Abstract
Objective
To identify developmental trajectories of anxiety symptoms for adolescent girls and boys. Trajectories were compared with regard to early-adolescent risk factors and psychiatric outcomes during adolescence and in young adulthood.
Method
A community sample of 2,230 adolescents was assessed three times across a six-year interval (10–17 years). Symptom scores of anxiety were analyzed with growth mixture models, stratified by gender.
Results
Three gender-specific anxiety trajectories were identified for both girls (93.3% low, 4.1% mid-adolescence limited, 2.6% mid-adolescence increasing) and boys (84.4% low, 9.5% mid-adolescence limited, 6.1% early-adolescence decreasing). Child, family and peer factors at baseline predicted group membership of the mid-adolescence limited anxiety trajectory and the early-adolescence decreasing anxiety trajectory in boys. Parental emotional problems predicted the early-adolescence anxiety increase trajectory in girls. Prevalence of anxiety disorders and depression during adolescence and in early adulthood was higher in both the mid-adolescence limited and the mid-adolescence anxiety increase trajectory.
Conclusions
The longitudinal course of anxiety symptoms during adolescence was characterized by three distinct gender-specific developmental trajectories. The most at-risk trajectory in girls was the mid-adolescence anxiety increase trajectory, and in boys the mid-adolescence limited trajectory. None of the environmental (i.e., child, family and peer) factors distinguished the at-risk trajectories from the other trajectories.
Keywords: anxiety, adolescence, developmental trajectories, determinants, and growth mixture modelling
Résumé
Objectif
Identifier les trajectoires développementales des symptômes d’anxiété pour les adolescents et les adolescentes. Les trajectoires ont été comparées à l’égard des facteurs de risque du début de l’adolescence et des résultats psychiatriques durant l’adolescence et le jeune âge adulte.
Méthode
Un échantillon communautaire de 2 230 adolescents (de 10 à 17 ans) a été évalué à trois reprises sur un intervalle de six ans. Les scores des symptômes d’anxiété ont été analysés à l’aide de modèles de croissance mixtes, stratifiés par sexe.
Résultats
Trois trajectoires d’anxiété sexospécifiques ont été identifiées pour les filles (93,3 % faibles, 4,1 % limitées à la mi-adolescence, 2,6 % croissantes à la mi-adolescence) et les garçons (84,4 % faibles, 9,5 % limitées à la mi-adolescence, 6,1 % décroissantes au début de l’adolescence). Les facteurs environnementaux des enfants, de la famille et des pairs au départ prédisaient l’appartenance du groupe à la trajectoire d’anxiété limitée de la mi-adolescence ainsi qu’à la trajectoire d’anxiété décroissante du début de l’adolescence chez les garçons. Les problèmes émotionnels parentaux prédisaient la trajectoire d’anxiété croissante du début de l’adolescence chez les filles. La prévalence des troubles anxieux et de la dépression durant l’adolescence et au jeune âge adulte était plus élevée tant dans la trajectoire d’anxiété limitée de mi-adolescence que dans la trajectoire d’anxiété croissante de mi-adolescence.
Conclusions
L’évolution longitudinale des symptômes d’anxiété durant l’adolescence était caractérisée par trois trajectoires développementales sexospécifiques distinctes. Chez les filles, la trajectoire la plus à risque était la trajectoire d’anxiété croissante de mi-adolescence, et chez les garçons, la trajectoire d’anxiété limitée de mi-adolescence. Aucun des facteurs environnementaux (c.-à-d., enfants, famille, pairs) ne distinguait les trajectoires à risque des autres trajectoires.
Keywords: anxiété, adolescence, trajectoires développementales, déterminants, et modèles de croissance mixtes
Introduction
Anxiety disorders are highly prevalent, cause considerable distress (e.g., strong association with suicidal ideation and attempts), and impose a substantial burden on society (Kessler et al., 2005; Boden, Fergusson, & Horwood, 2007). Adolescence is a risk phase for the development of anxiety disorders (Beesdo, Knappe, & Pine, 2009). Almost one in every three adolescents suffers from anxiety disorders and girls even more than boys (Merikangas et al., 2010). Also at a symptom level, adolescent girls experience higher levels of anxiety than boys (Hale, Raaijmakers, Muris, van Hoof, & Meeus, 2008; Hale, Raaijmakers, Muris, van Hoof, & Meeus, 2009; van Oort, Greaves-Lord, Verhulst, Ormel, & Huizink, 2011). Longitudinal studies have shown that although anxiety disorders can be limited to adolescence, they often persist into adulthood (Pine, Cohen, Gurley, Brook, & Ma, 1998). Moreover, anxiety disorders in adolescence increase the risk of other psychiatric disorders later in life, particularly depressive disorders (Bittner et al., 2004; Copeland, Shanahan, Costello, & Angold, 2009). Given the homotypic and heterotypic longitudinal persistence of anxiety disorders, early identification of at-risk adolescents is crucial as targeted prevention programs can then be delivered.
