Abstract
The purpose of this lecture was to give an overview of the natural history of adolescent idiopathic scoliosis (AIS), in order to serve as guidance in the decision of performing surgery or not for the specific patient with AIS. A literature review was performed. Studies concerning long-term outcome in patients with adolescent idiopathic scoliosis that had received no treatment were used. Outcome in terms of curve size, pulmonary function, back function and quality or life/social life was compared. The literature review showed that single thoracic curves of 50°–75° progress 0.73°/year over a 40-year period. AIS do not result in increased mortality, but pulmonary symptoms may be associated with larger curves. Back pain is more frequent among patients with AIS. No study using modern quality of life questionnaires exists, but for social function, childbearing, and marriage no apparent disadvantageous effects were reported compared to the healthy population. The conclusion is that most individuals with AIS and moderate curve size around maturity function well and lead an acceptable life in terms of work and family. Some patients with larger curves have pulmonary problems, but not to the extent that this affects the life span. This needs to be taken into account when discussing surgery with the individual patient.
Keywords: Adolescent idiopathic scoliosis, Natural history, Untreated
Introduction
Most surgeons indicate surgery for curves above 50° in patients with adolescent idiopathic scoliosis (AIS). However, a curve size of 50–80° can be considered more of a grey zone for the decision on performing surgery. The indications used are sometimes hazy and are not always clearly expressed, and concerns include future pulmonary problems and impairment of back function, as well as cosmetic concerns.
The reason for treatment of the individual patient needs to be clarified in each individual patient. The patient also needs correct information in order to be able to make a well-supported decision.
A number of reasons for surgery are regularly mentioned. The deformity itself might progress and cause an increased cosmetic problem for some patients. The major threat, though, is how the pulmonary function is affected over time. Pulmonary function is considered to be at its peak around the age of 20 years or just after, and a slow deterioration begins thereafter as part of the aging process. The gradual decline of pulmonary function from this age might give an extra burden to those who already in adolescence or at maturity have a reduced pulmonary function. An increase of the curve size further adds to the reduction of the pulmonary function. The impact on the patient’s general function, i.e., in the social life as well as in the working life and quality of life, is of great importance to many patients. More specific activities of the patient, i.e., those related to use of the back and affected by back pain, also affect the patient's general well-being. Therefore, the base for decision-making is complex and multifaceted.
The knowledge on what happens to the patient without treatment, i.e., natural history, is needed to support the decision whether to operate or not. The aim of any (scoliosis) treatment is to give the patient an acceptable life, throughout the whole life span.Therefore, knowledge about the long-term outcome of untreated AIS patients is needed.
The purpose of this paper was to give a concise overview of the natural history of adolescent idiopathic scoliosis.
Materials and methods
A literature review was performed. Studies with patients with adolescent idiopathic scoliosis that had received no treatment and long-term outcome were used. Outcomes in terms of curve size and progression, pulmonary function, back function and quality or life or social life was sought after and used for comparison.
Seven studies with enough patients and sufficient length of outcome were found to be suitable for this review, see Table 1.
Table 1.
Papers presenting long term follow up of untreated patients with adolescent idiopathic scoliosis used in this review
| Study | Diagnosis | Year of birtha | Age at FU | FU, y | n (% at FU from original group) | Curve size |
|---|---|---|---|---|---|---|
| Nilsonne 1968 | IS | 1885–1906 | 50–70 | >45 | 102 (90 %) | No radiography |
| Nachemson 1968 | IS (59) + congenital + miscell | 1900–1910 | 30–60 | 30–40 | 117 (90 %) | No radiography. Charts: “only 12 had minor curves” |
| Ascani 1986 | IS | 1940s | m 44 | m 33 (15–47) | 187 (45 %) | 69/187 > 50° |
| Edgar 1987 | IS (all but six had AIS) | 1950–1960 | m 34 | m 17 (10–27) | 77 (77 %) | m 73° |
| Weinstein (1981–2003) | AIS | 1940s | m 66 | m 51 (44–61) | 117 (37 %) | Thoracic m 85°, thoracolumbar m 90°, lumbar m 50°, double major m76°–79° |
a Calculated from information in the respective paper
Two studies, both Swedish, were published in 1968 and included groups of patients with idiopathic scoliosis (IS). The first study by Nilsonne [1] reported on 113 patients with idiopathic scoliosis that had been primarily seen between 1913 and 1918 at the age of 7–34 years. Out of the original group, 46 had died and 11 were lost, resulting in 56 who could be followed more than 45 years later at the age of between 50 and 70 years. The time for onset of the scoliosis was not possible to retract from the charts, i.e., the study included not only patients with AIS.
