Abstract
Injuries of the posteromedial corner of the knee are relatively common. These can be isolated or combined with other ligament lesions. In some cases the treatment of postero-medial corner injuries is controversial. After a brief description of the anatomy and biomechanics of the medial side of the knee, this paper reviews the indications for isolated and multiligamentous medial/posteromedial corner injuries both in the acute and in the chronic setting. In addition, the most common surgical techniques for repair and reconstruction are described in addition to outcomes based upon a review of the literature.
Introduction
Injuries to the medial collateral ligament (MCL) and posteromedial corner of the knee are very common and can be isolated or combined with other ligamentous lesions. A thorough understanding of the anatomy of the medial side of the knee is essential for a correct diagnosis and appropriate treatment. The high reparative potential of the MCL with conservative treatment and the complications (primarily knee stiffness) associated with surgical repair/reconstruction are at the base of the controversies regarding the treatment of medial/posteromedial ligamentous injuries. No decision algorithms are available and a wide variety of surgical techniques have been described regarding this topic. These include direct repair, capsular plication, and reconstruction procedures. The goal of this review is to discuss the indications, most common techniques, and outcomes of medial/posteromedial ligamentous injuries of the knee.
Anatomy and Biomechanics
The anatomy of the medial side of the knee has been extensively described by LaPrade et al1. The structures of the medial side of the knee include: 1) bony landmarks (medial epicondyle, adductor tubercle, gastrocnemius tubercle on the femur, medial tibial plateau, and the medial aspect of the patella), 2) ligaments (superficial medial collateral ligament, deep medial collateral ligament, posterior oblique ligament, medial patello-femoral ligament, and the postero-medial capsule), and 3) tendons (adductor magnus, medial head of the gastrocnemius, semimembranosus, and the pes anserinus). A thorough knowledge of the anatomy is essential in diagnosing and treating injuries to the medial side of the knee.
The superficial medial collateral ligament (sMCL) has one femoral and two tibial attachments (proximal and distal). The femoral attachment has an oval shape and is located 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. The proximal tibial attachment is primarily to soft tissues, mainly to the anterior arm of the semimembranosus tendon. The distal tibial attachment of the sMCL is just anterior to the posteromedial crest of the tibia (Fig 1). The average distance of the proximal tibial attachment is 12.2 mm from the tibial joint line. The average distance of the distal tibial attachment is 94.8 mm from the femoral attachment, and 61.2 mm from the tibial joint line. The average distance from the distal tibial attachment to proximal tibial attachment is 49.2mm1.
Figure 1. A) Medial view of the knee: attachment sites (Redrawn from: laprade Rf et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000–10). B) Medial aspect of the knee. C) sMCl distal tibial insertion. AT= adductor tubercle, ME= medial epicondyle, sMCl= superficial medial collateral ligament, Mpfl= medial patellofemoral ligament, and pOl= posterior oblique ligament. Mf= Meniscofemoral, MT= Meniscotibial, SM= Semimembranosus tendon, vMO= vastus medialis obliquus, GT= Gastrocnemius tendon, pES= pes Anserinus.
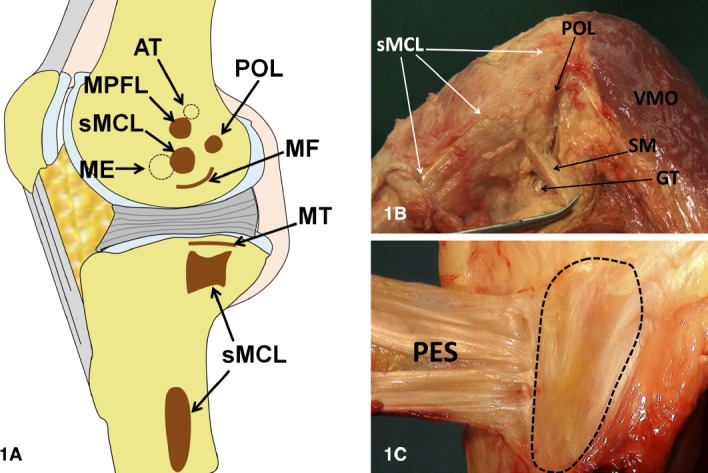
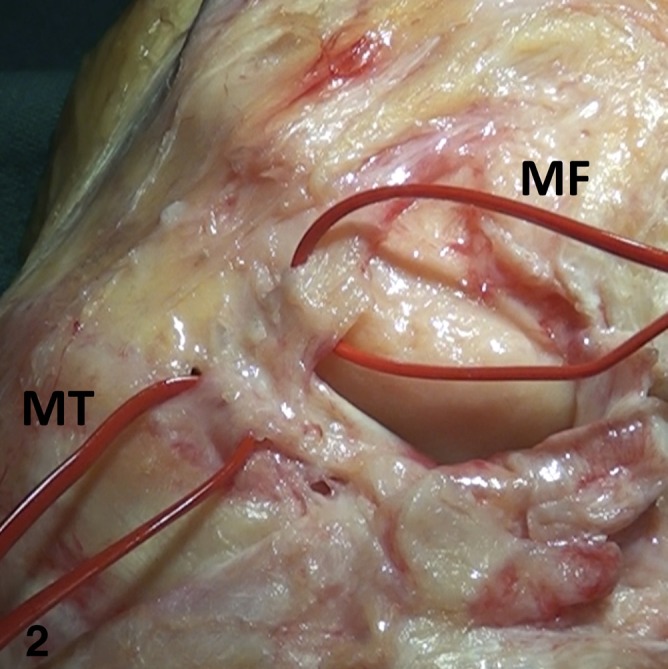
The deep medial collateral ligament (dMCL) is a thickening of the medial joint capsule. The dMCL consists of the meniscofemoral (MF) and meniscotibial (MT) ligaments (Fig 2). The MF ligament is longer than the MT ligament and its attachment is located 15.1 mm posterior and distal to the medial epicondyle The MT ligament is shorter, thicker and attaches just distal (3.2 mm average) to the cartilage of the medial tibial plateau1.
