Abstract
Idiopathic scoliosis is a growing spine disorder. Only a perfect knowledge of normal growth parameters such as bone age, stages of puberty, standing and sitting height, arm spam, Tanner stages, and weight allow the surgeon to plan the best treatment at the right moment. Measurements should be repeated and carefully recorded at regular intervals. Puberty is not a sudden event: it has a gradual onset and it is preceded by an incubation phase. It is not a point on a chart: it is a period that lasts two years beginning at a bone age of 11 and 13 years in girls and in boys, respectively. Two years of rapid growth (“acceleration phase”) are followed by three years of steady reduction of growth rates (“deceleration phase”). Skeletal maturation needs to be evaluated carefully to evaluate the progression risk of scoliosis during the phase of accelerating growth velocity. This article explains how to identify pubertal growth spurt, both clinically and radiographically, in order to correctly monitor patients with idiopathic scoliosis.
Keywords: Idiopathic scoliosis, Pubertal growth spurt, Puberty, Growth, Spine
Introduction
Growth is an essential element in the natural history of any orthopedic disorder in the growing child. Idiopathic scoliosis is a disorder of the growing spine. As growth and adolescent idiopathic scoliosis are interrelated, the spine surgeon needs to know the normal values for many of the growth parameters and how to measure them. Consequently, bone age, Tanner classification, stages of puberty, standing and sitting height, arm spam, and weight need to be considered in the analysis of any particular case. A thorough analysis of these parameters helps the clinician to plan the best treatment at the right moment. Duval-Beaupère and Lamireau [1] showed that the pubertal growth spurt is a turning point for idiopathic scoliosis progression: the younger the child, the higher is the risk for progression of a scoliotic curve. Thus, only a perfect knowledge of the normal growth parameters allows the clinician to better understand the risk of progression of a spinal deformity before, during, and after puberty.
Biometric measurements to monitor growth
A height gauge, scales, a metric tape, and a bone age atlas are required at the time of consultation. Measurements should be repeated and carefully recorded at regular intervals. The measurements provide a real-time image of growth, and comparison of the measurements with charts makes decisions easier [2, 3, 6]. The four most important biometric measurements for monitoring growth are:
Standing height is a global marker that consists of two components: sitting height and subischial height. These two regions often grow at different rates, at different times. For this reason, standing height does not always exactly correlate with the loss of trunk height in children with severe spinal deformities. It is therefore important to monitor changes in sitting height rather than in standing height [1–4].
Sitting height correlates strictly with trunk height, and in children with severe spinal deformities, the loss of sitting height is related to the severity of the deformity. Puberty commences at approximately 75 and 78 cm of sitting height in girls and boys, respectively. A gain in sitting height of 12–13 cm corresponds to puberty. When the sitting height is approximately 84 cm, 80 % of girls have menarche [1–4].
Arm span measurement is an indirect evaluation of standing height. Standing height is about 97 % of the arm span with a small gender difference. This relationship remains unchanged throughout puberty and into adulthood. Arm span is particularly helpful to estimate standing height in non-ambulatory children. As a rule of thumb, arm span divided by two is very close to sitting height, and divided by four it is close to the T1–S1 spinal segment [1–6].
Weight is an essential indicator. Children should always be weighed at each consultation. Weight increases by 20-fold between birth and skeletal maturity. A child weighs about 20 kg at age 5 years, 30 kg by age 10 years, and ≥60 kg by age 16 years. As a rule of thumb, it should be kept in mind that during the pubertal spurt, weight usually doubles. In children with a low body weight, the pubertal spurt changes are moderate as weight has to be at least 40 kg for the pubertal spurt to be normal [1–6].
The pubertal cycle
The pubertal cycle is the same regardless of ethnic origin and it follows a stereotypic course. Puberty is not a sudden event: it has a gradual onset and is preceded by an incubation phase. Clinical examination every 6 months allows the clinician to easily assess the growth velocity of the child and of the different body segments. Many decisions rest on recognizing the beginning of puberty, and growth velocity provides the best indicator of this change. The first sign of puberty is an increase in the growth rate of the standing height to greater than 0.5 cm (cm) per month or greater than 6–7 cm per year [7, 8]. At the beginning of puberty, the average remaining growth on the standing height is about 22.5 cm for boys and 20.5 cm for girls. The average remaining growth on the sitting height for boys is about 12.5 and 11.5 cm for girls.
