Abstract
Introduction
In 2003, an ICRC-SFD Ponseti program was introduced in southern Vietnam. Additional programs were introduced by the Prosthetics Outreach Foundation and independently by physicians trained at our center. The purpose of this study was to evaluate the impact, progress and challenges facing Ponseti practitioners and patients' family members in Vietnam. In addition, web-conferencing (Ponseti Virtual Forum) for continued medical education in the method was also assessed.
Methods
Multiple questionnaires were developed to conduct face-to-face practitioner interviews, focus group interviews, and parental interviews. Observation was done at multiple site clinics to determine or confirm additional challenges faced by practitioners. Web conferencing was introduced to sites in Ho Chi Minh City and Da Nang City.
Results
The number of clubfoot patients treated with the Ponseti method has increased over time with approximately 1,252 infants treated between 2003 and 2010. Specific challenges were identified relating to communication, networking, distance and transportation, and finances for both practitioners and parents. The PVF was not only found to facilitate rapid, relevant dissemination of medical knowledge – thus increasing physician and patient satisfaction – but it may also be found to act as an interface in which medical culture, insight, and compassion are shared benefiting all virtual forum participants.
Conclusion
The identified progress and challenges mirrored that of similar studies done in other countries with several factors affecting progress. Focusing on improving communication channels and networking while working with the ministry of health may improve the facilitation of the Ponseti method in Vietnam. Further implementation and evaluation of the PVF may act as a guide for current and future programs in Vietnam or other countries.
Introduction
Congenital clubfoot is considered to be the most common congenital birth defect of the musculoskeletal system. Eighty percent of children living with clubfoot reside in developing countries where the limitations of medical knowledge and scarcity of resources prevent the adequate care of these individuals. Left untreated it leads to long-term physical, psychological, emotional, and economical adversity for affected individuals and families. In addition, because up to 50% of these individuals are affected bilaterally, it becomes even more evident how neglected clubfoot is one of the most common physical disabilities in the world (1,2). In Vietnam—where the prevalence of clubfoot is estimated to be 1/1000 births—affected individuals face diminished prospects for education and employment, leading to a dependency on family or external aid (e.g., begging) for survival (3).
With a 95% success rate, the non-invasive and resource-efficient Ponseti method is especially well suited for use in developing countries, such as Vietnam, due to its low cost and high impact results (1). The method is safer, more economical, more comfortable, and more feasible than traditional surgery (8, 9, 10). Economically, in respect to Vietnam, the Ponseti method is two to three times more cost effective than surgery: Surgery costs VND 4,300,000; Ponseti method costs VND 1,400,000 (3). The simplicity of the method also lends itself as a potentially crucial piece in countries with a shortage of physicians and in countries where physicians are over burdened: in addition to orthopedic surgeons, the Ponseti method can be done by physical therapists, nurses, or other health care professionals (2, 3).
With recent initiatives by organizations such as the International Community of the Red Cross and the Prosthetics Outreach Foundation to establish the Ponseti method in Vietnam, a current evaluation of the method in Vietnam allows for the identification of factors aiding and challenging the method's dissemination. Interestingly, principles from Everett Roger's Diffusion of Innovation (4) and their application to a healthcare setting by Donald Berwick (11) indicate a complex interplay between the dissemination of an innovation, e.g., the Ponseti method, the viability of an innovation, the individuals implementing an innovation, and the social or organizational context and structure in which an innovation is introduced. The purpose of this study was to identify these factors through interviews with individual health care practitioners and patient's family members. In addition, the introduction of the Ponseti Virtual Forum was done to provide additional resources and continued medical education to health care practitioners in this country.
The Ponseti Virtual Forum (PVF) is a web-conference-based collaborative forum for Ponseti practitioners to converse in real time and exchange information regarding experiences with difficult cases, developments in the realm of the Ponseti method, or even other medical knowledge as the use of the virtual forum evolves. The PVF portal on the Global Campus is powered by Elluminate Live! software program (https://globalcampus. uiowa.edu/index.html and http://www.continuetolearn. uiowa.edu/ccp/tech-support/elluminate.htm) which functions in low band-width settings (specially suited for developing countries) while allowing for videoconferenc-ing, text messages, multimedia display and real-time document sharing.
Methods
Multiple methods were used to gather information in order to increase the validity of the study through triangulation (5, 6). To evaluate impact, the number of health care providers trained in the Ponseti method, where they practice, and the number of children with clubfoot treated with the Ponseti method were determined over the phone or in personal interviews. Candidates for interviews were from participants of the International Committee of the Red Cross training held in Ho Chi Minh City in 2007 and 2008 (3, 12), participants of the Prosthetic Outreach Foundation (POF) training sessions, and various other individuals referred by Dr. Nhi Manh Huynh from the Hospital of Traumatology and Orthopedics in Ho Chi Minh City. In addition, POF provided a count for the number of clubfoot treated in POF sponsored hospitals.