Figure 2. Deep medial collateral ligament. Mf= meniscofemoral ligament, MT= meniscotibial.
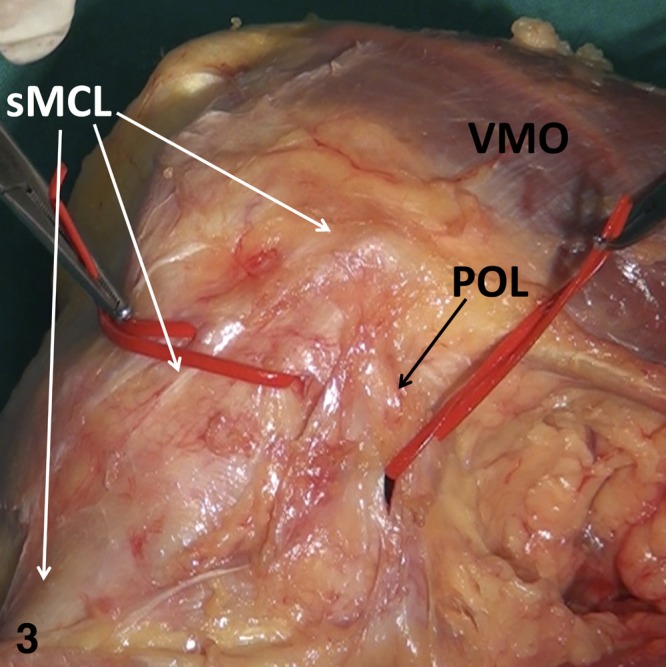
The posterior oblique ligament (POL) consists of 3 fascial attachments: superficial, central (tibial), and capsular. The 3 attachments course off the distal aspect of the semimembranosus tendon mainly, but also off the medial meniscus, posteromedial tibia, and medial head of the gastrocnemius (Fig 3). On average, the POL attaches on the femur 7.7 mm distal and 6.4 mm posterior to the adductor tubercle and 1.4 mm distal and 2.9 mm anterior to the gastrocnemius tubercle1.
Figure 3. Medial view of the knee. pOl= posterior oblique liga-ment, sMCl= superficial medial collateral ligament, vMO= vastus medialis obliquus.
Biomechanically, the MCL represents the main restraint to valgus forces and a secondary restraint to external/internal rotation and posterior translation of the tibia. The sMCL provides the greatest stability to valgus forces over the entire range of motion. The contribution of the sMCL to internal rotation stability increases beyond 30° of knee flexion when the posteromedial capsule is slackened. Sectioning the dMCL, if the sMCL is intact, produces almost no changes in terms of medial stability2. Conversely, the postero-medial capsule is in tension and provides some stability to valgus forces, posterior tibial translation, and internal rotation only with the knee extended3. The POL is able to provide both secondary stability to tibial internal and external rotation at early knee flexion and posterior stability to the tibia in knee extension The role of the POL becomes even more pronounced in the setting of MCL deficiency in both valgus and rotational stability4,5.
Clinical Examination and Imaging
During the clinical evaluation, an accurate history will lead the practitioner to suspect a medial sided knee injury when the traumatic mechanism includes a valgus force. Abnormalities in the gait should be noticed and the knee is evaluated for hemarthrosis or malalignment. Palpation along the course of the MCL may demonstrate tenderness to palpation suggestive of an MCL injury. Tenderness over the adductor tubercle or proximal medial tibia may indicate injury at the origin or insertion sites of the MCL. Pain over the medial joint line may indicate an associated medial meniscus tear.
The stability of the knee is then tested in all planes in order to evaluate antero-posterior, lateral, and rotational instability. Anteromedial rotatory instability is detected by performing the anterior drawer test while holding the tibia in external rotation. Any evidence of anterior subluxation of the medial tibial plateau during a valgus stress test with the knee in 30 degrees of flexion might also indicate the presence of anteromedial rotatory instability. Valgus stress should be performed at 0 and 30° of knee flexion. Although the American Medical Association classification is a valuable system, the authors prefer the Fetto & Marshall classification6. The Fetto & Marshall classification divides medial sided knee injuries into: grade 1 (no valgus laxity), grade 2 (valgus laxity at 30° of flexion) and grade 3 (valgus laxity at 0° and 30°). As mentioned, valgus instability at 30° of flexion (when the postero-medial capsule is slackened) is suggestive of a tear of the sMCL. On the other hand, with valgus instability at full extension both sMCL and postero-medial capsule are likely to be torn.
Weight bearing radiographs of the knee are obtained in antero-posterior and lateral views. If valgus malalignment is present a weight bearing long leg radiograph is obtained.
MRI is helpful in diagnosing associated bone and soft tissue injuries (anterior and posterior cruciate ligaments, postero-lateral corner, and medial meniscus) as well as determining the location and extent of medial/posteromedial ligamentous injuries.
Treatment Options
Conservative treatment consists of a hinged knee brace with weight bearing as tolerated and crutches for initial pain relief. The patient can start isometric and range of motion exercises immediately. Crutches are discontinued when the patient can walk without limping.
