Abstract
Purpose
Adults with complications from previous hypospadias surgery experience various problems, including urethral stricture, persistent hypospadias and urethrocutaneous fistula. Innate deficiencies of the corpus spongiosum and multiple failed operations makes further management challenging.
Materials and Methods
We reviewed our prospective urethroplasty database of men who presented with complications of previous hypospadias surgery. Patients were included in study if they had greater than 6 months of followup. Our surgical management was defined as an initial success if there were no urethral complications. The overall success rate included men with the same result after additional treatment.
Results
A total of 50 men had followup greater than 6 months (median 89) and were included in study. These 50 patients presented with urethral stricture (36), urethrocutaneous fistula (12), persistent hypospadias (7), hair in the urethra (6) and severe penile chordee (7). Patients underwent a total of 74 urethroplasties, including stage 1 urethroplasty in 19, a penile skin flap in 11, stage 2 urethroplasty in 11, urethrocutaneous fistula closure in 9, permanent perineal urethrostomy in 6, excision and primary anastomosis in 6, a 1-stage buccal mucosa onlay in 4, tubularized plate urethroplasty in 3, combined techniques in 3 and chordee correction in 1. In 25 men (50%) treatment was initially successfully. Of the 25 men in whom surgery failed 18 underwent additional procedures, including 13 who were ultimately treated successfully for an overall 76% success rate (38 of 50).
Conclusions
Managing problems from previous hypospadias surgery is difficult with a high initial failure rate. Additional procedures are commonly needed.
Keywords: urethra, hypospadias, postoperative complications, adult, reoperation
Hypospadias surgery in children has undergone significant evolution in the last decades. Staged surgical approaches have given way to 1-stage repair with excellent long-term results even for proximal hypospadias.1–4 Despite advances in technique some patients have complications and may require multiple surgeries during childhood, adolescence and even into adult-hood. Also, complications can develop with genital maturity in some patients, even those with apparently excellent outcomes during childhood.5 In men who present with urethral stricture, complications of previous hypospadias repair are common. At tertiary centers these complications are the leading cause of iatrogenic urethral stricture in men younger than 45 years.6
Varied problems arise in adults previously treated with surgery for hypospadias, including urethral stricture, persistent hypospadias, urethrocutaneous fistula, diverticulum, urethral calculi, obstruction from hair bearing skin used in previous repair and chordee.7 Men who present with these problems have often undergone multiple surgeries to create a patent urethra with an acceptable-appearing penis. After multiple surgeries the penile skin and urethra are often scarred and lack a normal dependable vascular supply, making additional surgical management difficult. In these challenging instances it is important to understand surgical outcomes to help guide the surgical approach and patient selection, and adequately counsel patients about expected results.
We describe our experience with treating adults with complications of previous hypospadias treatment. We expand on the strategies that we found to be successful in these difficult cases.
MATERIALS AND METHODS
We reviewed our prospectively collected, institutional review board approved urethroplasty database. Approximately 1,127 patients were treated with urethroplasty for urethral stricture disease by a single surgeon (JWM) from 1980 to 2009. Patients were included in the study if they underwent previous surgery for hypospadias and were older than 18 years. Demographic information on age and race, medical history and hypospadias surgical history were collected. Urethroplasty specific information, such as procedure type and number, and urethroplasty outcomes were recorded.
After surgery clinical history and uroflowmetry were done at 3-month intervals during year 1 and yearly there-after. Voiding cystourethrogram was performed at catheter removal, and retrograde urethrogram and voiding cystourethrogram were done during followup at 3 months and 1 year. Additional fluoroscopic images were obtained when subjective obstructive symptoms were present. Also, further fluoroscopic imaging was done when peak urinary flow decreased to less than 15 cc per second8 or a change in voiding pattern was seen on uroflowmetry during another followup visit.