Puberty is not a point on a chart: it is a period that lasts 2 years! Puberty begins at a bone age of 11 and 13 years in girls and boys, respectively. It is characterized by a significant increase in the growth rate [1–6]. Growth charts from Little et al. [7] and Song and Little [8] show that a standing height velocity of >6 cm/year in girls and >7 cm/year in boys is evidence that the patient is within his or her greatest growth spurt [1–6, 9]. This rapid and significant growth rate increase is called “peak height velocity” or the “acceleration phase.” During this phase, the average remaining growth on the standing height is about 16.5 cm for boys and 15 cm for girls, and the average remaining growth on the sitting height is about 8.5 for boys and 7.5 cm for girls. Another parameter which signals the beginning of puberty is Tanner stage 2 [10]. Secondary sexual characteristics develop throughout the course of puberty; the first appearance of pubic hair, the budding of the nipples, and the swelling of the testes are the first physical signs to signal the onset of puberty. In 77 % of boys, the first physical sign of puberty is testicular growth, which occurs, on average, 3.5 years before adult height in attained. In 93 % of girls, the first physical sign of puberty occurs about 2 years before menarche, and final height is usually achieved 2.5–3 years after menarche [1–6, 10].
The first 2 years of puberty, characterized by significant growth, are followed by 3 years of gradual growth characterized by a steady reduction in the growth rate (“deceleration phase”). During this phase, the average remaining growth on the standing height is about 6 cm for boys and 5.5 cm for girls, and the average remaining growth on the sitting height is about 4.1 for boys and 3.7 cm for girls [1–6, 10].
Each year of puberty corresponds to a weight increase of about 5 kg [3]. This information should be kept in mind when brace treatment is being considered. In addition, a scoliosis brace may less effective in a patient whose weight is ≥10 % above normal than when it is less.
Puberty and bone age
Bone age is an essential parameter to evaluate remaining growth.
Puberty starts at bone age 11 and 13 years in girls and in boys, respectively (Fig. 1). One of the first signs that is clearly visible on antero-posterior (AP) radiographs is ossification of the sesamoid bone of the thumb (Fig. 2).
Fig. 1.
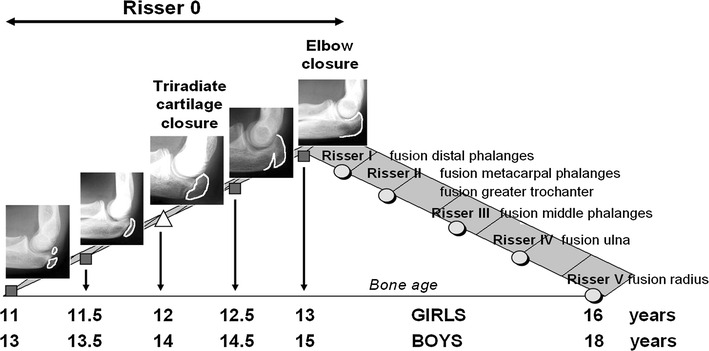
Pubertal diagram. The first 2 years of puberty constitute the acceleration phase. During this period, bone age can be evaluated on lateral elbow radiographs. The acceleration phase is followed by a 3-year period (deceleration phase) characterized by a steady decrease in growth rates [1–6]
Fig. 2.
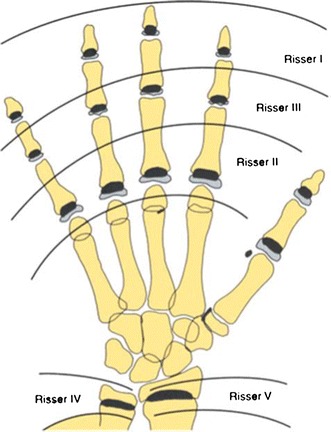
Antero-posterior hand and wrist radiographs. Risser grade I corresponds to fusion of the proximal phalanx. Maturation of the hand correlates with the Risser index [1–6, 11, 13, 15]
Ossification of the triradiate cartilage occurs at 12 and 14 years of bone age in girls and in boys, respectively. It corresponds to the mid-point of the acceleration phase, and the triradiate cartilage ossifies about 1 year after the onset of puberty [1–6, 9]. The acceleration phase ends at age 13 and 15 years of bone age in girls and in boys, respectively. At this point, the elbow (“elbow closure”) and the distal phalanx of the thumb are completely ossified. Once all elbow physis are ossified (radial head, medial and lateral condyle, trochlea, olecranon), remaining growth is about 6 cm in boys and 5.5 in girls. It is important to note that during the whole acceleration phase, the left iliac crest is still not ossified [1–6, 9, 11].
