Abstract
Introduction
Early infant diagnosis (EID) of HIV infection is an important service to reduce paediatric morbidity and mortality related to HIV/AIDS. Although South Africa has a national EID programme based on PCR testing, there are no population-wide data on the linkage of infants testing HIV PCR-positive to HIV care and treatment services.
Methods
We conducted a retrospective analysis of all public sector laboratory data from across the Western Cape province between 2005 and 2011. We linked positive HIV PCR results to subsequent HIV viral load testing to determine the proportion of infants who were successfully linked to HIV care.
Results
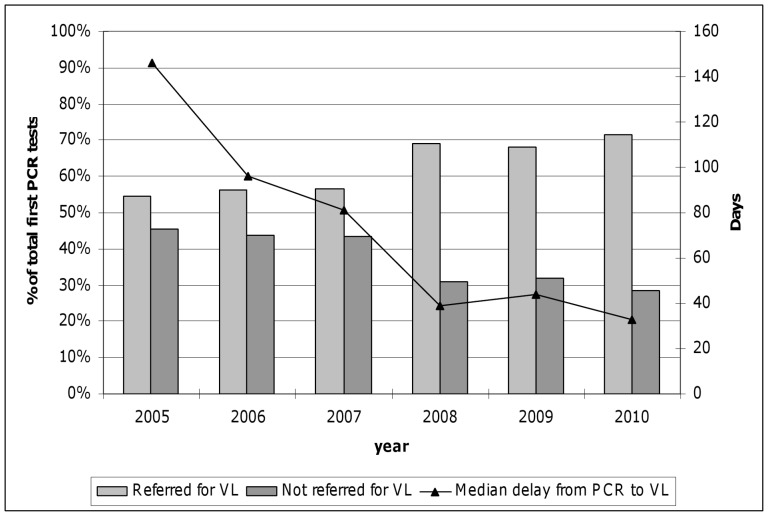
A total of 83 698 unique infant HIV PCR tests were documented, of which 6322 (8%) were PCR positive. The proportion of PCR-positive children declined from 12% in 2005 to 3% in 2011. Of the children testing PCR-positive, 4105 (65%) had subsequent viral load testing indicating successful linkage to care. The proportion of successfully linked infants increased from 54% in 2005 to 71% in 2010, while the median delay in days to successful linkage decreased from 146 days in 2005 to 33 days in 2010.
Discussion
From 2005 to 2011 there has been a reduction in the proportion of children testing HIV PCR-positive, and an increase in the proportion of infected infants successfully linked to HIV care and treatment, in this setting. However a large proportion of infected infants remain unlinked to antiretroviral therapy services and there is a clear need for interventions to further strengthen EID programmes.
Introduction
Across sub-Saharan Africa, mother-to-child-transmission (MTCT) of HIV infection remains an ongoing threat to child health. Despite the widespread implementation of PMTCT programmes, an estimated 390,000 infants were newly infected with HIV during 2010 alone [1]. Infant HIV infection often results in rapid HIV disease progression as approximately 50% of vertically-infected infants die in the first year of life [2]. In South Africa, where there were an estimated 40 000 new infant HIV infections during 2010, HIV contributes significantly towards preventable infant mortality [3], [4].
Early identification of perinatally-infected infants and rapid referral for initiation of antiretroviral therapy (ART) is an important intervention to promote child health [5], [6]. Early infant diagnosis (EID) of HIV by polymerase chain reaction (PCR) is routinely used to detect HIV infection in infants. Although EID is an important component of effective PMTCT programmes, HIV PCR testing is relatively expensive, requires specialised laboratory equipment, and is time consuming. This means the testing components of EID is firmly in the domain of centralised specialist laboratories. This in turn makes health systems issues and logistical considerations, such as conducting HIV testing in primary care facilities, transporting specimens to central reference laboratories, and return of results to primary care, a major concern [7], [8].
Across Africa, non-retention of patients and delays in testing and referral are major operational concerns facing EID programmes [9]. Loss to follow-up of infants between HIV testing, the return of results, and referral of infected infants to paediatric ART services has been documented in several settings [10]–[13]. Even when infants are retained throughout these steps, the delays involved in testing and referring infants for ART may be unacceptable given the high mortality observed in infected infants who are not yet on ART [12]–[15]. But while EID services across Africa face important challenges, systems for monitoring EID programmes are not well developed; as a result, there are few population-level data on the performance of EID services in identifying HIV-infected infants and referring them to ART services [16].