A statistical modelling technique to identify subgroups of individuals that will experience elevated levels of anxiety during adolescence is growth mixture modelling (Jung & Wickrama, 2008). Growth mixture modelling is used to ascertain subgroups of individuals within a population which follow a unique developmental pattern that is distinct from other subgroups. Growth mixture modelling cannot only improve our understanding of heterogeneity in the developmental course of anxiety problems across adolescence, but could also provide clues for early identification of adolescents prone to develop anxiety and depression by pinpointing early determinants of specific developmental anxiety trajectories and by clarifying the association between these anxiety trajectories and later psychopathology.
Growth mixture modelling has been used in several child studies on anxiety (e.g., Feng, Shaw, & Silk, 2008; Duchesne, Larose, Vitaro, & Tremblay, 2010; Côté et al., 2009). Duchesne et al. (2010), for instance, examined trajectories of anxiety symptoms in 2,000 children who were followed from kindergarten to the end of elementary school. They found a low (34%), low-increasing (20%), high-declining (32%), and high (14%) developmental trajectory of anxiety. Children in the high anxiety trajectory were more often inattentive and exposed to disciplinary practices at home, and less prosocial. Fairly similar anxiety trajectories (i.e., low, low-increasing, high-declining, and high-increasing) were found among boys between the ages of two and ten years in the study of Feng et al. (2008). Côté examined combined anxiety and depression symptoms trajectories, and also identified increasing trajectories and a low trajectory.
Two studies examined distinct developmental trajectories of anxiety symptoms across adolescence with a growth mixture modelling approach (Crocetti, Klimstra, Keijsers, Hale, & Meeus, 2009; Morin et al., 2011). In a five-wave longitudinal study starting between the ages of 10 and 20 years, Crocetti et al. (2009) found that 91% of the adolescents followed a trajectory characterized by initial low levels of anxiety that decreased over time, and 9% by higher initial levels that further increased over time. Girls were more likely to follow the high-increasing trajectory than boys. In the study of Morin and colleagues (2011) anxiety status in adolescents was evaluated six times, starting around the age of 12 years, during a four-year period. They identified five distinct anxiety trajectories, of which three trajectories were characterized by a stable pattern of no, a low level, or a high level of anxiety symptoms. The other two trajectories followed a curvilinear pattern, with one showing high levels at both entrance and leaving of secondary school and lower levels in between, and the other a peak during secondary school years. Despite the overrepresentation of girls in high or increasing anxiety trajectories, both studies did not statistically model developmental trajectories for girls and boys separately. As the typical longitudinal course of anxiety across adolescence differs between girls and boys (Hale et al., 2008, 2009; van Oort, Greaves-Lord, Verhulst, Ormel, & Huizink, 2009), we hypothesized gender-specificity in the trajectories.
The aim of this study was to examine: (1) gender-specific developmental trajectories of anxiety symptoms during adolescence; (2) which factors determine group membership of anxiety trajectories; and, (3) associations between anxiety trajectories and anxiety and depressive disorders during adolescence and in early adulthood. With respect to determinants of developmental trajectories, we examined a number of child (self-competence, temperament), family (parenting style, parental internalizing psychopathology, and life events) and peer factors (peer victimization), which were identified as risk indicators of high levels of anxiety during adolescence in a previous study in the same sample (van Oort et al., 2011).
Methods (summary)
This study is part of the TRacking Adolescents’ Individual Lives Survey (TRAILS), a prospective cohort of 2,230 Dutch adolescents initially aged 10–12 years, who are followed bi- or triennially, until the age of 25 (Huisman et al., 2008). So far, four data collection waves have been completed: T1 (N=2,230; response rate 76.0%; mean age (SD)=11.1 (0.6) years), T2 (N=2,149; response rate 96.4% of baseline participants; mean age (SD)=13.6 (0.5) years), T3 (N=1,816; response rate 81.4% of baseline participants; mean age (SD)=16.3 (0.7) years), and T4 (N=1,584 completed CIDI; response rate 71% of baseline participants; mean age (SD)=19.2 (0.6) years).
Anxiety symptoms were measured with a well-validated and reliable self-report measure (Revised Child Anxiety and Depression Scale; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) at the first three waves (10–17 years). The models were fit based on the RCADS scores at specific ages, rather than at each assessment.
At T1 (10–12 years), the following child, family and peer factors were measured with different questionnaires (see Supplementary Materials Section): self-competence, temperament (shyness, frustration, and effortful control), perceived parenting (overprotecting and rejecting parenting), life events up to T1 (illness and death in the family), parental current and lifetime internalizing problems, and peer victimization (victim, bully and bully-victim). At T4 (18–20 years), DSM-IV anxiety disorders and major depressive disorder were assessed retrospectively (10–17 years) and over the past year with the Composite International Diagnostic Interview 3.0 (Kessler & Ustun, 2004).