The deceleration phase follows “elbow closure.” At this point, on the AP radiograph of the left hand distal fingers phalanx are ossified. Ossification of the distal phalanx corresponds to Risser grade I. Risser I appears around 13.5 and 15.5 years of bone age in girls and in boys, respectively [6, 9, 12]. However, during the deceleration phase the Risser sign may not be always be present [11, 13–15]. The ossification of the greater throcanter cartilage occurs at Risser II–III or 14.5 and 16.5 years of bone age in girls and in boys, respectively. It corresponds to the mid-point of the deceleration phase.
In girls menarche occurs at age 13.5 years of bone age, usually when at Risser grade I. Menarche most often occurs at the beginning of the deceleration phase, when the rate of growth is slowing down. Little et al. [7, 13] showed that menarche occurs at a median of 7 months after the end of acceleration phase. Unfortunately, the onset of menses is not a predictable and reliable indicator of remaining growth. In these same studies, there was a large range in menarchal age, varying from 11 to 16 years, making this indicator a less precise predictor of remaining growth [7, 13]. However, menarche should be considered as an approximate landmark of the pubertal growth spurt. Menarche occurs during the deceleration phase of puberty: 42 % of the girls experience menarche before Risser I; 31 % at Risser I; 13 % at Risser II; 8 % at Risser III; 5 % at Risser IV. After 2 years of menarche, there is usually no more growth [4, 7, 11, 13]. At Risser I, remaining growth is about 4 cm, and lower extremities have completed growth. Remaining growth is about 3, 2, and 1 cm at Risser II, III, and IV respectively [2–6].
Bone age determination: “To treat complex problems with simple ideas”
Bone age can be determined by using different techniques and radiographs. Greulich and Pyle [16], Sampé and Pavia [17], Roo and Scröder [18], and Tanner et al. [19] described skeletal age assessment by using hand and wrist AP radiographs. However, other radiographs can also be used to assess skeletal age: the so-called “Oxford Method,” originally described by Acheson [20], uses pelvis radiographs, whereas Pyle and Hoerr [21] and Hoer et al. [22] utilize knee and foot radiographs, respectively. It is important that the orthopedist have a good knowledge of these methods and their limitations, especially when faced with difficult cases.
Greulich and Pyle atlas: hand and wrist radiographs
The Greulich and Pyle [16] atlas was introduced in 1959. It is a widely used bone age assessment method. However, this technique has some limitations, especially during puberty. In particular, 11.5 and 12.5 years of bone age in girls and 14.5 years of bone age in boys are not represented in the Atlas. Moreover, hand and wrist AP radiographs between 11 and 13 years of bone age in girls and between 13 and 15 years of skeletal age in boys are difficult to assess [12, 16].
Sauvegrain et al.: elbow radiographs
Sauvegrain et al. [23] developed a method to assess skeletal age by using AP and lateral radiographs of the left elbow. This method was introduced in 1962, and primarily in France and Belgium it has been widely used during the past four decades. The elbow undergoes typical morphological changes at the level of the distal epiphysis ossification centers. These changes are clearly identifiable before and during puberty. For this reason, elbow radiographs are adequate to study skeletal age around and during the pubertal spurt. More precisely, elbow radiographs provide useful information from bone age 10–13 years in girls and from bone age 12–15 years in boys [12, 23].
Dimeglio et al.: elbow radiographs
In 2005, Dimeglio et al., introduced a simplified method to determine bone age from lateral elbow radiographs. Between 11 and 13 years of bone age in girls and between 13 and 15 years of bone age in boys, the olecranon apophysis undergoes distinctive but typical morphological changes which allow the easy assessment of bone age at 6-month intervals [1–6, 9, 12, 23, 24]. Each stage has a distinctive and characteristic morphology:
Double ossification center. It is the beginning of puberty and corresponds to 11 and 13 years of bone age in girls and boys, respectively.
Half-moon shape. This corresponds to 11.5 and 13.5 years of bone age in girls and boys, respectively.
Rectangular shape. This corresponds to 12 and 14 years of bone age in girls and boys, respectively.