Patient outcomes were reported in 2 ways. Treatment was considered an initial success if patients underwent surgery and did not experience postoperative urethral specific complications for a minimum followup of 6 months. However, our overall success rate also includes men in whom treatment initially failed but was ultimately successful after additional surgery, including additional urethroplasty or direct vision internal urethrotomy. Surgery was defined as a failure when patients required intermittent catheterization or had other evidence of persistent urethral disease, such as recurrent stricture or urethrocutaneous fistula.
Patients were excluded from results analysis if they had less than 6 months of followup after the initial surgery. If the initial surgery failed, and patients underwent additional treatment for complications and were then lost to followup, the subsequent additional treatment was assumed to have failed.
RESULTS
Mean ± SD age of the 50 men with previous hypospadias repair was 38 ± 14.3 years (range 19 to 71). The most common presenting problem was urethral stricture in 72% of cases, followed by urethrocutaneous fistula in 24% and persistent hypospadias in 14%. Of the men 78% underwent surgery in childhood and 66% had been treated with multiple previous surgeries. The original hypospadias site could commonly not be determined reliably and, thus, it was not reported.
The 50 patients underwent a total of 74 urethroplasties. The type of urethroplasty varied (see table). After primary urethroplasty in the 50 men subsequent surgery was performed for planned closure of a stage 1 procedure or for complications. A total of 16 men underwent secondary urethroplasty, which was a planned stage 2 procedure in 8 and treatment for failed primary urethroplasty in 8. Six and 2 men underwent tertiary and quaternary urethroplasty, respectively.
Urethroplasty in 50 men with history of hypospadias repair
| No. Urethroplasties | |||||
|---|---|---|---|---|---|
| Urethroplasty Type | Primary | Secondary | Tertiary | Quaternary | Totals |
| Stage 1 | 15 | 2 | 1 | 1 | 19 |
| Penile skin flap | 12 | – | – | – | 12 |
| Perineal urethrostomy | 5 | 1 | – | – | 6 |
| Excision + primary anastomosis |
5 | 1 | – | – | 6 |
| Stage 2 | 3 | 9 | – | – | 12 |
| Tubularized plate | 3 | – | – | – | 3 |
| 1-Stage buccal mucosa graft onlay |
2 | 2 | – | – | 4 |
| Urethrocutaneous fistula closure |
2 | 1 | 4 | 1 | 8 |
| Chordee correction | 1 | – | – | – | 1 |
| Combined techniques | 2 | – | 1 | – | 3 |
| — | — | – | – | — | |
| Total No. | 50 | 16 | 6 | 2 | 74 |
All 50 men had more than 6 months of followup (median 89, range 6 to 198). The initial success rate was 50% (25 cases). In the 25 men in whom treatment failed the most common complications were urethral stricture in 46% and urethrocutaneous fistula in 42%. Other complications included periurethral infection in 4% of cases, buccal mucosa graft contracture in 4% and ventral urethral erosion in 4%. A total of 18 men (69%) required intervention for complications, including another 15 urethroplasties and 14 endoscopic procedures. Of these 18 men treatment was ultimately successful in 13, including 8 and 5 who underwent additional urethroplasty and a single direct vision internal urethrotomy or dilatation, respectively (see table). Counting these men the overall success rate was 76% (38 of 50). Of the 13 men in whom therapy ultimately failed 4 had a persistent urethrocutaneous fistula, 5 had a urethral stricture that was dependent on dilation or intermittent catheterization and 4 were lost to followup after treatment of complications that was assumed to have failed or had a pending outcome after complication treatment.
Patients were separated into 4 groups to analyze the success rate specific to a given surgical approach, including group 1—stage 1 urethroplasty, group 2—1-stage urethroplasty (penile skin flap, perineal urethrostomy, excision and primary anastomosis, tubularized plate, 1-stage buccal mucosa graft onlay and combined techniques), group 3—stage 2 urethroplasty and group 4—urethrocutaneous fistula closure.