For the evaluation of factors influencing its diffusion, the methods included:
Semi-structured interviews (face-to-face or phone based)
Interview questions involved both open-ended and closed-ended questions. A total of 106 individuals were contacted with 47 returning questionnaires. Focus groups. Two focus groups were organized in Ho Chi Minh City and Da Nang City with a cumulative total of 12 Ponseti participants.
Interviews with parents
A total of 99 parents were interviewed to compliment the health practitioner interviews. Interviews most often included perspectives from the mother, father, and/or extended family (grandparents, uncles, and aunts).
Direct observation of clubfoot clinics
Data collected from interviews and focus groups were recorded in Vietnamese, translated into English, encoded, and stored securely. In correlation with research done by Lu et al, (5), categories included topics related to: physician education, caregiver compliance, cultural aspects, public awareness, poverty, financial constraints on physicians/hospitals, and challenges of the treatment process.
The Ponseti Virtual Forum was introduced to the Da Nang Orthopedic and Rehabilitation hospital and to the Hospital of Traumatology and Orthopedics (HTO) in Ho Chi Minh City. A live session with an expert on clubfoot treatment (JAM) with physicians and patients at HTO was held with a total of 10 participants.
Results
Of the 49 practitioners (physicians, nurses, physical therapists, and cast technicians) responding to questionnaire requests, 10 individuals indicated they no longer practiced the Ponseti method. These individuals were from Southern, Central, and Northern Vietnam and represented 21 different hospitals throughout these regions. The reasons stated included not having seen clubfoot patients from the time of initial training or having switched medical specialties or departments. Questionnaires from 2 physical therapists were also removed due to the inability to complete visitation documents before the end of the research period. As a result, the following findings reflect the response of 37 practitioners.
Impact of the Program: Number of Practitioners Trained and Patients Treated
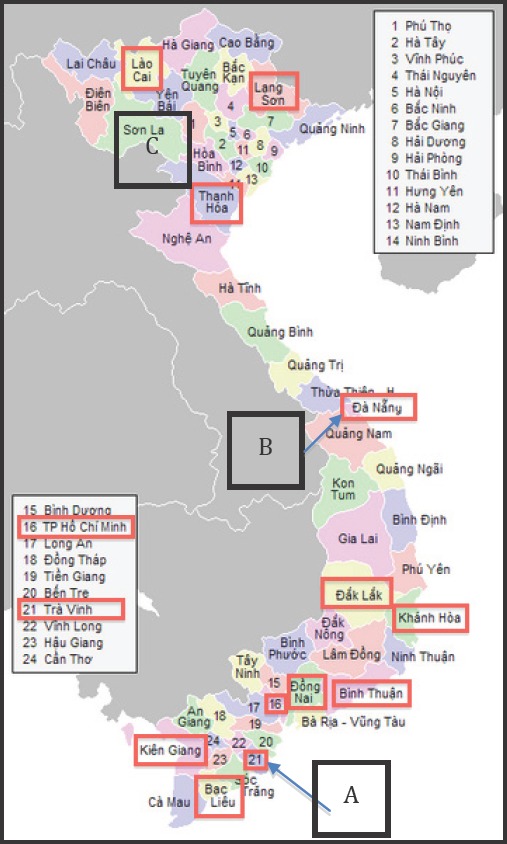
The exact number of practitioners trained was not found due to the lack of a central database or directory and loose networking between practitioners trained in the Ponseti method. However, from the total contacts provided in Vietnam, there are at least 120 individuals who have been trained in the Ponseti method. Considering all practitioners who responded, the 49 individuals practiced in various provinces of Southern (37 practitioners from 15 hospitals), Central (6 participants from 3 hospitals), and Northern (4 participants from 3 hospitals) Vietnam (Figure 1).
Figure 1. Map of Vietnam. Boxes indicate the province or city in which the interviewed health care providers practiced. (A) Over half of the interviewees were based in various hospitals in Ho Chi Minh City, #16. They included physicians, nurses, physical therapists, and cast practitioners. (B) Da Nang lies in central Vietnam and is the major clubfoot center for patients within that region. (C) Recent efforts by the Prosthetics Outreach Foundation to spread the Ponseti method in Northern Vietnam. In addition to the 3 boxed provinces, practitioners were also trained in Ha Noi, Ha Giang, Yen Bai, Cao Bang, Son La, and Quang Ninh.