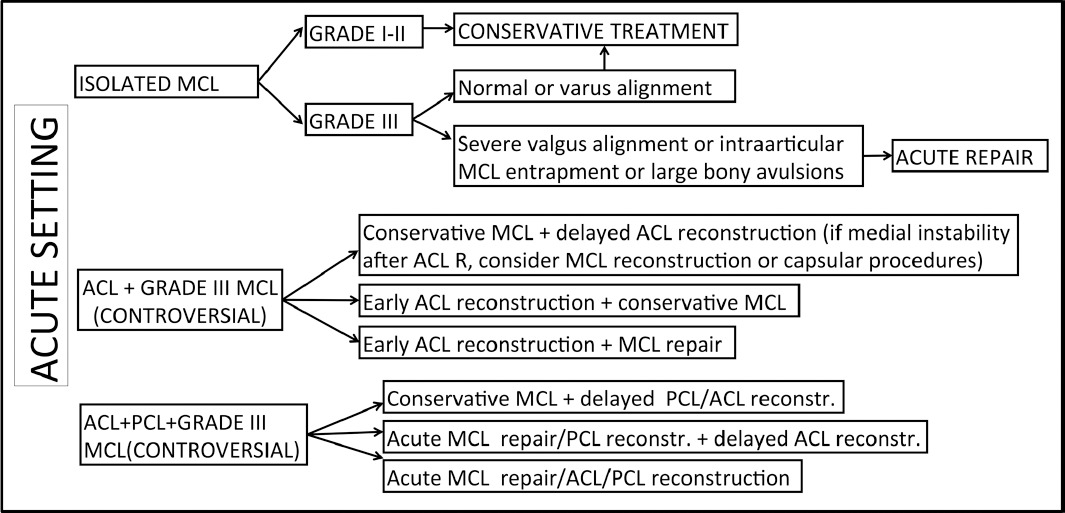
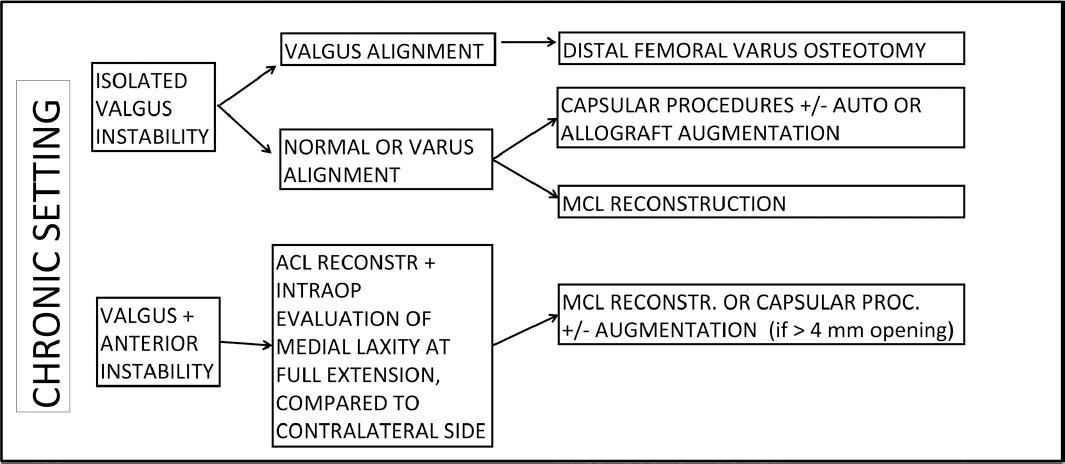
The indications for the treatment of medial side injuries of the knee in the acute and chronic setting are summarized in Table 1 and 2 respectively. The tables describe the algorithm of treatment derived from the review of the literature, with the possible options for every specific scenario. Key points in the decision making are: 1) chronicity of the MCL rupture (acute is considered < 3 weeks, subacute 3–6 weeks, and chronic >6 weeks); 2) alignment; 3) the presence of bony avulsions; or 4) MCL entrapment. In the acute setting, a grade I or II MCL can be managed conservatively. Conservative treatment can also be indicated in grade III MCL tears with neutral or varus limb alignment. In there is severe valgus alignment, intraarticular MCL entrapment, or large bony avulsions an acute MCL repair is indicated. The treatment of combined anterior cruciate ligament and grade III MCL tears is controversial. The first option is to conservatively treat the MCL and after 3–4 weeks perform an ACL reconstruction. If the knee is still unstable medially after the ACL reconstruction, an MCL reconstruction or capsular procedure can be concurrently performed. Alternatively, an early ACL reconstruction can be performed with conservative management of the MCL, in order to allow MCL healing with a more stable knee. The third option is a combined early ACL reconstruction with an acute MCL repair. The treatment is controversial also in case of combined ACL, PCL, and grade III MCL injuries. The treatment options include: 1) conservative management of the MCL with delayed ACL/PCL reconstruction; 2) acute MCL repair combined with PCL reconstruction and delayed ACL reconstruction; or 3) acute MCL repair combined with ACL/PCL reconstruction.
Table 1.
Medial knee instability: indications in the acute setting.
|
Table 2.
Medial knee instability: indications in the chronic setting.
|
In the chronic setting, a distal femoral varus osteotomy should be considered if isolated medial instability is associated with valgus limb alignment. In there is isolated valgus instability with neutral or varus alignment, capsular procedures with or without augmentation or MCL reconstruction are indicated. In the case of combined valgus and anterior instability, ACL reconstruction is performed and the knee is evaluated intraoperatively for medial laxity. If the knee shows at full extension a medial opening greater than 4 mm compared to the contralateral side, capsular procedures or MCL reconstruction can be considered.