Beginning of fusion. This corresponds to 12.5 and 14.5 years of bone age in girls and boys, respectively.
Complete fusion. This is the end of the pubertal spurt (end of the acceleration phase), and it corresponds to 13 and 15 years of bone age in girls and boys, respectively.
There is a simplified method to determine bone age from the olecranon. Based on our experience, this method is reliable and easy to learn, and it allows the pediatric orthopaedic surgeon to quickly assess bone age during the first 2 years of puberty [12].
Sanders et al.: hand radiographs
In 2008, Sanders et al. [25] have introduced a new method for assessing digital skeletal age that was derived from the Tanner–Whitehouse 3 method, which is based on a radiographic analysis of metacarpals and fingers. Eight stages are identified. Stage 3, and stage 4 corresponds to the acceleration phase. Stage 8 is the mature stage and corresponds to Risser grade 5 [25]. This method has been proven to be reliable, and it correlates more strongly with the behavior of idiopathic scoliosis than the Risser sign or Greulich and Pyle bone ages [11, 16, 23–25].
Risser sign: pelvis radiographs
The Risser sign is defined by the amount of ossification of the left iliac apophysisis. It was originally described in 1958 [11]. Children progress from Risser grade I to Risser grade V over a period of 1–3 years. However, during the acceleration phase of puberty, the iliac crest is still non-ossified. During this phase the Risser sign is still 0. Risser grade I appears around 13.5 years of bone age in girls and around 15.5 years of bone age in boys. Risser grade 0 covers about two-thirds of puberty and therefore the notion of Risser 0 can be misleading [11, 13, 14, 23–26].
Information coming from the ossification of the elbow, olecranon apophysis, or hand should complement Risser sign 0, which corresponds to the critical phase of accelerating growth velocity.
The scoliotic risk: anticipation is the key for an effective strategy
The risk of scoliosis varies with growth and is proportional to both remaining growth and the initial angulation of spinal deformity. It is high during the acceleration phase of puberty and it decreases progressively from Risser I through Risser V. A Cobb angle of 25° is frightening at the age of 5 years, an area deserving preoccupation at the onset of puberty, but reassuring at the end of puberty (Fig. 3).
Fig. 3.
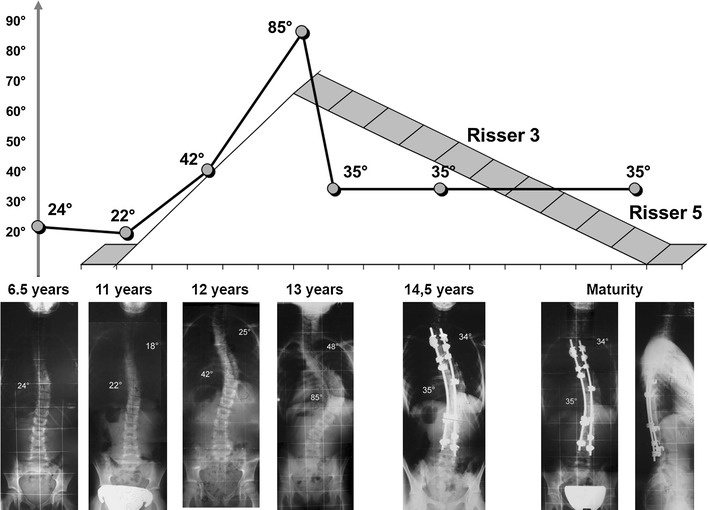
Progression of a spinal curvature during the pubertal growth spurt [1–6, 24]
Duval-Beaupère et al. [27], Lonstein and Carlson [14] and Charles et al. [24, 26, 29] demonstrated that in patients with idiopathic scoliosis, the main curve progression happens at the time of the most rapid adolescent skeletal growth, which is between 11 and 13 years of bone age in girls and between 13 and 15 years of bone age in boys [1–7, 9, 14, 26–29]. These authors also show that bone age, annual growth rate, and sexual secondary characteristics are all important indicators of the beginning of puberty. It is therefore clear that a scoliotic risk evaluation plays an essential role in the treatment of the disease. During the acceleration phase of puberty, a 5° curve is associated with a 10 % risk of progression, a 10° curve with a 20 % risk of progression, a 20° curve with a 30 % risk of progression, and a 30° curve raises the risk to virtually 100 % [1, 14, 26, 27, 29].