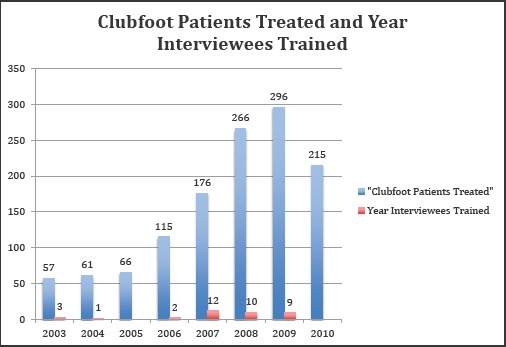
Determining the exact number of patients treated with the Ponseti method vs. surgical methods was not possible. The medical system in Vietnam generally preferred that patients took home their records. A few physicians did, however, keep a personal record of clubfoot patients they treated. With these records and in conjunction with question 15 on the practitioner questionnaire (Appendix 1), it was possible to estimate the number of patients treated by the interviewed practitioners: roughly 1,252 infants between 2003 and 2010 (Figure 2). In regards to practitioner site, 653 patients were treated in Southern Vietnam beginning in 2003 with the majority being treated in 2007 and 2008; 466 patients were treated in Central Vietnam beginning in 2003 with the majority treated in 2006 onwards. In Northern Vietnam, a total of 129 clubfoot cases were treated by POF sponsored hospitals with the number of cases per year doubled in 2010.
Figure 2. Clubfoot patients treated and year interviewees trained. Blue Bars: Reflects the self-reported number of patients treated by practitioners from the year they learned the Ponseti method to the time of the interview, June-July 2010. Red Bars: Indicates when each of the interviewed practitioners completed Ponseti training. Trainings were done by the International Committee of the Red Cross, Prosthetics Outreach Foundation, or at the University of Iowa. Of note, the number of patients treated in 2010 only reflect data up to June-July of 2010.
Challenges to the Diffusion of the Ponseti method
As with the introduction of many novel ideas, models, or methods in the US and abroad, the rapid development, progression, and implementation of the Ponseti method in Vietnam has not been without both unique and common (among other countries) challenges to both health care practitioners and patients' families.
Health Care Providers
The practitioner questionnaire included questions regarding the perceived advantages of the Ponseti method, ideas on how to better spread the method, and additional comments that individuals wished to share (Appendix 1). The most commonly identified advantage of the Ponseti method in Vietnam was its high success rates and low recurrences. It was regarded has a highly effective treatment for clubfoot. In addition, practitioners were appreciative of its non-invasive and low risk procedures. Other identified advantages were: ease of learning, ease of practicing, and versatility of who can learn the method.
Additional ideas on facilitation of the Ponseti method in Vietnam involved education and communication. In promoting the method to parents, many thought that more careful explanations about the treatment, treatment course and length, and importance of bracing could help increase treatment compliance. It was suggested by multiple individuals to present pictures, brochures, or posters to help parents better visualize and internalize the treatment process. It was also suggested that practitioners keep pictures of past cases, before and after treatment, to show to new families and to help the parents gain confidence in the Ponseti method and its practitioner. In the realm of education, most practitioners identified the need for educating the general public and also raising awareness in healthcare related schools or programs. Many suggested targeting obstetricians and midwives to better identify clubfeet and to be aware of the resources available for treatment. A community-based rehabilitation structure was also proposed.
Other comments included increasing availability of long-term training sessions, improving networking between providers within Vietnam and in other countries, requests for a way to be updated with new developments with the Ponseti method, having training sessions for the obstetrics department, and pondering on the availability of lighter casts to aid in improving patient comfort and parental concern.
Technique and Protocols
The use of long-leg casts is crucial to the treatment of clubfeet, and the vast majority of interviewees indicated the use of long-leg casts while 2 utilized non-protocol short-leg casts. Less homogeneity was seen with the Achilles tenotomy and anesthesia use (local vs. general). 7 practitioners “always” performed the Achilles tenotomy, whereas 25 “sometimes” did and 2 “never” did. 17 practitioners indicated the use of local anesthetics, 3 used general anesthesia, and 1 used both. Like cast specificity, the use of braces plays a significant role in preventing the recurrence of clubfoot once casting has corrected the position and form of the affected foot. 27 individuals used the “shoe with foot-abduction bar” as the brace of choice, 5 used AFOs, 2 indicated the use of Denis-Browne, and 1 did not use any bracing. Finally, half the practitioners utilized massage or physical therapy along with casting and bracing.
In assessing for various criteria that practitioners referenced in determining when the Ponseti method should or should not be used, four broad categories surfaced: age, severity, Pirani scale, and none. The age cutoff for the Ponseti use ranged from 2–7 years old; however, most of the practitioners indicated that they would always try the Ponseti method first before surgery regardless of age. Although the Ponseti method was ac-cepted by most as the first option for clubfoot treatment, a few practitioners continued to utilize the Turco surgical method (5 individuals) and 3 utilized the elastic taping, Denis-Browne method.