Many techniques have been described for the treatment of medial and postero-medial ligamentous injuries of the knee, including: 1) direct repair for selected acute cases, as described above; 2) capsular procedures, which consist in re-tensioning of the lax structures in the subacute/chronic scenarios; and 3) reconstruction procedures. Several different techniques described in the literature are reviewed below7–17. Currently there is no evidence regarding the surgical timing and treatment decision making with regards to which type of procedure or technique to use (i.e. capsular procedures versus reconstruction).
Surgical Approach
Examination under anesthesia is performed to completely assess the injury. Arthroscopy can be used to rule out any other associated lesions and to determine the site of the dMCL injury. In the acute setting, arthroscopy should be performed quickly and with gravity inflow, to minimize fluid extravasation. A hokey-stick (or longitudinal) incision is made from the medial proximal tibia to the medial femoral epicondyle, curving posteriorly in line with the intermuscular septum. For isolated repairs either distally or proximally, a more limited approach is used. In case of MCL reconstruction, some authors prefer a 2 incision approach to the femur and tibia. Attention should be paid to preserve the saphenous nerve. The crural and sartorial fascia is incised longitudinally. Hematoma is removed. The injured structures are then identified7.
Repair Technique
The injured structures are identified and should be repaired from the deepest structure outward. A peripheral tear of the medial meniscus is commonly seen (33%) and repaired with an open technique7. A MF ligament tear can be directly repaired using sutures alone or suture anchors. Suture anchor fixation is preferred for MT ligament tears (Fig 4A,B,C). If injured, the POL is repaired by direct suture back to the femur. Repair of the deep structures is completed with the knee held in varus and full extension7.
Figure 4. Repair technique. A,B,C) A meniscotibial ligament tear repaired with suture anchor fixation. D,E,F) Femoral avulsion of the sMCL repaired using suture Richard's staples.
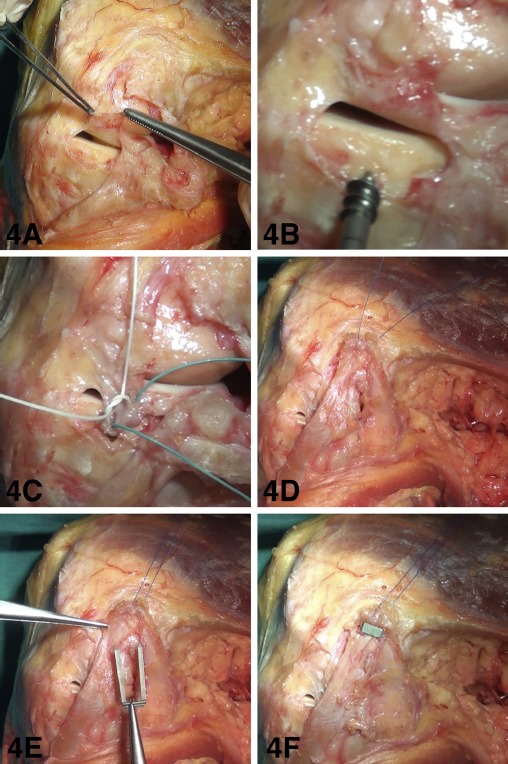
Femoral avulsion of the sMCL leaves the best tissue for repair using suture anchors, staples, or a screw and washer (Fig 4D,E,F). However, repair in this location is associated with post-operative stiffness more than in other locations8. Acute complete avulsions off of the tibia can be repaired using either suture anchors or staples7.
The semimembranosus portion of the POL can be repaired with interrupted absorbable sutures and sutured to the posterior border of the MCL in a pants-over-vest fashion. Occasionally, mid-substance and tibial-sided injuries require augmentation, due to the poor soft tissue quality. The sMCL is fixed at 30° of knee flexion7.
Capsular Procedures
Re-tensioning of the posteromedial structures
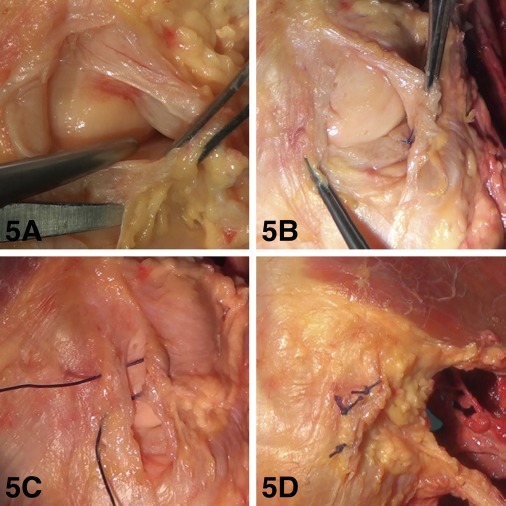
The surgical approach and dissection are carried out as described for the repair. The meniscus and the posteromedial structures are visualized and probed for laxity. The goal of this technique is to remove the laxity from the injured posteromedial structures by creating increased distance between the origin and insertion. The posteromedial capsule needs to be released from the meniscus and re-sutured to it in a more advanced position (Fig 5A,B). Then the lax structures are attached to an adjacent intact structure in a pants-over-vest fashion (i.e. lax POL is advanced forward and sutured to the intact sMCL) 9,10(Fig 5C,D).
Figure 5. Re-tensioning of the posteromedial structures. A,B) The posteromedial capsule is released from the meniscus and sutured to it in a more advanced position. C,D) The lax structures are re-approximated in a pants-over-vest fashion.