In South Africa, there are few data on the performance of EID services in referring infected infants to long-term care. We used routinely collected HIV laboratory data to investigate the overall levels of MTCT in the Western Cape Province, and the performance of the EID service in referring infected infants for ART, between 2005 and 2011.
Materials and Methods
PMTCT and EID services operate at public sector primary care clinics and hospitals throughout the Western Cape province. HIV PCR testing is used for HIV screening in HIV-exposed infants attending routine postnatal immunization clinics as well as for HIV diagnosis in children who present to hospitals. Prior to 2008, newly diagnosed infants were referred to specialist paediatric infectious disease clinics operated in secondary and tertiary hospitals for ART initiation and follow-up; the provision of ART was based on the 2004 WHO recommendations [17]. Following the results of the Children with HIV Early Antiretroviral Therapy (CHER) study released in 2008, ART initiation for all infected infants became policy across the province, with ART delivered through hospitals as well as a growing number of primary care clinics. Throughout, HIV viral load testing was routinely performed by ART services prior to treatment initiation. This ‘baseline’ viral load serves as a confirmation of the positive HIV PCR result and is a tool for which subsequent treatment efficacy can be measured.
Study Objective
This study sought to describe the linkage of HIV-infected children to ART care using public sector laboratory testing data.
Sources of Data
Data for this analysis are all HIV PCR and HIV viral load testing results from public sector health services in the Western Cape Province between January 2005 and July 2011. Data came from the central data warehouse of the National Health Laboratory Service, the sole provider of pathology services for the public health sector in South Africa. The following data were available: patient name and provincial folder number; health facility; type and date of test and test result; and patient date of birth and gender. We identified the first positive HIV PCR result for each child under the age of 2 years, and the first HIV viral load for each child under the age of 5 years, for inclusion in the analysis. Test results related to quality assurance/quality control, and tests of patients enrolled into clinical trials, were excluded.
Data Analysis
Data were analysed used Stata Version 11.0 (Stata Corporation, College Station, Texas, USA). We used the date of a child’s positive HIV PCR test result as the date of diagnosis, and used the date of the first HIV viral load as the date of first attendance at ART services. HIV PCR and viral load results for individual children were linked using combinations of folder number, name and date of birth. We defined ‘definite’ links as matching identical full surname or folder number in combination with an identical date of birth and ‘probable’ links as matching any combination of partial surname, date of birth and folder number. However, study findings did not differ appreciably between definitions, and the results presented here are based on all ‘probable’ linkages.
The delay in days between the first positive HIV PCR and the first HIV viral load test was used to estimate the delay between a PCR positive test result and a child’s first attendance at an ART clinic. Children who were HIV PCR-positive but did not have a HIV viral load test were considered to have not attended ART services. A specialist hospital was defined as a hospital where a paediatrician with infectious diseases training was present, while the remaining facilities are primary and secondary care facilities administered by doctors and/or nurses without specific paediatric infectious disease training. An urban facility was defined as the site of testing within the greater Cape Town area; the remaining facilities in the province are considered rural facilities.
In analysis, continuous variables were described using medians and interquartile ranges (IQR) while proportions with exact binomial 95% confidence intervals (CI) were calculated for categorical variables. Logistic regression models were used to examine the independent predictors of (i) positive HIV PCR test results, and (ii) the successful referral of infected children to ART services; the results are presented as odds ratios (OR) with 95% CI. Variables in the model were selected based on a priori evidence and findings of descriptive statistics.
Ethics Statement
The study was approved by the National Health Laboratory Services and the Research Ethics Committee of the Faculty of Heath Sciences at the University of Cape Town.
Results
A total of 83 698 children less than 2 years of age underwent HIV PCR testing at public sector health care services in the Western Cape between 2005 and 2011. Of these, 6322 (7.6%) tested positive, 76 956 (91.9%) tested negative and 418 (0.5%) of PCR results were equivocal (Table 1). The number of HIV PCR tests almost doubled over time, while the proportion of PCR-positive children declined from 12% in 2005 to 3% in 2011. The median age of first HIV PCR testing was approximately 4 months (IQR 3.1–5 months) during 2005 and decreased to 1.5 months (IQR 1.4–2.1 months) during 2011.