Stage 1 Urethroplasty
Of the men 16 underwent at total of 19 stage 1 urethroplasties for penile urethral stricture. A buccal mucosa graft was placed in 9 cases (47%) to replace the native urethral plate. In the remainder the native urethral plate was opened and approximated to penile skin. Initial success was achieved in 81% of the 16 men and ultimate success was achieved in 88% after secondary procedures. Eventually 8 men (50%) underwent closure at stage 2 urethroplasty, 5 (31%) did not elect stage 2 closure and 3 (19%) await surgery or have a pending outcome from complications of stage 1 urethroplasty.
1-Stage Urethroplasty
This group included 29 men who underwent a total of 35 procedures. Of these men 15 (52%) were initially treated successfully. Of the 14 men (48%) with complications 7 (24%) underwent additional urethroplasty, 4 (14%) underwent dilatation or direct vision internal urethrotomy and 3 (10%) were treated without an additional procedure. The outcome was successful in 5 men (17%) who underwent additional surgery or endoscopic treatment and in 1 (3%) with a small healed fistula. Counting these 6 men the overall success rate, was 72%. For 1-stage procedures the 12 patients who received a penile skin flap fared the worst with complications in 9 (75%) and surgical management that ultimately failed in 5 (42%).
Stage 2 Urethroplasty
Of the 11 men who underwent stage 2 urethroplasty 8 were treated with stage 1 urethroplasty at our institution and 3 who underwent stage 1 urethroplasty elsewhere presented for stage 2 closure. In 6 men (55%) previous first stage urethroplasty was done using buccal mucosa to replace the urethral plate. In men who underwent stage 2 closure the mean interval between stage 1 and stage 2 was 17 months. Only 4 cases (36%) were initially treated successfully. Ultimately another 4 men (36%) healed or had a small fistula that was successfully repaired. Thus, overall success was achieved in 8 men (73%).
Urethrocutaneous Fistula Closure
Nine men underwent urethrocutaneous fistula closure, including 2 with primary presentation of fistula and 7 with a postoperative urethrocutaneous fistula. These fistulas were closed primarily in several layers with a tunica dartos flap if local tissue permitted additional coverage. Although 12 men had a urethrocutaneous fistula at initial presentation, only 2 were included in this group since the remaining 10 had a fistula involving an area of stricture or persistent hypospadias and fistula treatment was incorporated into the global repair of the underlying urethral problem. One man was lost to followup and surgery was successful in 3 (37%) of the remaining 8. Of the 5 men (63%) with complications 2 (25%) were treated successfully with direct vision internal urethrotomy or an additional fistula closure. When including these 2 men, the overall success rate was 63%.
DISCUSSION
Reconstructive urology leaders have remarked on the difficulty of writing a satisfactory journal article on failed hypospadias repair.7,8 Given the heterogeneity and range of abnormalities of patients with failed hypospadias repair and the imperfect treatments provided, reporting outcomes is a challenge.
The complexity of these cases is highlighted by the largest report to date on failed hypospadias by Barbagli et al.8 In the 1,176 treated patients a median of 3 operations was required to repair primary hypospadias while almost 10% of patients required 5 or more operations.
Most groups who report these outcomes do so in conjunction with pediatric patients or adults without prior surgery who undergo initial repair.4,9–11 These reports often lack detail on preoperative problems and commonly describe only a single technique and its outcomes,11–14 not the myriad of surgeries needed in this patient population.
In addition to reporting our overall success rates, we grouped procedures to determine the success rate of any particular approach. Group 1 (stage 1 urethroplasty) had the greatest success rate of any group at 81%. We previously reported a similar stage 1 urethroplasty success rate of 84% in patients with heterogeneous causes of urethral sticture.15 However, the patients in this study with complications did not require surgical revision other than dilatation of stenosis at the urethrostomy site. This finding was dissimilar to our patients with previous hypospadias repair, who required surgical revision secondary to penile or graft related complications. In fact, 22% of the men treated with stage 1 urethroplasty using buccal mucosa experienced graft contracture. Contracture of buccal mucosa grafts was reported by others9,16 with a rate as high as 12% in hypospadias salvage surgery.14 The high rate of graft contracture in our series and others in the literature likely results from inadequate blood supply and scarring along the ventral corporeal bodies associated with previous failed surgeries.