En masse elevation
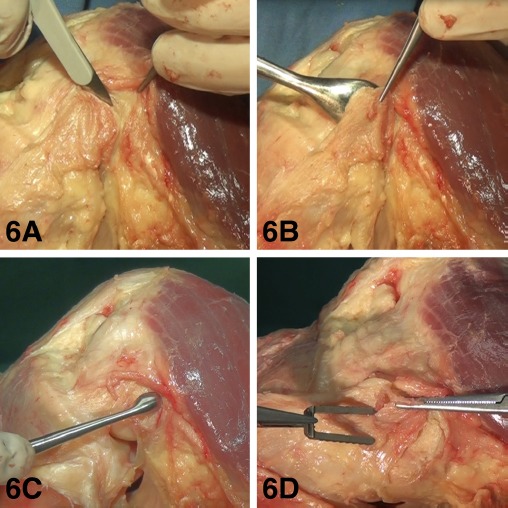
This procedure is indicated when a generalized laxity of the postero-medial structures is present. The weakest point (femoral or tibial) should be identified. The structures at the weakest attachment must be released as an entire tendon/ligament unit (en masse) (Fig 6A,B). This unit must be armed with sutures, re-tensioned, and fixed back to an isometric point on the bone. The bone around the isometric point is ‘‘roughed-up’’ until good bleeding is achieved (Fig 6C). Fixation can be achieved with staples or suture anchors9. (Fig 6D)
Figure 6. En masse elevation. A,B) The structures at the weakest attachment are released as an entire tendon/ligament unit (en masse). C) The bone around the isometric point is decorticated until good bleeding is achieved. D) Fixation of the entire complex can be accomplished with staples or suture anchors.
Reconstruction Techniques
Kim's technique
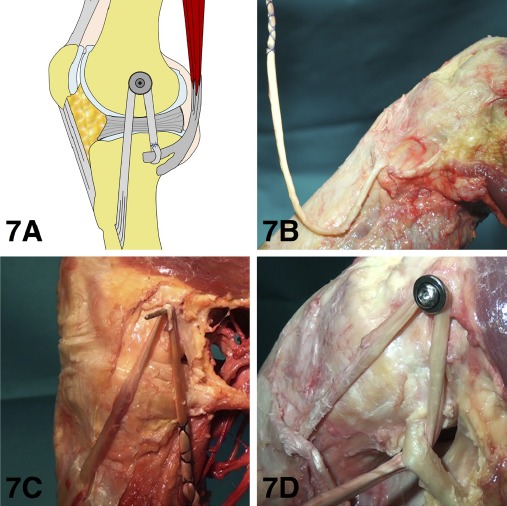
The semitendinosus is harvested, preserving the tibial attachment (Fig 7B). A K wire is inserted on the anterosuperior border of the medial femoral epicondyle. The semitendinosus tendon is looped around the wire and isometricity (<2 mm migration) is tested by pulling the suture at the tendon and moving the knee through a full ROM (Fig 7C). A 6.5 mm cancellous screw and an 18 mm washer are placed through a hole, drilled 9 mm (the radius of a washer) proximal to the isometric point (Fig 7D). Decortication is performed around the drill hole. After manual tensioning of the graft, the screw is tightened with the knee in 30° of flexion and varus stress. The free end of the graft is pulled under the direct head of the semimembranosus tendon and sutured to the tendon itself in 30° of knee flexion11.
Figure 7. kim's technique (see text). B) The semitendinosus is harvested preserving the tibial attachment. C) The semitendinosus tendon is looped around the k wire. D) A 6.5 mm cancellous screw and an 18 mm washer are placed into a tunnel drilled 9 mm (the radius of a washer) proximal to the isometric point on the femur.
Stannard's technique
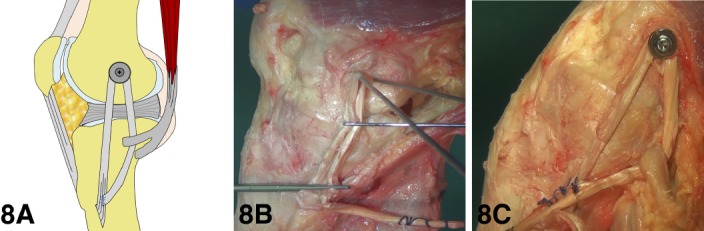
In Stannard's modification of Kim's technique12, the free end of the semitendinosus is sutured to the intact insertion of the semitendinosus itself on the tibia (Fig 8B,C). The graft is tensioned with the knee in approximately 40° of flexion and a slight varus stress.
Figure 8. A) Stannard's modification of kim's technique (see text). B) Evaluation of isometry of the graft. C) The free end of the semitendi-nosus is sutured to the intact insertion of the semitendinosus on the tibia.
Lind's technique
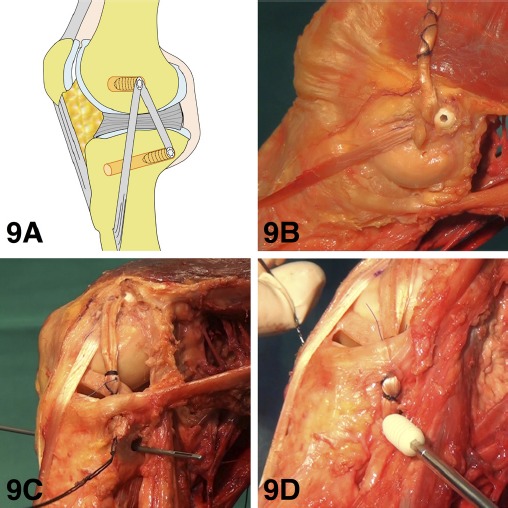
Incision, semitendinosus harvesting, and isometricity evaluation are as described by Kim. A tunnel (diameter of the double-looped tendon) is drilled in the isometric point. The tendon loop is then armed with a baseball suture, passed into the tunnel and fixed with an interference screw (same diameter as the tunnel) (Fig 9B). This is performed with the knee in 10° of flexion and neutral rotation. A tibial tunnel (same size of the graft) is then drilled in the posterior corner of the medial tibial condyle from anterior to posterior. The drill hole is aimed to exit 10 mm below the tibial plateau, posterior and lateral to the semimembranosus insertion. The free end of the graft is passed through the posterior tibial tunnel opening, and fixed here with an interference screw (same diameter as the tunnel) to reconstruct the posteromedial corner (Fig 9C,D). This is tightened with the knee in 60° of flexion and neutral rotation13.