Table 1. Early infant diagnosis data, Western Cape, South Africa, 2005–2011.
| HIV PCRpositive | HIV PCR negative | Total | Percent positive | OR (crude) | 95%CI | ||
| Year | 2005 | 1057 | 7594 | 8651 | 12% | 1.0 | (reference) |
| 2006 | 861 | 6193 | 7054 | 12% | 1.00 | 0.91–1.10 | |
| 2007 | 1170 | 11416 | 12586 | 9% | 0.74 | 0.67–0.80 | |
| 2008 | 1097 | 13279 | 14376 | 8% | 0.59 | 0.54–0.65 | |
| 2009 | 1035 | 14640 | 15675 | 7% | 0.51 | 0.46–0.56 | |
| 2010 | 793 | 14931 | 15724 | 5% | 0.38 | 0.35–0.42 | |
| 2011* | 311 | 8903 | 9214 | 3% | 0.25 | 0.22–0.29 | |
| Sex | Female | 3215 | 36648 | 39863 | 8% | 1.0 | (reference) |
| Male | 2848 | 36289 | 39137 | 7% | 0.89 | 0.85–0.94 | |
| Facility | Primary care facility | 3757 | 68605 | 72362 | 5% | 1.0 | (reference) |
| Specialist Hospitals | 2567 | 8351 | 10918 | 24% | 5.61 | 5.31–5.93 | |
| Urban facilities | Rural | 1953 | 22480 | 24433 | 8% | 1.0 | (reference) |
| Urban | 4372 | 54494 | 58866 | 7% | 0.92 | 0.87–0.98 | |
| Age at time of PCR | ≤2 months | 1999 | 41151 | 43150 | 5% | 1.0 | (reference) |
| >2 months | 4326 | 35823 | 40149 | 11% | 2.49 | 2.35–2.62 |
Factors associated with HIV PCR results amongst HIV-exposed children less than two years of age tested for the first time at public sector health facilities in the Western Cape Province of South Africa, January 2005 and July 2011.
For 2011, results are from January to June.
In 2005, 303 health facilities conducted HIV PCR testing, increasing annually to 341 facilities in 2010. Thirteen percent of PCR testing came from hospitals with specialist paediatric services and 69% of PCR tests were from urban facilities around Cape Town. No significant changes in the proportions of specialist hospital and urban PCR testing were observed over the study period; however infants tested at specialist hospitals were much more likely to be PCR positive (p<0.001). Just over half of infants (51%) were tested under 3 months of age, the age targeted for the current EID programme.
During the same period, 11 653 first HIV viral load tests were carried out in children <5 years of age at public sector health care facilities. The median viral load of the samples with detectible HIV was 150 390 copies (IQR 12 975–990 000 copies/ml). The number of facilities that conducted HIV viral load testing rose from 91 in 2005 to 220 in 2010 (Table 2). Sixty-nine percent of the first time paediatric HIV viral load tests was performed in an urban facility; this proportion declined from 73% in 2005 to 60% in 2010.
Table 2. Changes in early infant diagnosis, HIV viral load testing, and linkages to care over time.
| Year | |||||||
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | ||
| Number of facilities testing | HIV PCR | 271 | 276 | 312 | 330 | 322 | 343 |
| HIV Viral load | 91 | 133 | 149 | 203 | 216 | 220 | |
| PCR tests done | 8653 | 7065 | 12603 | 14416 | 15743 | 15922 | |
| Facility | Specialist Hospitals | 1242 | 1430 | 1793 | 1941 | 1839 | 1761 |
| Primary care facility | 7411 | 5634 | 10812 | 12477 | 13904 | 14161 | |
| % from specialist care | 14 | 20 | 14 | 14 | 12 | 11 | |
| Facilities | Urban | 5752 | 4206 | 8997 | 10265 | 11159 | 11120 |
| Rural | 2901 | 2858 | 3605 | 4153 | 4584 | 4802 | |
| % Urban samples | 67 | 60 | 71 | 71 | 71 | 70 | |
| Referral to care | Referred | 576 | 483 | 662 | 758 | 703 | 566 |
| Not referred | 481 | 378 | 508 | 337 | 332 | 227 | |
| % referred | 54 | 56 | 57 | 69 | 68 | 71 | |
Changes in HIV PCR/VL testing facilities and linkage to care for HIV PCR positive children less than two years of age attending public sector health facilities in the Western Cape Province of South Africa, January 2005 to July 2010.