In the second study, also in 1968, Nachemson [2] reported on patients that had originally been seen between 1927 and 1936 at the age of 1–25 years. This was a mixed group of scoliosis patients, including idiopathic scoliosis, congenital and miscellaneous types. It was noted that 59 out of the 117 followed patients had an idiopathic scoliosis. One hundred seventeen patients (90 % of the original group) were seen at the follow-up 30–40 years later, at ages between 30 and 60 years.
Patients in the first study group had been born approximately between 1885–1906 and in the second group between 1900–1910. Participants of both studies answered a questionnaire, and information was gathered from charts and registers; no radiographies were performed at the follow-up. Original curve sizes were described as moderate to severe and in the Nachemson study chart reviews revealed that “only 12 had minor curves”.
Pehrsson et al. reported further information on the Nachemson study group in a new follow-up published in 1991 [3] and 1992 [4] where mean age was 56 years. New tests for pulmonary function were performed, which could be compared with examinations performed during the 1960s.
The third study group has been followed during life with the first follow-up published by Colles et al. in 1969 [5] followed by a paper in 1981 [6] and the latest follow-up with a mean 51-year (44–61) follow-up [7]. Although a number of patients have been lost during follow-up, the studies of this patient group yields invaluable information, being the longest published follow-up of natural history of patients with AIS alone. At the last follow-up, 117 patients with a mean age of 66 years were followed.
Two other studies, by Ascani et al., published in 1986 [8], and by Edgar et al., published in 1987 [9] and 1988 [10], respectively, also contained useful information for this review. The Ascani study includes 187 untreated patients with idiopathic scoliosis (45 % of the original group) where patients with a mean age of 44 years had been followed for a mean of 33 (15–47) years after maturity. The 78 patients (out of original 100) included in the study of Edgar et al. were a mean of 34 years of age at the mean 17-year (10–27) follow-up.
For the three latter studies, radiographs had been performed at follow-up. Results are detailed in Table 1, the majority of the curves being above 50°. The patients from the Ascani et al. study, as well as the patients from Iowa, all were born during the 1940s, and from the Edgar study, with a somewhat shorter follow-up, during 1950–1960s. The fact that these three studies include patients born considerably later than those from the first two studies (1, 2) might explain the accuracy of the diagnoses of the patients, the stricter study groups, and the possibility for comparison with earlier radiographs.
Outcomes thought to be of relevance were: death (mortality rate), health impairment (including cause of deaths), curve progression, quality of life or social/working capacity and deformity/cosmetics. All studies did not include all types of results.
Results
Mortality
Nilsonne found that mortality increased 2.2 times in all patients with idiopathic scoliosis and 3.2 times for patients above 45 years of age. In the Nachemson study, the expected death rate was double that of the normal population. Further analysis showed that the patients with “miscellaneous cause” or congenital scoliosis had a significantly raised death rate in comparison with the idiopathic group. Ascani reported a mortality rate in patients with IS of 17 %, which was double compared to the normal.
In the Pehrsson follow up of the Nachemson study group from 1968, it was found that AIS does not result in increased mortality, compared to infantile or juvenile types (Fig. 1).
Fig. 1.
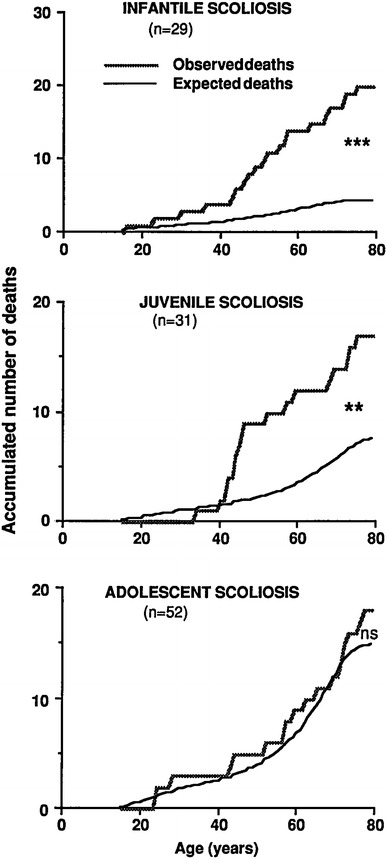
Cumulated number of observed deaths in patients with infantile, juvenile and adolescent scoliosis, and expected deaths. (Reprint with permission from Spine; [4])
These results are in line with the Weinstein’s 50-year follow-up series published in 2003, where the chance of surviving to age 65 is similar to a matched population. In 3 of the 36 deceased patients in this group, scoliosis was thought to contribute to death: one patient 63 years of age with a thoracic curve of 140°, one patient 69 years of age with a thoracic curve of 140°, and one patient 53 years of age with a double curve of 102/70°.