Figure 9. A) Lind's technique (see text). B) The tendon loop is armed in a baseball suture fashion, passed into the tunnel and fixed with an interference screw. C,D) The free end of the graft is passed through the posterior tibial tunnel opening, and fixed here with an interference screw.
Yoshiya's technique.
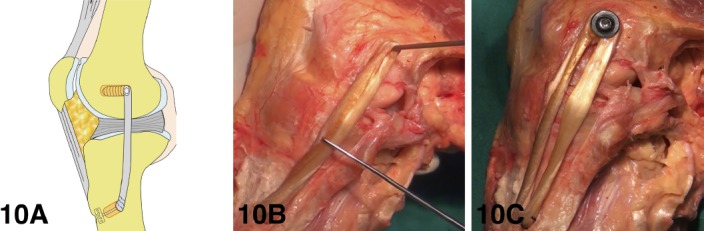
Two skin incisions (6–7 cm) are made at the proximal and distal insertions of the sMCL. The semitendinosus and gracilis tendons are harvested, detached distally, and each of them made into a single- or double-stranded tendon graft. Two sutures with an extracortical fixation device are attached to 1 end of the graft, while stay sutures are placed at the other end. The center of the insertion of the sMCL is selected as the distal attachment of the neoligament, while the proximal attachment is the medial epicondyle. Isometricity is evaluated with adjustments mainly on the femoral side (Fig 10B). The distal end is fixed with the extracortical device, and the proximal end with an interference screw or soft tissue screw and washer with the knee in 30° of flexion and a varus stress) (Fig 10C) 14.
Figure 10. A) Yoshiya's technique (see text). B) The center of the insertion of the sMCL is selected as the distal attachment of the reconstructed ligament, while the proximal attachment is the medial epicondyle. C) The distal end is fixed with an extracortical device, and the proximal end with an interference screw or soft tissue screw/washer.
Coobs, wijdicks et al. technique.
The technique consists of a reconstruction of the two main structures (sMCL and POL) of the medial side of the knee with use of two separate grafts with four reconstruction tunnels (Fig 11B,C,D).
Figure 11. A) Coobs, Wijdicks et al. technique (see text). B,C,D) Reconstruction of the sMCL and POL with the use of two separate grafts and four reconstruction tunnels.
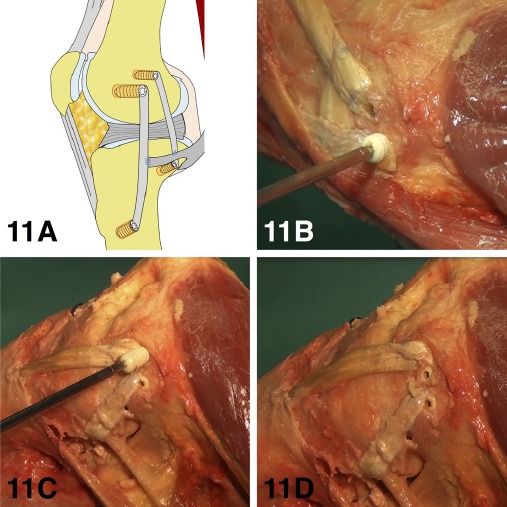
Allografts or gracilis and semitendinosus autografts can be used. Isometricity is evaluated with K wires and sutures for both bundles. Correctly sized tunnels are drilled at the isometric points. The sMCL is tightened at 30° of knee flexion and the POL is tightened at 0°. Fixation is achieved with interference screws15,16.
Borden's technique
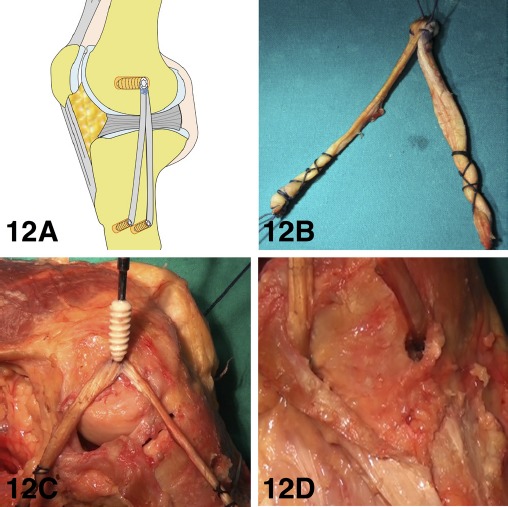
With a 2-incision approach, a passing pin is drilled into the medial epicondyle. Next, the suture is looped over the passing pin in the femoral epicondyle. The suture is then passed along the MCL and pulled from the tibial incision.
Isometry is tested by holding the suture at the anterior aspect of the MCL tibial insertion and moving the knee through a full range of motion. A pin is placed into the tibia at the isometric point. The hamstring tendons are then retracted posteromedially. The isometric point for a posterior tibial tunnel is then determined in a similar fashion. A second Steinmann pin is placed.
A tibialis anterior tendon is prepared in a double-bundle loop (Fig 12B). The femoral tunnel is drilled to a depth of 30 mm, and the tibial tunnels to a depth of 25 mm (same size as the graft ends). The graft is then pulled into the femoral tunnel and fixed with an interference screw (Fig 12C). The free ends of the allograft are then passed down the soft-tissue plane and retrieved from the tibial incision (Fig 12D). The posterior bundle is fixed with an interference screw with the knee in internal rotation and 60° of flexion. The anterior bundle is fixed in the same way, but with the leg internally rotated and flexed to 30°17.
