol abuse prevention among community residents, the protection of the rights of alcohol-dependent individuals and their families, and communication with specialized organizations and groups pertinent to the communities.
The Korean Alcohol Research Foundation (KARF), which had been established in April 2000, is the nation's first professional research center with the purpose of solving the alcohol concerns in Korea. It is operated with funds from alcohol beverages and alcohol manufacturing companies to protect alcohol consumers, which carry out the companies' social responsibility. The KARF has had major projects in the following areas: treatment of alcoholics, rehabilitation for alcoholics to prepare them to return to society, research on the prevention of drinking and a survey of the status of the drinking problem in Korea, training of specialists, and public relations activities to prevent alcoholism. In addition, the KARF runs a hospital, counseling center, and rehabilitation institution (residential facility, rehabilitation center, and halfway house). In 2000, KARF, along with the Ministry of Health & Welfare of Korea Government, assisted in establishing 4 alcohol counseling centers.
The Blue Bird Plan, a national alcohol policy, was launched by the Korean Ministry of Health and Welfare in August 2006, and the "Bluebird Plan 2010" was published as Korea's overall strategy to reduce alcoholism. Instead of executing an alcohol control policy, it focused on changing the traditional drinking culture and generous social atmosphere toward drinking. Its main purpose was to "refresh the social atmosphere with keen awareness of the seriousness of alcohol harm; minimize alcohol harm by improving health promotion and lifestyle; reduce prevalence of alcohol use and alcohol-related accidents; decrease risky drinking behavior of high-risk groups; and enhance alcohol-related medical and rehabilitation services and create public/private social safety environment against alcohol harm." The plan involved the employment of a first alcoholism prevention project for the general Korean population, a second alcoholism prevention project for risk groups, a third prevention project for alcohol-dependent patients, the establishment of a safe social environment to inhibit devastation caused by drinking, and infrastructure production to drive alcohol policies. In order to begin the pan-national launch of the alcohol devastation publicity campaign, the Bluebird Forum was established on March, 2007. Initially, the Bluebird Forum consisted of 11 non-governmental and 2 governmental organizations. In 2009, the Bluebird Forum comprised 20 non-governmental and 2 governmental organizations.
In 2010, the Alcohol Project Supporting Committee was founded and was set out to improve social awareness of alcoholism, providing technical support for alcohol counseling centers, steering the activation of the operation of centers via evaluation of the consultation services, carrying out training of alcohol specialists and pertinent civil servants, avoiding national and community-level alcohol devastation, instituting an alcohol rehabilitation system, and support for alcohol-related policies (http://www.alcoholcsc.or.kr/). The Alcohol Project Supporting Committee reported that the Bluebird plan was positive in revealing the overall aims of its alcoholism-related projects since 2006, however, it failed to secure appropriate budgets and establish action plans (23).
Alcohol treatment systems in the United States
In the United States, the Substance Abuse and Mental Health Services Administration (SAMHSA) was established in 1992 by the Congress, as the part of a reorganization of the federal administration of mental health services; the Alcohol, Drug Abuse, and Mental Health Administration (ADAMHA) was abolished and its service components were transferred to the newly-organized SAMHSA. SAMHSA is an operating division within the U.S. Department of Health and Human Services (HHS), and is in charge with reducing the impact of substance abuse and mental illness in the communities of America. SAMHSA has four centers: Center for Mental Health Services (CMHS) which concentrates on the prevention and treatment of mental disorders; Center for Substance Abuse Prevention (CSAP) which seeks to inhibit and lessen the abuse of illegal drugs, alcohol, and tobacco; Center for Substance Abuse Treatment (CSAT), which assist in the efforts of effective substance abuse treatment and recovery services; Center for Behavioral Health Statistics and Quality (CBHSQ) which has primary responsibility for the collection, analysis and dissemination of behavioral health data (http://www.samhsa.gov/about/).