Group 2 (1-stage urethroplasty) included patients treated with various surgeries. These surgeries were grouped together since the intent of the surgeries was a 1-stage operative solution. The success and ultimate success rates in this group were 52% and 72%, respectively. This is far lower than we would expect when comparing success rates in men without a history of hypospadias repair. For instance, buccal mucosa onlay has an 84% to 94% success rate when placed in a dorsal or ventral manner.17–20 Likewise penile skin flaps also have greater than 80% durable success at 10-year followup21 while excision and primary anastomosis of urethral stricture also has greater than 90% durable success.22,23 Poor vascularity due to previous repair was likely the underlying reason for the lower than expected success in this group, particularly in patients with a penile skin flap. These patients fared the worst with a 75% complication rate. We attributed this to the scarred nature of the penile skin and to the unpredictable anatomical blood supply after failed hypospadias repair. With time due to our poor outcomes using penile skin flaps we have evolved to mostly a 2-stage approach with buccal mucosa grafting for penile urethral stricture.
Group 3 (stage 2 urethroplasty) had the lowest initial success rate of 36% and urethrocutaneous fistula was the most common complication. Despite this high complication rate our overall 73% success rate is comparable to that of Barbagli et al, who noted 67% success in patients who underwent stage 2 repair with skin or buccal mucosa.24 Others reported outcomes that were much more favorable for hypospadias salvage using 2-stage repair.11,25 Meeks et al recently reported an 86% success rate.25 The contrast between success rates in our series and those of others must represent patient selection and differences in technique.
In group 4 (urethrocutaneous fistula closure) 50% of the small postoperative fistulas healed spontaneously with additional time for catheter drainage. Many reports do not mention small postoperative fistulas that heal spontaneously and the fistula rate in these studies only includes fistulas that persist and require surgery.7,24 We found that the success rate of urethrocutaneous fistula closure was poor at 37%, similar to our results of stage 2 urethroplasty. This may be explained by poor urethral vascularity in the 2 groups since staged surgical approaches were only used in the worst cases and postoperative fistulas may also arise from an ischemic area after urethroplasty. We used local tunica dartos flaps for tissue interposition to prevent fistula. In children a tunica vaginalis flap has been used to prevent fistula with primary hypospadias repair.26 Adding this flap might improve the fistula rate.
Our study is limited by several factors. This is a case series and procedures were done at a single institution by a single surgeon. For this reason there was a strong bias in our approach to hypospadias salvage that may have strongly influenced our outcomes.
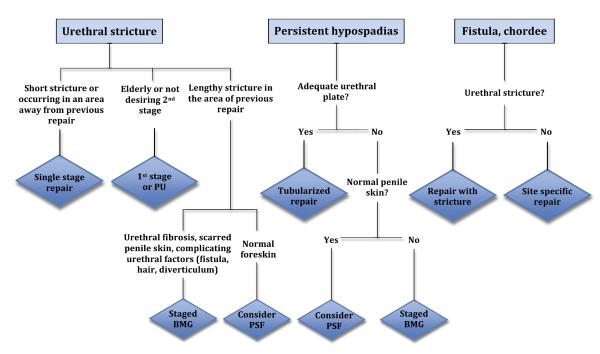
Selection of the surgical approach for any given patient generally depended on the presenting problem as well as the site and extent of urethral stricture disease, if present. The figure shows our treatment algorithm, which summarizes our general strategy for approaching patients with hypospadias failure. It cannot encompass all of the complexities and ancillary surgical maneuvers that may be needed in these heterogeneous cases. Generally in patients with strictures well away from the previous surgical site, such as the mid or proximal bulbar urethra, or short strictures with an otherwise healthy urethra, 1-stage operations can be done, including excision and primary anastomosis or buccal mucosa graft onlay urethroplasty. In patients with longer strictures or persistent hypospadias who have normal supple preputial skin we used a local or dorsolateral penile skin flap. In patients with extensive urethral stricture and penile scarring involving the preputial skin we offered stage 1 urethroplasty with excision of the urethral plate and buccal mucosa graft if necessary, or perineal urethrostomy. Older men and those with multiple failed operations in the past were the usual patients who elected this final option. Those with urethrocutaneous fistula or chordee but without stricture disease underwent site specific repair of the problem.