Linkage of PCR-positive Children to ART Services
Using the ‘definite’ matching criteria, we found 3414 of 6322 (54%) children with first positive HIV PCR who also had a HIV viral load conducted prior to ART initiation and were thus considered successfully linked to care. Under the ‘probable’ matching criteria we were able to match a further 691 PCR-positive children to HIV viral load results, resulting in a total of 4105 children (65%) who were HIV PCR-positive and had laboratory evidence of attending ART services.
The distribution of PCR-positive children who were and were not linked to ART services is shown in Table 3. Over the period, the proportion of linked children increased from 54% in 2005 to 71% in 2010. The linkage rate of children diagnosed HIV PCR-positive at specialist hospitals (69%) was substantially higher than at primary care centres (58%); despite contributing 13% of all PCR tests requested, the specialist hospitals accounted for 45% of all children successfully linked to ART services. In particular, Cape Town’s largest paediatric hospital contributed 25% of all children linked to ART services in the province. Related to this, successful linkage of PCR-positive children to ART services was significantly more likely at urban health facilities (68%) compared to rural facilities (50%). This difference appeared independent of urban-rural variation (OR 1.89, 95%CI 1.68–2.14). In addition, children older than 2 months of age appeared to be less likely to be linked (OR 0.73, 95% CI 0.64–0.81) compared to younger infants; this association persisted after adjusting for potential confounding variables such as the year of testing and facility of testing (OR 0.82, 95% CI 0.72–0.92).
Table 3. Proportion of HIV PCR-positive infants linked to HIV treatment services.
| HIV PCR-positive children with linked VL | |||||||
| Linked | Not linked | Total | Percent | OR (crude) | 95%CI | ||
| Year | 2005 | 576 | 481 | 1057 | 54% | 1.0 | (reference) |
| 2006 | 483 | 378 | 861 | 56% | 1.07 | 0.89–1.28 | |
| 2007 | 662 | 508 | 1170 | 57% | 1.09 | 0.92–1.29 | |
| 2008 | 758 | 337 | 1095 | 69% | 1.88 | 1.57–2.24 | |
| 2009 | 703 | 332 | 1035 | 68% | 1.77 | 1.48–2.11 | |
| 2010 | 566 | 227 | 793 | 71% | 2.08 | 1.71–2.53 | |
| Sex | Female | 1924 | 1134 | 3058 | 63% | 1.0 | (reference) |
| Male | 1715 | 994 | 2709 | 63% | 1.02 | 0.91–1.13 | |
| Facility | Primary care facility | 2061 | 1488 | 3549 | 58% | 1.0 | (reference) |
| Specialist Hospitals | 1687 | 775 | 2462 | 69% | 1.57 | 1.41–1.75 | |
| Urban facilities | Rural | 954 | 936 | 1890 | 50% | 1.0 | (reference) |
| Urban | 2794 | 1327 | 4121 | 68% | 2.07 | 1.85–2.31 | |
| Age at time of PCR | ≤2 months | 1257 | 599 | 1856 | 68% | 1.0 | (reference) |
| >2 months | 2491 | 1664 | 4155 | 60% | 0.71 | 0.63–0.80 | |
Factors associated with linkage of HIV PCR positive infants to antiretroviral therapy services among infants attending public sector health facilities in the Western Cape Province of South Africa, January 2005 to December 2010.
Delays from PCR-positive Diagnosis to ART Services
The median delay between the first positive HIV PCR test and the first viral load conducted as part of ART work-up was 146 days in 2005 (IQR 42–500 days) and decreased to 33 days (IQR 8–83 days) during 2010 (Figure 1). The largest decrease was observed during the period 2007–2008, as the delay halved from 81 days in 2007 to 39 days in 2008. Overall, 66% and 85% of these delays were less than 150 days and 365 days, respectively. In 2010, 83% of delays were less than 150 days compared to the 50% during 2005.
Figure 1. Linkage to antiretorivral therapy services.
Proportion of infants testing positive on HIV PCR who are successfully linked to antiretroviral therapy services (as indicated by HIV viral load testing), with median delay between PCR and linked viral load (VL) testing.