More extensive details of the study design, measures and statistical methods are given in the online Supplementary Materials section.
Results
Developmental trajectories of anxiety
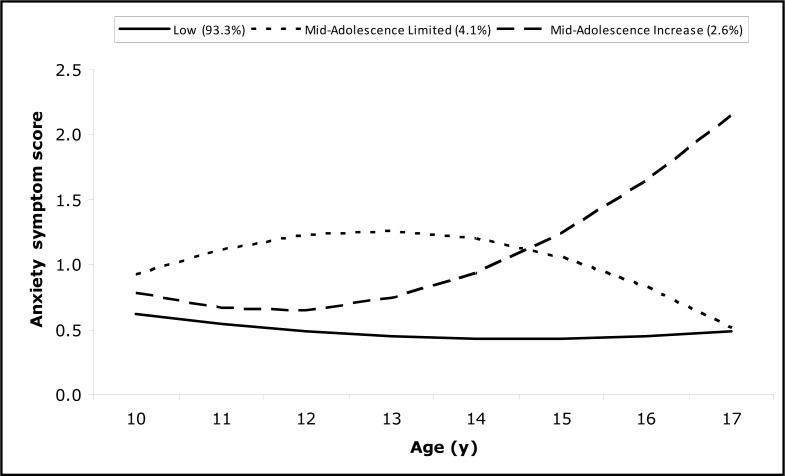
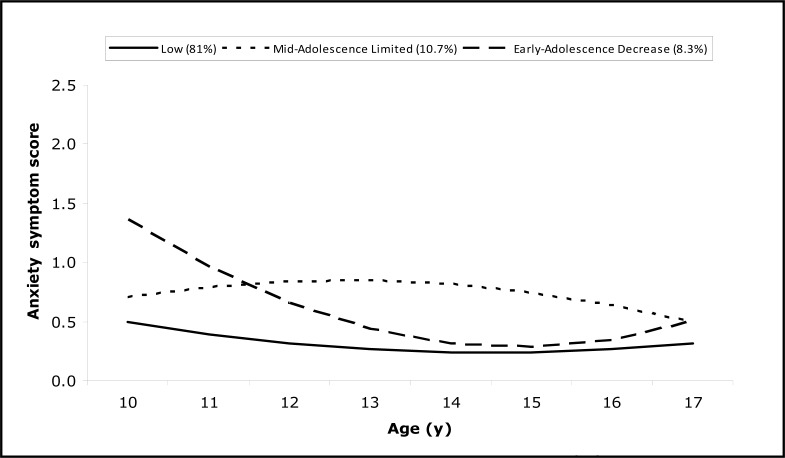
Growth mixture modelling (GMM) was used to identify distinct developmental trajectories of anxiety symptoms. Three distinct curvilinear anxiety trajectories were identified for both girls and boys (Figure 1 and 2). Model fit and parameter estimates of these trajectories are given in supplementary Tables A2 and A3.
Figure 1.
Developmental trajectories of anxiety for girls
Figure 2.
Developmental trajectories of anxiety for boys
Note: The Y-axis shows mean item scores on the anxiety questionnaire (0–3) and the X-axis shows age in years (10–17).
The first trajectory in girls was one of low anxiety symptoms (low trajectory; n=1,055; 93.3%). The second trajectory had an inverted u-shape (mid-adolescence limited (MAL) trajectory; n=46; 4.1%), reflecting an increase of anxiety symptoms between the ages of 10 and 13, followed by a decrease of anxiety between the ages of 13 and 17. The anxiety level of the MAL-trajectory decreased to the anxiety level of the low trajectory by the age of 17 years. The third trajectory was characterized by an initial small decrease of anxiety symptoms in early-adolescence followed by progressively increasing anxiety symptoms starting in mid-adolescence (mid-adolescence increase (MAI) trajectory; n=29; 2.6%).
For boys, a low trajectory (n=924; 84.4%) and MAL-trajectory (n=104; 9.5%) were identified, fairly similar to those in girls. The third trajectory was characterized by a progressive decrease of anxiety symptoms during early adolescence followed by a small increase of anxiety symptoms between 15 and 17 years (early-adolescence decrease (EAD) trajectory; n=67; 6.1%). With the current time window it is unclear whether the increase in anxiety symptoms in EAD-trajectory will continue into young adulthood.
Early determinants of developmental trajectories of anxiety
Tables 1 and 2 show the results of the multinomial logistic regression analyses regarding child, family and peer factors between 10 and 12 years as predictors of developmental anxiety trajectories for girls and boys.
Table 1.