Based on those studies, it therefore seems safe to conclude that AIS does not result in an increased mortality rate.
Health impairment
Cause of death due to cardio-pulmonary diseases was found in 60 % of the patients in the Nilsonne et al. study, while Nachemson et al. reported 80 %. Moreover, Nachemson et al. found that 15 out of 97 had serious heart and lung problems, of which 10 were on continuous medication. In the Ascani series with patients with thoracic curves of about 40°, 35 % had cardio-pulmonary symptoms. These studies however did not include only adolescent-type idiopathic scoliosis.
Respiratory failure
Pehrsson et al. found that large Cobb angles, low spirometric values and low total lung capacity were strong predictors of development of respiratory failure. A respiratory failure occurred 20 years later only in those with a vital capacity percent predicted less than 45 % and a curve size of greater than 110°. Respiratory failure develops in adults with scoliosis with a large curve size and a low vital capacity, while normal aging reduces the ventilatory capacity further. Respiratory failure can develop despite an unchanged scoliosis curve because of the normal aging.
These patients need to be monitored closely to discover an impaired respiratory function. An exaggerated decline of vital capacity can also be due to other factors, such as obesity, smoking or reduced diaphragmatic function.
In the 50-year follow-up of the Iowa patients it was found that 22 % of the patients had shortness of breath in every day activities in comparison to 15 % of the controls. This was associated to the scoliosis if the curve was thoracic and the curve size was above 80° or if large degrees of rotation of the curve existed.
Based on those studies, it therefore seems safe to conclude that pulmonary symptoms may be associated with larger curves.
Curve size/progression
Ascani reported that all curves increase after maturity with a general progression of mean 0.4° per year; the greater the curve at maturity the greater the increase. Thoracic curves tend to increase more than lumbar curves, and thoracic curves above 40° at maturity increased a mean of 20° per 33 years. Lumbar curves 80–90° at maturity increased a mean 1° per year over a 17 year period, as found by Edgar (1987).
Detailed information is found in the Iowa series 40 years follow-up, where 68 % of 133 curves in 102 patients were found to have increased since maturity. Single thoracic curves between 50° and 75° increased with a mean of 0.73° per year, 29.4° over a 40 year period. Additionally risk factors were increased apical vertebral rotation of more than 30 % and a Mehta angle above 20°.
At the 51-year follow-up, thoracic curves were mean 84° (mean 60° at maturity), thoracolumbar curves were mean 89° and 44°, and the thoracic component of double major curves 66° and 79°, respectively. For lumbar curves, the increase was mean 14° up to a curve size of 49° and for the lumbar component of double major curves increased 16° to mean 76°. In addition, 91 % of the patients showed evidence of arthritis or had other radiographic changes such as endplate abnormalities or osteopenia.
Back pain and function
The prevalence for back pain has been reported to be increased, but the severity may or may not be increased. Nilsonne reported that 90 % of the patients had back symptoms, while Nachemson found that 40 % had back pain. Low back pain occurred in 52 % of the patients in the Edgar study; the pain was not correlated to the curve, however, but rather to degenerative spinal changes. Sixty to seventy per cent of the Ascani patients reported the severity being modest or occasional back pain.
In the studies from Iowa, where all the patients had AIS and information on curve sizes could be found (see Table 1), 61 % of the patients admitted back pain at the 51 year follow-up; however, the majority had only mild or moderate pain.
Quality of life/social life
The patients who were middle-aged during the 1960s were working in 53 % in the Nilsonne series, while in the Nachemson study 71 % worked, the rest was disabled by the back and unable to work. Difficulties with physical activities was reported in the Nachemson series, especially in female patients with curve size >40°. In the Edgar series, with patients mean 34 years old during the 1980s, 94 % of the patients were working.
Ninety-eight per cent of the patients in the Iowa series, being mean 66 years of age at the “51 year follow-up”, were working, and the work and the level of disability was the same as the age—and sex-matched control group in the study.
Before the era of validated quality-of-life questionnaires, the social life was the existing measure of the acceptance and ability to live “a normal life”. Marriage rate was one measure of social success. In the Nilsonne series 24 % of the patients were married, and Ascani et al. reported 42 % marriage in patients with thoracic curves above 60°; other curve types however had higher marriage rates. A higher rate of marriage was reported by Edgar et al., 82 %, as well as from the Iowa series with 98 % of patients married.