The Consolidated Appropriations Act of 2004 instructed the Secretary of HHS to launch the Interagency Coordinating Committee on the Prevention of Underage Drinking (ICCPUD) and to issue an annual report which summarizes all the federal agency activities related to the prevention of underage alcohol use. HHS made ICCPUD a standing committee to provide ongoing, high-level leadership on this issue, and to serve as an instrument for managing the federal efforts aimed at preventing and reducing underage drinking. SAMHSA serves as the lead ICCPUD agency (https://www.stopalcoholabuse.gov/).
The American Board of Addiction Medicine, Inc. (ABAM) is a not-for-profit 501 organization whose mission is to examine and certify diplomates. ABAM was established in 2007 following by a committee of the American Society of Addiction Medicine. This action was taken as a method of recognizing qualified specialists in Addiction Medicine. ABAM offers a rigorous certifying examination that was developed by an expert panel and the National Board of Medical Examiners, as well as maintains a certification examination to ensure that ABAM-certified physicians maintain life-long competence in Addiction Medicine (http://www.abam.net/wp-content/uploads/2010/10/The-American-Board-of-Addiction-Medicine-Who-We-Are1.pdf).
Founded in 1974, as the National Association of Alcoholism Counselors and Trainers (NAACT), the organization's prime purpose was to develop a field of professional counselors with professional qualifications and backgrounds. The organization progressed and became the National Association for Alcoholism and Drug Abuse Counselors (NAADAC) in 1982, uniting the professionals who worked for positive outcomes in alcohol and drug services. NAADAC's Mission, its statement adopted 1998, is to lead, unify, and empower addiction focused professionals to achieve excellence through education, advocacy, knowledge, standards of practice, ethics, professional development and research.
CURRENT PROBLEMS OF THE ALCOHOL TREATMENT SYSTEM IN KOREA
Long-term Hospitalization
Mattes et al. (24) reported that in a 3-yr post-hospital follow-up study of psychiatric patients, the prognosis of the short-term hospitalization patients did not differ from that of the long-term hospitalization patients. Furthermore, long-term hospitalization increased cases of re-hospitalization over short-term hospitalization. The financial loss that results from an inappropriate extended hospitalization period and the rise in the problem of institutionalization clearly show the importance of short-term hospitalization and effective management within a regional community after discharge (25).
In Korea, however, long-term hospitalization and services geared towards institutionalization have been pointed out as problems. Suh et al. (26) investigated the hospitalization period, the regular access to outpatient clinics, and the rate of extended hospitalization for a 3-yr period for the first admitted psychiatric patients who were diagnosed with mental behavior disorder due to alcohol use (F10) (n=9,086) in 2005. During the 3 yr, the average hospitalization period of the patients was 138.5 days, the rate of their regular utilization of outpatient clinics was 3.9%, and the rate of their extended hospitalization (longer than 6 months) was 20.6%.
Lack of early detection and unconnected intervention system
Early detection and brief intervention emphasize that it is possible for individuals to modify their problematic drinking patterns (27, 28). Inherent in early detection is the notion that it is possible for individuals to learn to drink responsibly. The advantage of brief intervention is that it is quick and efficient to administer and can therefore be implemented in settings where resources may be scarce. However, the early detection and brief intervention services provided by primary medical centers are highly insufficient in Korea.
According to the evaluation report for the Bluebird Plan 2010 (23), although early detection of AUD patients was carried out at alcohol counseling centers, the services connecting patients to intervention were insufficient. Furthermore, the provision of screening tests, and the establishment of an information system were carried out only partially.
Budget insufficiency
According to the evaluation report for the Bluebird Plan 2010 (23), the proposed budget of 26.6 billion KRW (20.8 million USD) in 2009 was reduced substantially to the actual budget of 3.5 billion KRW (2.7 million USD), which made it more difficult to execute the projects. Since the budget for alcohol counseling centers is not stable, the continuity and stability of services are not secured.