Early determinants of anxiety trajectories for girls
| Early determinants a | Anxiety trajectories
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Low N = 1051
|
MAL N = 46
|
MAI N = 28
|
MALb
|
MAI b
|
MAI c
|
||||
| % | % | % | OR | (95%CI) | OR | (95%CI) | OR | (95%CI) | |
| Low self-competence | 21.1 | 52.2 | 21.4 | 4.07 | (2.24–7.41)*** | 1.02 | (0.41–2.54) | 0.25 | (0.09–0.73)** |
| Shyness | 24.4 | 17.3 | 23.9 | 0.65 | (0.28–1.48) | 0.96 | (0.35–2.65) | 1.49 | (0.44–2.06) |
| Frustration | 17.5 | 26.6 | 19.1 | 1.71 | (0.81–3.58) | 1.10 | (0.38–3.17) | 0.59 | (0.28–1.23) |
| Effortful control | 20.8 | 26.5 | 25.9 | 1.37 | (0.68–2.76) | 1.32 | (0.53–3.31) | 0.96 | (0.32–2.91) |
| Parenting – rejection | 15.1 | 45.7 | 14.3 | 4.73 | (2.58–8.67)*** | 0.94 | (0.32–2.75) | 0.20 | (0.06–0.66)** |
| Parenting – overprotection | 18.5 | 50.0 | 21.4 | 4.40 | (2.42–8.01)*** | 1.20 | (0.48–3.00) | 0.27 | (0.09–0.80)* |
| Parental internalizing problems | |||||||||
| Lifetime | 16.9 | 22.9 | 32.1 | 1.46 | (0.72–2.99) | 2.33 | (0.99–5.44)* | 1.59 | (0.53–4.72) |
| Current | 20.9 | 27.4 | 28.6 | 1.42 | (0.71–2.87) | 1.50 | (0.58–3.86) | 1.05 | (0.34–3.28) |
| Illness in the family | 37.1 | 50.1 | 58.2 | 1.70 | (0.94–3.09) | 2.37 | (1.08–5.19)* | 1.39 | (0.53–3.66) |
| Death in the family | 2.8 | 15.2 | 3.9 | 6.20 | (2.55–15.04)*** | 1.38 | (0.18–10.57) | 0.22 | (0.03–1.92) |
| Peer victimization | |||||||||
| Victim | 21.9 | 23.9 | 21.4 | 0.88 | (0.52–1.49) | 1.15 | (0.52–2.54) | 1.31 | (0.51–3.35) |
| Bully-victim | 7.9 | 23.9 | 7.9 | 2.42 | (1.41–4.18)*** | 1.06 | (0.34–3.29) | 0.44 | (0.13–1.50) |
| Bully | 13.6 | 15.2 | 7.1 | 0.90 | (0.46–1.68) | 0.62 | (0.20–1.91) | 0.69 | (0.19–2.46) |
Continuous variables were dichotomized at p80.
Low anxiety trajectory was the comparison class.
MAL trajectory was the comparison class.
p<0.05;
p<0.01;
p<0.001.
MAI = mid-adolescence-increase; MAL = mid-adolescence-limited
Table 2.
Early determinants of anxiety trajectories for boys
| Early determinants a | Anxiety trajectories
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Low N = 919
|
MAL N = 102
|
EAD N = 65
|
MAL b
|
EAD b
|
EAD c
|
||||
| % | % | % | OR | (95%CI) | OR | (95%CI) | OR | (95%CI) | |
| Low self-competence | 13.0 | 28.7 | 61.5 | 2.71 | (1.68–4.35)*** | 10.74 | (6.28–18.38)*** | 3.97 | (2.05–7.69)*** |
| Shyness | 19.1 | 24.8 | 17.5 | 1.39 | (0.84–2.28) | 0.89 | (0.44–1.78) | 0.64 | (0.28–.45) |
| Frustration | 23.4 | 26.7 | 33.8 | 1.19 | (0.74–1.93) | 1.67 | (0.95–2.92) | 1.40 | (0.70–2.81) |
| Effortful control | 15.6 | 15.9 | 6.5 | 1.02 | (0.57–1.83) | 0.37 | (0.12–1.15) | 0.36 | (0.10–1.26) |
| Parenting – rejection | 20.6 | 35.3 | 47.7 | 2.11 | (1.36–3.26)*** | 3.52 | (2.11–5.88)*** | 1.67 | (0.89–3.15) |
| Parenting – overprotection | 18.7 | 34.3 | 52.3 | 2.27 | (1.46–3.53)*** | 4.76 | (2.85–7.98)*** | 2.10 | (1.11–3.96)* |
| Parental internalizing problems | |||||||||
| Lifetime | 16.8 | 14.6 | 23.8 | 0.85 | (0.47–1.52) | 1.55 | (0.84–2.84) | 1.82 | (0.82–4.07) |
| Current | 21.4 | 20.2 | 30.1 | 0.93 | (0.55–1.57) | 1.58 | (0.89–2.81) | 1.70 | (0.81–3.58) |
| Illness in the family | 37.3 | 33.6 | 54.7 | 0.85 | (0.55–1.32) | 2.03 | (1.22–3.38)** | 2.39 | (1.25–4.55)** |
| Death in the family | 3.8 | 3.0 | 3.2 | 0.78 | (0.24–2.61) | 0.83 | (0.19–3.53) | 1.05 | (0.17–6.51) |
| Peer victimization | |||||||||
| Victim | 17.3 | 24.7 | 21.1 | 2.57 | (1.79–3.69) | 3.32 | (2.20–5.01) | 0.94 | (0.53–1.65) |
| Bully-victim | 11.4 | 31.3 | 41.0 | 1.33 | (0.91–1.93)*** | 1.24 | (0.78–1.98)*** | 1.29 | (0.79–2.13) |
| Bully | 21.1 | 10.8 | 13.9 | 0.48 | (0.29–0.78)*** | 0.61 | (0.35–1.05) | 1.27 | (0.63–2.59) |
Continuous variables were dichotomized at p80.