Figure 12. A) Borden's technique (see text). B) A tibialis anterior tendon allograft is prepared in a double-bundle loop. C) The graft is pulled into the femoral tunnel and fixed with an interference screw. D) The free ends of the allograft are passed down the soft-tissue plane and retrieved from the tibial incision.
Tips to find the isometric point
Finding the isometric point on the tibia, but mostly on the femur is essential to achieve good stability and avoid stiffness after MCL reconstruction. Three different methods can be used to find the isometric points:
1) Two K wires can be positioned at the presumptive isometric points. A suture is then looped around the K wires and held with a Kelly clamp. In case of isometricity the suture should have the same tension throughout the full range of motion (Fig. 13A).
Figure 13. Techniques to find the isometric points (see text).
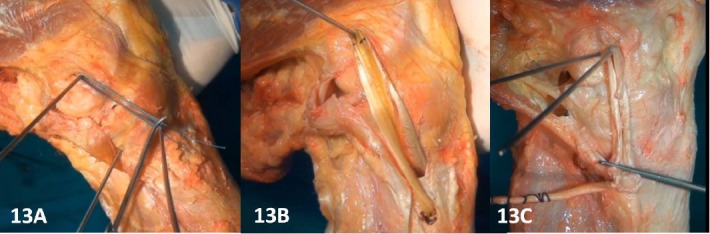
2) Alternatively, when a hamstring graft is left attached distally, a k wire is positioned at the isometric point on the femur, the graft is looped around it and marked with a surgical marker. The knee is then taken through a full range of motion. Displacement of the marks with respect to the K wire greater than 2 mm indicates a non isometric point on the femur (Fig. 13B)11.
3) Last, the graft can be looped around the K wire positioned at the presumptive isometric point on the femur and held with a Kelly clamp. If the graft is isometric, it will show uniform tension throughout a full range of motion (Fig. 13C).
Authors' preferred technique and post-operative rehabilitation
The authors' preferred technique is Kim's procedure. This technique is favored because it is easy, reliable, inexpensive, and allows for both sMCL and POL reconstruction. Although controversies exist regarding the most reliable surgical technique for reconstruction, isometricity is essential to obtain favorable results.
Post-operatively, the patient is kept in a hinged knee brace with protected weight bearing. Passive range of motion from 0 to 90 degrees is begun immediately. Hyperextension and flexion over 90 degrees should be avoided during the first 2 weeks. Isometric and closed kinetic chain strengthening are allowed immediately. Full range of motion is allowed 2 weeks after surgery, and full weight bearing is allowed 6 weeks after surgery. Return to full activities is generally allowed 6 months after surgery.
Outcomes
The outcomes are summarized in Table 3. Derscheid et al18 described the results of conservative treatment for acute grade I and II MCL injuries in 51 football players. They reported excellent outcomes for both groups, with a slightly longer recovery for grade II injuries. Similar results were reported by Lundberg19. Indelicato et al20 showed good or excellent results with conservative treatment for acute grade III injuries. Reider22 described similar results between early functional rehabilitation and surgery or immobilization for acute grade III MCL injuries. On the other hand Kannus et al. 21 showed poor results of conservative treatment for grade III injuries, with subsequent medial instability, dysfunction of the ACL, muscle weakness, and arthritis. Hughston et al23,24 reported excellent results with acute surgical repair of the medial side of the knee for anteromedial instability 2+ or more. Good results were reported in the acute and chronic setting after reconstruction procedures11,13,14.
Table 3.
Summary of the outcomes of conservativetreatment, repair, and reconstruction for knee medial instability.
| Author (year) | Type of injury | Acute/Chronic | N° patients | Treatment | Follow-up | Outcomes |
|---|---|---|---|---|---|---|
| Derscheid (1981)18 | Grade I-II | Acute | 51 (football players) | Conservative | Grade 1: return to play 10.6 days postinjury. Grade II: return to play 19.5 days post-injury |
|
| Lundberg(1996)19 | Grade I-II | Acute | 38 | Conservative | 10 years | At 4 years average Lysholm score |
| Indelicato (1990)20 | Grade III | Acute | 21 (football players) | Conservative | 46 months | Good or excellent results in 20 cases, average return to sport 9.2 weeks |
| Kannus (1988)21 | Grade II and III | Acute | 81 | Conservative | Long-term | Grade II: good results. Grade III: medial instability, dysfunction of the ACL, muscle weakness, and arthritis |
| Reider (1994)22 | Grade III | Acute | 35 athletes | Early functional rehabilitation | 5.3 years | Mean HSS score 45.9 (comparable to surgery and immobilization) |
| Hughston(1983)23 | Anteromedial instability 2+ or more | Acute | 89 | Surgical repair | 7.8 years | 94% back to preinjury level of performance |
| Hughston (1994)24 | Anteromedial instability 2+or more | Acute | 41 | Surgical repair | 20 years | 93% of good results and 7% of failures |
| Kim (2008)11 | Chronic | 24 | Reconstruction | >2 years | mean Lysholm score 91.9, and medial opening <2mm in 22 patients | |
| Lind (2009)13 | Grade 3 or 4 (IKDC) medial instability (with or without ACL, PCL, PLC) | Chronic | 50 | Reconstruction | >2 years | 98% of normal or nearly normal medial stability. 91% of subjective satisfaction. |
| Yoshlya(2005)14 | Grade III medial instablity | Acute and Chronic | 24 | Reconstruction | >2 years | 100% of normal or nearly normal IKDC score |
As shown in the outcomes table, the studies available in the literature are mostly case series, with heterogeneous study groups (with or without associated ligamentous injuries), and using different medial laxity grading systems or outcome scores. In light of these considerations, comparisons between the results reported between the studies are difficult to make.