Scarcity of alcohol experts/personnel and service standardization
Due to insufficient personnel specialized for alcoholism and their disproportionate concentration in the capital city of Seoul and its surrounding metropolitan areas, it is necessary to distribute resources related to alcohol treatment service and to train specialists. According to the evaluation report for the Bluebird Plan 2010 (23) in 2009, there were 41 alcohol counseling centers and 12 alcohol rehabilitation centers, which are less than the targeted 96 centers and 18 centers, respectively. In addition, service standardization at alcohol counseling centers, alcohol specialized hospitals, and alcohol rehabilitation institutions are insufficient. In 2011, alcohol addiction treatment guideline suitable to Korean characteristics utilizing evidence-based methods was proposed. However, their clinical applications to meet the requirements of Korean treatment systems need to be tested and further improvements are needed.
Insufficient legal policies and lack of Integrative treatment delivery system
The legal basis for the establishment and operation of alcohol counseling centers, which are the central organizations for the provision of services for alcoholism treatment and rehabilitation in regional communities, is insufficient. It is difficult to establish a consolidated integrative system due to the lack of an exclusive section for such within the Department of Health & Welfare. Thus, the consistency and continuity of pertinent treatments and policies on alcoholism are low, and tend to be limited to a single project. In addition, discussions of pertinent policies between the government and private specialist groups may be considered insufficient, and the establishment of comprehensive execution plans at the time of project planning is urgently required (29). With regard to the provision of alcoholism treatment services, although systematic and overall management in alcoholism prevention, alcohol withdrawal treatment, and rehabilitation treatment, is required, only segmented and cross-sectional services are being provided. In addition, post-discharge services in outpatient alcoholism treatment facilities and the connection system to rehabilitation services are unsatisfactory. Furthermore, continuous case management for alcoholism is insufficient.
DEVELOPMENTAL DIRECTION OF ALCOHOL TREATMENT SYSTEM IN KOREA
Outpatient-oriented alcohol treatment services
By actualizing prevention and treatment centered on outpatient-oriented services rather than treatment and rehabilitation as inpatients, resources including funds can be distributed effectively. The unnecessary long-term hospitalization of alcoholism must be reduced, and the return of alcoholics to their community and to society must be accelerated. By improving the environment that impairs the therapeutic approach due to the social stigma of alcoholism, the prevention, treatment, and rehabilitation services based on outpatient settings are expected to become stronger.
Strengthening of early detection and connection to an intervention system
Early detection and treatment of alcoholism is crucial in reducing its impact on a person's life and offers far better prognosis for overall health and wellbeing. Furthermore, it is important that the outpatient-oriented treatment system is a connected system including connection to some form of after-care following completion of admission treatment.
Securing a Budget
For the establishment and execution of effective alcohol policies, the budget for the execution of the policies must be urgently secured. In the financial system through which the funds are dispersed, it is difficult to be responsible for the service; and thus, additional funds must be secured and their stability ensured.
Securing experts/personnel and service standardization
For an active and efficacious treatment service system for the early diagnosis, treatment, and rehabilitation of alcoholism, it is important to secure experts on alcoholism and alcohol specialized institutions. Doing this enables the equal distribution of service access across regional communities.
The services of alcohol counseling centers, alcohol specialized hospitals, and alcohol rehabilitation centers should be standardized and operate according to evidence-based treatments. New treatment programs suitable to Koreans must be continuously developed and standardized.
Establishment of legal policies and integrated treatment delivery system
The continuous provision of addiction-related services must be strengthened; and to manage additional problems systemically and holistically, integrated alcohol addiction treatment and rehabilitation service delivery systems should be established. Overall and continuous management of treatment during the acute phase of alcoholism (detoxification, etc.), rehabilitation treatment, and training of alcoholics for returning to society are required. In addition, the postdischarge ambulatory treatments at the outpatient clinics and the system connected to the rehabilitation services performed primarily at the regional communities should be strengthened. Case management is required for individuals who are at high-risk for alcoholism or chronic and severe alcoholism.