Low anxiety trajectory was the comparison class.
MAL trajectory was the comparison class.
p<0.05;
p<0.01;
p<0.001.
MAL = mid-adolescence-limited; MAI = mid-adolescence-increase; EAD = early-adolescence decrease
For girls, group membership of the MAL-trajectory was predicted by low self-competence, rejecting and overprotective parenting, death in the family, and being a bully/victim. Group membership of the MAI-trajectory was predicted by lifetime parental internalizing problems and illness in the family. Compared with girls in the MAI-trajectory, girls in the MAL-trajectory had more rejecting (OR=5.0; p<.001) and overprotective (OR=3.7; p<.05) parents, and lower self- competence (OR=4.0; p<.01) in early adolescence.
For boys, group membership of the MAL-trajectory and of the EAD-trajectory was predicted by low self-competence, rejecting and overprotective parenting, and peer victimization; membership of the EAD-trajectory was also predicted by illness in the family. Whereas predictors overlapped for the trajectories in boys, the two groups differed from each other: compared with boys in the MAL-trajectory, boys in the EAD-trajectory were more likely to have an overprotective parent (OR=2.1; p<.05), to have low self-competence (OR=4.0; p<.001), and to have more illnesses in the family (OR=2.4; p<.01) in early adolescence.
Developmental trajectories of anxiety and anxiety and major depressive disorders (MDD)
Tables 3 and 4 show the results of the binary logistic regression analyses regarding the association between anxiety trajectories and anxiety disorders and MDD during adolescence and in early adulthood for girls and boys.
Table 3.
Association between anxiety trajectories and psychiatric disorders for girls
| Psychiatric disorders | Anxiety trajectories
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low N = 797
|
MAL N = 31
|
MAI N = 24
|
MAL a
|
MAI a
|
MAI b
|
|||||||
| n | (%) | n | (%) | n | (%) | OR | (95%CI) | OR | (95%CI) | OR | (95%CI) | |
| Adolescence | ||||||||||||
| Any anxiety disorder | 119 | (14.9) | 6 | (19.4) | 11 | (45.8) | 1.37 | (0.55–3.40) | 4.82 | (2.11–11.01)*** | 3.53 | (1.06–11.70) |
| Major depressive disorder | 132 | (16.6) | 10 | (32.3) | 12 | (50.0) | 2.40 | (1.10–5.21)* | 5.04 | (2.22–11.46)*** | 2.10 | (0.70–6.30) |
| Early adulthood | ||||||||||||
| Panic disorders / agoraphobia | 18 | (2.3) | 1 | (3.2) | 3 | (12.5) | - | - | - | |||
| Generalized anxiety disorder | 19 | (2.4) | 3 | (9.7) | 7 | (29.2) | - | - | - | |||
| Specific phobia | 105 | (13.2) | 5 | (16.1) | 3 | (12.5) | - | - | - | |||
| Social phobia | 68 | (8.5) | 4 | (12.9) | 8 | (33.3) | - | - | - | |||
| Any anxiety disorder | 176 | (22.1) | 10 | (32.3) | 13 | (54.2) | 1.68 | (0.78–3.63) | 4.17 | (1.84–9.47)*** | 2.48 | (0.83–7.46) |
| Major depressive disorder | 88 | (11.0) | 7 | (22.6) | 13 | (54.2) | 2.35 | (0.98–5.61) | 9.55 | (4.14–21.90)*** | 4.05 | (1.27–12.97) |
Low anxiety trajectory was the comparison class.
MAL trajectory was the comparison class.
p<0.05;
p<0.01;
p<0.001.
MAI = mid-adolescence-increase; MAL = mid-adolescence-limited
Table 4.