Particular challenges arose with the procedural skill aspect of the Ponseti method. As with many procedurebased skills, practice and continual constructive feedback are necessary for both improving technique and maintaining confidence, especially when faced with cases involving nuances and complications. The vast majority of individuals who no longer practiced the Ponseti method – despite receiving training – indicated the lack of confidence as the underlying reason. These individuals, provincial practitioners, were trained but would not see clubfoot patients until a month or more after the initial training session. By this time, practical knowledge had been forgotten, and the individuals were predisposed to refer patients to cities for treatment. One way this challenge has been approached was through increasing one-on-one interaction time and increasing directed hands-on experience with casting clubfoot within the hospital environment. Dr. Nhi of the Hospital of Traumatology and Orthopaedics has been providing weekly and recurring training sessions with cast technicians and physiotherapists within HTO and other hospitals. This may help to address the issues of developing technique, confidence, and ensuring higher quality and consistent results.
Provider and Medical Culture
Challenges for providers in implementing the Ponseti method within a clinical setting were interwoven with time constraints, casting environment, operation system of the hospital or clinic, and medical culture. In contacting and scheduling appointments with patients, the practitioner did so independently without ancillary staff. For orthopedic surgeons, clubfoot patients were often scheduled between obligate surgeries during “free” time when surgeons could either rest or schedule a higher paying procedure to be done (opportunity cost). Significant amount of time was needed to be spent on educating parents and family members to ensure the best treatment outcome; however, this was identified as challenging when considering high volumes of patients, when the medical culture does not include patient educa-tion during a standard visit, and when most patient visits are completed within 5 minutes. Under this context, an unpleasant time burden was associated with the Ponseti method.
Practitioner burden was also impacted by the casting environment. A broad range of hospital environments was observed; however, a typical urban hospital was often crowded and non-air-conditioned – quite significant considering Vietnam's geographic location. The tropical heat, within casting areas consisting of 5–6 tables serving both children and adults, was augmented by the heat produced from overcrowding. With overcrowding also comes noise from waiting patients, from the gentleman in an adjacent casting table getting his broken arm reset, and from the baby crying during the Ponseti method casting procedure – an uncomfortable situation for all involved, patient and provider.
A unique challenge to providers was identified by a few of the high volume physicians. A newborn with untreated clubfoot was easier to treat with the Ponseti method; however, these practitioners often received infants who were previously treated incorrectly resulting in new challenges in the application of the Ponseti method. Often the foot was found to be stiffer and less malleable, parents were more skeptical of any type of casting procedure, and infants were conditioned into fearing physicians and casting – leading to more disruptive casting sessions.
No financial barriers were suggested by any of the practitioners. Practitioners do not necessarily lose income from practicing the Ponseti method. Conversely, many practitioners indicated that practicing the Ponseti method was essentially volunteer work due the minimal reimbursement gained by using the Ponseti method as opposed to performing surgical procedures. One practitioner questioned: if the outlook of physicians was only to do procedures to make money, what would happen to the patients who were equally needy but not as lucrative for physicians. The practitioner challenged that there were many more rewards to look for, not just monetary compensation. To say that there were only opportunity costs and only psychological satisfaction gained from altruism would be inaccurate. Where the health care system provides minimal rewards in treating clubfoot with the Ponseti method, cultural customs provided opportunities for families to express their gratitude towards their practitioner. As one physician stated: “[…] During the last Tet celebration, I have received many rewards from the families. The Vietnamese people considers Tet as an occasion to give gifts/money to whom they love/want to compensate (for) what they received. The money sum varies from 100.000 VND to 500.000 VND. One gave me 20 kg of rice, the mother kept the rice in one hand, and the baby in the other hand! All of these things made me rewarded!”
Health Care System and Communications Network
Specific challenges were identified stemming from having no specific protocol or integration of clubfeet treatment within the health care system and medical education institutions. Interviewees in both individual and focus group sessions identified the need to improve clubfeet education of obstetricians, midwives, and general public to ensure early identification and proper treatment.
Challenges in patient referral were augmented by the lack of a central directory of Ponseti practitioners – whether phone or website. Many practitioners, even within the same city, were not aware of others who utilized the Ponseti method; one positive outcome of conducting interviews and group sessions was providing the opportunity for networking to occur. Providers noted the need to strengthen communication and familiarity between Ponseti practitioners to improve referrals to better serve and minimize the burden on traveling families, to provide opportunities in exchanging experiences and consultation for complex cases, and to develop social support of practitioners who volunteer time and effort to do the Ponseti method.