Algorithm of general strategy for surgical management of common presenting problems in men with previous hypospadias treatment. PU, perineal urethrostomy. BMG, buccal mucosa graft. PSF, penile skin flap.
CONCLUSIONS
In men with complications of previous hypospadias repair urethral stricture is the most common presenting problem, followed by urethrocutaneous fistula and persistent hypospadias. In this group of men urethroplasty complications are common despite modern urethroplasty techniques. Patients must be prepared and committed to the possibility of several surgeries to manage these problems. No single surgical approach is possible and many techniques must be used to achieve a successful outcome.
REFERENCES
- 1.Devine CJ, Horton CE. A one-stage hypospadias repair. J Urol. 1961;85:166. doi: 10.1016/S0022-5347(17)65301-1. [DOI] [PubMed] [Google Scholar]
- 2.Snodgrass WT, Lorenzo A. Tubularized incised-plate urethroplasty for proximal hypospadias. BJU Int. 2002;89:90. [PubMed] [Google Scholar]
- 3.Shukla AR, Patel RP, Caning DA. The 2-stage hypospadias repair. Is it a misnomer? J Urol. 2004;172:1714. doi: 10.1097/01.ju.0000138926.26530.f9. [DOI] [PubMed] [Google Scholar]
- 4.Li Q, Li S, Chen W, et al. Combined buccal mucosa graft and local flap for urethral reconstruction in various forms of hypospadias. J Urol. 2005;174:690. doi: 10.1097/01.ju.0000164759.49877.f4. [DOI] [PubMed] [Google Scholar]
- 5.Manzoni G, Bracka A, Palminteri E, et al. Hypospadias surgery: when, what and by whom? BJU Int. 2004;94:1188. doi: 10.1046/j.1464-410x.2004.05128.x. [DOI] [PubMed] [Google Scholar]
- 6.Lumen N, Hoebeke P, Willemsen P, et al. Etiology of urethral stricture disease in the 21st century. J Urol. 2009;182:983. doi: 10.1016/j.juro.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 7.Mundy AR. Failed hypospadias repair presenting in adults. Eur Urol. 2006;49:774. doi: 10.1016/j.eururo.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 8.Barbagli G, Perovic S, Djinovic R, et al. Retrospective descriptive analysis of 1176 patients with hypospadias repair. J Urol. 2010;183:207. doi: 10.1016/j.juro.2009.08.153. [DOI] [PubMed] [Google Scholar]
- 9.Fichtner J, Filipas D, Fisch M, et al. Long-term follow up of buccal mucosa onlay graft for hypospadias repair: analysis of complications. J Urol. 2004;172:1970. doi: 10.1097/01.ju.0000142451.78966.fb. [DOI] [PubMed] [Google Scholar]
- 10.Hensle TW, Tennenbaum SY, Reiley EA, et al. Hypospadias repair in adults: adventures and misadventures. J Urol. 2001;165:77. doi: 10.1097/00005392-200101000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Bracka A. Hypospadias repair: the two-stage alernative. Br J Urol. 1995;76:31. doi: 10.1111/j.1464-410x.1995.tb07815.x. [DOI] [PubMed] [Google Scholar]
- 12.Li L, Zhang X, Zhou S, et al. Experience with repair of hypospadias using bladder mucosa in adolescents and adults. J Urol. 1995;153:1117. [PubMed] [Google Scholar]