Association between anxiety trajectories and psychiatric outcomes for boys
| Psychiatric disorders | Anxiety trajectories
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low N = 602
|
MAL N = 79
|
EAD N = 43
|
MAL a
|
EAD a
|
EAD b
|
|||||||
| n | (%) | n | (%) | n | (%) | OR | (95%CI) | OR | (95%CI) | OR | (95%CI) | |
| Adolescence | ||||||||||||
| Any anxiety disorder | 39 | (6.5) | 12 | (15.2) | 4 | 9.3) | 2.59 | (1.29–5.18)*** | 1.48 | (0.50–4.36) | 0.57 | (0.17–1.90) |
| Major depressive disorder | 41 | (6.8) | 10 | (12.7) | 4 | 9.3) | 1.98 | (0.95–4.14) | 1.40 | (0.48–4.12) | 0.71 | (0.21–2.41) |
| Early adulthood | ||||||||||||
| Panic disorders / agoraphobia | 5 | (0.8) | 4 | (5.1) | 0 | (0.0) | - | - | - | |||
| Generalized anxiety disorder | 2 | (0.3) | 5 | (6.3) | 0 | (0.0) | - | - | - | |||
| Specific phobia | 17 | (2.8) | 5 | (6.3) | 6 | (14.0) | - | - | - | |||
| Social phobia | 21 | (3.5) | 14 | (17.7) | 3 | (7.0) | - | - | - | |||
| Any anxiety disorder | 41 | (6.8) | 20 | (25.3) | 7 | (16.3) | 4.64 | (2.55–8.44)*** | 2.66 | (1.12–6.35)* | 0.57 | (0.22–1.49) |
| Major depressive disorder | 31 | (5.1) | 9 | (11.4) | 5 | (11.6) | 2.37 | (1.08–5.18)* | 2.42 | (0.89–6.59 | 1.02 | (0.32–3.27) |
Low anxiety trajectory was the comparison class.
MAL trajectory was the comparison class.
p<0.05;
p<0.01;
p<0.001.
MAI = mid-adolescence-increase; MAL = mid-adolescence-limited; EAD = ; EAD = early-adolescence decrease
For girls, during adolescence the rate of anxiety disorders was elevated in the MAI-trajectory compared with the low and MAL-trajectory. The rate of MDD was elevated in both the MAL- and MAI-trajectories compared with the low trajectory during adolescence. The MAI-trajectory was strongly predictive of subsequent anxiety disorders and MDD in early adulthood. The MAL-trajectory did not predict a higher rate of anxiety disorders and MDD in early adulthood. Girls in the MAI-trajectory had significantly more MDD than girls in the MAL-trajectory in early adulthood.
For boys, during adolescence, the MAL-trajectory was associated with a higher rate of anxiety disorders, but the EAD-trajectory was not. No differences in the rate of MDD in adolescence were found between the three trajectories. Both the MAL- and EAD-trajectories predicted a higher rate of anxiety disorders in early adulthood. Only the MAL-trajectory predicted a higher rate of MDD in early adulthood. No significant differences were found in the rate of anxiety disorders and MDD between the MAL- and EAD-trajectories, neither during adolescence nor in early adulthood.
Discussion
The present study showed that growth mixture modelling is a valuable approach to detect heterogeneity in the developmental course of anxiety symptoms in adolescence, to identify at-risk subgroups of adolescents, and to provide clues for early prevention and intervention. The course of anxiety symptoms during adolescence was best described by three gender-specific trajectories.
In line with previous studies (Crocetti et al., 2009; Morin et al., 2011) we found that the vast majority of both girls and boys experience constant low anxiety levels throughout adolescence. A subgroup of girls and boys showed transient elevated anxiety levels. Morin et al. (2011) reported a similar MAL-trajectory. The initial increase in anxiety may be due to a stressful transition from primary to secondary school (Morin et al., 2011). The main concerns of adolescents are bullying, fear of getting lost, increased homework, and peer relationships in regard to the secondary school transfer (e.g., Zeedyk et al., 2003; Rice, Frederickson, & Seymour, 2011). These concerns in combination with a low self-competence, parental rejection and overprotection as well as being bullied could make the school transition overwhelming and anxiety-provoking (West, Sweeting, & Young, 2010).
The third trajectory was gender-specific. A subgroup of girls experienced a progressive increase in anxiety that sets off in mid-adolescence. In contrast, a subgroup of boys experienced a progressive decrease of anxiety symptoms during early adolescence followed by a small increase of anxiety symptoms between 15 and 17 years. The significant higher rate of anxiety disorders in boys in early adulthood might suggest that the later increase in anxiety level in the EAD-trajectory continues after the age of 17 years, yet only the prevalence of specific phobia in young adulthood was elevated in this group. The MAI- and EAD-trajectories were also found by Morin (i.e., based on Mplus defaults; 2011), and find support in previous findings that anxiety symptoms generally stabilize or decrease in boys, whereas girls generally show an increase throughout adolescence (Hale et al., 2008; Beesdo et al., 2009).