Patients' Parents and Family Network
Casting and Bracing
Unlike to the challenges facing providers, the obstacles parents faced were interdependent on education level, transportation, and personal financial ability. Bracing adherence and follow-up difficulties were the most mentioned challenges by both practitioners and parents. Parents sited feelings of pity and sympathy for their child's discomfort as bracing caused chaffing of the infant's skin and unbearable crying. Less commonly, concerns for comfort with casts and casting were voiced. Blisters and rashes from the humid weather were concerning to parents. The affordability of braces was an issue for some patients, and some physicians often purchased braces for their patients.
Following casting, follow-up visits were necessary to maintain brace fitting, to ensure bracing adherence, and to monitor for recurrence. However, due to the intricate interplay between parental education level, financial status, and burdens associated with distance and transportation, many parents ceased complying with follow-up schedules. In the most extreme cases of severe poverty, parents cut casting periods short as soon as their child's foot appeared “normal” or adequate for walking. In addition to educating parents regarding the importance and consequences of deviating from protocol, the financial ability of the parents needs to be considered as an additional complication in completing treatment.
Finance and Transportation/Distance
Financial instability and poverty colored the challenges that were associated with transportation and distance. For patients living in cities, this was usually not a major deterrent from completing treatment and adhering to follow-up visits. Many parents from provincial towns, however, lost as much as 5–10 hours for a one-way trip to urban hospitals for treatment. Parents identified that trips to the hospitals resulted in the loss of the day's wages, which was doubled due to needing 2 people to travel. If arriving early, parents often spent the night or early morning in a hospital common area. In the context of weekly visits and follow-up visits, this was seen to be a significant challenge to overcome. Many parents also identified the need to pool money or donation from neighbors in order to pay for bus fare, lodging, and food.
Cultural Aspects
For the vast majority of parents interviewed, the cultural norm was to seek treatment for their child's clubfoot in hopes of providing a better future. A few mothers identified having felt some degree of shame, as often husbands or in-laws attributed their child's deformity to something the mother or the mother's family had done. However, the mothers understood the necessity of obtaining treatment for the child rather than hiding the child. Practitioners also expressed similar views during the interviews.
A unique and uncommon case was found to have cultural traditions preventing the completion of the Achilles tenotomy. Despite the tenotomy being a minor surgery, grandparents of this specific child were highly protective and refused the procedure even after pleading done by the physician. In Vietnamese culture, the grandparents have great weight in decision-making, and parents show respect by following their wishes. In this specific tradition, the child with clubfeet was the first-born male of the eldest son of the grandfather. As such, the child was seen as the sole carrier the grandfather's bloodline, and any danger – tenotomy included – leading to the death of the child would effectively end the bloodline.
Another rare and unique cultural barrier to the Ponseti method was explained by a physician in Ho Chi Minh City. There was a belief that what others saw as a deformity, the family, with the affected child, saw as a “gift” or talent. By removing the deformity, the child would no longer be gifted and special.
Health Care System
Without specific guidelines for clubfeet treatment in the health care system and without a clear central database of Ponseti practitioners, parents and infants with clubfeet were the most adversely affected. 68% of parents were directly directed to Ponseti providers shortly after the birth of their child; however, roughly 30% of parents were sent home without further instruction or were told to seek treatment when the child was older. These parents independently sought for care and indicated being referred multiple times before eventually meeting a practitioner could perform the Ponseti method. As discussed earlier, these challenges caused delay in treatment and unnecessary conditioning of the child. Health care is free for all children under 6 in Vietnam; however, differences among hospital policies caused variations in what was covered under the insurance. In some hospitals, cotton used in casting was covered, whereas in other hospitals parents were required to purchase extra cotton.
Ponseti Virtual Forum
The virtual forum was introduced to two physicians – one in Ho Chi Minh City and the other in Da Nang. Preceding one of the focus group sessions, a virtual clinic session was held with my site mentor, ten of his colleagues, and the senior co-author (JAM) in Iowa City. Barriers and benefits of the virtual forums were assessed by post-survey questionnaires and observation.