The shortest delays in linkage of PCR-positive children to ART services were observed at specialist paediatric hospitals. The median delay of children at these hospitals was 13 days (IQR 5–68 days) compared to all other children who experienced a median delay of 87 days (IQR 28–287 days, p<0.001). The overall trend of reductions in delays over calendar years was similar for the two main specialist hospitals and all other facilities. The major reduction in delays during the 2007/2008 period was observed at both specialist hospitals and primary care centres.
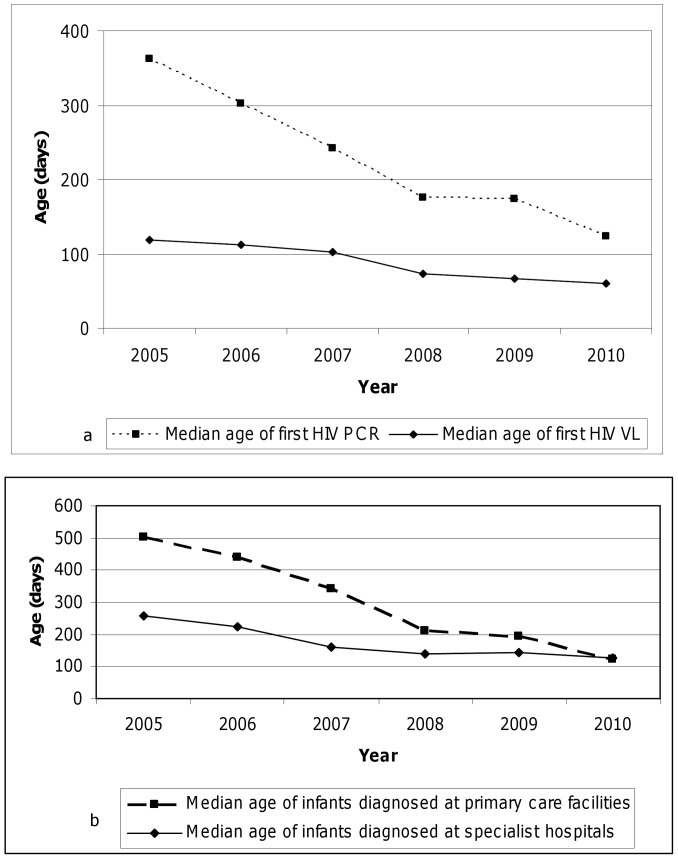
The median age of PCR-positive children undergoing their first attendance at ART clinics, as indicated by pre-ART HIV viral load testing, was 96 days over the entire study period (IQR 50–169 days). This age decreased from 119 days in 2005 to 60 days in 2010, with 2007/2008 being the year of the most significant decrease (from 103 days in 2007 to 73 days in 2008) (Figure 2a). However, the reduction in median age of HIV viral load was mainly observed outside the two specialist hospitals (Figure 2b); the age of first HIV viral load in two hospitals remained constant over the study period.
Figure 2. Age of children accessing early infant diagnosis and antiretroviral therapy services.
2a. The age children (in days) at the time of HIV PCR testing and attendance at antiretroviral therapy clinics (as indicated by HIV viral load testing), by year, among children attending public sector services in the Western Cape province, 2005–2010. The median age of first HIV viral load represent a small subset infants starting ART. This median age is mostly in the first 6 months due to the nature history of HIV disease progression in children. The median age of PCR reflects the age at which PCR testing are being used in all HIV exposed children, including much older children. 2b. The age children (in days) at the time of HIV viral load testing and attendance at antiretroviral therapy clinics, by year, among children attending public sector services in the Western Cape province, 2005–2010. The dotted line represents children diagnosed at primary care facility and the solid like represent children diagnosed at specialist facilities. The time to HIV diagnosis in primary care facilities had shown a great improvement over time, likely due to improved access to EID program. The diagnosis at specialist facilities represents children presenting with disease progression. In order to avoid HIV related paediatric mortality, the age of diagnosis at primary cares sites should be below the age of diagnosis at specialist hospitals.
Discussion
These data demonstrate that only a fraction of children in this setting who test HIV PCR-positive within the PMTCT EID programme are successfully linked ART services. This proportion increased substantially during the period 2005–2010∶71% of the HIV infected infants in 2010 had a subsequent HIV viral load indicating their attendance at ART services. In parallel, among HIV-infected children who were successfully linked to ART services, the time delay between HIV PCR-positive test results and first attendance at ART services decreased in each successive year, though the median delay remained greater than 1 month during 2010.