In girls, the MAI-trajectory was the most at-risk anxiety trajectory for the development of psychiatric disorders during adolescence and in early adulthood. In the MAI-trajectory almost 40% of the girls suffered from an anxiety disorder and 25% from a major depressive disorder in early adulthood, and in adolescence these rates were even higher. Girls in this at-risk trajectory had more parents with lifetime anxiety and depression as well as illnesses in the family as compared to girls in the low anxiety trajectory, but not as compared to girls in the MAL-trajectory. Thus we were not able to identify environmental (i.e., child, family and peer) factors that are specifically predictive of anxiety increase in mid-adolescent girls. This MAI-trajectory in girls might reflect the expression of underlying biological, including genetic, vulnerabilities (Zavos, Gregory, & Eley, 2012). Future research is needed to elucidate underlying mechanisms of anxiety increase in mid-adolescence. For prevention purposes, these findings stress the importance of either to provide a targeted prevention program in early-adolescence or to attentively following children during adolescence and to intervene when these children experience increased feelings of anxiety in mid-adolescence (Barrett, Farrell, Ollendick, & Dadds, 2006; Legerstee et al., 2008).
In boys, both the EAD- and the MAL-trajectories predicted subsequent anxiety disorders. These trajectories were predicted by low-self-competence and rejection by parents and peers. Perhaps these are the children that cope less well with the turmoil of adolescence, as the predictors include vulnerability factors that are quite general for adjustment problems in adolescence (Merikangas, 2005; Grills-Taquechel, Norton, & Ollendick, 2010). One may argue that the MAL-trajectory represents natural developmental variation and that moderately elevated anxiety levels are temporarily and surmountable. Challenges here are to decide whether or not such a group of adolescents should be targeted with interventions. Further, it remains to be studied why girls in the MAL-trajectory were at much lower risk for anxiety disorders.
Conclusion
The present study aimed to increase our understanding of the nature of anxiety development throughout adolescence, its determinants, and subsequent outcomes. Moreover, the results can be informative for further development of interventions and policy for prevention by providing background information on subpopulations to target (risk indicators), at which age (corresponding with changes in anxiety) and how urgently (associations with psychopathology).
Clinicians should be attentive for girls who experience increased feelings of anxiety in mid-adolescence. It is important to intervene early and offer these girls an evidence-based treatment program as they are at-risk for developing anxiety and major depressive disorders. It is also important for clinicians to keep in mind that the some adolescent girls and boys experience the transition from primary to secondary school as stressful, and that elevated anxiety levels during this transition are often transient, but associated with later disorders in boys. It is debatable whether intervention is needed to promote a successful transition to secondary school or whether it is better to monitor anxiety levels before offering an intervention.
SUPPLEMENTARY ONLINE MATERIALS
http://www.cacap-acpea.org/uploads/documents//Gender_Specific_Developmental_Legerstee_2013_02.pdf
Online materials include: Methods; Table A1 (Attrition analyses); Table A2 (Model fit statistics of anxiety trajectories stratified by gender); Table A3 (Parameter estimates of developmental trajectories of anxiety symptoms stratified by gender).
Acknowledgements / Conflicts of Interest
This research is part of the Tracking Adolescents’ Individual Lives Survey (TRAILS). Participating centres of TRAILS include various departments of the University Medical Center and University of Groningen, the Erasmus University Medical Center Rotterdam, the University of Utrecht, the Radboud Medical Center Nijmegen, and the Parnassia Bavo group, all in the Netherlands. TRAILS has been financially supported by various grants from the Netherlands Organization for Scientific Research (NWO), ZonMW, GB-MaGW, the Dutch Ministry of Justice, the European Science Foundation, BBMRI-NL, and the participating universities. We are grateful to all adolescents, their parents, and teachers who participated in this research, and to everyone who worked on this project and made it possible.