To achieve these, existing laws for addiction management must be revised. In addition, for the establishment of an independent delivery system by separating mental health problems and addiction problems, an addiction management committee must be established. The establishment of alcohol-related laws including mandatory alcohol education for drunken drivers, and mandatory alcohol treatment for alcohol-related criminals is urgently needed.
CONCLUSIONS
Current alcohol treatment system in Korea compared to the United States relatively shows the lack of integrative treatment delivery system. To establish integrative treatment delivery systems, it is important to set up an independent governmental administration on alcohol abuse, to secure experts on alcoholism, and to conduct outpatient alcoholism treatment programs and facilities in an open system including some form of continuing care or after-care following completion of the initial phase of treatment.
Footnotes
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (grant number A084589).
The majority of the studies described in this review were presented in a symposium at Asia-Pacific Society for Alcohol and Addiction Research (APSAAR) in February 2012.
References
- 1.OECD. OECD Health data 2011. [accessed on 1 November 2011]. Available at http://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_LVNG.
- 2.Ministry for Health & Welfare. The epidemiological survey of psychiatric illnesses in Korea. Seoul, Korea: Ministry for Health & Welfare; 2011. [Google Scholar]
- 3.Chou SP, Lee HK, Cho MJ, Park JI, Dawson DA, Grant BF. Alcohol use disorders, nicotine dependence, and co-occurring mood and anxiety disorders in the United States and South Korea: a cross-national comparison. Alcohol Clin Exp Res. 2012;36:654–662. doi: 10.1111/j.1530-0277.2011.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung WJ, Chun HJ, Lee SM. Socioeconomic costs of alcohol drinking in Korea. J Prev Med Public Health. 2006;39:21–29. [PubMed] [Google Scholar]
- 5.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 6.Addiction Treatment Guidelines Development Committee. Addiction treatment guidelines series. Seoul: Korean Academy of Addiction Psychiatry, Alcohol Project Supporting Committee; 2011. [Google Scholar]
- 7.Korean Academy of Addiction Psychiatry. Fall academic conference of Korean academy of addiction psychiatry. Seoul: 2011. Oct 14, [Google Scholar]
- 8.Namkoong K, Lee BO, Lee PG, Choi MJ, Lee E. Acamprosate in Korean alcohol-dependent patients: a multi-centre, randomized, double-blind, placebo-controlled study. Alcohol Alcohol. 2003;38:135–141. doi: 10.1093/alcalc/agg038. [DOI] [PubMed] [Google Scholar]
- 9.Tempesta E, Janiri L, Bignamini A, Chabac S, Potgieter A. Acamprosate and relapse prevention in the treatment of alcohol dependence: a placebo-controlled study. Alcohol Alcohol. 2000;35:202–209. doi: 10.1093/alcalc/35.2.202. [DOI] [PubMed] [Google Scholar]
- 10.Golovko SI, Zefirov Slu, Golovko AI, Shpilenia LS, Nekrasov IuA. Acamprosate: a novel treatment for alcoholism. Eksp Klin Farmakol. 2000;63:70–73. [PubMed] [Google Scholar]
- 11.Poldrugo F. Acamprosate treatment in a long-term community-based alcohol rehabilitation programme. Addiction. 1997;92:1537–1546. [PubMed] [Google Scholar]
- 12.Namkoong K, Farren CK, O'Connor PG, O'Malley SS. Measurement of compliance with naltrexone in the treatment of alcohol dependence: research and clinical implications. J Clin Psychiatry. 1999;60:449–453. doi: 10.4088/jcp.v60n0706. [DOI] [PubMed] [Google Scholar]