Our data demonstrate that the number of infants tested doubled over the six year period, while the proportion of infants testing PCR positive declined from 12% to 3%. The reduction in infant HIV prevalence is seen in both asymptomatic children in the primary care setting and infants tested in hospitals. This steady decline points to the successes of the PMTCT programme in the Western Cape province, mirroring gains nationally [18], [19].
Linkage of HIV-infected Infants to ART Services
There are several factors that may contribute to the failure of children testing HIV PCR positive in the EID programme to be linked to ART services. First, an infant could demise before the caregiver received the test result and/or attended the ART clinic. For example one Tanzanian study showed that 14% of caregivers received the EID result after their child had already died [12]. Second, even if a child is alive, HIV PCR test results may not be returned to caregivers. A previous study done in South Africa had shown that of 584 infants undergoing HIV PCR testing for EID at a routine immunization clinic, only 332 mothers (57%) returned to receive the results [13]. This type of loss to follow-up (LTF) is a major challenge, as it increases the risk of morbidity and mortality in infants due to untreated HIV infection [20].
Some of the phenomenon of LTF of mother-infant pairs is likely due to migration patterns of women during pregnancy and postpartum, as there is widespread anecdotal evidence of women from rural areas migrating to urban centres for antenatal care and delivery, and then returning to rural homes early postpartum. This form of ‘health migrancy’ has been documented in many parts of Africa [21], and presents a major challenge to continuity of care in maternal and child health. In the setting of our study this migration between health services may negatively bias our linkage to care estimate; the magnitude of this bias is difficult to estimate. An additional cause of phenomenon of LTF of mother-infant pairs operates at the level of health systems. In South Africa and elsewhere, EID testing is timed to coincide with the first infant immunization visit at 6 weeks of age, with results commonly returned to caregivers at the second immunization visit 10 weeks postpartum. Although this integration of EID into immunization services may reduce the burden of clinic visits for the caregiver, the 4-week interval between testing and receiving results may increase LTF and alternative systems for returning HIV PCR results need urgent consideration. For example, cellphone technology has been used to deliver EID results with some success in Zambia and warrants further investigation [22].
A third concern is LTF of caregiver/infant pairs who are diagnosed as HIV-positive but LTF before attending ART services. Prior to 2008 in this setting all HIV-infected infants were referred to specialist hospitals for ART care, and the time and cost of attending these hospital visits may present a barrier to many caregivers, particularly in rural areas [23]. Since 2008 there has been a shift towards paediatric ART services delivered through community-based primary care services, although since not all clinics offering EID also provide paediatric ART the separation of diagnostic and treatment services remains a barrier to rapid ART initiation in infants. In order to overcome these challenges in paediatric HIV care, a re-engineering of the current health systems to integrate the PMTCT, EID and infant HIV treatment is required. For instance, delivery of HIV specific services at immunization clinics instead of general paediatric clinics had been found to achieve superior uptake in Malawi [24].
Delays in Attending ART Services
The time delay between positive HIV PCR test results and presentation to ART services decreased between 2005 and 2010 but remained more than 5 weeks in the most recent period. Several factors contribute to these delays. First, the number of primary care facilities that provide paediatric ART has increased during the past few years, reducing delays related to geographically distant referrals. Second, HIV testing for EID is based on PCR technology in central laboratories, creating delays around the transport of specimens, testing and return of results; thereafter, infants with positive test results may require referral to separate facilities for ART screening (including baseline HIV viral load testing) and initiation. In light of the steps required, a 4–5 week delay may approach the minimum possible delay under the current system.
The development of point-of-care EID assays based on HIV PCR [25] or HIV p24 antigen detection [26] may play a valuable role in further reducing these delays. Having access to the EID result on the same day using point-of-care testing could mean that appropriate counseling and clinical management can be initiated during the same clinic visit. This could have a positive impact on the proportion of children starting ART as well as the delay between diagnosis and treatment, and this possibility warrants further research.