References
- Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: An evaluation of the friends program. Journal of Clinical Child and Adolescent Psychology. 2006;35(3):403–411. doi: 10.1207/s15374424jccp3503_5. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bittner A, Goodwin RD, Wittchen HU, Beesdo K, Hofler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? Journal of Clinical Psychiatry. 2004;65(5):618–626. 730. doi: 10.4088/jcp.v65n0505. quiz. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: Findings from a longitudinal study. Psychological Medicine. 2007;37(3):431–440. doi: 10.1017/S0033291706009147. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy. 2000;38(8):835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté SM, Boivin M, Liu X, Nagin DS, Zoccolillo M, Tremblay RE. Depression and anxiety symptoms: Onset, developmental course and risk factors during early childhood. Journal of Child Psychology and Psychiatry. 2009;50(10):1201–1208. doi: 10.1111/j.1469-7610.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- Crocetti E, Klimstra T, Keijsers L, Hale WW, 3rd, Meeus W. Anxiety trajectories and identity development in adolescence: A five-wave longitudinal study. Journal of Youth and Adolescence. 2009;38(6):839–849. doi: 10.1007/s10964-008-9302-y. [DOI] [PubMed] [Google Scholar]
- Duchesne S, Larose S, Vitaro F, Tremblay RE. Trajectories of anxiety in a population sample of children: Clarifying the role of children’s behavioral characteristics and maternal parenting. Development and Psychopathology. 2010;22(2):361–373. doi: 10.1017/S0954579410000118. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. Journal of Abnormal Psychology. 2008;117(1):32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grills-Taquechel AE, Norton P, Ollendick TH. A longitudinal examination of factors predicting anxiety during the transition to middle school. Anxiety Stress Coping. 2010;23(5):493–513. doi: 10.1080/10615800903494127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale WW, 3rd, Raaijmakers Q, Muris P, van Hoof A, Meeus W. Developmental trajectories of adolescent anxiety disorder symptoms: A 5-year prospective community study. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(5):556–564. doi: 10.1097/CHI.0b013e3181676583. [DOI] [PubMed] [Google Scholar]
- Hale WW, 3rd, Raaijmakers QA, Muris P, van Hoof A, Meeus WH. One factor or two parallel processes? Comorbidity and development of adolescent anxiety and depressive disorder symptoms. Journal of Child Psychology and Psychiatry. 2009;50(10):1218–1226. doi: 10.1111/j.1469-7610.2009.02115.x. [DOI] [PubMed] [Google Scholar]
- Huisman M, Oldehinkel AJ, de Winter A, Minderaa RB, de Bildt A, Huizink AC, Ormel J. Cohort profile: The Dutch ‘TRacking Adolescents’ Individual Lives’ Survey’; TRAILS. International Journal of Epidemiology. 2008;37(6):1227–1235. doi: 10.1093/ije/dym273. [DOI] [PubMed] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite Internation Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Legerstee JS, Huizink AC, Van Gastel W, Liber JM, Treffers PD, Verhulst FC, Utens EM. Maternal anxiety predicts favourable treatment outcomes in anxiety-disordered adolescents. Acta Psychiatrica Scandinavica. 2008;117(4):289–298. doi: 10.1111/j.1600-0447.2008.01161.x. [DOI] [PubMed] [Google Scholar]
- Merikangas KR. Vulnerability factors for anxiety disorders in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2005;14(4):649–679. vii. doi: 10.1016/j.chc.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication - Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin AJS, Maiano C, Nagengast B, Marsh HW, Morizot J, Janosz M. General Growth Mixture Analysis of adolescents’ developmental trajectories of anxiety: The impact of untested invariance assumptions on substantive interpretations. Structural Equation Modeling: A Multidisciplinary Journal. 2011;18(4):613–648. [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55(1):56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Rice F, Frederickson N, Seymour J. Assessing pupil concerns about transition to secondary school. British Journal of Educational Psychology. 2011;81(Pt 2):244–263. doi: 10.1348/000709910X519333. [DOI] [PubMed] [Google Scholar]
- van Oort FV, Greaves-Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: The TRAILS study. Journal of Child Psychology and Psychiatry. 2009;50(10):1209–1217. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- van Oort FV, Greaves-Lord K, Ormel J, Verhulst FC, Huizink AC. Risk indicators of anxiety throughout adolescence: The TRAILS study. Depression and Anxiety. 2011;28(6):485–494. doi: 10.1002/da.20818. [DOI] [PubMed] [Google Scholar]
- West P, Sweeting H, Young R. Transition matters: Pupils’experiences of the primary-secondary school transition in the west of Scotland and consequences for well-being and attainment. Research Papers in Education. 2010;25(1):21–50. [Google Scholar]
- Zavos HM, Gregory AM, Eley TC. Longitudinal genetic analyses of anxiety sensitivity. Developmental Psychology. 2012;48(1):204–212. doi: 10.1037/a0024996. [DOI] [PubMed] [Google Scholar]
- Zeedyk SM, Gallacher J, Henderson M, Hope G, Husband B, Lindsay K. Negotiating the transition from primary to secondary school: Perceptions of pupils, parents and teachers. School Psychology International. 2003;24(1):67–79. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
http://www.cacap-acpea.org/uploads/documents//Gender_Specific_Developmental_Legerstee_2013_02.pdf
Online materials include: Methods; Table A1 (Attrition analyses); Table A2 (Model fit statistics of anxiety trajectories stratified by gender); Table A3 (Parameter estimates of developmental trajectories of anxiety symptoms stratified by gender).