Idiopathic scoliosis, especially thoracic curves, tends to progress more during the first 2 years of puberty. About 75 % of curves ranging from 20° to 30° at onset of puberty end up with surgery. The percentage of patients undergoing surgery is almost 100 % if the deformity is over 30° at the onset of puberty (Fig. 3) [1, 24, 26, 29].
As a rule of thumb, the natural history of a scoliotic curve of the spine can be judged on the ascending side of the pubertal growth velocity diagram corresponding to the first 2 years of puberty (acceleration phase). During this period, any spinal curve increasing by 1° each month (12°/year) is likely to be a progressive curve that will require treatment, one increasing by 0.5° each month must be monitored closely, and any curve increasing by <0.5° each month can be considered to be mild [4].
Dimeglio’s simplified methods is a useful tool to assess bone age during the first 2 years of puberty, when the Risser sign is still 0. Information coming from the ossification of the olecranon apophysis complements Risser sign 0, which corresponds to the critical phase of puberty [26].
During the deceleration phase, which starts at 13 and 15 years of bone age in girls in boys, respectively, the elbow is completely ossified, the Risser sign can be I through V, and the risk of scoliosis progression is lower than during the acceleration phase [12, 24, 26, 29].
In particular, at Risser sign I there is a 10 % risk of progression for an 20° curve and a 60 % risk for a 30° curve; at Risser sign II there is a 2 % risk for a 20° curve and 30 % risk for a 30° curve; at Risser III there is a 12 % risk of progression for a curve of ≥20°; at Risser sign IV the risk of progression is markedly decreased; at Risser sign V skeletal maturation has ended [4, 14, 27, 29].
Conclusion
Age is a difficult notion to define. Bone age is a valuable indicator, and it may reduce causes of error if measured repeatedly, but it is a purely conventional measure.
Skeletal maturation needs to be evaluated carefully to evaluate the progression risk of scoliosis during the phase of accelerating growth velocity. The acceleration phase is a crucial period.
The use of morphological changes that characterize the olecranon apophysis during puberty has proved to be particularly simple and reliable method of bone age assessment during the acceleration phase of puberty. This method complements Risser 0, and it should be related to with regular sitting and standing height measurements and Tanner stages.
During the first phase of puberty, which is the ascending slope of the pubertal peak (acceleration phase), the left hand and then the elbow are the best sites to check. On the descending slope (deceleration phase) of the pubertal peak, the most useful elements are the hand and the Risser stage.
Anticipation is the key for an effective strategy. Treat at the right moment.
If there is an increase of the sitting height without worsening of the curve angulation, the treatment is definitely working well. If, on the other hand, an increase in the sitting height is accompanied by deterioration of angulation, the treatment needs to be reconsidered.
Do not stick with an ineffective treatment. Detect a failure of brace treatment early on and switch to surgery if necessary. There is no reason to wait for the end of puberty to do surgery. Be ready to adapt your strategy when puberty starts
Current treatments of patients with significant curvature and residual growth are possible due to screw constructs. Screw constructs can control/reduce the risk of the crankshaft phenomenon. The loss of sitting height will have to be corrected with surgery; it will be compensated for by straightening the curve, and the development of new constructs enables scoliosis to be reduced to 0°.
Conflict of interest
None.
Contributor Information
Alain Dimeglio, FAX: +33-4-73750291, Email: alaindimeglio@wanadoo.fr.
Federico Canavese, Email: canavese_federico@yahoo.fr.