Mental health is one aspect of the quality of life. Edgar reported that 10 % of the patients received treatment for depression and Ascani noted that 19 % had psychological disturbances. A validated questionnaire for diagnosis of depression was used in the last Iowa follow-up in 2003, making the potential for finding all patients with psychiatric problems higher than in previous studies. Despite this, they did not find any mental problems needing psychiatric treatment, with no difference towards the control population.
Cosmetic problems
Edgar found that 56 % of the patients were self-conscious or depressed about their body shape. If the curve size was above 90°, 77 % had those problems. Ascani noted that the patients reported a better cosmetic appearance at follow up than at maturity, despite a progression of the curve. At the 40-year follow up from Iowa, 21 % of the patients reported mild psychological reactions due to the deformity.
Summary
A summary of potential future risks to use for the decision of surgery or not in AS patients can be seen in Table 2.
Table 2.
Summary of risk for negative outcome in terms of various variables for idiopathic scoliosis
| Outcome variable | Increased risk or prevalence? | If? |
|---|---|---|
| Mortality | No increased risk | |
| Health impairment | Risk for respiratory failure after 20 years IF | Curve size >110° AND VC % predicted <45 % |
| Shortness of breath | Increased risk IF | Curve size >80° OR large degrees of rotation |
| Curve progression | Risk for progression for | Single thoracic curve 50–75° <1°/year |
| Back pain | Increased prevalence, but mostly mild/occasional | Lumbar curves not worse |
| Quality of life and function | As the normal population | |
| Cosmetic problems | Not a problem in most patients |
Regarding mortality, no increased mortality has been found.
The general health will be negatively affected by the development of a respiratory failure. Only patients with curve size above 110° and vital capacity (measured as per cent predicted) less than 45 % at maturity develop respiratory failure 20 years later. Moreover, an increased risk for shortness of breath exists if the curve at maturity has a size above 80° or includes a large degree of rotation.
There is a risk for curve progression for single thoracic curves of 50–75° with a rate of just below one degree per year.
The prevalence of back pain is increased, but the pain is mostly mild or occasional, and lumbar curves are not worse than other curves.
Quality of life and function will be at the same level as in the normal population. Cosmetic problems are not a major problem in most patients.
The predominant reasons for choice of whether to undergo surgery or not must be to counteract a development of respiratory symptoms, either milder symptoms or a fully developed respiratory insufficiency. Future curve progression must therefore also be taken into account.
Conclusion
AIS does not result in increased mortality, but pulmonary symptoms may be associated with larger thoracic curves. Single thoracic curves of 50–75° progress mean 0.73°/year over a 40-year period.
Back pain is more frequent among patients with AIS. No studies exist using modern quality of life questionnaires, but for social functioning and marriage rate no apparent disadvantageous effects were reported compared to the healthy population.
References
- 1.Nilsonne U, Lundgren KD. Long-term prognosis in idiopathic scoliosis. Acta Orthop Scand. 1968;39:456–465. doi: 10.3109/17453676808989663. [DOI] [PubMed] [Google Scholar]
- 2.Nachemson A. A long term follow-up study of non-treated scoliosis. Acta Orthop Scand. 1968;39:466–476. doi: 10.3109/17453676808989664. [DOI] [PubMed] [Google Scholar]
- 3.Pehrsson K, Bake B, Larsson S, et al. Lung function in adult idiopathic scoliosis: a 20 year follow up. Thorax. 1991;46:474–478. doi: 10.1136/thx.46.7.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pehrsson K, Larsson S, Oden A, et al. Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine. 1992;17:1091–1096. doi: 10.1097/00007632-199209000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Collis DK, Ponseti IV. Long-term follow-up of patients with idiopathic scoliosis not treated surgically. J Bone Joint Surg [Am] 1969;51:425–445. [PubMed] [Google Scholar]
- 6.Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg [Am] 1981;63:702–712. [PubMed] [Google Scholar]
- 7.Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559–567. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- 8.Ascani E, Bartolozzi P, Logroscino CA. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine. 1986;11:784–789. doi: 10.1097/00007632-198610000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Edgar MA. The natural history of unfused scoliosis. Orthopedics. 1987;10:931–939. doi: 10.3928/0147-7447-19870601-12. [DOI] [PubMed] [Google Scholar]
- 10.Edgar MA, Mehta MH. Long-term follow-up of fused and unfused idiopathic scoliosis. J Bone Joint Surg [Br] 1988;70:712–716. doi: 10.1302/0301-620X.70B5.3192566. [DOI] [PubMed] [Google Scholar]