Barriers
Technological and economical barriers were the most prevalent and were primarily related to resource limitations. To utilize the virtual forums, most of the physicians would need to obtain their own hardware (laptops) in addition to webcams or speakers to maximize the experience. During preparation setup, software compatibility with Java caused slight delays. Trouble-shooting this issue may also present as a barrier depending on the laptop used by the practitioner. Limited internet access also challenged the ability to access the virtual forum easily: select rooms had consistent wifi or LAN access; these rooms were often administration conference rooms rather than patient areas. Room availability and scheduling conflicts with patients would hamper room availability. The general use of computers among practitioners in Vietnam should also be considered. Although an increasing population of physicians were beginning to utilize computer technology, such as email, many physicians have not found efficiency in using these modes of communication to facilitate patient care (e.g., phone calls are faster in reaching an individual, hospital records are paper based, and limited internet connectivity). This predisposition may cause slight reluctance in utilizing the virtual clinics. Other issues that arose were more related to the actual virtual clinic session that was held in HTO. In regards to improvements to the session, the following was suggested: 1) more time for participants to discuss, 2) allowing audience access to the microphone (only 1 available), 3) participant timeliness, and 4) language barriers.
Benefits
Despite these challenges, benefits were readily identified. Post-survey questionnaires confirmed that the session with Iowa City was helpful and interesting, and participants stated they would use the program in the future. Participants indicated the potential to use the virtual forums for exchanging experiences with other physicians, for presenting clinical information, for communicating and sharing data with foreign physicians and national physicians. The ability to communicate via video and document sharing was also found as strength of the virtual forum. This may prove beneficial to rural practitioners who may have internet connectivity, as was the case with a hospital in Tra Vinh (4–5 hrs bus from Ho Chi Minh City) which received a Bill and Melinda Gates foundation grant for improving computer and internet access to practitioners and patients at that hospital.
From the virtual forum session, physicians specifically identified gaining knowledge regarding complications with the Achilles tenotomy in minor surgery rooms and clubfoot recurrence. Practitioners identified the strength of being able to readily ask questions and receive answers live by using the virtual forum. The benefits were found to extend to family members of the case study, as they were able to learn information immediately about their child's complication. Personal and professional development was identified by post-survey questionnaires. Individuals enhanced their knowledge in the area of recurrent clubfoot cases, improved interaction with patients, and strengthened communication and networking between those who attended the session. In attending the session, practitioners were able to meet others in the same field with similar interests in treating clubfeet and practicing the Ponseti method. Just as striking, the virtual forum session allowed one physician to better understand the importance of incorporating family member's comments in treating clubfoot. The virtual forum was not only found to facilitate rapid, relevant dissemination of medical knowledge – thus increasing physician and patient satisfaction – but it may also be found to act as an interface in which medical culture, insight, and compassion are shared benefiting all virtual forum participants.
Discussion
The ability to walk is crucial in navigating the societal structures of Vietnam. Therefore, complete, successful correction of clubfeet is necessary for both broadening the life paths available to an individual and preventing misconceptions of the Ponseti method from forming and detracting from the many strides that have occurred with the introduction of the technique to Vietnam in 2003. No evaluation of the entirety of the Ponseti programs (ICRC, POF, others) had been done, and the aim of the study was to identify the impact and challenges among these constituencies. Comparing the findings from Vietnam to other Ponseti sites in the world allows for the identification of common themes to aid in developing solutions applicable in all countries, while contrasting the unique challenges specific to Vietnam.
When considering other Ponseti sites with published results– the United States (New Mexico), Uganda, Ma-lawi, and China – similar challenges were seen facing both practitioners and patients despite the difference in population, culture, and geography.
Barriers practitioners faced were also similar among the different countries. In all countries, transportation and distance proved to be consistent challenges for parents. Specifically, the issue of building confidence and the difficulty of gaining practical experience in new trainees was a challenge identified by the studies done in China and Uganda (5, 6). Like the Vietnamese practitioners, some of the Chinese physicians believed the need for a higher level of experience before treatment efficacy could be attained. With this specific issue of continuing education, the virtual clinics would be able to facilitate exchange of knowledge and expertise with physicians within the country and outside the country.
Patient and their families in all countries found difficulties in obtaining treatment and adhering to bracing. Like Vietnam, poverty contributed to these challenges. In New Mexico, Avilucea et al. found a 12.5 fold increase in recurrence due to bracing non-adherence in those who made less than 20,000 USD/year. Interestingly, the reported causes for brace non-adherence were similar between Vietnam and New Mexico. Parents in both regions identified concern for infant comfort, appearance of a “normal” of foot, or not understanding the importance of bracing to prevent relapses (13). Similar to findings in China, parents in Vietnam also identified disruption in daily activities by bracing as an additional factor leading to non-adherence.
A preliminary study done by Evans et al. evaluating the ICRC-SFD training program in Vietnam found similar progress and challenges that were present in POF and other programs. Similarly, the study found variable Achilles tenotomy completion; however, in that study it was additionally found that the inability to perform the procedure contributed to the incompletion of the Achilles tenotomy. This study also raised bracing availability and parent adherence as other challenges facing the ICRC-SFD practitioners (12).