Strengths and Limitations
The interpretation of these data is subject to a number of limitations. While we included all HIV PCR tests conducted in public sector health facilities across the province, the coverage of the EID programme may not be complete, and the number of HIV-exposed infants who are not tested in the province is unknown. The EID coverage in low- and middle-income countries had been estimated to be around 15% [27]. However this is likely an underestimate for South Africa as more recent local data suggest the coverage in South Africa to be around 68% [1]. Second, we have used ‘baseline’ HIV viral load testing as a marker of attendance at ART services, which presumes that paediatric ART services adhere to policy guidelines and conduct viral load testing at an infant’s first ART clinic visit. While deviations from national guidelines for paediatric ART have not been documented, it is possible that some children were seen at ART clinics but do not have a viral load test; if this is the case, we may underestimate slightly the proportion of infected children who go on to start ART. It is also possible that children may access ART in the private sector and thus are not captured by our method, however private paediatric services account for a very small minority HIV related care in this setting, and thus this phenomenon is unlikely to impact our study findings. Third, as described above, there are multiple steps required for a child to be diagnosed as HIV PCR-positive and linked to ART services. Using laboratory data, we are unable to tell which specific barriers between EID and ART services are most important, and additional research is required to explore these in detail. Finally, these data should be generalized with caution, as the coverage of EID and ART services, and the strength of health systems more generally, varies widely between settings.
In summary, these data demonstrate that the proportion HIV-exposed infants testing PCR positive in the Western Cape province of South Africa has decreased dramatically since 2005. During the same period the proportion of HIV PCR-positive infants who subsequently attended ART services has increased substantially but remains suboptimal. While additional research is required to understand the barriers to successful ART referral, there is a clear need for interventions that facilitate linkage of infants diagnosed as HIV-infected to paediatric ART programmes. As the number of infant HIV infections decline, the absence of a direct system to trace HIV-infected infants and ‘fast track’ them onto ART is emerging as an important need in this setting as elsewhere in South Africa.
Acknowledgments
We would like to acknowledge the South African National Health Laboratory Service for providing the data for the study.
Funding Statement
Landon Myer is funded by the Elizabeth Glaser Pediatric AIDS Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organisation, The Joint United Nations Programme on HIV/AIDS, and The United Nations Children’s Fund (2012) Global HIV AIDS response - Epidemic update and health sector progress towards Universal Access - Progress report 2011. Geneva, Switzerland: WHO.
- 2. Chilongozi D, Wang L, Brown L, Taha T, Valentine M, et al. (2008) Morbidity and mortality among a cohort of human immunodeficiency virus type 1-infected and uninfected pregnant women and their infants from Malawi, Zambia, and Tanzania. Pediatr Infect Dis J 27: 808–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bourne DE, Thompson M, Brody LL, Cotton M, Draper B, et al. (2009) Emergence of a peak in early infant mortality due to HIV/AIDS in South Africa. AIDS 23: 101–106. [DOI] [PubMed] [Google Scholar]
- 4. Dramowski A, Coovadia A, Meyers T, Goga A (2012) Identifying missed opportunities for early intervention among HIV-infected paediatric admissions at Chris Hani Baragwanath hospital, Soweto, South Africa. Southern African Journal of HIV Medicine 12: 16–23. [Google Scholar]
- 5. Violari A, Cotton MF, Gibb DM, Babiker AG, Steyn J, et al. (2008) Early antiretroviral therapy and mortality among HIV-infected infants. N Engl J Med 359: 2233–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation (2010) WHO recommendations on the diagnosis of HIV infection in infants and children. Geneva, Switzerland: WHO. [PubMed]
- 7. Creek TL, Sherman GG, Nkengasong J, Lu L, Finkbeiner T, et al. (2007) Infant human immunodeficiency virus diagnosis in resource-limited settings: issues, technologies, and country experiences. Am J Obstet Gynecol 197: S64–S71. [DOI] [PubMed] [Google Scholar]