References
- 1.Duval-Beaupère G, Lamireau T. Scoliosis at less 30°. Properties of the evolutivity. Spine. 1985;5:421–424. doi: 10.1097/00007632-198506000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Dimeglio A, Bonnel F, Canavese F, et al. Normal growth of the spine and thorax. In: Akbarnia BA, et al., editors. The growing spine. 1. Berlin: Springer; 2011. pp. 13–42. [Google Scholar]
- 3.Dimeglio A, Canavese F. The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J. 2012;21:64–70. doi: 10.1007/s00586-011-1983-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dimeglio A, Canavese F, Charles YP. Adolescent idiopathic scoliosis: when and how much? J Pediatr Orthop. 2012;31(Suppl):S28–S36. doi: 10.1097/BPB.0b013e32834ee5f8. [DOI] [PubMed] [Google Scholar]
- 5.Dimeglio A. La croissance en orthopedie. Montpellier: Sauramps Medical; 1987. [Google Scholar]
- 6.Dimeglio A. Growth in pediatric orthopaedics. In: Morrissy T, Weinstein SL, editors. Lovell & Winter’s pediatric orthopaedics. 6. Philadelphia: Lippincott, William & Wilkins; 2005. pp. 35–61. [Google Scholar]
- 7.Little DG, Song KM, Katz D, Herring A. Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis. J Bone Joint Surg Am. 2000;82:685–693. doi: 10.2106/00004623-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Song KM, Little DG. Peak height velocity as a maturity indicator for males with idiopathic scoliosis. J Pediatr Orthop. 2000;20:286–288. [PubMed] [Google Scholar]
- 9.Dimeglio A. Growth in pediatric orthopaedics. J Pediatr Orthop. 2001;21:549–555. [PubMed] [Google Scholar]
- 10.Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity and weight velocity and the stages of puberty. Arch Dis Child. 1976;51:170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Risser JC. The iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 12.Dimeglio A, Charles YP, Daures JP, deRosa V, Kabore B. Accuracy of the Sauvegrain method in determining skeletal age during Puberty. J Bone Joint Surg Am. 2005;87:1689–1696. doi: 10.2106/JBJS.D.02418. [DOI] [PubMed] [Google Scholar]
- 13.Little DG, Sussman M. The Risser sign: a critical analysis. J Pediatr Orthop. 1994;14:569–575. doi: 10.1097/01241398-199409000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66:1061–1071. [PubMed] [Google Scholar]
- 15.Shuren N, Kasser JR, Emans J, Rand F. Revaluation of the use of the Risser sign in idiopathic scoliosis. Spine. 1992;17:359–361. doi: 10.1097/00007632-199203000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2. Stanford: University Press; 1959. [Google Scholar]
- 17.Sempé M, Pavia C. Atlas de la maturation squelettique. Paris: SIMEP; 1979. [Google Scholar]
- 18.De Roo T, Schroder HJ. Atlas van de skeletale leeftijd. Dordrecht: Intercontinental Graphics; 1977. [Google Scholar]
- 19.Tanner JM, Whitehouse RH, Marshall WA, Healy MJR. Assessment of skeletal maturity and prediction of adult height (TW2-Method) London: Academic Press; 1975. [Google Scholar]
- 20.Acheson RM. The Oxford method of assessing skeletal maturity. Clin Orthop. 1957;10:19–39. [PubMed] [Google Scholar]
- 21.Pyle SI, Hoerr NL. Radiographic atlas of skeletal development of the knee. Springfield: Thomas; 1995. [Google Scholar]
- 22.Hoerr NL, Pyle SI, Francis CC. Radiographic atlas of skeletal development of the foot and ankle. Springfield: Thomas; 1962. [Google Scholar]
- 23.Sauvegrain J, Nahm H, Bronstein N. Etude de la maturation osseuse du coude. Ann Radiol. 1962;5:542–550. [PubMed] [Google Scholar]
- 24.Charles YP, Canavese F, Dimeglio A. Skelettalterbestimmung am Ellbogen während des pubertären Wachstums. Orthopäde. 2005;34:1052–1060. doi: 10.1007/s00132-005-0856-z. [DOI] [PubMed] [Google Scholar]
- 25.Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90:540–553. doi: 10.2106/JBJS.G.00004. [DOI] [PubMed] [Google Scholar]
- 26.Charles YP, Dimeglio A, Canavese F, Daures JP. Skeletal age assessment from the olecranon for idiopathic scoliosis at Risser grade 0. J Bone Joint Surg Am. 2007;89:2737–2744. doi: 10.2106/JBJS.G.00124. [DOI] [PubMed] [Google Scholar]
- 27.Duval-Beaupère G, Dubousset J, Queneau P. Pour une theorie unique de l’evolution des scolioses. Presse Med. 1970;78:1141–1146. [PubMed] [Google Scholar]
- 28.Dimeglio A, Bonnel F. Le rachis en croissance. Paris: Springer; 1990. [Google Scholar]
- 29.Charles YP, Daures JP, de Rosa V, Dimeglio A. Progression risk of Idiopathic Juvenile scoliosis during pubertal growth. Spine. 2006;31:1933–1942. doi: 10.1097/01.brs.0000229230.68870.97. [DOI] [PubMed] [Google Scholar]