Conclusion
Understanding of the anatomy of the medial side of the knee, correct indications, and precise surgical technique are essential to achieve good results in the treatment of medial/postero-medial knee instability. The majority of patients who sustain MCL injuries of varying severity can achieve pre-injury activity level with nonoperative treatment alone. However, the treatment of grade III MCL injuries (with gross valgus instability at 0° of flexion) is still controversial. The most severe injuries (especially with severe valgus alignment, intra-articular MCL entrapment, large bony avulsions, or multiple ligament involvement) may require acute operative repair or augmentation. In addition, surgical reconstruction is indicated for isolated symptomatic chronic MCL laxity.
References
- 1.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000–10. doi: 10.2106/JBJS.F.01176. Sep. [DOI] [PubMed] [Google Scholar]
- 2.Warren LF, Marshall JL, Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am. 1974;56:665–674. [PubMed] [Google Scholar]
- 3.Grood ES, Noyes FR, Butler DL, et al. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63:1257–1269. [PubMed] [Google Scholar]
- 4.Haimes JL, Wroble RR, Grood ES, et al. Role of the medial structures in the intact and anterior cruciate ligament-deficient knee. Limits of motion in the human knee. Am J Sports Med. 1994;22:402–409. doi: 10.1177/036354659402200317. [DOI] [PubMed] [Google Scholar]
- 5.Petersen W, Loerch S, Schanz S, et al. The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament-deficient knee. Am J Sports Med. 2008;36:495–501. doi: 10.1177/0363546507310077. [DOI] [PubMed] [Google Scholar]
- 6.Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop. 1978;132:206–18. [PubMed] [Google Scholar]
- 7.Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77–90. [PMC free article] [PubMed] [Google Scholar]
- 8.Robins AJ, Newman AP, Burks RT. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med. 1993;21(1):20–5. doi: 10.1177/036354659302100104. [DOI] [PubMed] [Google Scholar]
- 9.Benjamin Jackson J, 3rd, Ferguson CM, Martin DF. Surgical treatment of chronic posteromedial instability using capsular procedures. Sports Med Arthrosc. 2006;14(2):91–5. doi: 10.1097/01.jsa.0000212310.39699.70. Jun. [DOI] [PubMed] [Google Scholar]
- 10.Hughston JC, Knee ligaments . Injury and Repair. St Louis: Mosby-Year Book; 2003. pp. 149–241. [Google Scholar]
- 11.Kim SJ, Lee DH, Kim TE, Choi NH. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br. 2008;90(10):1323–7. doi: 10.1302/0301-620X.90B10.20781. Oct. [DOI] [PubMed] [Google Scholar]
- 12.Stannard JP. Medial and posteromedial instability of the knee: evaluation,treatment, and results. Sports Med Arthrosc. 2010;18(4):263–8. doi: 10.1097/JSA.0b013e3181eaf713. Dec. [DOI] [PubMed] [Google Scholar]
- 13.Lind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med. 2009;37(6):1116–22. doi: 10.1177/0363546509332498. Jun. [DOI] [PubMed] [Google Scholar]
- 14.Yoshiya S, Kuroda R, Mizuno K, Yamamoto T, Kurosaka M. Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med. 2005;33(9):1380–5. doi: 10.1177/0363546504273487. Sep. [DOI] [PubMed] [Google Scholar]
- 15.Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92(5):1266–80. doi: 10.2106/JBJS.I.01229. May. [DOI] [PubMed] [Google Scholar]
- 16.Coobs BR, Wijdicks CA, Armitage BM, Spiridonov SI, Westerhaus BD, Johansen S, Engebretsen L, LaPrade RF. An in vitro analysis of an anatomical medial kne reconstruction. Am J Sports Med. 2010;38:339–47. doi: 10.1177/0363546509347996. [DOI] [PubMed] [Google Scholar]
- 17.Borden PS, Kantaras AT, Caborn DN. Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy. 2002;18(4):E19. doi: 10.1053/jars.2002.32235. Apr. [DOI] [PubMed] [Google Scholar]
- 18.Derscheid GL, Garrick JG. Medial collateral ligament injuries in football: Nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9:365–368. doi: 10.1177/036354658100900605. [DOI] [PubMed] [Google Scholar]
- 19.Lundberg M, Messner K. Long-term prognosis of isolated partial medial collateral ligament ruptures: A ten-year clinical and radiographic evaluation of a prospectively observed group of patients. Am J Sports Med. 1996;24:160–163. doi: 10.1177/036354659602400207. [DOI] [PubMed] [Google Scholar]
- 20.Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990;(256):174–7. Jul. [PubMed] [Google Scholar]
- 21.Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1988;(226):103–12. Jan. [PubMed] [Google Scholar]
- 22.Reider B, Sathy MR, Talkington J, Blyznak N, Kollias S. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22(4):470–7. doi: 10.1177/036354659402200406. Jul-Aug. [DOI] [PubMed] [Google Scholar]
- 23.Hughston JC, Barrett GR. Acute anteromedial rotatory instability. Long-term results of surgical repair. J Bone Joint Surg Am. 1983;65(2):145–53. doi: 10.2106/00004623-198365020-00002. Feb. [DOI] [PubMed] [Google Scholar]
- 24.Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1328–44. doi: 10.2106/00004623-199409000-00008. Sep. [DOI] [PubMed] [Google Scholar]