Limitations of the study included the inability to obtain concrete documentation to confirm patient count estimations made by interviewees. The demographics of those interviewed heavily favored those practicing in Southern Vietnam. In addition, the setting in which these interviews took place occurred primarily with physicians employed at least half time by public hospitals. These hospitals were also primary hospitals within cities and provinces rather than small clinics. Some limitations with interviews may have resulted from conducting the interviews with physicians present in some cases. Often, regardless of the presence of a physician, parents or other family members were hesitant to answer questions regarding difficulties they may have faced in obtaining treatment. This may have stemmed from cultural politeness. Limitation in to the virtual clinic implementation was present as only 2 sites were introduced to the PVF. However, the web conferencing was highly rewarded and future work will need to be done to fully evaluate its implementation.
Though an array of challenges was identified by practitioners and patients, the diffusion of innovation model provides a basis for formulating solutions in conjunction to the current social context in Vietnam. As identified by the multiple surveys, potential areas that can aid in facilitating the Ponseti method include improving communication channels between practitioners and between practitioners and patients, working with the national ministry of health, and continuing partnerships with foreign NGOs.
Potential methods to improving communication channels include: 1) Creating a directory or website to consolidate patient referral systems by identifying Ponseti practitioners. This would also allow for parents to easily find practitioners if they have internet access. 2) Practitioner use of virtual clinics for exchanging ideas and experiences within Vietnam and with providers worldwide. 3) Conferences to strengthen social channels and networking – a crucial interface in spreading innovation. 4) The use of text messaging has been found to improve communication between patients and healthcare providers leading to improved treatment follow up and adherence (14).
Because organizational systems contribute to the relative of adopting new innovations, working with the Vietnamese National Ministry of Health may aid in ensuring widespread education of clubfoot treatment both to the general public and to various healthcare fields. In addition, partnership with the VNMH may catalyze a system wide solution for improving communication between practitioners and patients in different hospitals and provinces.
Much of the progress the Ponseti method has encountered in Vietnam is due to the tireless dedication of practitioners essentially volunteering their time to face the challenges of treating clubfoot. At the same time, partnership with foreign NGOs have helped continue to build interest in the Ponseti method and also provide much needed support for Ponseti providers, whether in training sessions or finding ways to improve diffusion of the Ponseti method in Vietnam. Continued partnerships with NGOs will doubtlessly be necessary to enable the children of Vietnam access to life changing Ponseti method.
In conclusion, the identified progress and challenges mirrored that of similar studies done in other countries with several factors affecting progress. Focusing on improving communication channels and networking while working with the ministry of health may improve the facilitation of the Ponseti method in Vietnam. Further implementation and evaluation of the PVF may act as a guide for current and future programs in Vietnam or other countries.
Acknowledgments
This author would like to acknowledge Drs. Vo Quang Dinh Nam, Tran Quoc Tuan, Nguyen Cong Hoang, Du-ong Thanh Binh, Le Dinh An, Nguyen Ba Minh Phuoc, Pham Dong Doai, Angela Evans, and the Prosthetics Outreach Foundation for their site support and collaboration. Grants for the study were received from the Arnold P. Gold Foundation and the University of Iowa Medical Student Research Program.
Appendix 1
Clubfoot Questionnaire (For Healthcare Providers)
-
1.
Confirm name of provider:
-
2.
Confirm contact information:
-
3.
Where is your practice located (City/Province)?
-
4.
What type of physician are you?
-
5.
Where are your patients primarily from?
-
6.
How many clubfoot patients do you treat annually (per month)?
-
7.
What methods did you use last year to treat clubfoot?
-
8.
Who follows up on patients? (Nurse? Physician? Other? None?)
-
9.
Have you been trained in the Ponseti method?
-
10.
When did this training occur?
-
11.
Where did this training occur?
-
12.
What type of training? (theory/practice/both)
-
13.
How much did training cost?
-
14.
How many clubfoot patients have you treated since the training?
-
15.
How many clubfoot patients have you treated using the Ponseti method?
-
a.
Short or long leg casts?
-
b.
Achilles tenotomy? (Always/Sometimes/Never)
-
c.
What kind of braces? (shoes, AFOs, foot abduction-bar, others?)
-
d.
Do you anesthetize patients? (Yes/No) How often?
-
e.
Do you combine with massage? (Yes/No)
-
f.
Do you combine with physical therapy? (Yes/No)
-
g.
What criteria do you use to select the treatment to use for clubfoot patients? (Age/Complexity/Other)
-
a.
-
16.
Since your Ponseti training, how many patients have you treated using other methods? How many using surgery?
What other methods have you used?
-
17.
What do you feel are barriers for the Ponseti method?
-
a.
The method itself? (Yes/No, Explain)
-
b.