- 8. Tejiokem MC, Faye A, Penda IC, Guemkam G, Ateba NF, et al. (2011) Feasibility of early infant diagnosis of HIV in resource-limited settings: the ANRS 12140-PEDIACAM study in Cameroon. PLoS One 6: e21840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ciaranello AL, Park JE, Ramirez-Avila L, Freedberg KA, Walensky RP, et al. (2011) Early infant HIV-1 diagnosis programs in resource-limited settings: opportunities for improved outcomes and more cost-effective interventions. BMC Med 9: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hassan AS, Sakwa EM, Nabwera HM, Taegtmeyer MM, Kimutai RM, et al. (2012) Dynamics and Constraints of Early Infant Diagnosis of HIV Infection in Rural Kenya. AIDS Behav 16: 5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lofgren SM, Morrissey AB, Chevallier CC, Malabeja AI, Edmonds S, et al. (2009) Evaluation of a dried blood spot HIV-1 RNA program for early infant diagnosis and viral load monitoring at rural and remote healthcare facilities. AIDS 23: 2459–2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nuwagaba-Biribonwoha H, Werq-Semo B, Abdallah A, Cunningham A, Gamaliel JG, et al. (2010) Introducing a multi-site program for early diagnosis of HIV infection among HIV-exposed infants in Tanzania. BMC Pediatr 10: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rollins N, Mzolo S, Moodley T, Esterhuizen T, van Rooyen H (2009) Universal HIV testing of infants at immunization clinics: an acceptable and feasible approach for early infant diagnosis in high HIV prevalence settings. AIDS 23: 1851–1857. [DOI] [PubMed] [Google Scholar]
- 14. Creek T, Tanuri A, Smith M, Seipone K, Smit M, et al. (2008) Early diagnosis of human immunodeficiency virus in infants using polymerase chain reaction on dried blood spots in Botswana’s national program for prevention of mother-to-child transmission. Pediatr Infect Dis J 27: 22–26. [DOI] [PubMed] [Google Scholar]
- 15. Braun M, Kabue MM, McCollum ED, Ahmed S, Kim M, et al. (2011) Inadequate coordination of maternal and infant HIV services detrimentally affects early infant diagnosis outcomes in Lilongwe, Malawi. J Acquir Immune Defic Syndr 56: e122–e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chatterjee A, Tripathi S, Gass R, Hamunime N, Panha S, et al. (2011) Implementing services for Early Infant Diagnosis (EID) of HIV: a comparative descriptive analysis of national programs in four countries. BMC Public Health 11: 553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gilks CF, Crowley S, Ekpini R, Gove S, Perriens J, et al. (2006) The WHO public-health approach to antiretroviral treatment against HIV in resource-limited settings. Lancet 368: 505–510. [DOI] [PubMed] [Google Scholar]
- 18.Goga AE, Dinh TH, Jackson DJ for the SAPMTCTE study group (2012) Evaluation of the Effectiveness of the National Prevention of Mother-to-Child Transmission (PMTCT) Programme Measured at Six Weeks Postpartum in South Africa, 2010. South African Medical Research Council, National Department of Health of South Africa and PEPFAR/US Centers for Disease Control and Prevention. 2012.
- 19. Grimwood A, Fatti G, Mothibi E, Eley B, Jackson D (2012) Progress of preventing mother-to-child transmission of HIV at primary healthcare facilities and district hospitals in three South African provinces. S Afr Med J 102: 81–83. [DOI] [PubMed] [Google Scholar]
- 20. Becquet R, Marston M, Dabis F, Moulton LH, Gray G, et al. (2012) Children who acquire HIV infection perinatally are at higher risk of early death than those acquiring infection through breastmilk: a meta-analysis. PLoS One 7: e28510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vearey J (2012) Learning from HIV: exploring migration and health in South Africa. Glob Public Health 7: 58–70. [DOI] [PubMed] [Google Scholar]
- 22. Seidenberg P, Nicholson S, Schaefer M, Semrau K, Bweupe M, et al. (2012) Early infant diagnosis of HIV infection in Zambia through mobile phone texting of blood test results. Bull World Health Organ 90: 348–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Silal SP, Penn-Kekana L, Harris B, Birch S, McIntyre D (2012) Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Serv Res 12: 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McCollum ED, Johnson DC, Chasela CS, Siwande LD, Kazembe PN, et al. (2012) Superior Uptake and Outcomes of Early Infant Diagnosis of HIV Services at an Immunization Clinic Versus an “Under-Five” General Pediatric Clinic in Malawi. J Acquir Immune Defic Syndr 60(4): e107–e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jangam SR, Yamada DH, McFall SM, Kelso DM (2009) Rapid, point-of-care extraction of human immunodeficiency virus type 1 proviral DNA from whole blood for detection by real-time PCR. J Clin Microbiol 47: 2363–2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Parpia ZA, Elghanian R, Nabatiyan A, Hardie DR, Kelso DM (2010) p24 antigen rapid test for diagnosis of acute pediatric HIV infection. J Acquir Immune Defic Syndr 55: 413–419. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organisation, The Joint United Nations Programme on HIV/AIDS, and The United Nations Children’s Fund (2010) Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector - Progress report 2010. Geneva, Switzerland: WHO.