- 13.Sahin C, Sayhan T. Use of buccal mucosal grafts in hypospadias crippled adult patients. Ann Plast Surg. 2003;50:382. doi: 10.1097/01.SAP.0000037274.65665.FF. [DOI] [PubMed] [Google Scholar]
- 14.Snodgrass W, Elmore J. Initial experience with staged buccal graft (Bracka) hypospadias reoperations. J Urol. 2004;172:1720. doi: 10.1097/01.ju.0000139954.92414.7d. [DOI] [PubMed] [Google Scholar]
- 15.Eliot SP, Eisenberg ML, McAninch JW. First-stage urethroplasty: utility in the modern era. Urology. 2008;71:889. doi: 10.1016/j.urology.2007.11.051. [DOI] [PubMed] [Google Scholar]
- 16.Metro MJ, Wu H, Snyder HM, et al. Buccal mucosal grafts: lessons learned from an 8-year experience. J Urol. 2001;166:1459. doi: 10.1016/s0022-5347(05)65809-0. [DOI] [PubMed] [Google Scholar]
- 17.Elliot SP, Metro MJ, McAninch JW. Long-term follow up of the ventrally placed buccal mucosa onlay graft in bulbar urethral reconstruction. J Urol. 2003;169:1754. doi: 10.1097/01.ju.0000057800.61876.9b. [DOI] [PubMed] [Google Scholar]
- 18.Kellner DS, Frachia JA, Armenakas NA. Ventral onlay buccal mucosal grafts for anterior urethral strictures: long-term follow up. J Urol. 2004;171:726. doi: 10.1097/01.ju.0000103500.21743.89. [DOI] [PubMed] [Google Scholar]
- 19.Kane CJ, Tarman GJ, Summerton DJ, et al. Multi-institutional experience with buccal mucosa onlay urethroplasty for bulbar urethral reconstruction. J Urol. 2002;167:1314. [PubMed] [Google Scholar]
- 20.Barbagli G, Palmineri E, Guazzoni G, et al. Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique? J Urol. 2005;174:955. doi: 10.1097/01.ju.0000169422.46721.d7. [DOI] [PubMed] [Google Scholar]
- 21.Whitson JM, McAninch JW, Elliot SP, et al. Long-term efficacy of distal penile circular fasciocutaneous flaps for single stage reconstruction of complex anterior urethral stricture disease. J Urol. 2008;179:2259. doi: 10.1016/j.juro.2008.01.087. [DOI] [PubMed] [Google Scholar]
- 22.Eltahawy EA, Virasoro R, Schlossberg SM, et al. Long-term follow up for excision and primary anastomosis for anterior urethral strictures. J Urol. 2007;177:1803. doi: 10.1016/j.juro.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 23.Barbagli G, De Angelis M, Romano G, et al. Long-term follow up of bulbar end-to-end anastomosis: A retrospective analysis of 153 patients in a single center experience. J Urol. 2007;178:2470. doi: 10.1016/j.juro.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 24.Barbagli G, De Angelis M, Palminteri E, et al. Failed hypospadias repair presenting in adults. Eur Urol. 2006;49:887. doi: 10.1016/j.eururo.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 25.Meeks JJ, Erickson BA, Gonzalez CM. Staged reconstruction of long segment urethral strictures in men with previous pediatric hypospadias repair. J Urol. 2009;181:685. doi: 10.1016/j.juro.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 26.Snow BW, Cartwright PC, Unger K. Tunica vaginalis blanket wrap to prevent urethrocutaneous fistula: an 8-year experience. J Urol. 1995;153:472. doi: 10.1097/00005392-199502000-00061. [DOI] [PubMed] [Google Scholar]