For providers? (Yes/No, Explain)
-
c.
For the healthcare system in China? (Yes/No, Explain)
-
d.
For patients/culture/parents (e.g. patient doesn't want to wear braces; parents don't force patients to wear braces; stigma of brace;)? (Yes/No, Explain)
-
e.
Physical barriers/distance/transportation? (Yes/No, Explain)
-
f.
Financial barriers for patients? (Yes/No, Explain)
-
g.
Financial barriers for providers/hospitals? (Yes/No, Explain) (for example, if using the Ponseti method causes physicians/hospitals to receive lower income when compared with other methods.
-
a.
-
18.
How do you think neglected clubfoot can be prevented/How do you think we can reduce the time before patients with clubfoot are identified and treated?
-
19.
Do you have an electronic file of clubfoot data you would be willing to share?
-
20.
If the information we discussed is published, there will be no identifiers. Thank you for your time. Your answers are very helpful for this study. Do you have any questions?
References
- 1.Morcuende Jose A. “Congenital Idiopathic Club-foot: Prevention of Late Deformity and Disability by Conservative Treatment With the Ponseti Technique.”. Pediatric Annals. 2006;35(2):128–30. doi: 10.3928/0090-4481-20060201-13. Feb; 132-6. [DOI] [PubMed] [Google Scholar]
- 2.Saltzman Hanna M. “Foot Focus: International Initiative to Eradicate Clubfeet Using the Ponseti Method.”. Foot & Ankle International. 2009;30(5):468–71. doi: 10.3113/FAI-2009-0468. May. [DOI] [PubMed] [Google Scholar]
- 3.Evans Angela M, Thanh Do V. “A Review of the Ponseti Method and Development of an Infant Club-foot Program in Vietnam.”. J Am Podiatr Med Assoc. 2009;99(4):306–1. doi: 10.7547/0980306. Jul-Aug. [DOI] [PubMed] [Google Scholar]
- 4.Rogers Everett. Diffusion of Innovation. NY: Free Press; 2003. [Google Scholar]
- 5.Lu Ning, Zhao LI, Du Qing, Liu Yakun, Oprescu Florin, Morcuende Jose. “From Cutting to Casting: Impact and Initial Barriers to the Ponseti Method of Clubfoot Treatment in China.”. Iowa Orthop J. 2010;30:1–6. [PMC free article] [PubMed] [Google Scholar]
- 6.McElroy T, Konde-Lule J, Neema S, Gitta S. Uganda Sustainable Clubfoot Care. “Understanding the Barriers to Clubfoot Treatment Adherence in Uganda: a rapid ethnographic study.”. Disability and Rehabilitation. 2007;29(11–12):845–55. doi: 10.1080/09638280701240102. June. [DOI] [PubMed] [Google Scholar]
- 7.Staheli lynn. Clubfoot: Ponseti Management. Global Help. 3rd Edition. 2009. Available from www.global-help.org. [Google Scholar]
- 8.Herzenberg JE, Radler C, Bor N. “Ponseti versus traditional methods of casting for idiopathic clubfoot.”. Pediatr Orthop. 2002;22(4):517–21. July-August. [PubMed] [Google Scholar]
- 9.Ippolito E, Farsetti P, Caterini R, Tudisco C. “Long-term comparative results in patients with congenital clubfoot treated with two different protocols.”. J Bone Joint Surg Am. 2003;85-A(7):1286–1294. doi: 10.2106/00004623-200307000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Siapkara A, Duncan R. “Congenital talipes equi-novarus Review of current management.”. J Bone Joint Surg Br. 2007;89-B:995. doi: 10.1302/0301-620X.89B8.19008. [DOI] [PubMed] [Google Scholar]
- 11.Berwick Donald. “Disseminating Innovations in Health Care.”. JAMA. 2003;289(15):1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 12.Evans Angela. “Preliminary evaluation of implementing the Ponseti method for correction of clubfoot in Vietnam.”. J Child Orthop. 2010;4:553–559. doi: 10.1007/s11832-010-0290-6. September. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avilucea Frank, Szalay Elizabeth, Bsch Patrick, Sweet katherine, Schwend Richard. “Effects of Cultural Factors on Outcome of Ponseti Treatment of Clubfeet in Rural America.”. J Bone Joint Surg Am. 2009;91:530–40. doi: 10.2106/JBJS.H.00580. [DOI] [PubMed] [Google Scholar]
- 14.Mahmud Nadim, Rodriguez Joce, Nesbit Josh. “A text message-based intervention to bridge the healthcare communication gap in the rural develop ing world.”. Technology and Health Care. 2010;18:137–44. doi: 10.3233/THC-2010-0576. [DOI] [PubMed] [Google Scholar]