- 13.Kim SG, Kim CM, Choi SW, Jae YM, Lee HG, Son BK, Kim JG, Choi YS, Kim HO, Kim SY, et al. A micro opioid receptor gene polymorphism (A118G) and naltrexone treatment response in adherent Korean alcohol-dependent patients. Psychopharmacology (Berl) 2009;201:611–618. doi: 10.1007/s00213-008-1330-5. [DOI] [PubMed] [Google Scholar]
- 14.Johnson BA, Rosenthal N, Capece JA, Wiegand F, Mao L, Beyers K, McKay A, Ait-Daoud N, Anton RF, Ciraulo DA, et al. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298:1641–1651. doi: 10.1001/jama.298.14.1641. [DOI] [PubMed] [Google Scholar]
- 15.Furieri FA, Nakamura-Palacios EM. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68:1691–1700. doi: 10.4088/jcp.v68n1108. [DOI] [PubMed] [Google Scholar]
- 16.Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, Abenavoli L, D'Angelo C, Caputo F, Zambon A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370:1915–1922. doi: 10.1016/S0140-6736(07)61814-5. [DOI] [PubMed] [Google Scholar]
- 17.Anton RF, Kranzler H, Breder C, Marcus RN, Carson WH, Han J. A randomized, multicenter, double-blind, placebo-controlled study of the efficacy and safety of aripiprazole for the treatment of alcohol dependence. J Clin Psychopharmacol. 2008;28:5–12. doi: 10.1097/jcp.0b013e3181602fd4. [DOI] [PubMed] [Google Scholar]
- 18.Kim JW, Choi YS, Shin KC, Kim OH, Lee DY, Jung MH, Lee BC, Kang TC, Choi IG. The effectiveness of continuing group psychotherapy for outpatients with alcohol dependence: 77-month outcomes. Alcohol Clin Exp Res. 2012;36:686–692. doi: 10.1111/j.1530-0277.2011.01643.x. [DOI] [PubMed] [Google Scholar]
- 19.Kelly JF. Self-help for substance-use disorders: history, effectiveness, knowledge gaps, and research opportunities. Clin Psychol Rev. 2003;23:639–663. doi: 10.1016/s0272-7358(03)00053-9. [DOI] [PubMed] [Google Scholar]
- 20.Alcoholics Anonymous. This is A.A. New York: Alcohol Anonymous World Services, Inc; 1984. [Google Scholar]
- 21.Jung JG, Kim JS, Kim GJ, Oh MK, Kim SS. Brief insight-enhancement intervention among patients with alcohol dependence. J Korean Med Sci. 2011;26:11–16. doi: 10.3346/jkms.2011.26.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee SH, Han DH, Oh S, Lyoo IK, Lee YS, Renshaw PF, Lukas SE. Quantitative electroencephalographic (qEEG) correlates of craving during virtual reality therapy in alcohol-dependent patients. Pharmacol Biochem Behav. 2009;91:393–397. doi: 10.1016/j.pbb.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 23.Alcohol Project Supporting Committee. Evaluation report on the Bluebird Plan 2010. Seoul, Korea: Alcohol Project Supporting Committee; 2010. [Google Scholar]
- 24.Mattes JA, Rosen B, Klein DF. Comparison of the clinical effectiveness of "short" versus "long" stay psychiatric hospitalization. II. Results of a 3-year posthospital follow-up. J Nerv Ment Dis. 1977;165:387–394. doi: 10.1097/00005053-197712000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Thornicroft G, Bebbington P, Leff J. Outcomes for long-term patients one year after discharge from a psychiatric hospital. Psychiatr Serv. 2005;56:1416–1422. doi: 10.1176/appi.ps.56.11.1416. [DOI] [PubMed] [Google Scholar]
- 26.Suh SK, Kim Y, Park JI, Lee MS, Jang HS, Lee SY, Lee JS. Medical care utilization status and associated factors with extended hospitalization of psychiatric patients in Korea. J Prev Med Public Health. 2009;42:416–423. doi: 10.3961/jpmph.2009.42.6.416. [DOI] [PubMed] [Google Scholar]
- 27.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The alcohol use disorders identification test. Guidelines for use in primary care. Geneva, Switzerland: WHO; 2001. [Google Scholar]
- 28.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 29.Yoon MS. The current situation and developmental direction of Korean addiction service delivery system. Ment Health Soc Work. 2010;35:234–266. [Google Scholar]


